During pregnancy, the mother's thyroid gland bears an increased load until the fetus develops its own thyroid gland. During pregnancy, the activity of the thyroid gland especially increases in the first half of the term, because this organ is not yet developed in the baby. Thyroxine (or tetraiodothyronine, T4) and triiodothyronine (T3) are the most important thyroid hormones that ensure the development of organs and systems starting from the first weeks of pregnancy. Therefore, it is so important that they are produced in the right quantities.
Diagnosis of thyroid diseases
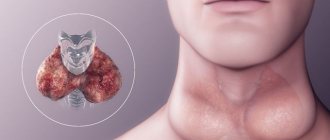
It is necessary to conduct a survey of the patient to collect characteristic complaints, a general examination (skin color, moisture or, conversely, dry skin and mucous membranes, hand tremors, swelling, the size of the palpebral fissure and the degree of its closure, visual enlargement of the thyroid gland and the front of the neck), palpation thyroid gland (increase in its size, isolated thickening of the isthmus of the gland, consistency, pain and mobility, presence of large nodes).
1. Level of thyroid hormones. TSH (thyroid stimulating hormone) is an indicator that is used to screen for thyroid disease; if this indicator is normal, then further testing is not indicated. This is the earliest marker of all dyshormonal thyroid diseases.
The TSH norm in pregnant women is 0.2 - 3.5 µIU/ml
T4 (thyroxine, tetraiodothyronine) circulates in the plasma in two forms: free and bound to plasma proteins. Thyroxine is an inactive hormone that is metabolized into triiodothyronine, which already has all its effects.
Free T4 norm:
I trimester 10.3 - 24.5 pmol/l II, III trimester 8.2 - 24.7 pmol/l
Norm T4 general:
I trimester 100 - 209 nmol/l II, III trimesters 117 - 236 nmol/l
The norms for TSH, free T4 and total T4 in pregnant women differ from the general norms for women.
T3 (triiodothyronine) is formed from T4 by the elimination of one iodine atom (there were 4 iodine atoms per 1 molecule of the hormone, and now there are 3). Triiodothyronine is the most active hormone of the thyroid gland; it is involved in plastic (tissue construction) and energy processes. T3 is of great importance for metabolism and energy exchange in brain tissue, cardiac tissue and bone.
Normal T3 free 2.3 - 6.3 pmol/l Normal T3 total 1.3 - 2.7 nmol/l
2. Level of antibodies to various components of the thyroid gland. Antibodies are protective proteins that the body produces in response to an aggressive agent (virus, bacteria, fungus, foreign body). In the case of thyroid diseases, the body exhibits immune aggression towards its own cells.
To diagnose thyroid diseases, indicators of antibodies to thyroglobulin (AT to TG) and antibodies to thyroid peroxidase (AT to TPO) are used.
The norm of AT to TG is up to 100 IU/ml The norm of AT to TPO is up to 30 IU/ml
Among antibodies for diagnosis, it is advisable to study antibodies to thyroid peroxidase or both types of antibodies, since isolated carriage of antibodies to thyroglobulin is rare and has less diagnostic value. Carriage of antibodies to thyroid peroxidase is a very common situation that does not indicate a specific pathology, but carriers of these antibodies develop postpartum thyroiditis in 50% of cases.
3. Ultrasound of the thyroid gland. Ultrasound examination determines the structure of the gland, the volume of the lobes, the presence of nodes, cysts and other formations. Doppler ultrasound determines blood flow in the gland and in individual nodes. Ultrasound is performed for initial diagnosis, as well as over time to monitor the size of lobes or individual nodes.
4. A puncture biopsy is taking an analysis precisely from a lesion (nodule or cyst) with a thin needle under ultrasound control. The resulting liquid is examined microscopically to look for cancer cells.
Radionuclide and x-ray methods during pregnancy are strictly prohibited.
Thyroid and pregnancy
The thyroid gland is a butterfly-shaped gland weighing 15-20 g, which is located on the front surface of the neck in its lower third. The thyroid gland produces hormones such as thyroxine
(T4) and
triiodothyronine
(T3). In the blood, most of the thyroid hormones are bound to the carrier protein and are inactive, while only a small free fraction of hormones is active and performs its functions.
The function of the thyroid gland is under the control of the hypothalamic-pituitary system. Thyrotropin-releasing hormone is synthesized in the hypothalamus
(TRG).
This hormone, entering the pituitary gland, stimulates the formation of thyroid-stimulating hormone
(TSH), which in turn stimulates the activity of the thyroid gland and the formation of T4 and T3. Thyroid hormones are involved in almost all processes of the body, regulating metabolism, the synthesis of vitamins (vitamin A in the liver), and also take part in the functions of other hormones in the body.
Diseases of the thyroid gland are accompanied by both a decrease and an increase in its function. These diseases can affect the course and outcome of pregnancy, as well as the condition of the newborn. However, with timely detection and correction, almost any pathology of the thyroid gland is not a contraindication to planning and prolonging pregnancy. Pregnancy rarely develops against the background of severe endocrine pathology, since it often leads to impaired reproductive function and infertility.
The most common diagnosis during pregnancy is diffuse enlargement of the thyroid gland.
(goiter) with preservation of euthyroidism and
autoimmune thyroiditis
, leading to changes in hormonal levels in the body.
During pregnancy, the functional state of the thyroid gland changes, which must be taken into account when assessing its condition. In this regard, for the correct interpretation of laboratory parameters reflecting the activity of the thyroid gland, it is important to take into account the following: a combined determination of the level of TSH and free T4 is necessary
;
determination of total T4 and T3 is not informative, since during pregnancy their levels are always increased by 1.5 times; the amount of TSH in the first half of pregnancy is normally reduced in 20-30% of women with singleton and 100% with multiple pregnancies; the level of free T4 in the first trimester is slightly elevated in approximately 2% of pregnant women and in 10% of women with suppressed TSH; the level of free T4, determined in late pregnancy, is borderline reduced with a normal amount of TSH; To monitor the effectiveness of treatment of thyroid pathology, a combined determination of the level of free T4 and TSH is used, and in the case of treatment of thyrotoxicosis
, the level of free T4 alone is used.
To diagnose autoimmune pathology of the thyroid gland, it is advisable to examine only antibodies to thyroid peroxidase (AT-TPO). Carriage of TPO antibodies is a common phenomenon in the population, which does not always have a pathological significance; however, women who carry antibodies to TPO develop postpartum thyroiditis in 50% of cases. To assess the functional state of the thyroid gland during pregnancy, in addition to hormonal studies, echographic examination (ultrasound of the thyroid gland) and fine-needle aspiration biopsy can be used.
Iodine deficiency diseases
Iodine deficiency diseases are pathological conditions that develop due to iodine deficiency and can be prevented by normalizing iodine intake. According to WHO, 30% of the world's population have iodine deficiency diseases. Iodine is an essential component of thyroid hormones. Normally, pregnant women should receive 200 mcg of iodine daily
.
A decrease in iodine intake during pregnancy leads to chronic stimulation of the thyroid gland, a relative decrease in the level of thyroxine in the blood and the formation of goiter in both the mother and the fetus
.
Such patients are more likely to give birth to children with mild psychomotor impairments, and the risk of complicated pregnancy increases, which manifests itself in the form of spontaneous abortions, premature births, congenital malformations of the fetus, and complications during childbirth. Newborn children often experience decreased thyroid function and mental retardation. The most obvious manifestation of iodine deficiency and insufficient intake of iodine into the body is diffuse euthyroid (non-toxic) goiter - a diffuse enlargement of the thyroid gland without compromising its function. “endemic goiter” is also used to refer to goiter caused by iodine deficiency.
.
Enlargement of the thyroid gland during iodine deficiency is a compensatory reaction to ensure the synthesis of a sufficient amount of thyroid hormones under conditions of iodine deficiency. The second most common manifestation of iodine deficiency is the development of nodular goiter
.
Insufficient iodine intake in the body is determined using various research methods. Determination of TSH and thyroglobulin
in blood serum, as well as ultrasound of the thyroid gland help to objectively assess the severity of the pathology. The functional state of the thyroid gland is determined by the level of free T4 and T3 and TSH in the serum. The most effective method of replenishing iodine deficiency is the use of iodized table salt. Since pregnancy is the period of greatest risk for the development of severe iodine deficiency diseases, already at the planning stage, it is advisable for women to prescribe individual iodine prophylaxis with physiological doses of iodine - 200 mcg per day in the form of precisely dosed medications (Iodomarin, Iodide 100/200) or mineral-multivitamin complexes for pregnant women. It is advisable to carry out iodine prophylaxis throughout the entire period of pregnancy and breastfeeding.
The only contraindication for iodine prophylaxis is pathological hyperthyroidism (Graves' disease). The patient has a euthyroid goiter
is not a contraindication for planning pregnancy.
The exception is extremely rare cases of giant goiter with compression phenomena. The main condition for planning pregnancy is reliable maintenance of euthyroidism, which, if necessary, can be ensured by the administration of L-thyroxine
(“Euthyrox”). Treatment of nodular goiter outside pregnancy usually has two goals: reducing the size of the nodule and eliminating clinical symptoms in the presence of hyperfunction of the gland. However, during pregnancy there is no need to achieve a radical reduction in goiter. At a minimum, this is due to the fact that pregnancy is limited and it is difficult to achieve a significant reduction in the volume of the thyroid gland in such a short period of time. In addition, even with sufficient iodine intake during pregnancy, there is a slight increase in the volume of the thyroid gland. Before starting treatment, patients with nodules exceeding 1 cm in diameter undergo an aspiration biopsy of the node.
If, based on a cytological examination, a diagnosis of follicular adenoma of the thyroid gland is established or a malignant neoplasm is suspected, surgical treatment is indicated. Conservative treatment is possible only if a nodular colloid goiter is detected that does not exceed 3 cm in diameter. Most often, it is precisely such nodular formations that are detected. Development of nodular colloid goiter
, as well as diffuse euthyroid goiter, is largely associated with chronic iodine deficiency in the body. Before starting treatment, it is necessary to conduct a hormonal study. Treatment of euthyroid goiter includes the use of three treatment options: monotherapy with iodine preparations; monotherapy with L-thyroxine preparations; combination therapy with iodine and L-thyroxine preparations. Treatment is carried out strictly individually under the supervision of a doctor. Therapy for euthyroid goiter is carried out for at least 6 months, followed by a follow-up examination and assessment of thyroid function.
Nodular goiter and pregnancy
The prevalence of thyroid nodules among pregnant women is 4%
. In the vast majority of cases, nodular colloidal proliferating goiter is detected, which is not a tumor disease of the thyroid gland and, as a rule, does not require surgical treatment. This disease is not a contraindication for planning pregnancy if the nodes do not exceed 4 cm in diameter and are not accompanied by compartment syndrome. If a colloidal proliferating goiter is first detected in a pregnant woman and its size reaches 4 cm, but does not cause compression of the trachea, then surgical treatment is postponed until the postpartum period.
If a nodule larger than 1 cm in diameter is detected, an aspiration biopsy
. Ultrasound control significantly increases the information content of the biopsy. During pregnancy, the risk of increasing the size of nodular and multinodular colloid goiter is not great. Since in the vast majority of cases the function of the thyroid gland in this pathology is not impaired, individual iodine prophylaxis with physiological doses of iodine is recommended for patients during pregnancy. In any case, monitoring of thyroid function is indicated by determining the level of TSH and free T4 in each trimester of pregnancy.
Hypothyroidism and pregnancy
Hypothyroidism is a condition caused by decreased thyroid function and characterized by a reduced level of thyroid hormones in the blood serum. Conditions characterized by a decrease in the secretion of thyroid hormones, regardless of the specific cause that caused the decrease in its functional activity, are usually called primary hypothyroidism. Among the causes of primary hypothyroidism are: abnormalities in the development of the thyroid gland; iodine deficiency diseases; thyroiditis; thyroidectomy; radioactive iodine therapy and thyroid irradiation; congenital hypothyroidism; long-term intake of excess iodine; thyroid tumors. The prevalence of hypothyroidism among pregnant women is 2%
.
Clinically, hypothyroidism is manifested by such signs as general weakness, decreased performance, convulsive muscle contractions, joint pain, drowsiness, depression, forgetfulness, decreased attention and intelligence, increased body weight, decreased heart rate and decreased breathing rate, dry skin, hair loss. rough voice, nausea, constipation, amenorrhea and skin swelling. With hypothyroidism, all processes in the body slow down. In conditions of lack of thyroid hormones
energy is generated with less intensity, which leads to constant chilliness and a decrease in body temperature.
Another manifestation of hypothyroidism may be a tendency to frequent infections. Hypothyroidism in a pregnant woman is most dangerous for the development of the fetus and, first of all, for the development of its central nervous system. The most sensitive method for diagnosing hypothyroidism is to determine the level of TSH, an elevated level of which indicates decreased activity of the thyroid gland, and conversely, a low level of TSH indicates thyrotoxicosis. Thus, the principle of feedback is observed between the levels of thyroid hormones and TSH: when the levels of thyroid hormones decrease, the TSH level increases, and vice versa, when the levels of T4 and T3 increase, the TSH level decreases. However, when interpreting the data obtained, it must be remembered that low TSH levels can also be observed during pregnancy, pituitary gland pathology and other diseases. Normal values for thyroid hormone levels vary depending on the test method, however, in most laboratories they are within the range for T4 - 50-160 nmol/l, for T3 - 1-2.9 nmol/l, for TSH - 0 .5-5.5 mIU/l.
Compensated hypothyroidism is not a contraindication for planning pregnancy. The only treatment for hypothyroidism is thyroid hormone replacement therapy. L-thyroxine is used for this purpose. Treatment and dose adjustment of the drug is carried out under the strict supervision of a physician. Monitoring the adequacy of therapy is assessed by the level of TSH and free T4, which must be examined every 8 to 10 weeks. The goal of therapy is to maintain low-normal TSH levels and high-normal free T4 levels.
Autoimmune thyroiditis and pregnancy
Autoimmune thyroiditis ( Hashimoto's thyroiditis
) is the main cause of spontaneous hypothyroidism. Autoimmune diseases occur when the immune system is unable to recognize tissues of its own body from “foreign” ones, and autoantibodies to thyroid tissues are formed in the body.
For autoimmune thyroiditis
(AIT), when the thyroid gland is affected by an autoimmune process, its additional physiological stimulation does not lead to an increase in the production of thyroid hormones, which is necessary for adequate fetal development in the first half of pregnancy. Moreover, hyperstimulation of the altered thyroid gland can lead to hypothyroidism during pregnancy. However, not every increase in AT-TPO levels indicates AIT. Diagnostic criteria, when identifying a combination of which it is advisable for a pregnant woman to prescribe L-thyroxine therapy, are: an increase in the level of AT-TPO; an increase in TSH levels in early pregnancy of more than 2 mIU/l; an increase in the volume of the thyroid gland by more than 18 ml according to ultrasound.
For diagnosis, blood tests for the level of TSH, thyroid hormones, and antibodies to the thyroid gland are of fundamental importance. Since carriage of AT-TPO does not have clinical manifestations, it is necessary to diagnose this pathology before 12 weeks of pregnancy. If an elevated level of AT-TPO is detected without other signs of AIT, a dynamic assessment of thyroid function during pregnancy is necessary in each trimester.
Treatment with L-thyroxine is prescribed depending on the TSH level. It was noted that women with elevated levels of AT-TPO, even without thyroid dysfunction, have an increased risk of spontaneous abortion in the early stages
.
Thyrotoxicosis and pregnancy
Thyrotoxicosis syndrome is a collective concept that includes conditions that occur with a clinical picture caused by excess levels of thyroid hormones in the blood. "hyperthyroidism" is sometimes used to refer to this condition.
. Currently known diseases accompanied by the clinical picture of thyrotoxicosis are divided into two groups.
- Group 1 - thyrotoxicosis combined with hyperthyroidism: thyroxic adenoma; multinodular toxic goiter; thyrotropinoma; thyroid cancer; hyperthyroid phase of autoimmune thyroiditis; diffuse toxic goiter.
- Group 2 - thyrotoxicosis occurring without hyperthyroidism: subacute thyroiditis; postpartum and painless thyroiditis; radiation thyroiditis; thyroiditis caused by taking amiodarone or α-interferon.
Pathological thyrotoxicosis during pregnancy develops relatively rarely. Its prevalence is 1-2 cases per 1000 pregnancies. Almost all cases of hyperthyroidism in pregnant women are associated with diffuse toxic goiter ( Graves disease
). This pathology is a systemic autoimmune disease that develops as a result of the production of antibodies to the TSH receptor, clinically manifested by an enlargement of the thyroid gland with the development of thyrotoxicosis syndrome in combination with extrathyroid pathology.
Graves' disease is not a contraindication for prolonging pregnancy. In women with moderate and severe disease, infertility develops in almost 90% of cases. Diagnosis of Graves' disease during pregnancy is based on a complex of clinical data and the results of laboratory and instrumental studies. One of the first signs of thyrotoxicosis during pregnancy is often vomiting of pregnancy. At the same time, diagnosing thyrotoxicosis can be difficult, since pregnancy is often complicated by vomiting in the early stages even without thyroid pathology.
The characteristic symptoms of thyrotoxicosis - sweating, feeling hot, palpitations, nervousness, enlarged thyroid gland - are also often found during normal pregnancy. However, eye symptoms specific to Graves' disease may be a clue to the diagnosis, but blood tests measuring thyroid hormone and TSH levels are required to definitively determine the presence of the disease. Long-term thyrotoxicosis is dangerous for the development of miscarriage
, congenital deformities in a child.
However, with proper and timely treatment with thyreostatic drugs, the risk of these complications is not higher than in healthy women. When Graves' disease is first diagnosed during pregnancy, all patients are advised to undergo conservative treatment. Intolerance to thyreostatics is currently considered as the only indication for surgical treatment during pregnancy. Immediately after surgery, pregnant women are prescribed levothyroxine at a dose of 2.3 mcg per kg of body weight. With untreated and uncontrolled diffuse toxic goiter, there is a high probability of spontaneous abortion.
During the first trimester of pregnancy, the use of any medications is extremely undesirable due to their possible teratogenic effect. Therefore, for mild thyrotoxicosis, antithyroid drugs may not be prescribed. Moreover, pregnancy itself has a positive effect on the course of diffuse toxic goiter, which manifests itself in the need to reduce the dose or even discontinue antithyroid drugs in the third trimester.
Standard treatment is carried out with tableted thyreostatic drugs.
: imidazole derivatives (thiamazole, mercazolil, methizol) or propylthiouracil (propyl), the latter being the drug of choice during pregnancy, since it penetrates the placenta to a lesser extent and reaches the fetus.
Treatment is carried out under the supervision of a doctor with individual selection of the dose of the drug. The main goal of thyreostatic therapy during pregnancy is to maintain free T4 levels at the upper limit of normal (21 pmol/l). If indicated, surgery on the thyroid gland
can be performed during pregnancy, but is currently prescribed to patients only if conservative treatment is impossible. The operation is safe in the second trimester of pregnancy (between 12 and 26 weeks).
Thyroid tumors
Thyroid tumors are divided according to histological characteristics into benign (follicular and papillary adenoma, teratoma
) and malignant.
The incidence of thyroid cancer
is 36 per 1 million population per year and is detected 2 times more often in women.
Very often, thyroid cancer is a single painless nodule, which is regarded as an adenoma or nodular goiter. However, this formation tends to grow rapidly, acquires a dense consistency and causes a feeling of pressure in the thyroid gland. The functional state of the thyroid gland, as a rule, remains within normal limits, and only with a significant tumor size can hypothyroidism and, much less frequently, moderate thyrotoxicosis develop.
Almost the only indication for surgical treatment when a thyroid nodule is detected in a pregnant woman is the detection of cancer according to a cytological examination of material obtained as a result of a puncture biopsy
.
The optimal period for surgical treatment is the second trimester of pregnancy. After thyroidectomy,
the patient is immediately prescribed
levothyroxine
at a dose of 2.3 mcg/kg body weight.
Patients with a history of thyroid cancer can plan pregnancy if: at least one year after treatment with I-131 there is no negative dynamics according to periodic determination of thyroglobulin levels; have received treatment for high-grade thyroid cancer in the past; Suppressive therapy is carried out (levothyroxine at a dose of 2.5 mcg per kg of weight). Women planning a pregnancy continue to receive levothyroxine at the same dose, since it closely matches the levothyroxine requirement of a pregnant woman with hypothyroidism.
For women who have received treatment for undifferentiated and medullary thyroid cancer, pregnancy planning is contraindicated according to today's ideas. The exception is patients who underwent prophylactic thyroidectomy for various types of familial forms of medullary thyroid cancer.
After appropriate examination and treatment under the supervision of an endocrinologist, the following categories of patients with thyroid pathology can plan pregnancy: women with compensated primary hypothyroidism that developed as a result of autoimmune thyroiditis or surgical treatment of non-tumor diseases of the thyroid gland; patients with various forms of euthyroid goiter (nodular, multinodular, mixed), when there are no direct indications for surgical treatment (significant size of nodular goiter, compression syndrome); women who carry antibodies to the thyroid gland in the absence of dysfunction. In these patients, during pregnancy it is necessary to conduct a dynamic assessment of thyroid function with determination of TSH and free T4 levels in each trimester of pregnancy. In addition, pregnant women with goiter should undergo dynamic ultrasound examination.
Women with uncompensated hypothyroidism as a result of autoimmune thyroiditis or after surgical treatment of non-tumor pathology of the thyroid gland can plan pregnancy after achieving euthyroidism against the background of levothyroxine replacement therapy. In patients with thyrotoxicosis, after achieving stable remission, pregnancy can be planned after 2 years. radioactive iodine therapy
- Pregnancy should be postponed for 1 year. With surgical treatment of Graves' disease, pregnancy can be planned in the near future against the background of hormone replacement therapy. Therefore, it is important to make an appointment with an endocrinologist as early as possible in order to detect this or that disease!
Make an appointment with specialists by calling a single call center:
+7(495)636-29-46 (metro stations “Schukinskaya” and “Street 1905 Goda”). You can also make an appointment with a doctor on our website, we will call you back!
Causes
Hyperthyroidism is not a diagnosis, but only a syndrome caused by increased production of thyroid hormones. In this condition, the concentration of T3 (thyroxine) and T4 (triiodothyronine) increases in the blood. In response to an excess of thyroid hormones in the cells and tissues of the body, thyrotoxicosis develops - a special reaction accompanied by an acceleration of all metabolic processes. Hyperthyroidism is diagnosed mainly in women of childbearing age.
Diseases in which hyperthyroidism is detected:
- diffuse toxic goiter (Graves disease);
- autoimmune thyroiditis;
- subacute thyroiditis;
- thyroid cancer;
- pituitary tumors;
- ovarian neoplasms.
Up to 90% of all cases of thyrotoxicosis during pregnancy are associated with Graves' disease. Other causes of hyperthyroidism in expectant mothers are extremely rare.
Recommendations for pregnant women with an enlarged thyroid gland
What to do if there is an enlargement of the thyroid gland during pregnancy?
Of course, you must immediately consult a doctor for a timely examination. Pay attention to how you feel, have your appetite increased, have you developed unusual weakness or fatigue, have you noticed a feeling of fatigue?
An additional method of prevention may be following a diet and eating iodine-containing foods.
These pathological changes are easier to prevent. Therefore, we should not forget about the threat posed by dysfunction of the thyroid gland during pregnancy.
Symptoms
The development of thyrotoxicosis is based on the acceleration of all metabolic processes in the body. When the production of thyroid hormones increases, the following symptoms occur:
- low weight gain during pregnancy;
- increased sweating;
- rise in body temperature;
- warm and moist skin;
- muscle weakness;
- fast fatiguability;
- exophthalmos (bulging eyes);
- enlargement of the thyroid gland (goiter).
Symptoms of hyperthyroidism develop gradually over several months. Often the first manifestations of the disease are detected long before the child is conceived. It is possible to develop hyperthyroidism directly during pregnancy.
Excessive production of thyroid hormones interferes with the normal functioning of the cardiovascular system. The following symptoms occur against the background of hyperthyroidism:
- tachycardia (increased heart rate more than 120 beats per minute);
- increased blood pressure;
- feeling of heartbeat (in the chest, neck, head, abdomen);
- heart rhythm disturbances.
Over a long period of time, hyperthyroidism can lead to the development of heart failure. The likelihood of severe complications increases in the second half of pregnancy (28-30 weeks) during the period of maximum stress on the heart and blood vessels. In rare cases, a thyrotoxic crisis develops, a condition that threatens the life of the woman and the fetus.
Thyrotoxicosis also affects the state of the digestive tract. Due to excess synthesis of thyroid hormones, the following symptoms occur:
- nausea and vomiting;
- increased appetite;
- pain in the umbilical region;
- diarrhea;
- liver enlargement;
- jaundice.
Hyperthyroidism also affects the functioning of the nervous system. An excess of thyroid hormones makes a pregnant woman irritable, moody, and restless. Mild memory and attention impairments are possible. Hand tremor is characteristic. With severe hyperthyroidism, the symptoms of the disease resemble those of a typical anxiety disorder or manic state.
Endocrine ophthalmopathy develops in only 60% of all women. Changes in the eyeball include not only exophthalmos, but also other symptoms. Very characteristic is a decrease in the mobility of the eyeballs, hyperemia (redness) of the sclera and conjunctiva, and rare blinking.
All manifestations of hyperthyroidism are most noticeable in the first half of pregnancy. After 24-28 weeks, the severity of thyrotoxicosis decreases. Remission of the disease and disappearance of all symptoms is possible due to a physiological decrease in hormone levels.
Expectation of the baby and the “behavior” of ShchZ
But the conception took place safely, the future mother’s health is good. Or are there still warning signs? These include:
- feeling of constant fatigue;
- disturbances of heart rhythm, sleep, appetite, gastrointestinal tract, mental activity;
- increased blood pressure, sweating;
- tremor, more often of the arms and/or legs, less often - almost total;
- severe toxicosis;
- unhealthy weight fluctuations;
- neuropsychic problems: feelings of fear, irritability, depression (without objective reasons);
- excessive hair loss.
Statistics. Among pregnant patients of endocrinologists, 45% (that is, almost every second) have various disorders of the thyroid gland.
The reason for this is the changes that occur in the body of the mother and child under her heart. They need to be sorted out.
Gestational transient thyrotoxicosis
The functioning of the thyroid gland changes with the onset of pregnancy. Soon after conceiving a child, there is an increase in the production of thyroid hormones - T3 and T4. In the first half of pregnancy, the fetal thyroid gland does not function, and its role is taken over by the maternal gland. This is the only way the baby can receive the thyroid hormones necessary for his normal growth and development.
An increase in the synthesis of thyroid hormones occurs under the influence of hCG (human chorionic gonadotropin). This hormone is similar in structure to TSH (thyroid-stimulating hormone), so it can stimulate the activity of the thyroid gland. Under the influence of hCG in the first half of pregnancy, the concentration of T3 and T4 almost doubles. This condition is called transient hyperthyroidism and is completely normal during pregnancy.
In some women, the concentration of thyroid hormones (T3 and T4) exceeds the norm established for pregnancy. At the same time, a decrease in TSH levels occurs. Gestational transient thyrotoxicosis develops, accompanied by the appearance of all the unpleasant symptoms of this pathology (excitation of the central nervous system, changes in the heart and blood vessels). Manifestations of transient thyrotoxicosis are usually mild. Some women may have no symptoms of the disease.
A distinctive feature of transient thyrotoxicosis is indomitable vomiting. Vomiting with thyrotoxicosis leads to weight loss, vitamin deficiency and anemia. This condition lasts up to 14-16 weeks and goes away on its own without any therapy.
Thyroid dysfunction during pregnancy
The thyroid gland is an endocrine gland. It is part of the endocrine system, has vital importance and synthesizes hormones: iodine-containing (T3 (triiodotyranine), T4 (thyroxine)), peptide (calcitonin), deposits tyrosine (one of the essential amino acids) in the form of thyroglobulin protein.
Thyroid hormones are directly involved in regulating the human internal environment (homeostasis): energy exchange, tissue respiration, and organization of iron and calcium ions.
In modern medicine, there are three groups of thyroid dysfunction:
- Hypothyroidism – disorders associated with decreased levels of hormone production (hypofunction)
- Thyrotoxicosis is a disorder associated with increased levels of hormone production (hyperfunction).
- Thyrotoxicosis, which is (not accompanied by) accompanied by hyperthyroidism
Complications of pregnancy
Against the background of hyperthyroidism, the likelihood of developing the following conditions increases:
- spontaneous miscarriage;
- placental insufficiency;
- delayed fetal development;
- gestosis;
- anemia;
- placental abruption;
- premature birth;
- intrauterine fetal death.
Excessive production of thyroid hormones primarily affects the mother's cardiovascular system. Blood pressure rises, heart rate increases, and various rhythm disturbances occur. All this leads to disruption of blood flow in large and small vessels, including the pelvis and placenta. Placental insufficiency develops - a condition in which the placenta is not able to perform its functions (including providing the baby with the necessary nutrients and oxygen). Placental insufficiency leads to delayed growth and development of the fetus, which adversely affects the health of the child after birth.
Transient thyrotoxicosis, which occurs in the first half of pregnancy, is also dangerous for the woman and the fetus. Uncontrollable vomiting leads to rapid weight loss and a significant deterioration in the condition of the expectant mother. The incoming food is not digested, and vitamin deficiency develops. Lack of nutrients can cause spontaneous miscarriage up to 12 weeks.
Mother's thyroid gland and child's intelligence
The fetal thyroid gland begins to independently synthesize thyroid hormones only in the second trimester of pregnancy. Until this moment, the fetus grows and develops due to the hormones of its mother, which pass well through the placental barrier.
In the early stages of pregnancy, more precisely, in its first weeks, these hormones play a major role in the formation and formation of the central nervous system. In fact, during this period the foundations of the intellect of the future person are laid. At the same time, the formation of the hearing organ and brain structures that are responsible for motor (motor) functions occurs.
This proves that with a pronounced deficiency of hormones in the first trimester, children are born with symptoms of neurological cretinism: irreparable loss of human intelligence, deaf-muteness, and motor disorders. Such disturbances in brain formation in the first trimester are irreversible. Therefore, it is so important to maintain normal functioning of the gland at the beginning of pregnancy.
Causes of reduced maternal gland function
Maintaining euthyroidism directly depends on the compensatory capabilities of the gland itself. And in a healthy thyroid gland these possibilities are extremely high. It is capable of compensatory rapid increase in its volume when its function decreases for any reason.
At the initial stage, this increase occurs within normal sizes, and subsequently a goiter develops, which ensures the synthesis of an adequate amount of thyroid hormones.
But with prolonged exposure to unfavorable factors, the compensatory capabilities of the thyroid gland are depleted and its function decreases. This happens especially quickly during pregnancy and in adolescents during a period of intensive growth.
First, minimal thyroid insufficiency occurs, which has no clinical or laboratory changes. Then this condition turns into subclinical hypothyroidism, which also has no clinical manifestations, but altered laboratory parameters appear. And then manifest hypothyroidism appears with all its clinical picture.
This is facilitated by:
- living in regions where there is an endemic deficiency of iodine, selenium, zinc and other nutrients
- exposure to goitrogenic (thyroid goiter-causing) environmental factors: pollution with chemical waste, smoking or inhalation of cigarette smoke
- autoimmune thyroid diseases
- deficiency of iron, vitamin B12, folic acid
Consequences for the fetus
Maternal hormones (TSH, T3 and T4) practically do not penetrate the placenta and do not affect the condition of the fetus. At the same time, TSI (antibodies to TSH receptors) easily pass through the blood-brain barrier and enter the fetal bloodstream. This phenomenon occurs with Graves' disease, an autoimmune lesion of the thyroid gland. Diffuse toxic goiter in the mother can cause the development of intrauterine hyperthyroidism. It is possible that a similar pathology may occur immediately after the birth of a child.
Symptoms of fetal hyperthyroidism:
- goiter (enlarged thyroid gland);
- swelling;
- heart failure;
- growth slowdown.
The higher the TSI level, the higher the likelihood of complications. With congenital hyperthyroidism, the likelihood of intrauterine fetal death and stillbirth increases. For children born at term, the prognosis is quite favorable. In most newborns, hyperthyroidism goes away on its own within 12 weeks.
Thyroid gland after childbirth
Unfortunately, symptoms of many autoimmune diseases that improve during pregnancy reappear after childbirth. One of the most common thyroid diseases that develops after childbirth is postpartum thyroiditis. It develops according to almost the same pattern as autoimmune thyroiditis. This disease begins two to three months after birth, the activity of the thyroid gland temporarily increases. And a few months after childbirth, hypothyroidism occurs; after a few more months, the activity of the thyroid gland normalizes, its activity becomes normal. Some women may experience only one phase of postpartum thyroiditis. Despite the fact that this condition belongs to the group of self-healing diseases, the activity of the thyroid gland in about 40% of women who have gone through the hypothyroidism phase during PPT decreases within a year after childbirth, and another 20% of women show signs of hypothyroidism after three to four years. If postpartum thyroiditis occurs after the first pregnancy, there is a high risk of its development in subsequent pregnancies.
PPT, although a fairly common complication after childbirth, often goes unnoticed, since its symptoms are similar to normal postpartum symptoms (weakness, hair loss, depression, etc.)
The hyperthyroid phase of postpartum thyroiditis is similar to DTG, however, the disease in the case of PPT does not require treatment and goes away on its own. Sometimes beta blockers are prescribed to lower the heart rate. Taking thyreostatic drugs during PRT is ineffective and can contribute to the onset of hypothyroidism. During hypothyroidism, thyroid hormones are prescribed.
According to one version, it is recommended to diagnose antibodies to the thyroid gland at the 12th week of pregnancy. In case of a positive result, it is recommended that further studies be carried out in order to promptly identify PPT and most effectively treat it. However, there are also opponents of this technique, who claim that there is no need to determine antibodies in the early stages, since PRT in most cases cures on its own and without consequences. In any case, pregnancy, childbirth and the postpartum period are the times when monitoring a woman’s body should be maximum.
Diagnostics
To determine hyperthyroidism, it is necessary to donate blood to determine the level of thyroid hormones. Blood is taken from a vein. The time of day doesn't matter.
Signs of hyperthyroidism:
- increased T3 and T4;
- decreased TSH;
- the appearance of TSI (with autoimmune damage to the thyroid gland).
To clarify the diagnosis, an ultrasound of the thyroid gland is performed. The condition of the fetus is assessed during an ultrasound examination with Doppler measurements, as well as using CTG.
Processes occurring in the thyroid gland during pregnancy.
The metabolism in a woman's body undergoes significant changes during pregnancy. This happens under the influence of the needs of the developing fetus. The tissues of the embryo - the chorion - in the first trimester of pregnancy produce human chorionic gonadotropin (HCG), a hormone whose structure practically repeats the structure of TSH. Thus, hCG has a stimulating effect on the activity of the thyroid gland, respectively, its volume and hormone production increase. This condition is called physiological hyperthyroidism. High activity of the thyroid gland provokes increased absorption of dietary iodine and increased excretion in the urine. If at the beginning of pregnancy there is a decreased level of the T4 hormone, this can lead to disturbances in the formation of the brain, and the development of cretinism in the baby is likely. Until the very end of pregnancy, the amount of thyroid hormones remains increased; it decreases only before childbirth.
Treatment
Outside of pregnancy, priority is given to drug treatment using radioactive iodine preparations. Such drugs are not used in obstetric practice. The use of radioisotopes of iodine can disrupt the course of pregnancy and interfere with the normal development of the fetus.
Antithyroid drugs (not radioisotopes) are used to treat pregnant women. These drugs inhibit the production of thyroid hormones and eliminate the symptoms of thyrotoxicosis. Antithyroid drugs are prescribed in the first trimester immediately after diagnosis. In the second trimester, the dosage of the medication is reviewed. When hormone levels normalize, complete discontinuation of the drug is possible.
Surgical treatment for hyperthyroidism is indicated in the following situations:
- severe course of thyrotoxicosis;
- lack of effect from conservative therapy;
- large goiter with compression of neighboring organs;
- suspected thyroid cancer;
- intolerance to antithyroid drugs.
The operation is performed in the second trimester, when the risk of spontaneous miscarriage is minimized. The extent of surgical intervention depends on the severity of the disease. In most cases, a bilateral subtotal strumectomy (excision of most of the thyroid gland) is performed.
Hyperthyroidism that cannot be treated is an indication for termination of pregnancy. Abortion is possible up to 22 weeks. The optimal time for an induced abortion is considered to be up to 12 weeks of pregnancy.
Thyrotoxicosis
Thyrotoxicosis (increased function of the thyroid gland) develops relatively rarely during pregnancy (in 1-2 per 1000 pregnancies). Almost all cases of thyrotoxicosis in pregnant women are associated with Graves' disease (GD or toxic diffuse goiter, a chronic autoimmune disorder in which there is an enlargement and hyperfunction of the thyroid gland) and the development of hyperthyroidism against the background of the stimulating influence of hCG. If a woman had Graves' disease before pregnancy, then the risk of exacerbation (relapse) of the disease is high in the early period of pregnancy.
Inadequate treatment of thyrotoxicosis is associated with the development of complications: spontaneous abortion, slow intrauterine development of the fetus, stillbirth, premature birth, preeclampsia, heart failure.
If a woman with Graves' disease plans to undergo ART programs, then only against the background of stable normalization of thyroid function (at least 24 months, i.e. 18 months of treatment + normal thyroid hormone levels for at least 6 months without treatment!). Inadequately treated Greivas disease is clearly associated with adverse pregnancy outcomes, particularly the risk of miscarriage, in ART programs!
The assessment of thyroid function is carried out by the level of thyroid-stimulating hormone (TSH), thyroid hormones in the blood (T4, T3) with an assessment of the titer of “thyroid-stimulating” antibodies in the blood (ABs to rTSH should be significantly increased!).
According to modern concepts, thyrotoxicosis due to Graves' disease is not an indication for termination of pregnancy, since effective and relatively safe methods of conservative treatment of this disease have now been developed.
If a pregnant woman (including a young woman with preserved ovarian reserve and planning ART) has thyrotoxicosis, the main goal of treatment is to prescribe thyreostatics (drugs that suppress the synthesis of thyroid hormones) in the minimum effective dose to maintain T4 level is at the upper limit of normal or slightly above normal. Propylthiouracil (PTU) is considered the drug of choice (taking into account safety for the fetus) in the first trimester; from the second trimester, thiamazole (tyrosol) is used in an equivalent dose. Monitoring of T4 and T3 levels is carried out every 4 weeks.
With an increase in pregnancy, there is a natural decrease in the severity of thyrotoxicosis and a decrease in the need for drugs, which in most women in the third trimester of pregnancy, as a rule, are completely discontinued. When taking small doses of PTU (100 mg/day) or tyrosol (5-10 mg), breastfeeding is quite safe for the child. However, 2-3 months after birth, in most cases, a relapse (worsening) of thyrotoxicosis develops, requiring an increase in the dose of thyreostatic.
An alternative method of treating thyrotoxicosis in a woman outside pregnancy (including a young woman with preserved ovarian reserve and planning ART) against the background of Graves' disease (or its relapse after therapy with thyreostatics) may be therapy with radioactive iodine (I-131). After radioactive iodine therapy, planning an independent pregnancy or conducting ART programs is possible only 12 months after the end of treatment; during the entire treatment period (12 months), it is necessary to use effective methods of contraception - radioactive iodine therapy is contraindicated during pregnancy and lactation!
You should know that in women of advanced reproductive age (over 35 years old) with reduced ovarian reserve, the treatment of choice for Graves' disease is surgical removal of the thyroid gland (thyroidectomy). This treatment tactic is recognized as the most effective and safe and makes it possible to plan ART as soon as possible! The tactics of long-term treatment with thyrotoxicosis (more than 1.5 years) and follow-up (6 months) to confirm stable normalization of thyroid function, as well as the high probability of relapse of thyrotoxicosis during pregnancy in ART programs are not justified in women of late reproductive age.
Often in the postpartum period there is an exacerbation of thyroid disease (in 5-9% of all women), which occurred in the mother before conception. Therefore, after childbirth, such women should continue to be monitored by an endocrinologist.
Pregnancy due to hypothyroidism
Hypothyroidism is a condition in which the production of thyroid hormones is reduced.
Causes:
1. Autoimmune thyroiditis (the most common cause of hypothyroidism, the essence of the disease is damage to the thyroid gland by its own protective antibodies) 2. Lack of iodine 3. Damage by various types of influence (drugs, radiation exposure, surgical removal, etc.) 4. Congenital hypothyroidism
A separate cause is considered to be relative hypothyroidism that develops during pregnancy. There are enough thyroid hormones for normal life, but in conditions of increased consumption during pregnancy, they are no longer needed. This may indicate that there are disorders in the gland, but they only appeared against the background of increased load.
Classification:
1. Subclinical hypothyroidism. Hypothyroidism, which is detected by laboratory tests, but does not manifest itself with obvious clinical signs. This stage of hypothyroidism can be detected during examination of an infertile couple or when contacting about excess weight gain, as well as in other cases of diagnostic search. Despite the fact that there is no bright clinic, metabolic changes have already begun, and they will develop if treatment is not started.
2. Manifest hypothyroidism. This stage of hypothyroidism is accompanied by characteristic symptoms.
Depending on the presence and effect of treatment, there are:
- compensated (there is a clinical effect from treatment, TSH levels have returned to normal) - decompensated
3. Complicated. Complicated (or severe) hypothyroidism is a condition that is accompanied by severe dysfunction of organs and systems and can be life-threatening.
Symptoms:
1. Changes in the skin and its appendages (dry skin, darkening and roughening of the skin of the elbows, brittle nails, loss of eyebrows, which begins from the outer part).
2. Arterial hypotension, less commonly, increased blood pressure, which is difficult to treat with conventional antihypertensive drugs.
3. Fatigue, even severe, weakness, drowsiness, memory loss, depression (the complaint that “I wake up already tired” often appears).
4. Weakening of taste, hoarseness of voice.
5. Weight gain with decreased appetite.
6. Myxedema, myxedema lesion of the heart (swelling of all
tissues), accumulation of fluid in the pleural cavity (around the lungs) and in
pericardial region (around the heart), myxedema coma (extremely
severe manifestation of hypothyroidism with damage to the central nervous system
Diagnostics:
On palpation, the thyroid gland can be diffusely enlarged or only the isthmus, painless, mobile, consistency can vary from soft (testy) to moderately dense.
1. Study of thyroid hormones. The TSH level is above 5 µIU/ml, T4 is normal or reduced.
2. Antibody research. AT to TG is above 100 IU/ml. AT to TPO is above 30 IU/ml. Elevated levels of autoantibodies (antibodies to one's own tissues) indicate an autoimmune disease, most likely in this case the cause of hypothyroidism is autoimmune thyroiditis.
3. Ultrasound of the thyroid gland. Ultrasound can detect changes in the structure and homogeneity of thyroid tissue, which is an indirect sign of thyroid disease. Small nodules or cysts may also be found.
Hypothyroidism and its effect on the fetus.
Hypothyroidism affects approximately one in 10 pregnant women, but only one has obvious symptoms. But the effect of a lack of thyroid hormones on the fetus is manifested in both.
1. Effect on the development of the fetal central nervous system (CNS). In the first trimester, the fetal thyroid gland is not yet functioning, and the development of the nervous system occurs under the influence of maternal hormones. If they are deficient, the consequences will be very sad: malformations of the nervous system and other defects, cretinism.
2. Risk of intrauterine fetal death. The first trimester is especially important, when the fetal thyroid gland is not yet functioning. Without thyroid hormones, the entire spectrum of metabolism is disrupted, and embryo development becomes impossible.
3. Chronic intrauterine fetal hypoxia. Lack of oxygen adversely affects all processes of fetal development and increases the risk of intrauterine death, the birth of low birth weight babies, premature and discoordinated births.
4. Impaired immune defense. Children with a lack of thyroid hormones in the mother are born with reduced immune function and have poor resistance to infections.
5. Congenital hypothyroidism in the fetus. If the mother has the disease and is not fully compensated, the fetus has a high risk of congenital hypothyroidism. The consequences of hypothyroidism in newborns are very diverse, and you need to know that if left untreated, they become irreversible. Characteristic: delayed physical and psycho-motor development, up to the development of cretinism. With early diagnosis and timely initiation of treatment, the prognosis for the baby is favorable.
Consequences of hypothyroidism for the mother
Manifest hypothyroidism, compared to subclinical hypothyroidism, has the same complications, but much more often.
1. Preeclampsia. Preeclampsia is a pathological condition characteristic only of pregnant women, manifested by a triad of symptoms: edema - arterial hypertension - the presence of protein in the urine (read more in our article “Preeclampsia”).
2. Placental abruption. Premature abruption of a normally located placenta occurs due to chronic placental insufficiency. This is a very serious complication of pregnancy with high maternal and perinatal mortality.
3. Anemia in pregnant women. Anemia in pregnant women is already extremely common in the population, but in women with hypothyroidism, the clinical picture of anemia (drowsiness, fatigue, lethargy, skin manifestations and hypoxic condition of the fetus) is superimposed on the same manifestations of hypothyroidism, which enhances the negative effect.
4. Post-term pregnancy. Against the background of hypothyroidism, various types of metabolism are disrupted, including energy, which can lead to a tendency to post-term pregnancy. A pregnancy lasting more than 41 weeks and 3 days is considered post-term.
5. Complicated course of labor. For the same reason, childbirth can be complicated by weak labor forces and incoordination.
6. Bleeding in the postpartum period. The risk of hypotonic and atonic bleeding in the afterbirth and early postpartum period is increased, as the general metabolism is slowed down and vascular reactivity is reduced. Bleeding significantly complicates the course of the postpartum period and ranks first among the causes of maternal mortality.
7. The risk of purulent-septic complications in the postpartum period is increased due to reduced immunity.
8. Hypogalactia. Reduced breast milk production in the postpartum period can also be caused by thyroid hormone deficiency.
Treatment:
The only scientifically proven treatment method is hormone replacement therapy. Patients with hypothyroidism are prescribed lifelong treatment with L-thyroxine (levothyroxine) in an individual dosage. The dosage of the drug is calculated based on the clinical picture, the patient’s weight, and the duration of pregnancy (in the early stages the dosage of the hormone is higher and then reduced). The drug (trade names “L-thyroxine”, “L-thyroxine Berlin Hemi”, “Eutirox”, “Thyreotom”), regardless of the dosage, is taken in the morning on an empty stomach, at least 30 minutes before meals.
Prevention:
In endemic areas, iodine prophylaxis is indicated for life in various regimens (with interruptions).
During pregnancy, taking iodine supplements is recommended for all pregnant women in a dose of at least 150 mcg, for example, as part of complex vitamins for pregnant women (Femibion Natalcare I, Vitrum Prenatal).
Please note that the popular drug Elevit pronatal does not contain iodine, so potassium iodide preparations (iodomarin, iodine-active, 9 months potassium iodide, iodine balance) are additionally prescribed.
The dosage of iodine preparations starts at 200 mcg; as a rule, this is enough for prevention.
Taking iodine preparations begins 3 months before the expected pregnancy (if you are sure that the thyroid gland is healthy and only prevention is needed) and continues throughout the entire period of gestation and lactation.
Hypothyroidism
In a situation where a woman has a thyroid disease even before pregnancy, leading to a decrease in its function (hypothyroidism), physiological hyperstimulation of the thyroid gland during pregnancy (on its own or in IVF programs) to one degree or another affects its reserve capabilities, and even the use powerful compensatory mechanisms are not sufficient to ensure such a significant increase in the production of thyroid hormones during pregnancy.
Hypothyroidism during pregnancy is most dangerous for the development of the fetus and, first of all, damage to the central nervous system, intrauterine death, the formation of congenital malformations, as well as the birth of a low-weight child, and neurological diseases in the newborn. The state of hypothyroidism in the mother increases the risk of spontaneous abortion, postpartum hemorrhage, and preeclampsia (a cerebrovascular accident that can lead to cerebral edema, increased intracranial pressure, and functional disorders of the nervous system).
An assessment of thyroid function is carried out for all women with reproductive disorders (infertility, miscarriage, etc.). Timely correction of thyroid dysfunction is carried out by an endocrinologist at the stage of preparation for ART programs!
Compensated hypothyroidism is not a contraindication for planning pregnancy, incl. in ART programs! (in women with compensated hypothyroidism upon pregnancy and an increasing need for thyroid hormones, the dose of levothyroxine (L-T4) that they took before pregnancy is immediately increased by approximately 30-50%).
Thyroid function is assessed only by the level of thyroid-stimulating hormone (TSH) in the blood (a hormone secreted by the anterior pituitary gland, a gland located on the lower surface of the brain that has a direct stimulating effect on the functioning of the thyroid gland).
As mentioned above, normally in the early stages of pregnancy a highly normal or even elevated level of thyroid hormones is characteristic, and therefore, “according to the principle of negative feedback”, a low or even suppressed (in 20-30% of women) TSH level will be noted: < 2, 5 honey/l.
It is advisable to carry out screening for thyroid dysfunction at the earliest possible time: preferably during determination (β-subunits of hCG to confirm pregnancy!
If the TSH level exceeds 2.5 mIU/l, the woman is indicated for replacement therapy with levothyroxine (L-T4). It is advisable to monitor TSH and T4 blood levels every 4 weeks in the first trimester, and then as necessary. Adequate replacement therapy is considered to be maintaining TSH levels at the lower limit of reference values for the corresponding stage of pregnancy.
Pregnancy due to hyperthyroidism
Hyperthyroidism (thyrotoxicosis) is a disease of the thyroid gland, accompanied by increased production of thyroid hormones.
Thyroid hormones are catabolic, that is, they accelerate metabolism. With their excess, the metabolism accelerates significantly, calories obtained from carbohydrates and fats are burned at a high speed, and then protein breakdown occurs, the body works to the limit and “wears out” much faster. The breakdown of muscle proteins leads to dystrophy of the heart muscle and skeletal muscles, impaired conduction of nerve fibers and absorption of nutrients in the intestine. Almost all complications of thyrotoxicosis for the mother and fetus are associated with an enhanced catabolic effect.
Causes:
1. Diffuse toxic goiter (or Graves-Bazedow disease, which consists in the fact that the body produces autoantibodies to TSH receptors, so the receptors become insensitive to the regulatory effects of the pituitary gland and the production of the hormone becomes uncontrolled).
2. Nodular goiter (nodules form in the thyroid gland, which provide hyperproduction of thyroid hormones).
3. Tumors (thyroid adenoma, TSH-secreting pituitary tumors, ovarian struma - a tumor in the ovary that consists of cells similar to thyroid cells and produces hormones).
4. Overdose of thyroid hormones.
Specific causes of thyrotoxicosis in a pregnant woman are:
- transient increase in the level of thyroid hormones, which is physiologically determined (depends on the level of hCG). As a rule, this condition is temporary, is not accompanied by a clinic and does not require treatment. But sometimes pregnancy can become the starting point for thyroid disease, which developed gradually, but only manifested itself under conditions of increased stress.
— excessive vomiting of pregnant women (severe early toxicosis) can provoke hyperfunction of the thyroid gland.
- hydatidiform mole (tumor-like growth of the chorionic villi, in which pregnancy has occurred, but does not develop). The condition is detected in the earliest stages of pregnancy.
Classification
1. Subclinical hyperthyroidism (T4 level is normal, TSH is low, no characteristic symptoms).
2. Manifest hyperthyroidism or obvious (T4 level is increased, TSH is significantly decreased, a characteristic clinical picture is observed).
3. Complicated hyperthyroidism (arrhythmia such as atrial fibrillation and/or flutter, cardiac or adrenal insufficiency, obvious psychoneurotic symptoms, organ dystrophy, severe weight deficiency and some other conditions).
Symptoms
1. Emotional lability, groundless worry, anxiety, fears, irritability and conflict (appearing in a short period of time).
2. Sleep disturbance (insomnia, frequent waking up at night).
3. Tremor (hand tremors, and sometimes general tremor).
4. Dryness and thinning of the skin.
5. Increased heart rate, which is observed persistently, the rhythm does not slow down at rest and during sleep; rhythm disturbances such as atrial fibrillation and flutter (disconnected contraction of the atria and ventricles of the heart, the rhythm frequency sometimes exceeds 200 beats per minute).
6. Shortness of breath, decreased exercise tolerance, fatigue (a consequence of heart failure).
7. Rare blinking of the eyes, dry cornea, tearing, in clinically advanced cases, protrusion of the eyeball, decreased vision due to optic nerve dystrophy.
8. Increased (“ravenous”) appetite, colicky abdominal pain for no apparent reason, periodic causeless loose stools.
9. Weight loss due to increased appetite.
10. Frequent and copious urination.
Diagnostics
On palpation, the gland is diffusely enlarged, nodules can be palpated, palpation is painless, the consistency is usually soft.
1) Blood test for quantitative hormone content: TSH is reduced or normal, T4 and T3 are increased, AT in TPO and TG is usually normal.
2) Ultrasound of the thyroid gland to determine its size, tissue homogeneity and the presence of nodules of various sizes.
3) ECG to determine the correctness and frequency of the heart rhythm, the presence of indirect signs of cardiac muscle dystrophy and repolarization disorders (conduction of electrical impulses).
Consequences of hyperthyroidism for the fetus
- spontaneous abortion, - premature birth, - delayed growth and development of the fetus, - birth of low-birth-weight children, - congenital pathologies of fetal development, - antenatal fetal death, - development of thyrotoxicosis in utero or immediately after the birth of the baby.
Consequences for the mother
- Thyrotoxic crisis (a sharp rise in thyroid hormones, accompanied by severe agitation, up to psychosis, increased heart rate, a rise in body temperature to 40-41 ° C, nausea, vomiting, jaundice, in severe cases coma develops). — Anemia of a pregnant woman. — Premature detachment of a normally located placenta. — Development and progression of heart failure, which, when advanced, becomes irreversible. - Arterial hypertension. - Preeclampsia.
The main signs and causes of thyroid dysfunction during pregnancy
Consider hypothyroidism. Signs of hypothyroidism include both physical ailments and psychological disorders, such as:
- drowsiness and weakness,
- bradycardia,
- increased fatigue,
- dyspnea,
- decrease in lung volume;
- frequent constipation, nausea,
- flatulence;
- weight gain (rapid, unjustified by changes in eating habits);
- decreased concentration, disturbance of emotional status (depression);
- brittle hair, dry skin;
- menstruation disorders (aminorrhea, uterine bleeding);
- mastopathy;
- problems with conception;
- feeling of cold (chilliness).
There are several causes of hypothyroidism during pregnancy - iodine deficiency (territorial), surgery for the thyroid gland, autoimmune thyroiditis (antibodies to the tissues of the own gland).
The latter disease causes the destruction of gland cells and a decrease in hormone production.
The next type of disorder that we will consider is thyrotoxicosis. This type of pathology in pregnant women is registered more often than hypothyroidism. The most common type of thyrotoxicosis occurring in women during pregnancy is diffuse toxic goiter, a disease associated with hyperplasia and hyperfunction of the thyroid gland. The most striking manifestation of thyrotoxicosis in pregnant women is severe vomiting. However, this sign does not facilitate the diagnosis of this type of disease, because vomiting can accompany pregnancy in the early and late stages without connection with thyroid pathology. Therefore, we will also pay attention to other signs of thyrotoxicosis, which include:
- anemia;
- diarrhea;
- tremor;
- tachycardia;
- arrhythmia;
- increased sweating;
- heat intolerance;
- decrease, sometimes with increased appetite, body weight;
- low-grade fever (increased body temperature 37-37.3 degrees);
- thyrotoxic crisis;
- exophthalmos;
- hyperreflexia.
By the way, we recommend reading the article Cyst in the thyroid gland - is it dangerous?
Newborns whose mothers suffered from thyrotoxicosis experience constipation, decreased muscle tone and level of reflexes, swelling and dryness of the skin, and thickening of the tongue.
We should also draw the attention of expectant mothers to such a phenomenon as postpartum thyroiditis. This phenomenon is due to the fact that a moderate increase in the functions of the thyroid gland is replaced by a period of moderate decline in its functions. This condition can occur during the first three months after birth. And, quite often, “self-healing” occurs after 6-8 months. Those. gland function is restored to normal levels without drug intervention. Or when exposed to mild thyrocine replacement therapy. However, you cannot count on the fact that everything will go away spontaneously, because... postpartum thyroiditis poses a risk of transition to the stage of persistent hypothyroidism in the future.