Complications of lumbago 299
In modern society, spondylosis of the lumbosacral region no longer appears after the age of 40, but is diagnosed in many young people aged 28–35 years. This degenerative dystrophic disease associated with complex destruction of the spinal column can lead to disability and loss of the ability to move independently in space. In the early stages, it gives a feeling of slight stiffness and loss of freedom to perform certain movements.
Spondylosis of the lumbosacral spine is the most common localization of the pathological process. The disease itself manifests itself in the form of excessive deposition of calcium salts on the bone tissues of the vertebral bodies. There is a gradual deformation and sclerosis of the endplates and periosteum. When spines and calluses form, the process of leaching calcium and phosphorus salts from bone trabeculae can simultaneously be observed.
The pathogenesis of this pathological process includes several important stages:
- disruption of the diffuse nutrition of the cartilaginous tissues of the intervertebral discs, which are designed to provide reliable protection of the vertebral bodies and the radicular nerves extending through their foraminal openings;
- dehydration and loss of elasticity of the cartilage tissues of the intervertebral discs, reduction in their height (protrusion stage);
- collision of adjacent vertebral bodies during serious physical activity and the formation of microscopic chips and cracks on their surface;
- deposition of calcium salts at cracks;
- injury to surrounding soft tissues by osteophytes and pull of inflammatory reaction factors into this area;
- strengthening the process of calcification of surrounding tissues.
If timely treatment is not started, spondylosis of the lumbosacral spine progresses rapidly. This leads to complete fusion of the affected vertebral bodies, loss of flexibility and shock-absorbing capacity of the spinal column.
Currently, conservative treatment of spondylosis is possible only in the initial stages. If the disease is diagnosed at stages 1-2, then the patient has a chance to completely restore the health of his spine without surgical intervention. It is best to use manual therapy methods, therapeutic exercises, physiotherapy, kinesiotherapy, etc. for these purposes. If the pathology is detected at stages 3-4, then the best solution would be to undergo surgery, and then undergo a course of rehabilitation in order to restore one’s physical activity and prevent the risk of recurrence of this disease in the future.
Causes
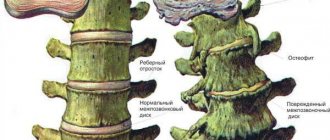
Comparison of spondylosis and other degenerative changes of the spine
Spondylosis of the lumbosacral spine is formed mainly due to disruption of the activity and structure of the intervertebral discs. The body tries in every possible way to adapt to work in completely new and not entirely familiar conditions.
Spondylosis is characterized by the formation of bone growths - osteophytes, which try to fix each vertebra in its natural position, preventing their loss or displacement.
Significant growth of osteophytes provokes impaired mobility of the spine, as a result of which the disease can even lead to disability. There are certain factors that provoke this condition, namely:
- eating disorders;
- excessive body weight;
- metabolic diseases;
- sedentary lifestyle;
- sedentary work;
- significant physical activity.
In addition, this disease can occur in professional athletes, as well as people whose professional activities involve constant vibration. Chronic diseases of internal organs and injury to the spinal column can also provoke the occurrence of pathology.
What it is?
Spondylosis of the lumbosacral region is understood as one of the complications of osteochondrosis and, at the same time, a complex independent disease.
The basis of the pathology is changes in the spine of a dystrophic and degenerative nature, causing the appearance of osteophytes - pathological changes in the structure of the vertebrae. Osteophytes are overgrowths of bone tissue and are the main symptom of the disease. Therefore, diagnosing spondylosis of the lumbosacral region, as a rule, does not take much time.
Clinical picture
At the early stage of development of spondylosis, there are no symptoms of the disease . As the osteophytes grow, the person begins to feel a dull, nagging pain.
Pain in the lower back is similar to the pain that occurs with radiculitis. However, in the case of spondylosis, the pain becomes less if the patient is in the fetal position or flexed position, where the torso is tilted forward and down.
As the pathology progresses, the nerve roots are pinched , and osteophytes grow and put force on the intervertebral discs . The result is acute pain in the lower back, spreading to the lower limbs. Sometimes patients experience numbness in their calves, ankles and toes, but such phenomena are short-lived.
Prevalence and significance
Spondylosis can affect different parts of the spine , but in most cases it is observed in the lumbosacral region, because in this place the spinal column experiences the greatest load.
Video: “What are spinal osteophytes?”
Symptoms
In the initial stages, spondylosis almost does not manifest itself at all and the patient does not experience any painful sensations. Pain begins to appear only during the period of intensive growth of neoplasms, at a time when they begin to excessively irritate the spinal column.
At the initial stage of the disease, painful sensations can be dull, aching in nature and are localized in the lower back. Pathology can only be detected by X-ray examination. One of the most characteristic signs of the disease is a decrease in the intensity of painful sensations or their complete cessation when the body is tilted forward. In this position, the load on the spine is reduced and thus the patient experiences significant relief.
In addition, over time, tension in the lower back may increase, which provokes vascular spasm. Painful sensations increase over time and periodically they can radiate to the leg. In addition, damaging spondylosis can manifest itself as periodic numbness of the legs.
Symptoms of spondylosis
Characteristic signs of spondylosis:
- lumboischialgia;
- sensory disturbances in the foot area;
- crawling sensation, numbness in the calves, tingling in the legs (manifestations of paresthesia);
- limited mobility in the lumbosacral region.
The diagnostic distinguishing sign of spondylosis is a decrease in pain in the fetal position (curling up) and when bending forward, since the load on the anterior longitudinal ligament of the spine in this position is reduced - this is the difference between spondylosis and radiculitis.
With spondylosis, in the morning there is always stiffness in movements in the lower back and legs; when trying to move, a synchronized increase in pain is evidence of the appearance of osteophytes. Unpleasant sensations noticeably decrease after doing exercises and exercises. Relief comes after rest and reducing the load on the lower back. Later, lameness and pain in the leg appear, which do not disappear with rest.
When palpating the spinous processes, the neurologist necessarily detects the appearance of pain in the patient. This occurs due to compression of the nerve endings. In the later stages, a new symptom appears: the patient is absolutely unable to straighten the knee. If lumbar spondylosis is left untreated, the curvature of the spine increases and scoliosis develops. The range of movements is also sharply reduced.
With prolonged static loads (staying in one position at work, constant sitting or standing), the paravertebral muscles spasm and do not work, and their chronic inflammation develops. Therefore, all problems with the spine must be solved immediately, without starting them.
Spondylosis most often deforms the 3rd and 4th lumbar vertebrae, the sacrum is not affected; and with osteochondrosis, the 5th lumbar and 1st sacral vertebrae are most often affected. At first there may be no pain; they appear later, in advanced stages, becoming dull and constant.
If a vertebral subluxation occurs, the pain becomes sharp and intense. If left untreated, complete immobility may occur. As the process progresses, posture changes; skin sensitivity decreases; with severe infringement of the nerve roots, sensitivity disappears completely.
There are 3 degrees of pathology:
- Spondylosis 1st degree - lower back pain is periodic; 2nd degree - the pain becomes constant and stiffness appears.
- Spondylosis of the 2nd degree already reduces the patient’s quality of life; patients cannot work fully and need to be transferred to light work or registered as a 3rd group of disability.
- 3rd degree - pain is severe, paresthesia is present, movements are limited, disability is possible. All symptoms of lumbar spondylosis can be combined into 3 groups: reflex, radicular and vascular. Reflex are all kinds of manifestations in the lumbar region: lumbago - attacks of sharp pain in the lower back that occur suddenly, immediately. More often associated with awkward movements, heavy lifting, coughing, etc. In this case, profuse sweat appears. With rest, the pain subsides slightly, but does not allow movement, appearing again.
Lumbodynia, or lumbago, is prolonged pain in the lower back due to the development of radicular syndrome; worse when standing and calm down in a horizontal position. They are usually preceded by cooling. They go away on their own in a few days. But sometimes they transform into lumboischialgia.
Lumboischialgia is a combination of lumbar pain and sciatica: pain in the buttock, back of the leg, but not up to the foot. Radicular-vascular changes - when ischemia develops in areas of compression, the radicular veins and arteries also find themselves in a compressed state. Paralysis and paresis of the legs may develop.
Diagnostics
To make a correct diagnosis and select the most appropriate method of therapy, it is imperative to perform a comprehensive examination. It involves an X-ray examination of the spinal column. The photographs are taken in several standard and additional lateral projections. This research technique allows you to assess the condition of the vertebrae, identify osteophytes, and also assess the level of pathology of individual areas of the spinal column. Additionally, tomography may be prescribed, which is used to determine the presence of pathology.
Important! Only a high-quality, comprehensive, thorough examination will allow us to determine the presence of pathology and select a method of therapy.
Cervical spine
The cervical vertebrae are small in size, less durable, and have poorly developed muscles compared to other vertebrae. At the same time, the cervical spine is the most mobile and is subject to heavy loads. Long-term preservation of a non-physiological position of the neck overloads the intervertebral discs and ligaments of the spine.
Cervical spondylosis most often develops as a protective reaction to pathological changes in the intervertebral discs that accompany osteochondrosis. The resulting osteophytes increase the area of support for the discs and prevent damage caused by dehydrated intervertebral discs. However, the progressive process of proliferation of osteophytes leads to fusion of the vertebrae with each other, complicating the mobility of the cervical spine. In addition, bone growths narrow the canals of the spine and impinge on nerve fibers and blood vessels.
Compression of the vertebral artery can lead to a mini-stroke. The development of the disease is influenced not only by age, but also by a number of factors:
- Long-term statistical loads, sedentary work.
- Congenital disorders of the spine.
- Compression fracture of the cervical vertebra.
- Impaired metabolism, causing the deposition of calcium salts.
- Hormonal pathologies.
- Frequent hypothermia.
- Hereditary predisposition.
- Predisposing circumstances include poor posture, curvature of the spine, and increased cervical lordosis.
Reference! Patients diagnosed with spondylosis are recommended to sleep on a hard surface to reduce microtrauma to the spine.
Treatment
Treatment of lumbosacral spondylosis should be carried out comprehensively, since only in this way can the most positive results of therapy be achieved. The method of therapy is selected only after diagnosis, during which the localization of the pathology and the degree of damage to the nervous system are taken into account.
Therapy involves the use of medications, as well as physical therapy techniques. In addition, an additional massage course, special gymnastics and swimming are provided. Among the main areas of physiotherapeutic techniques are magnetic therapy and acupuncture.
Patients for whom absolutely any physical exercise is strictly contraindicated are prescribed phonophoresis with the use of hydrocortisone. Medicinal products that significantly slow down the ongoing processes of cartilage damage are indicated. To eliminate painful sensations, anti-inflammatory drugs are indicated, in particular, such as Diclofenac or Nimesulide.
In acute and excessively advanced stages of pathology, when conservative methods do not bring the required result, surgical intervention is performed.
Treatment methods for spinal spondylosis
There are several possible ways to treat spondylosis and osteochondrosis, including restorative and symptomatic therapy. The formation of bone growths on the spine is irreversible and the disease cannot be completely eliminated by any treatment method. However, the use of basic techniques makes it possible to slow down the progression of the disease, relieve pain and improve blood supply to tissues, as well as reduce the consequences.
Before starting treatment, it is important to establish the extent of the lesion, as well as the causes of its occurrence. Diagnosis is carried out with the participation of a surgeon and neurologist. In some cases, consultation with a therapist and other specialists may be necessary.
Drug treatment
The use of medications is necessary to relieve the main symptoms: pain and spasms. Anti-inflammatory medications and tissue repair agents are also used.
Anti-inflammatory drugs against non-steroidal spondyloarthrosis:
- Arthrotek (prescribed twice a day in one dosage);
- Plivalgin (one tablet three times a day);
- Ketorolac (three times a day according to dosage).
Chondroprotectors in injection form:
- Alfutop (10 milligrams for three weeks);
- Artradol (up to thirty-five injections per day);
- Rumalon (one dosage every three days).
To restore bone and cartilage tissue:
- Aloe extract (rub the affected area daily for two to three weeks);
- Contractutex (use in the coccyx and lower back area daily for a month).
For external use, patients are prescribed ointments and creams against persistent pain in the lower back and back, which contain capsaicin. Warming medications:
- Ketonal;
- Nise;
- Fastum-gel;
- Voltaren-gel.
Drug therapy is used in the treatment of deficient spondylosis only as supportive and is not considered mandatory.
Healing Fitness
Exercise therapy allows you to strengthen the muscle corset, relieve pain, improve the functioning of the spine and prevent serious complications. Classes, as a rule, take place in a lying or sitting position and begin with the easiest and simplest exercises. Gradually, the load and intensity of physical training increases, and lifting of the lower limbs and bending are added.
Universal exercises for the lumbosacral region:
- Lie on your back, pressing your arms tightly to your body. Bend one leg at a time at a slow pace.
- In the same position, alternately move one leg to the side, sliding along the floor.
- Lying on your back, raise your head 45 degrees and hold in this position for eight seconds.
- Perform the “bicycle” exercise, raising your legs as high as possible.
- Alternately lift your legs 90 degrees.
Spinal stretch:
- Lie on your back, fold your arms along your body
. Bend your knees and pull your chests in, trying to reach your chin. Perform at a slow pace for up to ten seconds. - stand up
. Slowly tilt your head back and forth seven to eight times.
Perform each movement four to eight times. Before doing this, warm up in the form of light jogging for five minutes, bending and rotating to the sides and stretching the muscles of the limbs.
The group of exercises, as well as the number of approaches and repetitions, is determined individually, taking into account the characteristics of the disease, the cause of its occurrence and the stage of progression.
Exercises can be done only with stable pain relief.
During gymnastics, you need to pay attention to your own feelings. So, if severe pain occurs with sudden movements, it is necessary to repeat the exercise at a slower pace and with greater caution. If the pain syndrome recurs, it is necessary to temporarily exclude movement from the treatment and consult a doctor.
Physiotherapy
Physiotherapy is included as an additional therapeutic method in the package of measures. With its help, blood supply to the affected tissues is restored, lost functionality is partially restored, pain is relieved, and the progression of spondylosis is slowed down. The following methods are effective:
- phonophoresis;
- acupuncture;
- laser use;
- exposure to paraffin compounds;
- mud treatment;
- electrophoresis.
The selection of physiotherapy methods is also carried out on an individual basis. A separate point in correcting the spine is massage.
Surgical exposure
Surgery is a last resort in the fight against spondylosis and is used only if less radical methods do not improve the condition. During surgery, bone growths that affect nerve endings and cause pain are removed, and the spinal discs are realigned.
Traditional methods
Along with traditional methods of treatment, it is also possible to use folk recipes against spondylosis deformans. In this case, the following are effective:
- Compresses
. Lotions made from horseradish leaves, as well as using turpentine and vinegar, are effective. In liquids, it is enough to moisten a gauze pad and apply it to the sore area for seven to ten minutes. After this time, a slight burning sensation may occur. Horseradish will need to be crushed into a paste, placed on the painful area, covered with a woolen napkin and left for twelve hours. - Baths with medicinal decoctions
. For three liters of boiling water you will need to take three hundred grams of dry grass (pine needles, chamomile, birch leaves). Leave the solution for fifteen minutes, then pour it into the prepared hot bath, after straining. - Honey overload for oral administration
. Add a glass of liquid honey to three liters of juice and leave for two weeks to ferment. Drink three tablespoons of the finished product ten minutes before meals. - Rubbing
. Pour half a glass of grated radish pulp with the same amount of pure vodka, add two tablespoons of salt and a glass of liquid honey. Infuse the composition for seven days. Use for rubbing painful areas.
Rubbing can also be done using camphor oil. However, it is important to take measures to avoid damaging your clothes. The disease should be treated with warming agents carefully to avoid burns and allergies.
To achieve the best effect, it is recommended to perform the procedures immediately before bedtime.
General recommendations and diet
When treating spondylosis, the diet and quality of nutrition are important. It is recommended to include fruits and vegetables (especially pickled ones), cottage cheese and butter (with a small amount of table salt) in the diet. It is advisable to reduce the consumption of vegetable oil; dressing salads with vinegar is beneficial. Jellies and aspic, cartilage, and marmalade are of particular importance in the diet.
It is important to take precautions when visiting chiropractors. You should use the services of only trusted specialists. Excessive stress on the spine is prohibited.
Drug therapy
To begin physical therapy, you must first get rid of pain and eliminate inflammation of damaged nerve fiber endings. Anti-inflammatory drugs are widely used for this. They are helping:
- eliminate painful sensations;
- reduce swelling;
- eliminate inflammation.
To achieve a better effect of therapy, chondroprotectors can be additionally prescribed, which help restore cartilage tissue and drugs that improve blood circulation.
Physiotherapeutic procedures
Vacuum therapy. This is a special massage technique that uses cans of various sizes. The procedures are done two weeks every other day for 15 minutes. They will help improve blood circulation and increase the functionality of the ligamentous apparatus.
Electrophoresis with Ionoson. The events are carried out in a course of 15 procedures. Medications are injected through the surface of the skin using galvanic current.
Heat treatment. Thermotherapy will help remove waste products from the body, activate metabolic processes, improve muscle functionality, and reduce discomfort.
You may be interested in: How to treat lumbar protrusion
Magnetotherapy. The number of procedures depends on the severity of the disease. The treatment course is 100 or 200 minutes, they are divided into 10 sessions. The procedures are carried out 1-2 times a day. They speed up recovery processes and eliminate pain.
Hirudotherapy. Treatment with leeches is effective; 5-7 procedures of 10-30 minutes are prescribed. The procedures can eliminate the painful symptoms of spondylosis and improve the patient’s condition.
Mud therapy. To achieve a healing effect, you need to carry out 10 procedures for 30 minutes. Treatments with therapeutic mud activate the outflow of lymph in muscle tissue, relieving muscle tightness.
Phonophoresis. Medications are administered using ultrasound. They stop inflammatory processes and improve blood circulation. A course of 12-15 procedures of 10 minutes each is required.
Physiotherapeutic techniques
One of the most effective methods of combating the formation and progression of spondylosis is considered to be specially selected gymnastics. Additionally, you can include massages. Such activities help reduce pain and restore motor activity of the spinal column.
Gymnastics involves carrying out special exercises aimed at strengthening a weakened muscle corset and subsequently improving the mobility of the vertebrae.
Important! If you have spondylosis, you should not bend your lower back excessively or throw your head back too far.
Gymnastics, combined with drug therapy, can significantly strengthen muscles and reduce the likelihood of spinal column deformity.
Acupuncture is widely used in combination with conventional physiotherapy techniques. This technique allows you to very quickly get rid of pain and discomfort expressed in the painful condition of the spinal column. Acupuncture allows you to quickly relieve an acute attack of pain, and easily eliminate the pinching of nerve fiber endings that occurs as a result of the inflammatory process.
Occurrence and development of the disease
With age, intervertebral fluid becomes less, vertebral discs wear out, and joints wear out. This occurs due to a slowdown in metabolism in bone tissue, which causes fewer mineral components in the spine. Calcium is deposited in the intervertebral discs and their cartilage becomes stiffer, losing its elasticity. Calcium also accumulates in connective tissues, making them less flexible, causing disorders in the human musculoskeletal system.
As the disease progresses, osteophytes grow, making the spinal column less and less mobile and, thereby, depriving a person of the ability to make full movements.
Spondylosis of the lumbar spine can be caused by the following factors:
- Metabolic disorders, when calcium salts, supplied in excess, are stored in the cracks between the joints, forming osteophytes there;
- Excessive inertial load on the lower back, caused by prolonged exposure to a position that is unnatural for the spine;
- Strength loads, for example, lifting weights, in the absence of constant training;
- Previous injuries and damage to the lumbar and sacral spine;
- A person’s predisposition to such diseases due to constitutional characteristics or heredity;
- Physical inactivity, as a result of which the ligaments and muscles of the lumbar spine atrophy, destruction of joint tissue occurs;
- Deformation of bone composition that occurs due to age;
- Various tumors and past diseases caused by infections.
Prevention
With spondylosis, doctors advise you to adhere to absolutely all instructions and recommendations, since only in this way is it possible to quickly eliminate the disease and return to a full life.
Since this disease belongs to the category of inflammatory processes, care must be taken to ensure that the body does not become overcooled at all, especially in the winter season. As a result of excessive weight, the load placed on a person's spine can increase significantly, which is why a special diet must be used.
It is imperative to constantly engage in specially selected gymnastics, excluding only lifting excessively heavy objects. Since spondylosis is a chronic pathology, you need to periodically visit a doctor to conduct a thorough examination of the condition of the spinal column.
Causes of spondylosis development
The causes of deforming lumbar spondylosis are:
- Dynamic loads are physical tension of the muscles that surround the spine, against the background of severe physical inactivity.
- Static loads - staying in one uncomfortable position for too long.
- Traumatic injuries to the muscles and ligaments of the spine in the sacral and lumbar regions.
- Age-related changes in the tissues of the spinal column.
- Hereditary and constitutional predisposition.
- Infectious tumors and diseases.
Why does spondylosis deformans occur?
Deformations that have formed due to an increase in the size of bone tissue are indicative of this disease. The growing bone structures acquire hypertrophied sizes, causing muscle spasm (tightening), restriction of movements in the lumbar area and its transition to the sacrum.
Spondylosis
Important! If the onset of the disease is not treated, the bone growths increase in size, giving rise to osteophytic formations. Their serious size causes severe pain, affecting and damaging nerve endings and even spinal cord tissue.
Increased pain in developing spondylosis is also accompanied by loss of moisture from the tissues of the intervertebral discs, which goes into the cracks of the fibrous ring. Because of this, they shrink, lose height, and the spine deforms even more.
If we name the main cause of spondylosis, it will sound like this - this is the “response” of the spine to excessive load placed on the vertebral bodies. In turn, the load can be caused by many factors.
Painkillers
Table. Causes of spondylosis.
| Cause | Description |
| The very first and most common cause is injury to the ligaments or muscles located in the lower spinal regions. Sometimes even microtrauma is enough to “trigger” the mechanism of spondylosis. |
| Heavy physical labor requiring the participation of the lumbar region (lifting or carrying heavy objects), or vigorous physical activity. |
| The opposite of the previous named condition, in which the muscles are inactive, remain static for a long time, and freeze in an uncomfortable or incorrect position. |
| We are talking about a sudden strong tension of untrained or unprepared muscles. |
| Genetic weakness of cartilage structures, which is inherited often together with the fragility of the musculoskeletal system. |
| The age factor entails numerous changes, including in vertebral tissues, causing their weakening and deformation. |
| Frequent infectious lesions affect the integrity of all tissue structures of the body, not excluding vertebrates. |
| If the focus of cancer is in close proximity to the spinal area, the tumor-like formation, growing, can mechanically affect the tissues of the spine, damaging them. |
“Relationships” with osteochondrosis
There is a medical theory according to which osteochondrosis becomes a harbinger and “provocateur” of deforming spondylosis of the lumbar region. In cases of osteochondrosis, degeneration affects the entire fibrous ring, both from the inside and outside (while in spondylosis - only from the outside). But ring ruptures are identical, and they also lead to an increase in the mobility of the vertebral segments, their shifting, displacement, and deformation. In its fourth stage, osteochondrosis forms the same growths of bone tissue that are characteristic of deforming spondylosis.
Osteochondrosis of the lumbar region
By the way. True, if experts who claim that these two diseases are equal, and neither follows from the other. With the wider spread of osteochondrosis, it is worth noting that the first pain that the patient pays attention to is caused by spondylosis.
Both diseases in combination, and each separately, can develop into lumbar radiculitis. With it, pain begins to spread from the lumbar area to the sacral, coccygeal, gluteal, and also affects the femoral areas and legs.
The essence of the disease
The reasons for the development of spondylosis deformans have not been fully established. Some scientists consider the pathology as a destructive dystrophic lesion of the lumbar region, others - that the disease occurs due to a single injury or multiple repeated microtraumas of the longitudinal ligaments against the background of protrusion of the fibrous rings of the intervertebral discs. The rings lose their ability to withstand the pressure of the pulpy kernels. When exposed to significant loads, they bend and detach the longitudinal ligaments from the areas of their connection with the surfaces of the lumbar vertebral bodies. Factors that provoke the development of spondylosis deformans include:
- elderly and senile age;
- severe acute or chronic diseases of the joints and pathologies of internal organs;
- excess body weight;
- serious sports or professional physical activity;
- spinal injury - severe bruises, fractures, prolonged compression.
Osteophytes.
After the longitudinal ligaments are torn off, a slight hemorrhage occurs, and then a growth of bone tissue gradually forms. Repeated injury causes a new detachment with the formation of an osteophyte. At the same time, the size of the vertebrae does not change for a long time, and there is no decrease in their functional activity. This explains the long asymptomatic course of the disease. What happens as the pathological process progresses:
- bone growths compress the anterior longitudinal ligaments;
- mobility of the anterior spinal column is limited;
- in some cases, the intervertebral foramina narrows.
When conducting research, it was found that the development of pathology can be provoked by diseases occurring against the background of metabolic disorders. For example, gout, in which crystals of uric acid salts are deposited in bone and joint tissues, ligaments, and tendons.
The formation of osteophytes changes the anatomical structure of the anterior spinal column. Doctors consider the formation of bone growths to be a protective adaptive reaction of the body. In this way he tries to stabilize the spinal column. The presence of marginal bone growths prevents the deformed vertebrae from moving.
Degrees of spondylosis
The growths develop gradually over several years. Therefore, in the initial stages, a person does not even notice any changes. The disease is usually divided into 3 stages:
- First . The patient begins to complain of minor lower back pain, which may disappear without taking medication. Speaking about the mobility of the spine, slight stiffness is felt. At the initial stage, spondylosis can be regarded as the body’s response to static overstrain in the lower back. At the same time, muscle spasms are often observed.
- Second . If treatment is not started, a pathological process develops. This means that the area of contact between the bones gradually increases. At this stage of the disease, the patient may suffer from pinched nerve roots and sometimes the spinal cord.
- At the third stage of development of the disease, the intervertebral disc loses its elasticity due to dehydration. The height of the disc decreases, which causes severe pain. Speaking of the intervertebral disc, it becomes almost invisible and overgrown with bone tissue on all sides.
Stages of spondylosis