Glioma, which affects parts of the brain, is a heterogeneous tumor that develops from neuronal precursor cells. This is the most common type of primary malignant neoplasm in the head cavity. The total number of malignant lesions of the central nervous system is 60%.
In photographs it often looks like a nodule with poorly defined, blurred boundaries. It is localized mainly in the area of the optic nerve or ventricles, less often in the brain stem structures. Dimensions range from 2-50 mm. Usually grows slowly with no metastasis process.
Classification of pathology
Glioma is a form of malignant neoplasm that develops in the structures of the brain, which determines the nature and degree of manifestations. There are several types of pathology. Classification is carried out according to the following criteria:
- Localization (subtentorial, supratentorial).
- Degree of malignancy.
- The nature of the course is the rate of development of pronounced clinical symptoms after a latent, hidden period.
- The ability to grow and spread into surrounding tissues.
- Rate of progression.
Glioma formed in the brain is a malignant tumor that grows from auxiliary nerve cells (glia), and is not a consequence of metastases penetrating the central nervous system, which indicates the primary nature of the neoplasm. In medical practice, it is believed that brain glioma is formed as a result of pathological changes in astrocytic (astrocytoma), oligodendroglial (oligodendroglioma) or ependymocyte (ependymoma) germs.
There are mixed forms of pathology: oligoastrocytomas, astroblastomas, neoplasms of the choroid plexus. Recent studies show that the disease develops in the presence of underdeveloped, damaged, slowly dividing glial cells. Malignant degeneration usually does not affect mature, full-fledged cells of brain structures. The type and phenotype of the pathology depend on genetic factors.
Diffuse
Diffuse glioma is characterized by scattered distribution in the tissues of the medulla. The tumor may form a node followed by diffuse proliferation into surrounding tissues or develop without a central node. A diffusely growing tumor cannot be completely removed during surgery. Even under a microscope, the boundaries between areas of healthy and degenerated cells are difficult to distinguish.
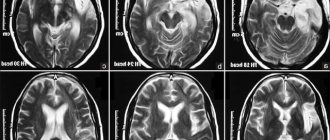
Symptoms are nonspecific due to diffuse damage to different parts of the brain. Diagnosis is difficult for the same reason. The MRI image shows changes in tissue structure. A biopsy does not give a clear answer to the question of whether diffuse glioma is benign or malignant in the brain, because the histological structure of the tumor may differ in different areas of the lesion.
Diffuse glioma affecting the brain stem in children usually has a high level of malignancy and a poor prognosis. It disrupts the functioning of all vital systems of the body. Gliomatosis in brain structures develops from macroglial cells and is characterized by damage to the myelin sheaths and diffuse tissue damage.
Optic nerve glioma
This type is more often diagnosed in children. It grows in the area of the optic nerve, spreading into the chiasm zone or cranial cavity. It manifests itself as a deterioration in visual function, atrophic changes in the tissues of the optic nerve, and a state of exophthalmos - pathological protrusion of the eyes while maintaining the size of the eyeball.
Chiasm lesion
Chiasm is a site located at the base of the trunk in the diencephalon region. It is a plexus of optic nerves. As the tumor grows, it penetrates into the cavity of the eye orbit, hypothalamus, and ventricle. It manifests itself as metabolic disorders, deterioration of the endocrine system, decreased visual acuity, and cerebral hypertension. The disease is curable with an exophytic form of growth - germination into a free cavity, and not inside the tissues of the organ. The tumor is removed during surgery.
Low-grade glioma
Low-grade neoplasms grow slowly. The prognosis for a similar glioma found in the brain of children is unfavorable. If the tumor affects vital structures, death is possible. This form of pathology is diagnosed in children aged 5-15 years; the total number of malignant brain lesions is 30-40%. With a diagnosed glioma, which is characterized by a low degree of malignancy, the patient can live longer than 7 years.
What symptoms accompany cancer pathology?
The clinical picture unfolds as the tumor develops. Malignant tumors grow quickly, while benign ones grow slowly. Glioma is characterized by infiltrative growth. Symptoms depend on the location of the tumor and its nature. Manifestations of a growing glioma resemble signs of neurological disorders, so for a long time patients do not suspect the presence of a tumor. A person is bothered by frequent headaches, dizziness, and tinnitus. If the tumor covers the optic nerve, there is a sharp drop in vision, protrusion of the eyeball, and involuntary eye movements. Brain stem glioma disrupts the activity of the vestibular apparatus, impairs speech and hearing, and affects the mental state. Symptoms of brain tumor pathology:
The pathology is manifested by such signs as loss of orientation in space and memory lapses.
- headache that is not relieved by medications;
- nausea and vomiting;
- seizures;
- paralysis of the nerves of the face, vocal cords, limbs;
- loss of orientation in space;
- "dropsy of the brain";
- distortion of skin sensitivity;
- memory impairment or loss;
- epilepsy attacks;
- feeling of heaviness in the eyeballs.
The growth of glioma provokes changes in the patient’s psyche and behavior; he becomes irritable and aggressive.
Symptoms
Pronounced signs of pathology appear in the later stages of development, when the neoplasm grows and begins to compress surrounding structures. The life prognosis for children and adults is relatively unfavorable. Life expectancy with diagnosis varies depending on the type of tumor and the nature of its course. A child with brain damage often develops macrocephaly - a significant increase in the size of the head.
In childhood, the growth of a malignant tumor is accompanied by a lag in mental and physical development, pain in the head or back, nausea, dizziness, loss of appetite, and sleep disturbance. Motor disturbances, paralysis, and convulsions are possible. Symptoms of glioma affecting the brain in adults include:
- Pyramid disorders. Disorders resulting from damage to the pyramidal tracts are manifested by pathological changes in motor skills, paralysis of the limbs, spasticity, and unnatural foot and wrist reflexes.
- Malfunctions of the vestibular apparatus.
- Deterioration of cognitive abilities, dementia.
- Pain in the head area.
- Epileptic seizures.
- Cranial neuropathy. Disorders of the functions of the cranial nerves, which are accompanied by deterioration of vision and hearing.
- Cerebral hypertension.
- Sensory deficit.
- Sensitivity disorder.
Symptoms of glioma depend on its location. Symptoms intensify if the tumor grows into the space filled with cerebrospinal fluid - the tract and ventricles. The circulation and outflow of cerebrospinal fluid is disrupted, which provokes the development of hydrocephalus and an increase in intracranial pressure.
Symptoms of brain glioma
Symptoms of brain glioma depend on the location and are:
- primary focal, they arise due to the direct impact of the oncological tumor on the brain structures or due to ischemia of a tissue area or substance that compresses the tumor;
- secondary focal, occur when the medulla is displaced and/or pinched in the foramina: greater occipital or tentorial, as well as due to ischemia of the cerebral zone, which is not adjacent to the oncological process, but receives nutrition through vessels that are compressed by the tumor.
Early symptoms of brain tumors
Symptoms of frontal lobe tumors
The frontal lobe is larger than other brain regions and is located anterior to the central one and extends downwards to the lateral fissure, which is called the Sylvian fissure. The most commonly diagnosed neuroepithelial glioma of the frontal lobe of the brain and meningioma.
- Tumors of the medial and basal region of the frontal lobe
They are manifested by age-related mental disorders of the patient.
With emotional disorders, patients:
- emotionally overexcited, aggressive and prone to depression;
- cannot critically assess their condition and behavior;
- with a decrease in intelligence, they lose interest not only in everyone around them and work, but also in treatment.
Symptoms of brain glioma in the frontal lobe confirm epileptic seizures.
Based on the results of a neurological examination, it is stated:
- anisoreflexia (increased reflexes on the opposite side);
- pathological reflexes on the palms and chin;
- frontal ataxia;
- oral automatism.
If the frontal lobe is affected in the posterior regions, mild muscle paresis is noted on the opposite limbs and the lower half of the face.
Early symptoms of brain glioma in the precentral gyrus are characterized by movement disorders. Due to slowly growing formations: astrocytomas, meningiomas, angioreticularis, ischemia of nearby brain tissue begins, and motor cells of the cortex are irritated. This is indicated by periodic clonic muscle spasms on the side opposite the tumor, without loss of consciousness.
The growing tumor formation further irritates the cortex, involving other muscle groups in the convulsive syndrome. In children, seizures are short, like convulsions. With further growth of the formation, the motor cells are destroyed, so the convulsions gradually stop, but paresis and paralysis occur.
Malignant intracerebral lesions affect the motor area, so progressive monoparesis or hemiparesis increases, but there are no seizures. If they affect the frontal lobe, then there will be no sense of smell, that is, anosmia or hyposmia will appear on the affected side or on both sides.
If the left frontal lobe near the posterior part is affected, speech motor skills are disrupted: it slows down, is sometimes interrupted, and is lost. Patients have difficulty pronouncing complex words and phrases with letters that sound different, such as “r”. It all ends with motor aphasia - loss of the ability to speak, but speech understanding remains.
- Symptoms of meningioma and other tumors
Read here: Somatostatinoma: features of development and growth
With the slow growth of meningioma - an extracerebral tumor located in the area of the falx cerebri, in the fossa of the skull in front, less often - on the side of the brain, there may be no symptoms. When it becomes huge, the patient will constantly be bothered by a headache. Further symptoms are characterized by a slow increase in mental changes. At the same time, criticism is reduced. It is possible to detect congested optic discs, and their secondary atrophy also occurs. If the sense of smell is impaired, then the meningioma is localized in the fossa of the skull in front.
Diagnosis of glioma in the frontal lobe
To diagnose a glioma in the frontal lobe, do the following:
- electroencephalography. It clearly detects an active pathological focus;
- echo-encephalography - to detect a displaced signal, M-echo - to determine tumor clots in the posterior sector of the frontal lobe;
- pneumoencephalography - to identify changes in the configurations of the anterior horns in the lateral ventricles;
- angiography - to detect in the frontal pole an arcuate displacement of the cerebral artery with branches from the front to the opposite side;
- CT scan for a clear idea of the size and location of the cancer node.
Symptoms of tumors in the parietal lobe
The parietal lobe consists of the postcentral gyrus, parietal lobes: superior and inferior.
The tumor focus in the postcentral gyrus manifests itself:
- attacks of paresthesia on the back of the body increasing in frequency and duration;
- loss of sensitivity, and successively: mild hypoesthesia, mono- and hemihypesthesia;
- convulsions, paresis, paralysis, if the motor cells of the precentral gyrus are irritated if it is close to the tumor formation.
In the superior parietal lobule of the cerebral cortex, the tumor creates painful paresthesia. They can spread to the torso and limbs on the opposite side. Sensitivity in the muscle-articular, two-dimensional-spatial and area of its localization is deeply upset. The patient does not feel the position of the hand in space; he has apraxia and ataxia. With paresis of the arm, muscle atrophy of a flaccid nature is possible. After arm muscle spasms and paresthesia, an epileptic seizure may begin.
In the inferior parietal lobule, a tumor formation disrupts superficial sensitivity. If it is located near the motor zone, then it manifests itself as convulsions, and at the same time movements are disrupted. Before an epileptic seizure, convulsions of the facial muscles occur on the opposite side, and later - in the upper and lower limbs. Paresthesia attacks before a seizure (skin sensitivity disorders) follow the same path.
If the gyrus of the dominant hemisphere is affected, then visuospatial analysis and synthesis are disrupted, and the following occurs:
- alexia - reading becomes frustrated;
- agraphia – writing is impaired;
- acalculia – loss of ability to count.
Diagnosis of tumors of the parietal lobe
Brain cancer in the parietal lobe is diagnosed:
- angiography: detect displaced branches of the anterior cerebral artery, pathological vascular changes (glomeruli, tortuous passages);
- for meningioma - contrast study of blood vessels to identify the location, size and boundaries of the formation and the vessels supplying it with blood;
- pneumoencephalogram, while observing how much the ventricles have shifted in the direction opposite to the tumor.
Symptoms of temporal lobe gliomas
The middle fossa of the skull includes the temporal lobe; it is delimited from the frontal lobe by the lateral groove. There are medial contacts of the third ventricle and midbrain with the temporal lobe.
Intracerebral lesions irritating the posterior parts of the temporal gyrus from above lead to epileptic seizures after hallucinations:
- visual (the patient can admire paintings of nature, paintings, animals and people on a non-existent wall);
- gustatory (a metallic taste is felt in the mouth, a burning sensation);
- olfactory (smells like rotten eggs, kerosene, smoke, rotten food);
- auditory (machines and devices make noise in your head, mice squeak, grasshoppers chirp, music sounds);
- visceral: attacks of angina, bloating, belching and pain.
As the tumor in the temporal lobe progresses, the frequency of hallucinations and epileptic seizures may increase and then stop. The patient thinks that recovery is coming, but in fact the corresponding cortical taste, auditory and smell centers are destroyed in the brain. Relapse of the disease destroys the cortical centers on one side without changing the function of these analyzers.
With partial damage to the optic tract, homonymous hemianopia is observed: complete, partial or quadrant, that is, partial blindness with loss of perception of the same halves of the visual field: left or right.
If the left temporal, parietal and occipital lobes are affected, then hearing, speech analysis and synthesis are impaired. Further, with the onset of the development of sensory aphasia, the patient already loses understanding of the speech of others and cannot speak coherently and correctly himself.
The nature of tumor formation and its growth rate affect the clinical picture and course of the disease.
Namely:
- When meningioma grows slowly, it does not produce symptoms, only when it is large in size, general cerebral symptoms slowly increase;
- the formation of benign formations - astrocytomas, oligodendrogliomas is also long-term, but accompanied by pronounced symptoms of lesions;
- glioblastomas and other cerebral malignant lesions grow rapidly, increasing the volume of the temporal lobe and forcing the hippocampal gyrus to penetrate into Bichat's fissure or tentorial foramen, which form the brain stem and the edge of the cerebellar tentorium notch.
Diagnosis of temporal lobe gliomas
Investigated for glioma:
- a pneumoencephalogram, on it the lower horn will not be identified in the lateral ventricle, or its compression will be noticeable. The ventricles will be displaced in the direction opposite to the tumor. The lateral ventricle will be pressed upward, and in the third ventricle the arcuate bend will also be pressed in the opposite direction from the tumor.
- echoencephalography to detect a shift of the M-echo signal in the direction opposite to the oncological process.
- angiography to determine: deviation of the middle cerebral artery with branches upward, rectangular displacement of the anterior cerebral artery beyond the central line, and to detect newly formed vessels if there is its own vascular network in the temporal lobe.
- for meningioma - a cranial radiograph, which is necessary to identify the destruction of the pyramid of bones: temporal or the bottom of the middle cranial ventricle (Yaad Ki). The scaly part of the temple bone becomes thinner or destroyed when the formation is convexital and when it emerges under the temple muscle.
Symptoms of tumors of the occipital lobe
The occipital lobe is considered the smallest. At the border with the parietal and temporal lobes, it is divided by the calcarine groove into a wedge above and a lingual gyrus below.
The initial stages of the oncological process in the occipital region are manifested by visual hallucinations - photopsia. The patient sees bright flashes of light, circles, lines, stars that appear in both eyes, but in opposite visual fields.
Next, the centers of vision begin to collapse, so vision begins to fall out, like homonymous hemianopsia: complete or partial (quadrant). In this case, the central field of vision is preserved or lost. Later, dyschromatopsia occurs in the visual fields from opposite sides - color perception is disrupted.
If both lobes are affected, then complete optical agnosia begins - visuospatial analysis and synthesis are disrupted. New formations in the occipital region cause the development of corresponding lesions in the parietal lobe.
When the cerebellum is compressed, ataxia, areflexia, muscle hypotonia appear, and gait becomes unsteady. Before epileptic seizures, photopsia of the visual aura begins.
Diagnostics . Auxiliary methods are used to obtain additional information about the location of the oncological process: vertebral angiography, pneumoencephalography, CT.
Read here: Hodgkin's lymphoma, what is it?
Symptoms of subcortical tumors
Subcortical include formations that affect the striatum: the thalamus and nuclei: in the form of lentils and with tails. They (usually glioblastoma) also involve in the oncological process the internal capsule, the plate of the roof, the cerebral peduncle with the ventricles, which are located nearby.
Characteristic signs:
- hypertension inside the skull with rapid or slow progression;
- in the nerves of vision - stagnant discs;
- tremor of the limbs on opposite sides;
- changes in muscle tone;
- dystonia;
- autonomic disorders on opposite sides: pathological sweating, dermographism, difference in skin temperature, vascular reactions.
Diagnostics
Carry out:
- CT to clearly determine the size and location of glioma;
- angiography to detect: upward displacement of the pericallosal artery, straightening and downward displacement of the proximal zone of the middle cerebral artery, arcuate displacement of the anterior cerebral artery anteriorly, for contrasting tumor vessels;
- electroencephalography to detect pathoactivity emanating from the depths of brain structures.
Symptoms of oncological process in the lateral ventricles
Glial ependymoma grows into one of the walls of the lateral ventricle, meningioma forms in its cavity.
The main signs of glioma are characteristic:
- intracranial hypertension with paroxysmal and intense headache with acute dilatation of the ventricle;
- the appearance of vomiting, fainting;
- position of the head in case of occlusive disorders: the patient is forced to throw it back or tilt it to the side;
- congestive optic discs, decreased vision;
- epileptic seizures without previous phenomena, but at the same time tonic convulsions appear;
- mental changes: memory deteriorates, lethargy and lethargy appear;
- with the growth of ependymoma and irritation of the roof plate, compression of the cerebrum: manifestation of paresis of the upper gaze, spastic hemiparesis, hemihypesthesia and diplopia.
Diagnostics . To identify tumor formations in the ventricles, the cerebrospinal fluid, where the level of protein is usually exceeded, is examined, xanthochromia (yellow tissue) and cytosis (increased levels of cellular elements) are determined.
Venticulography is performed to detect hydrocephalus.
A CT scan shows where the tumor is located, what its size and nature are, and where it originally developed from.
Symptoms of oncological process in the third ventricle
With a long-term asymptomatic course of glioma and meningioma, astrocytoma, the oncological process increases and in case of liquorodynamic disorders and repeated hydrocephalus, it “signals”:
- attacks of headache accompanied by vomiting, which depends on changes in the position of the body or head;
- fainting, restless movements, weakness, falling, loss of consciousness, decerebrate rigidity when changing position;
- rare attacks of epilepsy;
- pathological drowsiness;
- paroxysms accompanied by high blood pressure, vegetative-vascular disorders, that is, the appearance of red spots on the body, profuse sweating, disturbances in breathing and heart rhythm;
- mental disorders. Namely: the patient becomes lethargic, depressed, constrained, aspontaneous, his consciousness is confused, but may, on the contrary, be restless, foolish, euphoric;
- congestive optic discs.
Tumors at the bottom of the ventricle atrophy the visual nerves and change its fields - leading to bitemporal hemianopsia, as well as endocrine metabolic disorders associated with sexual activity:
- hypofunction of the gonads occurs, premature puberty;
- sexual weakness and amenorrhea are noted;
- no sexual desire;
- secondary sexual characteristics are underdeveloped.
Diagnostics. The cerebrospinal fluid is examined for the presence of a protein, the level of which always increases in gliomas, and the number of cells increases.
Symptoms of cancer in the posterior cranial fossa
The fossa of the skull contains the cerebellum, IV ventricle, cerebellopontine angle and brain stem. Tumors in these areas include mainly glioma, astrocytoma and cystic angioreticuloma. Meduloblastoma is often diagnosed in children. Glioblastoma is less common, and oligodendrogliomas are very rare.
Cerebellum
Tumors that grow deep in the brain from cerebellar cells are called intracerebral. Extracerebral are formations that develop from the meninges, blood vessels and nerve roots of the skull. In adults, benign astrocytoma and angioreticuloma are more often observed; in children, the lesion can be malignant or benign.
When the cerebrospinal fluid pathways are compressed by cancer and internal hydrocephalus develops, their manifestation is noted:
- paroxysmal headache occurs with vomiting at its peak, with remissions and exacerbations;
- the posture of the head and torso is disrupted when occlusion occurs. Namely: patients are forced to tilt their heads to the side or forward, kneel and elbows, sharply tilt their heads down or lie face down (with an oncological process in the median aperture of the IV ventricle and the tumor mass grows into the cerebellar cistern);
- Pain occurs in the cervical and occipital areas, radiating to the arms, and the head is thrown back.
Cerebellar vermis
If the cerebellar vermis is affected, symptoms appear as:
- static ataxia;
- gait changes;
- muscle hypotension;
- weakening knee and heel reflexes;
- manifestations of areflexia.
IV ventricle
The bottom, roof, lateral recesses of the fourth ventricle and the plexus of vessels contain ependyma, from the cells of which glioma begins to slowly grow. The first symptoms to be detected are in the nuclear formations of the rhomboid fossa. Isolated vomiting is noted, accompanied by visceral crises, dizziness, headaches in the cervical and occipital sectors.
With the appearance of hiccups, attacks of pain in the skull and vomiting, and a forced position of the head, statics and gait begin to be disturbed.
The disease is complicated by:
- nystagmus, diplopia, decrease or loss of auditory reflexes on both sides;
- the appearance of paresis or paralysis of gaze;
- lack of sensitivity of facial organs;
- increasing bulbar disorders;
- violation of conductive, motor and sensory functions;
- unstable pathoreflexes;
- increased intracranial pressure, congestive discs in the optic nerves.
Floor of the fourth ventricle
At the bottom of the fourth ventricle and its components, the impact of the oncological process causes manifestations of horizontal and, less often, vertical nystagmus. The trigeminal, abducens and, less commonly, facial cranial nerves are affected. In the upper part of the worm, static ataxia and vestibular disorders are noted: vestibular and cochlear; patients often feel dizzy and have impaired gait.
When the aqueduct and midbrain are pinched, there is a violation of the oculomotor innervation, an increase in paresis of the upper gaze, to the side, and the reaction of the pupil to light decreases, or symptoms of aflexia appear: one or more reflexes disappear. Intentional hand trembling will be combined with impaired coordination of movements.
Herniation occurs with an increase in tumor formation and an increase in hypertension inside the skull due to the gradual lowering of the cerebellar tonsils into the occipital foramen, compression and deformation of the medulla oblongata due to a change in the position of the head and body.
Cerebellar hemispheres
In the cerebellar hemispheres, the development of slowly growing cyst-forming benign gliomas with occlusive-hypertensive symptoms more often occurs: increasing headaches with vomiting. Next, focal symptoms appear on the affected side: unilateral ataxia, impaired muscle hypotonia and motor coordination. The corneal reflex is suppressed or lost, the apples of the eyes move rhythmically with horizontal nystagmus. There is a gradual involvement of the VI, VII, VIII, IX and X cranial nerves in the oncological process, then pyramidal insufficiency begins.
If the tumor compresses the opposite hemisphere of the cerebellum, then symptoms will appear on both sides.
They appear on the side of the tumor:
- forced position of the head and the patient in bed;
- painful attacks of the head with vomiting and dizziness when changing position;
- redness of the face, pathological tendon reflexes;
- breathing and pulse disturbances;
- cerebellar monoparesis or hemiparesis accompanied by tendon pathoreflexes;
- in the later stages: lethargy, lethargy, stunning due to hypertension inside the skull.
Read here: The process of adenocarcinoma
Cerebellopontine angle
In the cerebellopontine angle, neuroma of the VIII vestibulocochlear nerve can develop from epineurium cells. More often it is located in the internal auditory canal of the temple, less often along the canal, forming the cerebellopontine angle. The consistency of the neuroma is denser than the brain substance. Therefore, the tumor capsule does not grow in, but compresses it.
In the first stages, hearing gradually decreases on the part of the tumor. Since it is compensated by the healthy ear, deafness is discovered late, with the appearance of vestibular disorders, spontaneous horizontal nystagmus when looking on both sides, more in the direction opposite to the tumor.
From the side of the neuroma, taste may be lost on the first half of the tongue (from the tip) if the intermediate nerve in the area of the internal auditory tract is damaged. Tumor formation compresses the trigeminal nerve, which early leads to a decrease in the sensitivity of the nasal mucosa and the corneal reflex on the tumor side. There may be minor damage to the facial nerve.
If the neuroma is located along the auditory canal, then the facial nerve is severely affected by strong compression with the intermediate nerve. As a neuroma grows on its side, brainstem and cerebellar signs of damage to the III, VI, IX, X, XII cranial nerves, liquorodynamic disturbances, congestive optic discs, cerebellar hemitaxy accompanied by headache appear.
With a neuroma of the vestibulocochlear nerve, the pyramid of the temple bone changes: the auditory canal inside the organ expands, the apex of the pyramid disappears (self-amputates), which can be seen on an x-ray.
Brain stem
The brain stem includes the pons, midbrain, and medulla oblongata, where cerebral gliomas often arise. In this case, alternating syndromes develop: on the part of cancer formation, one or more cranial nerves cease to function. On the healthy side, motor function is impaired, sensitivity is upset or lost. As the oncological process spreads, the nerve nuclei of the skull are damaged. In the later stages, intracranial hypertension develops. The tumor is difficult to remove, so the prognosis is poor.
Causes
The causes of tumor formation are not well understood. The disease is associated with a mutation of glial cells. The likelihood of getting sick increases in people with a genetic predisposition, living in unfavorable environmental conditions, and having been exposed to radiation (ionizing radiation).
The risk of developing a malignant neoplasm increases in children and adults with diagnosed neurofibromatosis, diagnosed Hippel-Lindau syndrome, Li-Fraumeni syndrome or tuberous sclerosis. A prerequisite for the growth of degenerated cells is radiation therapy, which was carried out in the treatment of leukemia, retinoblastoma and other forms of cancer.
Concept
Glioma is diagnosed in 60 patients out of a hundred who have various tumors in the brain. This tumor got its name due to the fact that it begins to grow from glial cells.
Glia are one of the structures of the nervous system, in the formation of which cells of different shapes take part. Glial cells fill the spaces between capillaries and neurons, and during normal brain development they constitute 10% of its volume.
With age, there is a decrease in neurons and an increase in glia volume. Glial cells surround nerve trunks, perform a protective function and help in transmitting impulses.
Glioma usually looks like a node with unclear boundaries, its color is pink, grayish, and in rare cases dark red. The shape of the tumor is spindle-shaped, round, the size is from 2 mm, in some people tumors are detected reaching the size of a large apple.
Glioma is characterized by infiltrative growth, which does not allow one to clearly establish the boundary between pathological and healthy tissues.
The symptoms of developing gliomas are similar to neurological diseases and it is often because of this that incorrect treatment is carried out in the initial stages. A neoplasm that affects glial cells is detected in people of different ages. Still, gliomas are most often found in young people and children.
Diagnostics
When making a diagnosis, the neurologist conducts neurological tests, studies the medical history, and prescribes additional instrumental examination. Diagnostics is performed using the following methods:
- MRI and CT of brain structures.
- Biopsy is a sample of tumor tissue.
- Echoencephalography, electroencephalography, vascular angiography, ophthalmoscopy, lumbar puncture are auxiliary diagnostic methods that provide additional information and allow us to clarify the details of damage to brain structures.
Positron emission tomography helps determine the degree of aggressiveness and rate of tumor growth. Neoplasms detected at an early stage are easier to treat.
How are glial tumors classified?
The disease is divided into 9 categories:
- Astrocytic tumor is divided into ordinary, pilocytic and anaplastic astrocytoma, among them there is glioblastoma and pleomorphic xanthoastrocytoma.
- Oligodendroglial tumor is also considered.
- The next one will be the ependymal one.
- Then choroid plexus disease.
- Mixed glioma is also noted.
- Neuroepithelial dysembryoplastic tumor.
- Neuronal, as well as mixed neuronal-glial disease.
- Parenchymal inflammation involving the pineal gland.
- Embryonic type of neoplasm.
Astrocytic tumors have aggressive growth; in this way they are usually divided into slow-growing and fast-growing. These neoplasms are divided into 4 degrees according to the histological gradation of malignancy. The classification of the disease is based on determining the degree of cellularity in cellular or nuclear polyphorism, as well as in endothelial proliferation with the participation of mitoses and necrosis.
Treatment
To cure the disease, it is important to detect the onset of pathological processes at an early stage. Treatment options for gliomas that form in the brain include:
- Chemotherapy. Taking antitumor medications.
- Radiation therapy. Treatment with ionizing radiation.
- Surgical intervention is surgical removal of the tumor.
- Stereotactic radiosurgery is a single exposure to a dose of radiation directly to the lesion.
The prognosis is conditionally favorable. Correct treatment of diagnosed grade 1 glioma increases the patient's life expectancy by an average of several years. Typically, the life expectancy of patients with highly malignant glioma formed in the brain does not exceed 2 years (25% of cases).
The meaning of glioma
The most common brain tumors are gliomas. They begin to appear due to defective neurogliocytes. They develop genetic abnormalities that lead to further impairment of function and growth. Usually such cells are called immature. When they settle in one place, a tumor appears.
Gliomas account for 60% number of tumors of the central nervous system. This disease is commonly referred to as uncontrolled and unexplained growth that alters the development and normal functioning of brain cells.
Glioma and its classification
Glioma (neuroglioma) is a voluminous extracerebral formation that externally looks like a pinkish, grayish-white (sometimes dark red) nodule with unclear outlines. A glial tumor can be located in the wall of the brain ventricle and in the chiasm zone (chiasm glioma). Sometimes a tumor can be found in the nerve trunks; rarely, but it happens, glioma grows into the meninges or cranial bones.
The shape of the glial tumor is round or spindle-shaped, size from 2-3 mm to the size of a large apple. Typically, this type of cancer develops slowly and does not have a tendency to metastasize. But glioma is characterized by high infiltrative growth, which means that the border between healthy tissue and tumor tissue is difficult to discern even under a microscope. This type of tumor is also accompanied by degeneration of surrounding nerve tissue.
There are three main types of glial cells:
- Astrocytes;
- Oligodendrogliocytes;
- Ependymocytes.
Depending on the type from which the tumor begins to develop, its types are distinguished:
- Astrocytoma;
- Oligodendroglioma;
- Ependymoma.
The most common type of cancer diagnosed is astrocytoma; it occurs in almost half of patients diagnosed with glioma. Oligodendroglioma is detected in 8-10% of patients, and ependymoma – in 5-8%. There are also mixed brain gliomas - choroid plexus tumors and neuroepithelial tumors of unknown origin (oligoastrocytomas and astroblastomas, gliosarcoma).
Important! Many readers recommend!
Monastic gathering of Father George. Which contains 16 herbs, it is an effective remedy for the treatment and prevention of various diseases. Helps strengthen and restore immunity, remove toxins and have many other beneficial properties
Doctors' opinion..."
According to the WHO classification, there are 4 degrees of malignancy:
- Grade I is a slowly growing benign glioma, these include: giant cell astrocytoma, juvenile astrocytoma, pleomorphic xanthoastrocytoma, angiocentric glioma;
- Grade II is considered a borderline type, since although a glioma of this grade is characterized by slow growth and has only one sign of malignancy (usually cellular atypia), it can degenerate into a glioma of III or IV degrees of malignancy;
- Grade III is characterized by the presence of 2 out of three signs: mitotic figures, endothelial microproliferation or nuclear atypia. These include: anaplastic glioma;
- Grade IV is characterized by the presence of an area of necrosis (multimorphic glioblastoma).
There is also a tumor classification based on location. They are:
- Supratentorial (located above the cerebellum). They are located in the cerebral hemispheres, where there is no possibility for the outflow of cerebrospinal fluid and venous blood;
- Subtentorial (below the cerebellum). They are located in the posterior cranial fossa.
Predisposing factors
The occurrence of a malignant tumor is always the result of a mutation of cells that acquire the ability to grow uncontrollably and destroy neighboring tissues. 5–10% of such disorders are inherited, most often in combination with other changes. These are the so-called pathological tumor syndromes. For example, with Lie-Fraumel disease, a combination of astrocytoma with breast cancer, bone and soft tissue sarcomas, and leukemia is inherited. In neurophyromatosis type 1, optic nerve gliomas are combined with pheochromocytoma (adrenal neoplasm), neurofibromas (benign tumors from nerve fiber sheaths) and hamartroma (tissue developmental abnormality) of the retina.