Urethritis, or inflammation of the urinary tract, is a fairly common disease in pregnant women. The following predisposing factors are identified that provoke the development of urethritis during pregnancy:
- Most often, the disease is provoked by a bacterial infection that enters a woman’s body during sexual intercourse. The main causative agents of infectious diseases are gonococci, chlamydia, microplasma, and ureaplasma infections. All of them can be transmitted during sexual intercourse before and during pregnancy, and appear after a certain time.
- Severe hypothermia is no less a private factor in the development of urethritis.
- Untreated infectious, inflammatory diseases of a hidden nature (for example, cystitis).
- Allergic reactions (most often to personal hygiene products, food).
- Congenital, acquired defects of the genitourinary system.
- Overwork due to excessive emotional and physical stress.
- Insufficient fluid intake.
- Failure to comply with basic hygiene rules.
- Too frequent consumption of spicy, smoked, salty foods, and sweet, highly carbonated drinks.
Types of urethritis
Medicine distinguishes 2 types of urethritis: infectious and non-infectious.
INFECTIOUS . Infectious urethritis is the occurrence of inflammatory processes that were caused by infection. The development of urethritis can be triggered by chlamydia, ureaplasma, gonococcus, etc. All these and many other bacteria are pathogens of infectious diseases that can live in a woman’s body before pregnancy, but their manifestation is possible only after conception against the background of a decrease in immunity characteristic of pregnancy.
NON-INFECTIOUS .
The occurrence of non-infectious urethritis is possible as a consequence of trauma or the development of allergies. Its appearance during pregnancy is associated with the presence of a growing fetus, which puts pressure on the urinary canal.
Diagnosis of the disease
On examination, redness of the external opening of the urethra and surrounding tissues is observed. When pressing on the urethra, the patient experiences pain. Purulent discharge may also be observed.
In order to confirm the diagnosis, the following tests must be performed:
- General blood analysis.
- General urine analysis.
- Urinalysis according to Nechiporenko to determine leukocytes and erythrocytes in the urine. This allows you to assess the condition of the urinary tract and kidneys.
- Bacteriological examination of urine, in some cases allowing to determine the causative agent of the disease.
- A smear from the urethra for analysis using the polymerase chain reaction method to identify the pathogen (this is the most accurate analysis to identify the pathogen).
- Swab for bacterial culture. Allows you to determine the sensitivity of pathogenic microorganisms to antibiotics.
Causes of urethritis during pregnancy
There is no particular predisposition of the body to the occurrence of urethritis, but external factors can have a sufficient influence on the occurrence of the disease. The causes of urethritis during pregnancy include:
- hypothermia;
- the presence of sexually transmitted diseases and sexually transmitted infections;
- errors in nutrition and diet. Salty, pickled, bitter, sour, spicy, alcoholic foods enter the bladder, and in case of excess of these products, irritation of the urethra is possible;
- decreased immunity;
- exposure to toxic and radiation factors;
- the presence of infections (chlamydia, ureaplasma, gonococcus, trichomonas, mycoplasma);
- performing medical interventions and procedures;
- presence of urolithiasis;
- the presence of gynecological diseases.
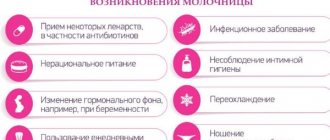
Causes of inflammation in pregnant women
Urethritis is divided into venereal (specific) and non-venereal (non-specific). In the first case, the infection enters the body of a pregnant woman through sexual contact. A specific form of the disease can be caused by:
- Neisseria gonorrhoeae (gonorrhea).
- Trichomonas vaginalis (trichomoniasis).
- Chlamydia trachomatis. (chdamidia).
- Human papillomavirus (human papilloma virus).
- Candida (fungi of the genus Candida).
With the development of a nonspecific form of the disease, the pathogen enters from the source of chronic inflammation, moving through the blood or lymph. The disease can be caused by:
- Streptococcus (streptococci).
- Escherichia coli (Escherichia coli).
Factors contributing to the development of urethritis
Non-infectious urethritis in pregnant women can be caused by the following reasons:
- Chronic constipation.
- Injuries to the genital organs.
- Active sexual relations.
- Allergic reaction.
- Metabolic disorders, resulting in an increase in the amount of phosphates or urates in the urine.
- Urolithiasis, in which the mucous membrane is damaged by passing stones.
- The appearance of tumors in the urethral area.
- Gynecological diseases.
Note! The appearance of urethritis in pregnant women can be facilitated by factors such as decreased immunity, chronic inflammation of the pelvic organs, hypothermia, drinking insufficient amounts of fluid or violations of personal hygiene rules.
Symptoms of urethritis during pregnancy
A woman's body has a shorter urethra, which contributes to weaker manifestations of urethritis compared to men. Sometimes urethritis may be asymptomatic or accompanied by minor signs, to which the woman often does not pay much attention. Typically, symptoms of urethritis during pregnancy are:
- the appearance of pain, itching, burning when urinating;
- the appearance of purulent discharge from the external urethra;
- the appearance of redness;
- manifestation of pain at rest in the presence of chronic urethritis.
Complications
Any infectious diseases of the genitourinary system and urethritis in particular can provoke serious health problems. Incorrect or untimely treatment can lead to complications such as:
- Prostatitis
- Balanoposthitis
- Pyelonephritis
- Vesiculitis
- Cystitis
- Inflammation of the testicle or foreskin
- Pelvic inflammatory disease
- Infertility
- Epididymitis
- Reactive arthritis
If the infection remains in the body for a long time, the urethra narrows, which threatens urinary retention, and, consequently, problems with the bladder and kidneys.
Why is urethritis dangerous during pregnancy?
Any infection that affects the female body can have a serious impact on the course of pregnancy and the development of the fetus. Why is urethritis dangerous during pregnancy? The degree of risk of developing fetal pathologies depends on the type of urethritis in the pregnant woman and the type of infection that caused the onset of urethritis.
A less dangerous disease is non-infectious urethritis during pregnancy, since there is no chance of infection of the fetus with dangerous microbes. But it is necessary not to ignore the treatment of the disease, since if advanced forms develop, there is a possibility that non-infectious urethritis will develop into other diseases of the genitourinary system, which are more serious.
The most dangerous is considered to be urethritis that occurs due to chlamydia or ureaplasmosis, since these infections have the ability to penetrate the amniotic fluid, through which the fetus can be infected. As a result, developmental pathologies may appear.
There is a high probability that the baby will be infected during childbirth as it moves through the birth canal. In case of such infection, the newborn may develop conjunctivitis, pneumonia, and gonococcal infection.
Caution: venereal urethritis!
You should be especially wary of gonococcal urethritis. Its causative agent is a dangerous pathogen that can reach the embryo and cause inflammation of the membranes, sepsis, intrauterine death or premature birth. Along with a direct threat to life, a newborn can become infected with gonococci during childbirth in the birth canal and acquire, among other things, gonococcal conjunctivitis, which can lead to blindness. It is worth noting that gonococci can be infected not only through sexual contact, but also indirectly through the use of hygiene items from sick people.
Urethritis can be caused by a wide variety of microorganisms, including opportunistic ones.
No less dangerous is urethritis in pregnant women, caused by chlamydia. Since the pathogen penetrates well into the amniotic fluid, it can cause infectious damage to the fetus and loss of pregnancy. In the first trimester of pregnancy, developmental arrest or miscarriage may occur due to placental insufficiency. At later stages, the risk of infectious damage to the fetal organs increases. Since chlamydial urethritis can occur without severe symptoms, the presence of this infection must be proactively excluded in every pregnant woman. This pathogen is a classic example of a disease that is sexually transmitted.
Opportunistic pathogens of urethritis include mycoplasma, which may not appear in a woman under normal conditions. But since pregnancy is a stress for the body, undermining its defenses, the pathogen can become active and provoke termination of pregnancy or its fading. For a child, this infection remains dangerous when passing through the birth canal, since the pathogen can be swallowed and cause inflammation of the nasopharynx and respiratory tract. Often after childbirth, mycoplasmosis causes complications in the woman in labor - inflammation of the endometrium - endometritis.
Treatment of urethritis with folk remedies in women
Urethritis caused by Trichomonas vaginalis is one of the most common species. It is almost always asymptomatic, which makes its diagnosis difficult and contributes to the chronicity of the process. A characteristic sign of Trichomonas urethritis is a strong burning sensation and a sensation of “pins and needles” in the urethra. Infection occurs through sexual contact. The waste products of these microorganisms are dangerous, as they are toxic to the host organism.
Toxoplasmosis urethritis is dangerous for the fetus due to the threat of termination of pregnancy at any stage, inflammation of the placenta or its insufficiency, intrauterine growth retardation, hypoxia, spastic syndrome, damage to the liver, lungs and brain. In addition, Toxoplasma creates favorable conditions for the penetration and reproduction of other pathogens. The body's susceptibility to viruses - herpes, HIV, human papillomavirus - especially increases.
Diagnosis of urethritis during pregnancy
Diagnosis of urethritis consists of several stages. First of all, when diagnosing urethritis during pregnancy, it is necessary to analyze the patient’s complaints: when did signs of the disease appear, what are their manifestations. The specialist can also find out the details of the patient’s life, the presence of chronic or prolonged inflammatory processes, the operations performed, and examine the patient.
- A specialist performs microscopy of a smear of secretions taken from the urethra to determine the presence of urethritis and its type.
- If urethritis becomes chronic, urethroscopy and urethrography are additionally performed.
- In addition, during the diagnosis of urethritis during pregnancy, a bacteriological culture of the smear is provided. This stage is carried out in order to determine the sensitivity of the causative agent of urethritis to antibiotics intended for use for treatment.
- To detect any changes in the structure of the organs of the genitourinary system, it is necessary to perform an ultrasound.
- The final stage of diagnosing urethritis during pregnancy is to conduct a PCR study aimed at identifying pathogens or infections that can be transmitted sexually.
Additionally, studies may be ordered to study the current condition of the child: whether urethritis had an impact on the development of the fetus, what is the likelihood of the disease affecting the child, etc. If urethritis is of infectious origin, then there is a possibility of a number of complications, which, first of all, affect the development of the fetus.
The harmful effects of urethritis can affect the condition of the child even after childbirth. Infection can be caused by pathologies in the development of vital organs and tissues of the fetus; in exceptional cases, urethritis can cause miscarriage.
Diagnostics
Diagnosis of urethritis is carried out using laboratory and instrumental research methods.
If this disease is suspected, the following is prescribed:
- a general urine test to detect bacteria, mucus and blood;
- a general clinical blood test, which evaluates hemoglobin, determines the level of red blood cells, leukocytes and platelets - these indicators may indicate the development of an active inflammatory process in the body;
- a microscopic smear from the urethra, which allows you to detect the causative agent of the disease that caused urethritis - this method is the most reliable;
- bacterial culture involves the study of biological material in order to determine pathogenic microflora and the degree of its sensitivity to antibiotics;
- ELISA and RIF - studies are carried out to identify antibodies of different classes produced by the human body as a response to infection;
- PRC diagnostics allows you to exclude sexually transmitted infections by detecting bacteria in a smear.
The final diagnosis is made by taking into account the patient’s complaints of poor health and problems with urination.
Treatment of urethritis during pregnancy
Depending on the nature of urethritis, treatment of the disease is prescribed. If it was caused by an infection, then the woman needs hospital treatment, which involves the use of the most conservative antibiotics so as not to harm the development and health of the fetus. In addition, it is planned to prescribe drugs that have a local effect and conduct a course of immunotherapy.
Treatment of non-infectious urethritis during pregnancy is carried out at home after doctor’s instructions. Prescribed medications should relieve inflammation and eliminate the cause of the disease.
For any type of urethritis during pregnancy, it is necessary to restore the properties of the walls of the urethra, restore the vaginal microflora and strengthen the protective functions of the immune system.
Complex actions, the purpose of which is to restore the properties of the walls of the urethra, are of particular importance in the case of diagnosing complex forms of the disease, when there is no direct connection between inflammation and infection.
Urethritis will recur until infection of the urethra by microorganisms penetrating from the vagina is stopped. This vicious circle can be broken thanks to the population of the vagina with microorganisms that should be there.
During long-term treatment and the presence of inflammation of the urethra, the immunity of the entire body and the wall of the urethra often suffers, so it is necessary to prescribe an individual course of restoration of the immune system.
BOUGIENATION OF THE URETHER CHANNEL . If the case of the disease is advanced, when the infection has been managed, but the symptoms have not gone away, it is necessary to perform bougienage of the urethra, in which the mucous membrane of the urethra is cauterized using a special chemical. This method is advisable due to the fact that in complex chronic forms of urethritis, the mucous part of the urethra changes. This phenomenon is irreversible. After cauterization, a scab appears, under which new healthy tissue begins to grow. All symptoms disappear 1-3 days after the procedure.
Symptoms of the disease
The main manifestations of symptoms of female urethritis are as follows:
- purulent, unpleasant-smelling discharge of a gray, green hue is released from the mucous membrane of the urethra, this is especially noticeable in the morning, during the first urination;
- redness, itching, swelling, sharp pain in the genital area;
- frequent urge to go to the toilet.
Prevention of urethritis
To prevent urethritis in women, it is necessary to protect the body from the effects of certain factors that can cause disruption of the vaginal microflora and decreased immunity. The main methods of preventing the development of urethritis include:
- avoiding severe hypothermia;
- responsible approach to hormonal changes;
- avoiding severe stress;
- protection from sexually transmitted infections;
- compliance with hygiene rules;
- maintaining regular sex life;
- avoiding the occurrence of chronic problems with stool (constipation, diarrhea);
- regular nutrition with the consumption of proper and healthy foods;
- regular visits to the gynecologist;
- ensuring adequate rest and sleep.
Infectious urethritis
Speaking about infectious causes of urethritis, the most often suspected are Escherichia coli, gonococci (the causative agents of gonorrhea) or chlamydia (the causative agents of chlamydia). You can find a special classification into venereal (gonorrheal, trichomonas, viral) and non-venereal (staphylococcal, streptococcal, colibacillary) urethritis.
Pathogens enter the urethra through the bloodstream or through the urinary tract. Streptococci and staphylococci often enter from the outside during vulvovaginitis, during various manipulations with insufficiently sterile instruments (catheterization, for example), and due to neglect of personal hygiene.
Due to the anatomical features of women, intestinal microflora easily penetrates the urethra and becomes a common cause of inflammation.
Escherichia coli belongs to the so-called facultative microorganisms that are constantly present in the human body. They live mainly in the large intestine, where their activity is balanced by other microorganisms. E. coli (Escherichia coli) becomes pathogenic when normal microflora is suppressed by antibiotics, with a general weakening of the immune system. From dirty laundry or improper washing, E. coli is transferred from the large intestine to the urethra. This is facilitated by the anatomical proximity of the opening of the urethra and rectum in women.
Venereal urethritis is a disease acquired through direct sexual contact with a sick person or a carrier of pathogenic bacteria. This is how gonococci, chlamydia, ureaplasma and mycoplasma are transmitted. The ease of development of an infectious disease is due to the presence of “folds” in the urethral mucosa, in which bacteria are very well retained.
Possible consequences of urethritis
For women, this disease is considered a big problem. Some pathogens can cross the placenta, causing intrauterine damage to the fetus. The likelihood of spontaneous abortion increases, delays in the baby’s development are observed, and its organs may not be fully formed.
If a therapeutic course is not carried out, the expectant mother is at risk of developing an ascending form of infection of the ureteral system. There is a possibility that the infection will enter the uterus, which can cause a miscarriage.
Prevention
During pregnancy, you need to listen to your feelings and take measures against pathologies. To reduce the risk of urethritis, you need to pay attention to the following recommendations:
- normalize the rest regime;
- maintain hygiene;
- avoid hypothermia;
- avoid stressful situations;
- adjust the diet;
- have sex with a partner, use contraception;
- Visit a gynecologist regularly to check your health.
With responsible adherence to these preventive measures, urethritis and pathologies can be avoided. If the disease begins to manifest itself, self-medication is unacceptable; the pregnant woman is responsible not only for her health, but for the successful development of the fetus.
You cannot take medications without your doctor's knowledge. This applies to drugs and folk remedies. Some herbal remedies are dangerous and sometimes cause miscarriage. The specialist will identify the cause of the disease, determine its degree, and prescribe an adequate course of therapy, taking into account the nuances.
Causes of pathology during pregnancy
There is no particular predisposition of the body to the occurrence of urethritis, but external factors can have a sufficient influence on the occurrence of the disease. The causes of urethritis during pregnancy include:
- hypothermia;
- the presence of sexually transmitted diseases and sexually transmitted infections;
- errors in nutrition and diet. Salty, pickled, bitter, sour, spicy, alcoholic foods enter the bladder, and in case of excess of these products, irritation of the urethra is possible;
- decreased immunity;
- exposure to toxic and radiation factors;
- the presence of infections (chlamydia, ureaplasma, gonococcus, trichomonas, mycoplasma);
- performing medical interventions and procedures;
- presence of urolithiasis;
- the presence of gynecological diseases.
A woman's body has a shorter urethra, which contributes to weaker manifestations of urethritis compared to men. Sometimes urethritis may be asymptomatic or accompanied by minor signs, to which the woman often does not pay much attention. Typically, symptoms of urethritis during pregnancy are:
- the appearance of pain, itching, burning when urinating;
- the appearance of purulent discharge from the external urethra;
- the appearance of redness;
- manifestation of pain at rest in the presence of chronic urethritis.
Urethritis is an inflammation of the walls of the urethra. A distinction is made between infectious and non-infectious diseases.
- Infectious. It is observed when affected by pathogenic microflora (Escherichia coli and various coccal bacteria), and poses the greatest danger during pregnancy.
- Non-infectious. It is observed in cases of injury to the organs of the urinary system, a congenital narrow urethra, and during pregnancy. Tends to become infectious.
The active development of urethritis occurs due to weakening of the muscles of the ureter and urethra under the influence of progesterone, hormonal changes and changes in metabolic processes. In addition, the physiological structure of the female urethra allows infection to enter directly from the environment. Therefore, during pregnancy, during routine examinations, various tests are often carried out for infections and the presence of bacteria in the urine.
The 10 main factors predisposing to the occurrence of infectious and inflammatory processes are:
- Sexually transmitted diseases of a partner, after sexual intercourse with whom the pregnant woman becomes infected. A woman may already have an infection, but become more active during pregnancy.
- Being in a cold room, hypothermia, wearing clothes inappropriate for the weather.
- Untreated inflammatory diseases of the urinary system.
- Allergies to various hygiene items or food products.
- Pathologies of the urinary system.
- Improper diet and drinking regime.
- Poor personal hygiene.
- Stressful situations and overwork.
- Urolithiasis of the kidneys.
- Catheterization for urine collection.
There are specific and nonspecific urethritis during pregnancy. This separation is important because the therapy will be very different.
- Nonspecific urethritis is observed when an infection develops from bacteria inhabiting the microflora of a pregnant woman. And such bacteria appear at the time of weakening of immunity.
- Specific urethritis is observed during the development of infection from sexually transmitted bacteria, such as chlamydia, mycoplasma, and ureaplasma.
Any form of urethritis during pregnancy requires mandatory and immediate treatment, as the risk of complications for the mother and fetus increases. This is especially true for acute urethritis. The bacteria spread up the urinary tract and can cause pelvic inflammation, which in turn increases the risk of infection in the fetus.
During pregnancy, the symptoms of urethritis do not differ from the usual condition.
- Frequent or strong urge to go to the toilet.
- Changes in the process of urination (retention or incontinence).
- Burning pain in the urethral canal.
- Discharges of various types, depending on the concomitant disease.
- Pain in the groin area.
- Redness of the outer labia.
Such discomfort should alert a woman during pregnancy. You should consult a doctor if any of the above symptoms are present.
The causes of urethritis in pregnant women are divided into non-infectious and infectious. The first group of predisposing factors includes:
- hypothermia; previously experienced medical interventions in the genitourinary system (a smear was taken from the girl’s urethra, a catheter was inserted, and a cytoscopy was performed - an examination of the bladder using a cytoscope);
- urinary tract injuries (as a result of kidney stones, for example);
- neglect of personal hygiene rules;
- wearing tight clothes and underwear;
- hormonal changes;
- allergic reactions (to medications, food, for example);
- weakened immune defense, frequent acute respiratory viral infections and acute respiratory infections;
- disordered eating, frequent diet violations (eating spicy, sour, salty foods, pickled delicacies, soda);
- infrequent urination, long waits for the opportunity to empty the bladder;
- insufficient daily water consumption;
- anatomical features of the structure of the genitourinary system.
The infectious prerequisites for the development of urethritis during pregnancy include various infectious and inflammatory diseases that affect the genitourinary system of the expectant mother (cystitis, pyelonephritis, vulvitis, vaginosis and others). In addition, uncontrolled or unprotected sex life can lead to infection of the expectant mother with urethritis pathogens such as chlamydia, gonococci, ureaplasma, and mycoplasma. A girl can get these ailments both before conception and during pregnancy.
Progressive urethritis is manifested by the following symptoms:
- changes in discharge from the urethra (they become mucous or purulent in nature, change the smell, as well as color towards a greenish or bluish tint, an admixture of blood may appear);
- redness and itching of the skin occurs in the genital area;
- during the process of emptying the bladder, a burning sensation or stinging sensation appears;
- the urge to urinate becomes more frequent.
A feature of urethritis in girls, including pregnant women, is that pathogens that spread sexually are present both in the vagina and in the urethra. This is due to the anatomical structure of these organs and the presence of a close functional connection between them.
Diagnosis of urethritis during pregnancy
The doctor collects the expectant mother’s complaints and compiles an anamnesis. The lifestyle of a pregnant girl is important. The doctor takes into account the presence of chronic diseases and inflammatory processes, and also finds out whether the mother has encountered infections of the genitourinary system and surgical intervention in this area. A gynecological examination by an obstetrician-gynecologist is mandatory.
For an accurate and unambiguous diagnosis of urethritis, a pregnant woman will need to undergo a number of medical measures:
- urethroscopy - examination of the urethra (contraindicated in the acute stage of urethritis);
- microscopy of a gynecological smear - analysis of scrapings from the cervical canal of the cervix and vagina;
- pass a urine test (general) and glass samples - the degree of damage to the urinary tract is revealed;
- bacteriological culture of a urological smear of the urethra and urine in order to determine the degree of susceptibility of the irritant to antibiotics;
- Ultrasound of the pelvis, bladder and kidneys;
- PCR diagnostics – the most common pathogens are searched for in pregnant women’s smears, including those transmitted through sexual contact.
In pregnant women, urethritis actively develops against the background of decreased immunity, as well as hormonal disorders and imbalances. A weakened body becomes extremely vulnerable to various types of infections. For this reason, pathogens that contribute to the development of urethritis, which may have previously lived in the vagina and urethra, are activated precisely after conception.
- Traumatic damage to the urethra by fragments of stones passing through it.
- General hypothermia of the body.
- Insufficient fluid intake.
- Failure to comply with personal hygiene rules.
- The presence of urological diseases of an infectious-inflammatory nature.
- Sexually transmitted infections. It should be emphasized that infection can occur even before pregnancy, but not manifest itself as painful symptoms.
- Tendency to allergic reactions.
- Disturbances in the functioning of the genitourinary system.
- Fetal pressure on the urinary canal.
- Excessive consumption of spicy foods.
- Chronic fatigue.
- The presence of defects in the structure of the genitourinary system, both congenital and acquired.
- Excessive physical and psychological stress.
- Disorders of the circulatory process in the pelvic organs.
Features of treatment
To get rid of an infectious disease, you need to choose a remedy for the pathogen. A feature of the treatment of pregnant women is the careful selection of antibacterial drugs that cannot harm the fetus. This is important in the 1st trimester, this time is characterized by the formation of the child’s organs and systems. If the therapy is chosen incorrectly, deviations in the baby’s development are possible.
Treatment for a woman is selected by the attending physician
For the same reason, medications are prescribed to nursing mothers with caution; many medications can pass into breast milk and into the baby’s body. Such drugs can be harmful; when treating nursing mothers, they either choose gentle medications or transfer the baby to artificial feeding.
Treatment of urethritis should solve three main problems:
- Eliminate the inflammatory process in the urethra.
- Stabilize the vaginal microflora.
- Restore the defenses of the expectant mother's body.
Antibacterial drugs are selected taking into account the type of pathogen. In addition to systemic treatment, locally acting agents are prescribed in the form of creams, gels, and ointments with an antibacterial effect.
A procedure for washing the urethra with disinfectant solutions is prescribed.
Complex treatment includes taking vitamin complexes and immunomodulators. You definitely need to review your diet and make the necessary adjustments. First of all, it is recommended to increase the volume of liquid, leaning on sour berry fruit drinks and juices. It is important to exclude spicy, spicy foods and alcoholic drinks.
Complex treatment includes taking vitamin complexes, immunomodulators
It is necessary to undergo treatment, the disease will cause complications - the child will develop conjunctivitis, pneumonia, and otitis media of an infectious nature immediately after birth. It is difficult for a fragile body to endure illness, so it is better to avoid this development of events. As mentioned above, with gonococcal infection, the danger to the fetus is great - placental insufficiency, miscarriage, and fetal death are possible.
As for complications for the pregnant woman’s body, untimely treatment threatens to make the process chronic, the source of inflammation will expand, harmful microorganisms will enter the organs of the genitourinary system, causing malfunction and complications.