Feel
The 12th week of pregnancy has already arrived, which means that from this moment on, the future mother, if she suffered from toxicosis, will most likely begin to feel better. Yes, yes, the placenta is slowly taking over life-supporting functions, the corpus luteum has “done” its work, and therefore, nausea and vomiting will most likely now be a thing of the past. But, unfortunately, this applies more to “traditional” pregnancy, but if the pregnancy is designated as multiple, the symptoms of toxicosis may remain with it for some time. As well as emotional outbursts, irritability and nervousness caused by hormonal changes in the body.
Even if a woman, due to toxicosis, has lost a little weight in the first weeks of pregnancy, starting from the 12th week, her body weight will begin to increase: plus 500 grams weekly is considered the norm. The new life growing in the womb of a woman requires “the maximum” from the mother’s body, and therefore all its systems and organs work at full capacity. Blood volume increases, its circulation increases, the lungs and kidneys work more actively, the heart beats faster. At the same time, urination is “adjusted” - the frequent urge to go to the toilet “little by little” will no longer bother the woman, as at the beginning of pregnancy. But there may be a problem with bowel movement: the growing uterus puts pressure on it, bowel function slows down, which can lead to constipation.
Stomach
At the 12th week of pregnancy, the expectant mother can already feel how her belly is slowly beginning to enlarge. Usually, if pregnancy is new for a woman, then the belly begins to grow later; at week 12 it has practically not increased, the expectant mother feels comfortable and ordinary clothes still fit her. If this is not the woman’s first pregnancy, then the belly usually begins to enlarge earlier, often forcing the expectant mother to start looking for looser-fitting clothes already at 12 weeks. Often, the growth of the abdomen is accompanied by itching; this is a kind of “hint” for a woman to worry about choosing suitable products that will help avoid the formation of stretch marks, not only on the stomach, but also on the chest and hips. In addition, on the stomach, at the 12th week of pregnancy, it can be indicated by pigment spots and a dark stripe, which, starting from the navel, goes down. Experts reassure: there is nothing wrong with this, these phenomena are temporary and are not a cause for concern.
Uterus at 12 weeks of pregnancy
It is probably not difficult to guess that the belly begins to grow precisely in connection with the gradual increase in the size of the uterus. Thus, the uterus at 12 weeks of pregnancy usually increases to such a size that it simply becomes cramped in the hip area. At this stage, the width of the uterus “grows” to about 10 centimeters, therefore, it goes beyond its usual location and rises into the abdominal cavity. A woman can even fully feel and palpate its increased size.
Why is ultrasound screening performed at 12 weeks of pregnancy?
An important period in the life of every expectant mother is 12 weeks of pregnancy - ultrasound screening for the first time, as a rule, is carried out during this period. First of all, the study is carried out to identify possible deviations, both in the development of the baby and in the health of the pregnant woman. Many people hope to find out the gender of the baby. And, although by this time he had already developed primary sexual characteristics, they are still so small that it is extremely difficult to see them on a sonogram.
An ultrasound examination at 12 weeks of pregnancy is carried out to determine the number of fetuses, the volume of amniotic fluid, the size and shape of the uterus, and the position of the placenta. At this stage, the main parameters are also measured, giving an idea of the development of the future baby. Based on these data, the doctor can make a conclusion as to whether there is a risk of having a child with serious defects. Depending on this, additional examinations may be prescribed.
Ultrasound is usually performed transabdominally. Simply put, through the skin of the abdomen. A special gel is applied to it, allowing you to see the clearest picture possible, and then an ultrasonic sensor is passed over it. All information is displayed on the monitor. The procedure is absolutely painless and does not cause discomfort for either the expectant mother or the baby.
Sometimes more detailed research is required. In this case, a transvaginal ultrasound is performed, when the sensor is inserted into the vagina. This allows you to accurately assess the size of the fetal collar area (deviations from the norm clearly indicate the risk of developing Down's disease), diagnose sexual diseases in a woman, and find out other specific points.
When the pregnancy period is 12 weeks, ultrasound screening allows future parents not only to learn about the health of the fetus, but also to see it and hear the heartbeat.
This is what often helps them fully realize that they will soon have a baby. Ultrasound screening at 12 weeks: an important examination that helps to obtain information about the growth and development of the child
Ultrasound
Typically, at the 12th week of pregnancy, the first ultrasound examination occurs, with the help of which the doctor determines the size of the fetus and also establishes the estimated delivery date. An ultrasound at the 12th week of pregnancy becomes a real revelation for the expectant mother: her first acquaintance with the baby takes place, she already distinguishes him as a tiny person who is destined to be born in the near future. Although such indicators are extremely important in an ultrasound examination, ultrasound at 12 weeks of pregnancy can also show other, much more important results.
Thus, during an ultrasound examination, the doctor assesses the condition of the uterus and determines its tone, analyzes the location of the placenta, eliminates the possibility of ectopic pregnancy and clearly establishes how many fetuses develop in the womb. A woman can already observe her unborn baby on an ultrasound monitor, but without the help and explanation of a doctor she will not always be able to make out where everything is and how the baby is feeling now. Don’t be shy about asking the doctor for clarification - he can answer all the mother’s questions, thereby introducing her closer to her baby.
The doctor compares the ultrasound results at the 12th week of pregnancy with the indicators indicated in the table of normal values. This will make it possible to determine whether everything is going “as usual”, and in the future the indicators of the first ultrasound examination will be compared with the indicators of repeated ultrasound examinations. Thus, the specialist will be able to monitor whether the pregnancy is progressing normally and whether there are any abnormalities.
It happens that early diagnosis becomes a disappointing “surprise” for parents: an ultrasound at 12 weeks of pregnancy can already give an answer as to whether the baby is at risk of congenital defects or chromosomal abnormalities. Unfortunately, such diseases cannot be treated, and parents, learning about the abnormalities, are tormented by a difficult choice: keep the baby or still resort to termination of pregnancy.
Biochemical screening of the first trimester of pregnancy
This stage of the study must be carried out after an ultrasound scan. This is an important condition, because all biochemical indicators depend on the duration of pregnancy, down to the day. Every day the norms of indicators change. And ultrasound allows you to determine the gestational age with the accuracy that is necessary for conducting a correct study. At the time of donating blood, you should already have ultrasound results with the indicated gestational age based on CTE. Also, an ultrasound may reveal a frozen pregnancy or a regressing pregnancy, in which case further examination does not make sense.
Preparing for the study
Blood is drawn on an empty stomach! It is not advisable to even drink water in the morning of this day. If the test is carried out too late, you are allowed to drink some water. It is better to take food with you and have a snack immediately after blood sampling rather than violate this condition.
2 days before the scheduled day of the study, you should exclude from your diet all foods that are strong allergens, even if you have never been allergic to them - these are chocolate, nuts, seafood, as well as very fatty foods and smoked foods.
Otherwise, the risk of obtaining unreliable results increases significantly.
Let's consider what deviations from normal levels of β-hCG and PAPP-A may indicate.
Screening at 12 weeks of pregnancy
An even more informative method for assessing fetal development and the course of pregnancy according to the norm can be screening at the 12th week of pregnancy. This is a comprehensive study that covers not only ultrasound, but also a biochemical blood test. A blood test involves measuring two markers in a woman’s body – free b-hCG (free beta subunit of human chorionic gonadotropin) and PAPP-A (pregnancy-associated plasma protein A). In this regard, the first screening is also called a double test.
Optimally, screening is carried out three times throughout pregnancy, and the first is recommended to be carried out just between 11 and 13 weeks. The fact is that screening at the 12th week of pregnancy, which necessarily includes an ultrasound of the fetus, is aimed at studying the so-called “collar zone” of the fetus. Such a study makes it possible to exclude gross malformations of the fetus and even anomalies that are incompatible with life. The collar zone, the area of the neck between the skin and soft tissues where fluid accumulates, is a non-permanent marker. As the baby develops, the norms of the collar space change, and therefore its examination must be carried out strictly within certain periods. And, in addition, an analysis of the state of the collar zone can be carried out provided that the operator is highly qualified and specially trained, otherwise the presumptive diagnosis can be strongly doubted.
In turn, a study of hormone levels (free b-hCG and PAPP-A) carried out as part of screening at the 12th week of pregnancy makes it possible to determine the degree of risk of developing certain abnormalities in the fetus. For example, an increase in the values of free b-hCG on average by half may be a reason for suspicion of the presence of trisomy 21 (Down syndrome) in the fetus, a decrease - trisomy 18 (Edwards syndrome).
However, despite the high information content, screening at the 12th week of pregnancy is by no means a reason for a final analysis. This study only establishes the degree of risk and the possibility of having trisomy 21, trisomy 18, as well as a neural tube defect. Screening results become the basis for further research using special methods. Among other things, if the tests are questionable, the doctor usually refers the expectant mother to a geneticist, who, in turn, recommends other additional studies.
Learn more about diagnosing Down syndrome
Mainly, an ultrasound examination at 11-13 weeks of pregnancy is performed to identify Down syndrome. The main indicator for diagnosis becomes:
- Neck space thickness (TNT). TVP is the distance between the soft tissues of the neck and the skin. An increase in the thickness of the nuchal translucency may indicate not only an increased risk of having a child with Down syndrome, but also that other genetic pathologies in the fetus are possible.
- In children with Down syndrome, most often the nasal bone is not visualized at 11-14 weeks. The contours of the face are smoothed.
Before 11 weeks of pregnancy, the thickness of the nuchal translucency is so small that it is impossible to adequately and reliably assess it. After the 14th week, the fetus develops a lymphatic system and this space can normally be filled with lymph, so the measurement is also not reliable. The incidence of chromosomal abnormalities in the fetus depending on the thickness of the nuchal translucency.
| TVP, mm | Frequency of anomalies, % | Increased TVP | Normal TVP |
| 3 | 7 | ||
| 4 | 27 | ||
| 5 | 53 | ||
| 6 | 49 | ||
| 7 | 83 | ||
| 8 | 70 | ||
| 9 | 78 |
When deciphering the screening data of the 1st trimester, it should be remembered that the thickness of the nuchal translucency alone is not a guide to action and does not indicate a 100% probability of the presence of the disease in the child.
Therefore, the next stage of screening of the 1st trimester is carried out - taking blood to determine the level of β-hCG and PAPP-A. Based on the obtained indicators, the risk of having a chromosomal pathology is calculated. If the risk based on the results of these studies is high, then amniocentesis is suggested. This is taking amniotic fluid for a more accurate diagnosis.
In particularly difficult cases, cordocentesis may be required - taking cord blood for analysis. Chorionic villus sampling may also be used. All of these methods are invasive and carry risks for the mother and fetus. Therefore, the decision to perform them is decided by the woman and her doctor jointly, taking into account all the risks of carrying out and refusing the procedure.
Analyzes
In addition to an ultrasound examination and a biochemical blood test, the doctor may prescribe some other tests for the expectant mother at the 12th week of pregnancy. Usually, a woman has to undergo all scheduled tests when registering at the antenatal clinic. But it happens that tests at the 12th week of pregnancy may be needed due to a woman’s late visit to the gynecologist about pregnancy. Or it happens that tests at the 12th week of pregnancy are needed for an extended examination of the expectant mother in connection with her condition - as an additional control tool.
In addition to the traditional blood test for AIDS, syphilis, hepatitis B, blood type and Rh factor, by this time a blood test for sugar, as well as a biochemical analysis, should already be taken. Among other things, an analysis at the 12th week of pregnancy, examining “biochemistry”, will determine the level of hCG in the body of the expectant mother. And a biochemical blood test is carried out, as mentioned above, as part of a screening examination of the pregnant woman. If there are any suspicions of specific diseases, the woman may also be sent for hormone tests and tests for urogenital infections.
Conducting a second screening
The second examination is usually done at 20-24 weeks of pregnancy. At this stage of pregnancy, ultrasound and blood biochemistry are performed. Only at this stage the blood is tested not for two, but for three hormones (hCG, estriol norm, ACE). A high level of hCG indicates that the timing was set incorrectly, or that there are several fetuses in the uterus. If hCG is higher than normal, this may indicate the development of pathologies in the unborn baby. An elevated ACE means that the fetus has developed cirrhosis of the liver. Also, a high ACE rate may indicate the following facts:
- development of two or more fruits;
- neural tube problems;
- kidneys do not develop properly;
- an umbilical hernia has developed;
- nonunion of the abdominal wall;
- other pathological processes in development.
When ACE is below normal, this indicates a delay in the baby's development, fetal death, and the risks of Down and Edwards syndromes. A low ACE level may indicate an error in setting the gestational age. For the safe bearing of a child, normal levels of the hormone estriol play an important role. A low level of this hormone indicates a threat of miscarriage or pathological disorders in the fetus. The level may decrease if the pregnant woman has liver or kidney disease, or if the woman takes hormones.
The second screening is also called the triple test. It is better to take a triple test on the same day - this guarantees a more accurate result.
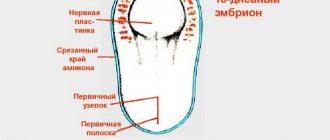
Fetus at 12 weeks of gestation
All these actions are necessary both to monitor the condition of the expectant mother and to carefully monitor the formation and normal development of the fetus at 12 weeks of pregnancy. At this stage, it has already grown significantly: the fetus is at the 12th week of pregnancy, 10 weeks old, weighs about 14 g, and reaches a length of 6 to 9 cm (from the crown to the tailbone). From this moment on, by the way, his growth rate and length are a much more important indicator for doctors than his weight.
The fetus at the 12th week of pregnancy is already practically formed, all its systems and organs are actively working and continue to develop. So, the fingers are divided and marigolds form on them, a unique imprint is formed on the pads of the fingers, the top layer of skin is renewed, and where eyebrows and eyelashes will appear in the future, fluff appears. Vellus hairs also appear on both the chin and upper lip.
By the way, the fetus at the 12th week of pregnancy already actively “expresses emotions” with its face: it grimaces, opens and closes its mouth, and even puts a finger in its mouth. At the same time, the baby waves its arms and legs, and also tumbles and “swims” freely in the mother’s womb.
At this stage, the baby’s internal organs, in parallel with the fact that they are functioning, still continue to develop. The baby’s intestines, having “taken” their place, periodically contract, the liver synthesizes bile, and the pituitary gland and thyroid gland produce hormones and iodine. Bone tissue continues to mature, the baby’s muscles become stronger, the heart beats quickly, the kidneys and nervous system work fully. And at this stage, in addition to red blood cells, leukocytes also begin to form in the fetal blood - the immune system is increasingly improved.
12 week pregnancy video
12 week pregnancy photo
Ultrasound screening standards at 12 weeks
Fetal condition
An ultrasound scan gives a clear picture of how many fetuses are in the womb. On the monitor you can see exactly how they are located. Depending on this, the doctor makes a note about the characteristics of the presentation. It indicates which part is closest to the birth canal - the baby’s head, legs or pelvis. At this stage, this indicator is not particularly important, because the baby now has enough space to turn freely in the womb. Closer to the 32nd week, if the presentation is incorrect, the doctor should already take appropriate measures.
The main component of the first ultrasound examination during pregnancy is fetometry - the measurement of indicators that are especially important for the 12-week period. These include:
- BPR is the size of the fetal head between the parietal bones. Normally, this figure is about 21 mm.
- DlB or DB – thigh length. Should be from 7 to 9 mm.
- DHA – chest diameter. On average, it is 24 mm at this time.
- KTR is the size from the crown to the tailbone. At 12 weeks, the average is 51 mm. However, quite strong fluctuations are allowed here. With other normal indicators, a size in the range from 43 to 59 mm will not be a deviation.
- Thickness of the collar area. This parameter is important for determining the risk of developing Down syndrome. Normal values vary from 0.71 to 2.5 mm. The critical size is 2.7 mm.
- The overall height of the unborn baby at this stage should be approximately 8 - 8.5 mm.
- Weight – indicators ranging from 17 to 19 g will be considered normal.
At this stage - 12 weeks of pregnancy - ultrasound screening may include some other studies. Thus, head and abdominal circumference, heart size, and shoulder length are often measured. Only by comparing all the indicators together can the doctor judge the presence of certain abnormalities.
Condition of the uterus
At this stage of pregnancy, the length of the cervix is measured during an ultrasound examination. Normally it should be about 30 mm. The critical threshold is 20 mm. In this case, the woman is prescribed bed rest or hospitalization, sometimes requiring surgical intervention.
At 12 weeks, an ultrasound screening necessarily evaluates the condition of the uterine muscles. If the doctor says o, then there is a risk of miscarriage. To reduce the risk, special treatment is prescribed - outpatient or inpatient.
Placenta
An ultrasound examination can also assess the condition of the placenta. Ideally, it should be attached to the anterior or posterior wall of the uterus and located far enough from the os of the uterus (at least 70 mm). Otherwise, treatment is prescribed. Most often, the situation returns to normal closer to childbirth.
Amniotic fluid
Ultrasound shows the amount and condition of amniotic fluid. If in conclusion the doctor diagnoses “polyhydramnios” or “oligohydramnios”, this means that there is too much fluid in the first case, or not enough in the second. Both may indicate infection, central nervous system disease, or kidney problems. Cloudiness of the amniotic fluid is also considered a deviation - most often, this indicates a particular disease, so additional examination is required.
Ultrasound at 12 weeks of pregnancy allows you to identify various diseases and problems in the development of the fetus in the early stages. This gives every opportunity to take timely measures. It is during this period of time that the doctor, based on ultrasound data, can name the expected date of birth most accurately. The procedure does not cause any discomfort and is considered safe for the expectant mother and her baby. However, disputes often arise in the medical community regarding the effect of ultrasound on the fetus. Some experts consider this exposure potentially dangerous. Therefore, ultrasound should be resorted to only if there are compelling reasons for this.
Pain
All this “magic” that happens in mom’s tummy should not normally be accompanied by painful sensations. True, mild and mild pain in the 12th week of pregnancy, felt in the lower abdomen, can be explained by the tension of the ligaments that support the growing uterus. At the same time, doctors often justify lower back pain by a change in the center of gravity due to a gradually growing abdomen, and also by a softening of the supporting ligaments and discs under the influence of progesterone.
At the same time, lower back pain can also be caused by a bladder infection, so in such a situation it is still better to consult a doctor and, if necessary, undergo an examination. It would also be useful to consult a specialist if pain in the lower abdomen appears periodically during the 12th week of pregnancy, is aching and pulling, and also if pain in the lower abdomen lasts for 2-3 hours. And, moreover, they are accompanied by bloody discharge - this dangerous sign indicates the threat of premature termination of pregnancy. If a woman reacts in time when painful sensations appear, a miscarriage can be avoided, so it is necessary to seek help immediately.
Discharge
Bloody discharge at the 12th week of pregnancy, even minor, should always alert a woman. Moreover, if they are also accompanied by abdominal pain - all this indicates the risk of spontaneous abortion. But spotting that appears after a gynecological examination or sexual intercourse can be explained by erosion of the cervix. And this condition is also a sufficient reason to contact a specialist and undergo additional examination.
Normally, discharge at the 12th week of pregnancy is moderate, light or with a milky tint, uniform consistency and a slight sour odor. There should be no pus, mucus, green or yellow, cheesy discharge or discharge with a strong and unpleasant odor: such discharge becomes a sign of infection. A change in the consistency and color of the discharge may be a symptom of thrush, chlamydia, or trichomoniasis, which require mandatory treatment, because the infection is quite capable of affecting the fetus.
Bleeding
Bleeding at the 12th week of pregnancy always requires consultation with a doctor, because it is always defined as a very dangerous sign. Although bleeding of various types is considered a fairly common occurrence in the early stages of pregnancy, you should never take risks and let the situation take its course - in order to prevent a possible miscarriage, the harbinger of which is bleeding at the 12th week of pregnancy.
Bleeding, which is accompanied by cramping or nagging pain in the lower abdomen and painful sensations in the lower back, is especially dangerous. Indeed, in addition to the threat of spontaneous abortion, such bleeding may also indicate an ectopic pregnancy - a complex and pathological pregnancy that poses a threat to the health and life of a woman.
Purpose of the survey
The first trimester of pregnancy is coming to an end, when the embryo is most vulnerable to various adverse factors. By this time, the mother’s body should already have time to form a placenta instead of the corpus luteum, which was needed in the early stages. If everything is going correctly at the moment, the presence of serious pathologies can be ruled out. At the same time, the fetus is already large enough for it to be possible to notice any problems upon examination.
In order to be fully prepared by the time of birth and avoid complications of pregnancy in the second and third trimester, you need to identify weaknesses, if any, now. Therefore, the first screening is carried out. The next one will be carried out at 16–20 weeks, depending on the results of the first examination.
Cold at 12 weeks of pregnancy
The twelfth week ends one of the critical periods of pregnancy - the first trimester, after which the baby will no longer be afraid of most anomalies and malformations. But for now, in this last and important week of the first trimester, you still need to take care, including colds.
A cold in the early stages can cause a lot of trouble: provoke the development of placental insufficiency, fetal hypoxia, and significantly increase the risk of miscarriage. After all, if suffered on the feet and “untreated,” a cold at the 12th week of pregnancy still remains a significant danger: it can cause malformations of the baby, even incompatible with life, which can ultimately result in spontaneous abortion.
The situation is significantly complicated by the fact that colds in the early stages of pregnancy cannot be treated with medications to avoid negative consequences. In this case, only traditional medicine and some herbal remedies are suitable - and then only after consultation with a doctor.
Rest and bed rest are mandatory for a woman during the treatment of a cold. Drinking plenty of fluids (warm, but not hot) is recommended - herbal teas, rosehip decoction, berry fruit drinks made from lingonberries, raspberries, and currants. Honey is also useful - albeit in small quantities, since it has a strong allergenic effect. Honey can be added to tea or drunk with warm milk. Warm milk mixed with Borjomi mineral water is also considered a good remedy for treating colds, primarily against coughs. You can also fight a cough with the help of marshmallow mixture, syrup or Doctor MOM lozenges, Gedelix.
It is imperative to consult a doctor again if a cold at the 12th week of pregnancy does not go away within 3-4 days, if its symptoms intensify, headaches are observed against the background of the cold, and a cough accompanied by wheezing does not go away. Moreover, mandatory consultation with a specialist is required if a cold at the 12th week of pregnancy is accompanied by a high temperature - 38 degrees or more.
Temperature
The temperature at the 12th week of pregnancy, which is slightly above normal and fluctuates around 37-37.5 degrees, can be either a variant of the norm (this is how the body reacts to increased levels of progesterone in a woman’s body) or indicate hidden diseases. Tests will help identify these diseases - usually inflammatory ones provoke changes in the levels of leukocytes, as well as the erythrocyte sedimentation rate (ESR). And yet, more often than not, a slightly elevated temperature at the 12th week of pregnancy is a characteristic feature of the expectant mother’s body.
But a noticeable high temperature at the 12th week of pregnancy, accompanying any disease, poses a significant threat to the baby. Thus, under the influence of high temperatures, pregnancy loss can occur even at this stage, therefore a long-lasting high temperature is simply not acceptable. But most antipyretic drugs are prohibited at the 12th week of pregnancy (the only exception is paracetamol, and then only with the permission of a doctor). So what to do?
First of all, do not “disdain” folk methods of lowering the temperature - rubbing with cool water with the addition of a small amount of vinegar, wet and cool lotions on the ankles and hands, a cool shower. But all this is only after a doctor has been called to your home: he will help determine the degree of danger of high fever and prescribe a dosage in which paracetamol will not cause much harm.
Alcohol
You should also abstain from alcohol during the 12th week of pregnancy, as well as during the entire period of pregnancy. A conscientious mother is clearly interested in ensuring that her baby is born as a full-fledged and healthy baby, while alcohol at 12 weeks of pregnancy, consumed even in the smallest doses, can prevent this.
At this stage, the formation of the brain is still ongoing, and no specialist will take the responsibility to guess how alcohol will affect this process. Thus, alcohol can cause irreparable damage to brain cells, even destroying some of them, which will not recover in the future. The effects of alcohol can appear in this case even several years after the baby is born: at some point it will become clear that the child has difficulty learning, is overly excitable and hyperactive, and suffers from poor memory.
In a more severe case, alcohol at 12 weeks of pregnancy can still cause severe malformations of the child and physical deformities, affecting the formation of bone tissue and muscle development. Alcohol in large quantities, constantly penetrating the placenta to the baby and having a toxic effect on it, can even lead to miscarriage. Therefore, alcohol at 12 weeks of pregnancy should definitely be excluded from the life of the expectant mother.
Diagnostic result and its interpretation
Screening data is deciphered only by a doctor. Don't try to understand the metrics on your own. Misinterpretation of the results will only bring you anxiety. Statistics show that in 7 cases out of 10, the data obtained indicate the normal development of the child and the absence of defects and malformations.
The following indicators are considered a good result.
- The size of the fetus corresponds to the term or deviates from it by no more than 3 days. At 10 weeks, the length of the embryo from the crown to the sacrum ranges from 33 to 49 mm. At 11 weeks this figure is 42-58 mm. At week 12, CTE is 51-73 mm.
- The thickness of the collar space is 1.5-2.2 mm. This size is indicative for the period from 10 to 13 weeks. Deviations from established norms may indirectly indicate chromosomal abnormalities of the fetus.
- The size of the nasal bone is 3 mm or more at 12 weeks. If screening is done earlier, the nasal bone should be detected, but it is still very difficult to measure. The absence of this indicator most likely suggests the presence of Down syndrome in the child.
- The results of laboratory tests are also evaluated. The level of human chorionic gonadotropin stops increasing at this time. High values indicate pathologies of the placenta or possible Edwards syndrome. The later the screening is carried out, the lower the hCG level.
Sex at 12 weeks pregnant
But if a woman feels satisfactory and there are no contraindications for carnal pleasures, it is not at all necessary to refuse sex. Moreover, at the end of the first trimester of pregnancy, toxicosis and its accompanying symptoms slowly recede, the woman enters a certain period of “heyday” and the dangers that were characteristic in the early stages of pregnancy also gradually become a thing of the past.
The only contraindication to sex, both in the first weeks and in the 12th week of pregnancy, may be the threat of miscarriage. And then, in this case, restrictions on sex are usually imposed by doctors just before the 12th week. Other reasons that will be a reason for a woman to take care may be a multiple pregnancy and a low location of the placenta (this will be determined by a routine ultrasound). If pregnancy is not accompanied by such characteristic “features”, sex at 12 weeks can be safely practiced.
The only thing is not to be too active and not “overzealous”, avoiding the partner’s pressure on the stomach and monitoring internal sensations after sexual intercourse. For example, cramps that can appear after carnal pleasures are usually classified as normal. But, if cramps do not go away for some time after sex, and are also accompanied by bleeding, you should immediately call a doctor.
You should also, if possible, consult a doctor if you experience spotting after sex at 12 weeks of pregnancy, but it is not accompanied by pain. This sign may indicate that a pregnant woman has cervical erosion.
Nutrition
Nutrition at the 12th week of pregnancy must be complete and balanced: the baby’s rapidly developing body needs as much nutrients and nutrients as possible. They are found in required quantities in “healthy” foods: meat and fish, dairy and fermented milk products, cereals, vegetables and fruits. Moreover, the method of their preparation occupies an important place: it is better to boil or bake food when cooking (fried food causes heartburn), vegetables and fruits are eaten raw (fiber improves intestinal motility and reduces the likelihood of developing constipation).
A full breakfast is important; it is advisable to always eat a portion of the first meal as a starter, and dinner should be light. It is better to eat, again, more often, but in small portions, avoiding overeating. If some foods suddenly begin to cause aversion in a woman due to pregnancy, you can always find an “alternative” to them: for example, if you do not want and do not accept meat, you can completely replace it with fish. Don't like boiled fish? You can try baking it. Yes, and one more thing: there is no point in torturing yourself and trying to “squeeze” into the stomach a product that the expectant mother simply does not like at the moment, but which, according to all the characteristics, is extremely useful for pregnant women. For example, many women during pregnancy simply cannot look at cottage cheese, even though it seems to bring exceptional benefits to the body of mother and baby. But food eaten forcefully will definitely not be good for future use, so it’s still better not to go against your taste “senses”.