Interstitial nephritis occurs before the age of 50 years, the inflammatory process in the immune system destroys the loose connective structure of the renal tissue, and the nephron canal system is affected. With this disease, there are no changes in the renal sinus, where the final urine is excreted. The main filter in the human body is the kidneys. Reproducing the metabolism of proteins and carbohydrates, maintaining the balance of water and salt in the body, normalizing hormonal levels and secreting the necessary enzymes is the merit of this organ. The slightest violation of one link leads to a chain of problems. There are various forms of this disease, they differ in the course and mechanism of development of the process and the causes of its occurrence.
The mechanisms of formation of the interstitial form of nephritis are antibody and immune complex. The antibody mechanism develops during penicillin intoxication and crisis, which is expressed by transplant rejection. Immune complex development is preceded by systemic lupus erythematosus, long-term NSAID therapy and lymphoproliferative syndrome.
Inflammatory edema and vascular spasm form in the kidney tissues, leading to ischemia and narrowing of the tubules, inside which the pressure increases. The flow of ions through the organ decreases, and the creatinine index increases. If ischemic kidney disease is pronounced, then the risk of developing papillary necrosis increases, which is accompanied by a large amount of blood in the urea.
Basic information about the disease
So, interstitial nephritis is an inflammatory pathology of the kidneys, which is of a non-infectious abacterial nature. In the presence of this disease, pathological processes occur in interstitial tissues and affect the tubular apparatus of the nephrons.
This disease is considered an independent nosological form. It differs from pyelonephritis, first of all, in that in the presence of pathology, any destructive changes in the renal tissues do not occur, that is, the process of inflammation does not spread to the area of the calyces and pelvis.
Interstitial nephritis (ICD 10 N 11.0) can appear at absolutely any age. It can even occur in newborns or elderly patients. But most often this disease is registered in the age category from twenty to fifty years. The clinical picture of interstitial nephritis is characterized by a decrease in the functionality and performance of the renal tubules; therefore, the presented pathology can be called tubulointerstitial nephritis or tubulointerstitial nephropathy.
Pathogenesis
The development of acute interstitial nephritis is associated with the entry into the blood of a toxic product or bacterial toxin, which, when reabsorbed by the tubules, damages the tubular basement membrane. After reabsorption, antigenic substances cause an immunological reaction with the fixation of immune complexes in the interstitial tissue and the wall of the tubules. Immune inflammation and allergic edema develop in the interstitium. The inflammatory process in the interstitium leads to compression of the tubules and vessels. Intratubular pressure increases and, as a consequence, a drop in effective filtration pressure in the glomeruli of the kidneys.
A reflex vascular spasm and ischemia of the renal tissue develop, and a decrease in renal blood flow. The glomerular apparatus is initially relatively intact. As a result of a decrease in intraglomerular blood flow, a drop in glomerular filtration occurs, which causes an increase in the concentration of creatinine in the blood serum. Interstitial edema and tubular damage, leading to a decrease in water reabsorption, causes polyuria and hyposthenuria, despite a decrease in glomerular filtrate. Impaired tubular function leads to electrolyte shifts, the development of tubular acidosis, and impaired protein reabsorption, manifested by proteinuria.
Morphology of interstitial nephritis. Light microscopy depends on the severity of the process. There are three stages of development - edematous, cellular infiltration and tubulo-necrotic.
The edematous stage is characterized by swelling of the interstitium with minor cellular infiltration. At the cellular stage, there is pronounced infiltration of the kidney stroma with lymphocytes and macrophages, less commonly a variant with a predominance of plasma cells and eosinophils. In the 3rd stage, necrotic changes in the tubular epithelium are determined.
The distal nephron and collecting ducts are mainly affected. Features of the morphological picture in children include a significant frequency of signs of glomerular immaturity, their hyalinosis and insufficient differentiation of the tubules.
Electron microscopy reveals nonspecific changes in the tubular apparatus. Research using monoclonal sera allows us to identify T-lymphocytes CD4 and CD8.
In a number of patients, severe ischemia of the papillary zone can provoke the development of papillary necrosis with massive hematuria.
Electrolyte disturbances in acute interstitial nephritis are reduced to increased excretion of sodium and potassium. Functional kidney disorders are characterized by a decrease in the secretory and excretory function of the tubules, a decrease in the optical density of urine, titratable acidity and ammonia excretion in the urine.
[24], [25], [26], [27], [28], [29]
Acute and chronic form of the disease
Acute interstitial nephritis usually manifests itself as inflammatory changes in interstitial tissues. In more severe cases, this process can provoke the development of kidney failure. True, this disease has a predominantly favorable prognosis.
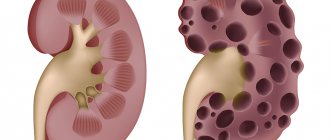
Chronic interstitial nephritis is characterized by fibrosis of interstitial tissues, damage to the renal glomeruli, and in addition, tubular atrophy. The chronic type of the disease leads to nephrosclerosis. This form of the disease can cause chronic kidney failure.
Interstitial nephritis occurs in children.
According to the development mechanism, the following forms are distinguished:
- Primary. In this case, the pathological process develops in the renal tissue independently, and not against the background of another disease.
- Secondary. It develops against the background of an existing kidney disease and significantly complicates its course. It can also develop due to the presence of leukemia, diabetes, gout and other diseases in the body.
Features of the course of the disease in children
Interstitial nephritis occurs quite often in children. It can even occur in newborns who are diagnosed with nephropathies. In most clinical cases, the diagnosis was confirmed in premature babies. As a rule, their illness develops as a reaction of the body to a toxic or hypoxic effect.
In children, the first sign of the disease is the appearance of edema. Polyuria then develops. There is an increase in creatinine and urea levels in the blood. In almost all cases, the disease in children is diagnosed in the acute period. But there have been cases when the disease took a chronic course. This was due to incorrect and untimely treatment.
Main causes of pathology
The main causes of this disease include a number of different factors, for example:
- Use for the treatment of all kinds of drugs. We are talking about antibiotics, fluoroquinolones, non-steroidal drugs, sulfonamides, diuretics, for example, the use of Penicillin, Ampicillin, Cephalothin, Gentamicin, Ibuprofen, Captopril, Naproxen and so on.
- Past infectious pathologies that are caused by various bacteria, for example, streptococcus or diphtheria.
- Previous illnesses caused by viruses, for example, cytomegalovirus or hemorrhagic fever.
- The presence of diseases of the immune system, for example, the development of systemic lupus erythematosus.
- Development of myeloma.
- Poisoning with heavy metals, for example, lead, mercury, cadmium and the like.
- Metabolic disorder in humans.
If the underlying cause of interstitial nephritis remains unclear, it is called idiopathic. Now let's find out what symptoms accompany this disease.
Why does it occur
Acute tubulointerstitial nephritis can occur due to various causes.
Quite often it becomes a consequence of taking certain drugs, especially antibiotics such as Rifampicin, aminoglycosides, and cephalosporins.
Pathology can also arise due to:
- analgesics;
- non-steroidal anti-inflammatory drugs;
- immunosuppressants;
- sulfonamides;
- Allopurinol;
- diuretics;
- barbiturates.
There have been recorded cases of the development of nephritis as a result of the use of radiopaque agents, certain chemicals, ethyl alcohol, etc. This phenomenon occurs in cases where a person is prone to allergies or has sensitivity to one of the components. Other reasons include:
- radiation exposure;
- poisoning by poisons of various origins;
- infectious (viral or bacterial) diseases that a person has suffered seriously;
- urinary tract obstruction (when the prostate, colon and bladder contain tumors);
- some systemic diseases: lupus erythematosus, scleroderma.
In children, nephritis may occur after vaccination. There are a number of cases when doctors are unable to fully understand the cause of the development of pathology.
Symptoms of the disease
The clinical symptoms of interstitial nephritis directly depend on the degree of intoxication, and in addition, on the level of intensity of the disease. Symptoms of the acute form of this pathology usually appear three days after the onset of infectious diseases, such as, for example, tonsillitis, tonsillitis, influenza, sinusitis, and so on. Symptoms may also appear after the use of antibiotics, medicinal serums and diuretics.
Most often, against the background of chronic interstitial nephritis, patients experience weakness along with lethargy, loss of appetite, nausea or vomiting. Often, all these symptoms can be accompanied by an increase in body temperature. Muscle pain, an allergic skin rash, and also a slight increase in blood pressure are also possible.
The acute form of interstitial nephritis is not characterized by impaired urination and swelling does not occur. Only in extremely severe cases of this disease, patients may experience a decrease in the amount of urine they receive. This can occur until the complete cessation of urinary flow, thus developing anuria.
The symptoms of interstitial nephritis are very unpleasant.
From the first days, patients may also develop renal failure of varying severity, however, with adequate treatment, these manifestations are completely reversible. They usually go away after a couple of weeks. The concentration functions of the kidneys most often return to normal after three months.
Symptoms of interstitial nephritis also depend on the form of the disease.
Features of tubulointerstitial nephritis in childhood
In children, acute nephritis occurs most often while taking medications. The chronic form is caused either by congenital disorders or metabolic disorders.
The acute form in children manifests itself clearly - pain in the abdomen and lower back, lethargy, nausea, headaches, and a sharp loss of strength. Urine with sediment, cloudy, with blood. The child urinates frequently; oliguria usually does not occur in children. With proper treatment, symptoms disappear completely after 2-3 weeks. In case of acute inflammation, the child needs strict bed rest. The principles of therapy are the same as for adult patients:
- discontinuation of the drug that caused nephritis;
- prescription of drugs to improve renal hemodynamics (Trental, Eufillin, Rutin);
- relieving edema of interstitial tissue using diuretics;
- use of antioxidants and antihistamines;
- normalization of metabolic processes - ATP, cocorboxylase are prescribed;
- elimination of electrolyte disturbances (introduction of saline solutions).
In severe cases, in the absence of positive dynamics within 2–3 days from the start of therapy, corticosteroids are indicated.
In the acute period of tubulointerstitial nephritis, the child is prescribed bed rest to reduce the load on the filtering function of the kidneys
The chronic form of the disease in children, like adults, is asymptomatic in the first stages. Young patients may experience increased fatigue, weakness, and loss of appetite. Progressive tubular disorders lead to loss of renal concentrating ability. Polyuria is accompanied by severe thirst, the development of the disease is manifested by dry and pale skin, and a tendency to allergic rashes.
Renal calcium acidosis increases and leads to the gradual development of muscular dystonia, osteodystrophy (pathological changes in bone tissue). A sick child begins to lag significantly in growth, bone tissue becomes fragile, which is fraught with pathological fractures. The “salt-losing kidney” syndrome is manifested by hypotension up to collapse (a decrease in pressure to critical levels and a sharp disruption of the blood supply to vital organs). Sclerosis of the renal structures leads to symptoms of severe renal failure.
Long-term course of chronic tubulointerstitial nephritis in children leads to degenerative changes in bone tissue
In the treatment of chronic forms of pathology in children, the following drugs are used:
- vitamins and antioxidants to stabilize the membranes of cellular structures;
- products that improve microcirculation;
- coenzymes to normalize metabolism (Phosphaden, lipoic acid, Carnitine, Lipamide);
- anti-sclerotic to prevent fibrotic degeneration of renal structures (Plaquenil, Chloroquine).
Iontophoresis procedures for the kidney area with Lidaza and Aloe are recommended.
A sick child needs a diet, limited exercise, prevention of hypothermia, clinical observation, sanatorium-resort treatment and timely treatment of general and kidney infections.
Forms of the disease
In addition to the main forms of the disease (acute and chronic), this pathology is further divided into the following four types:
- Development of an extensive form of interstitial nephritis. In this case, the patient exhibits all the clinical symptoms of the disease.
- Against the background of a severe form, manifestations of acute kidney failure along with prolonged anuria may occur.
- With the development of the abortive form, patients do not have anuria, and, in addition, a favorable course of the disease is observed along with a rapid restoration of kidney function.
- With the development of the focal form, mild clinical symptoms of interstitial nephritis are observed. Polyuria may occur, which will result in excessive urine production. This type of disease has a favorable course, with patients recovering quickly.
It should be noted that chronic nephritis differs from the acute form in that it has a more unfavorable course. In the later stages of the disease, changes in the functioning of the kidneys are noted, and glomerulosclerosis develops. In this case, the development of chronic kidney failure is also possible.
Among the symptoms of interstitial nephritis in adults, wave fever is often observed along with an allergic itchy rash, lumbar pain, anuria or polyuria, dry mouth and thirst, increased blood pressure and anemia. The development of glomerulosclerosis can lead to swelling and proteinuria. The prognosis for treatment of chronic interstitial nephritis directly depends on the rate of development of kidney failure. In addition, the prognosis depends on the degree of damage to the renal tangles.
Types of jade
Acute nephritis is characterized by sharp manifestations of symptoms, a rapid decrease in the performance and functioning of the renal system. Accompanied by micro-blood clots in the urine, temperature and pain in the lumbar area.
Chronic nephritis is an extreme stage of the disease in which the tubules die at the site of urine formation. With fibrosis, the kidney is compressed, both ureters and vessels in the renal system are blocked, and glomerular filtration is impaired. The end result will be the suspension of kidney function and the death of the tubules.
Mechanisms of nephrotoxicity in the presence of an acute form
Experts identify five mechanisms of nephrotoxicity in the development of acute interstitial nephritis:
- The process of redistribution of renal blood flow along with its decrease.
- Development of ischemic damage to glomerular and tubular basement membranes.
- The occurrence of a delayed hypersensitivity reaction.
- The process of direct damage to tubular cells through enzymes in the presence of anoxia.
- Development of selective cumulation in the kidneys.
The nature of tubular dysfunction can vary greatly depending on the location of the lesion.
Recommendations for interstitial nephritis will be given below.
Causes of acute interstitial nephritis
Most experts consider interstitial nephritis as the most severe renal reaction in the chain of general body reactions to drug administration. Among the medications for the development of acute interstitial nephritis, the following are important: antibiotics (penicillin, ampicillin, gentamicin, cephalosporins); sulfa drugs; non-steroidal anti-inflammatory drugs; barbiturates; analgesics (analgin, amidopyrine); preparations containing lithium, gold; cytostatics (azathioprine, cyclosporine); salts of heavy metals - lead, cadmium, mercury; radiation intoxication; administration of serums, vaccines.
It is not so much the dose of the drug that matters, but the duration of its use and increased sensitivity to it.
It has been established that immune inflammation and allergic edema develop in the interstitial tissue of the renal medulla.
Acute interstitial nephritis can also be observed with infections such as hepatitis, leptospirosis, infectious mononucleosis, diphtheria, as well as with shock and burns.
[18], [19], [20], [21], [22], [23]
Diagnosis of this pathology
As part of the diagnosis of this disease, the following methods of examining the patient are taken:
- Carrying out an analysis of the patient’s complaints along with collecting an anamnesis of the disease.
- A general blood test.
- Carrying out a biochemical analysis of urine.
- Taking the Zimnitsky and Roberg sample.
- Conducting a serological study.
- Performing a study to determine specific microglobulins present in the urine.
- Conducting urine culture to identify and determine bacteria.
- Performing an ultrasound examination of the kidneys.
- Taking a kidney biopsy.
In addition to the above research methods, other diagnostic methods can be performed at the discretion of the attending physician.
Diagnostic methods
When examined by a doctor, first of all, the patient should tell about the health problems that could cause such negative consequences. The most accurate diagnostic method that can indicate pathological changes in the structure of the kidneys is ultrasound. It makes it possible to assess the condition of the glomeruli and tubules.
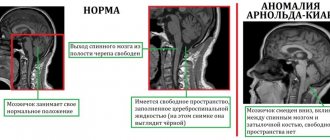
More accurate data are obtained from CT or MRI. Such diagnostic methods are the most modern and informative today. With their help, you can assess the condition of the kidneys even at the cellular level. Acute tubulointerstitial nephritis is also diagnosed by other methods, in particular:
- urine culture - needed to identify bacterial content of urine in the laboratory;
- Zimnitsky's test is one of the laboratory methods that makes it possible to assess whether the kidneys are capable of concentrating urine;
- Reberg's test - an analysis that makes it possible to find out how successfully the kidneys can cope with their main function - excretory, whether the renal tubules can absorb useful substances;
- biopsy - involves taking a small piece of kidney tissue for further research in the laboratory;
- serological study - an autoimmune type analysis, the purpose of which is to identify antibodies to the structural parts of the urinary system in the patient’s blood;
- detection of b2-microglobulin in the patient’s blood - normally it should be completely absent, its presence indicates damage to the kidney framework;
- biochemical blood test;
- general blood test;
- urine test.
Differential diagnosis helps to distinguish the acute type of tubulointerstitial nephritis from acute renal failure and diffuse. In the case of a chronic course of the disease, its undulation and the concentration of uric acid in urine and blood are taken into account.
Treatment of the disease
Early diagnosis is extremely important for the treatment of interstitial nephritis, along with the abolition of medications that provoke the development of this disease. If possible, the number of drugs used should be reduced, replacing them with nephrotoxic agents and non-toxic drugs. Against the background of polyuria, the volume of fluid consumed should be increased, and with oliguria, on the contrary, reduced. Patients with oligoanuria are prescribed hemodialysis, which helps restore kidney function. If necessary, a short course of glucocorticoid treatment is carried out, and in addition, cytostatics are used.
The prognosis for treatment of acute interstitial nephritis is usually favorable. The immediate recovery of patients occurs within a few weeks; in extreme cases, it takes a couple of months. Against the background of slow recovery of kidney function and prolonged anuria, acute interstitial nephritis can become chronic.
The development of a chronic form of the disease necessarily requires restoration of the patient's water and electrolyte metabolism. Among other things, measures are being taken to eliminate the causes of interstitial damage. Therapy is also aimed at normalizing the functions of the urinary tract. In addition, therapy is carried out aimed at treating chronic kidney failure.
Clinical guidelines for interstitial nephritis should be strictly followed.
Disease treatment program
Treatment of such a problem should be aimed at eliminating provoking factors and restoring renal function. Thus, therapy is carried out according to the following scheme:
- Exclusion of cause-and-effect factors causing the development of the chronic nature of the disease. To do this, you should completely discontinue the medications that caused the pathological processes.
- If there are no symptoms of chronic pyelonephritis, then patients are prescribed a physiologically complete diet that can provide the sick person with the necessary amount of carbohydrates, proteins, fats and, of course, vitamins. It is equally important to limit the patient’s consumption of table salt. This is especially advisable in the presence of high blood pressure.
- Carrying out symptomatic treatment of interstitial nephritis. Such therapy should include the use of a medicine called Enalapril. This drug can have a beneficial effect on renal hemodynamics, thanks to which the level of proteinuria is reduced.
- It is also necessary to prescribe steroid hormones. This is especially true if nephritis begins to progress rapidly or has an extremely severe course.
- Correcting low levels of sodium and potassium in the body as a result of urinating too frequently.
- The use of medications that improve microcirculation. For example, in this case, patients should be prescribed drugs in the form of “Curantil” and “Troxevasin”.
Symptoms of kidney inflammation in a child
May 6, 2020 Doctor
Inflammation of the kidneys is a fairly common disease in children, which can be caused by family history, a weak immune system, or simple hypothermia. Due to physiology, girls are more often susceptible to inflammatory disease, since their urethra is shorter and wider, which is a favorable condition for the entry of pathogenic bacteria.
The disease is divided into several types:
- primary and secondary;
- unilateral and bilateral;
- acute or chronic.
In medical practice, several forms of kidney inflammation are identified:
- pyelonephritis;
- glomerulonephritis;
- interstitial nephritis.
Causes
The inflammatory process of the urinary system (nephritis) can develop for a variety of reasons. Children in the age group from 3 to 7 years are at risk. Nephritis can act as a primary or concomitant disease. Very often it develops against the background of hypothermia or as a concomitant illness with acute respiratory infections, sore throat, and various infections. The risk of developing inflammation increases if the baby suffers from chronic diseases (diabetes mellitus or tonsillitis).
The main reasons for the development of nephritis:
- genetic predisposition;
- weakness of the immune system;
- the presence of concomitant infectious processes;
- autoimmune disorders;
- hypothermia;
- allergy;
- complications after suffering from acute respiratory viral infections, tonsillitis and other diseases of the upper respiratory tract;
- previous skin diseases;
- previous scarlet fever;
- the presence of a bacterial infection that affects the kidneys through the urinary tract (coccal infection, E. coli, etc.).
Most often, kidney inflammation is a consequence of an infection, that is, a peculiar reaction of the body to the activity of pathogenic microflora. Due to this process, the functionality of the kidneys is impaired, the nature and process of urine outflow changes. The fundamental factors for the development of nephritis can be called:
- presence of chronic diseases;
- decreased normal blood supply to the kidneys;
- physiological abnormalities in the structure of the organs of the urinary system;
- failure to comply with personal hygiene rules (especially in girls);
- disordered eating.
Clinical picture
Children of any age can suffer from nephritis. Often the inflammatory process is asymptomatic, the blurred clinical picture and the difference in the symptoms that appear make diagnosis difficult.
Common symptoms of nephritis:
- pain in the lumbar region;
- a sharp increase in temperature to high values;
- disturbance of the urination process.
As inflammation develops, the following signs may appear:
- heaviness in the sides and back;
- change in the character of urine (turbidity);
- swelling of the skin, which manifests itself more after sleep;
- weakness, apathy;
- intoxication of the body;
- pallor and cyanosis of the skin and mucous membranes;
- sleep disturbance;
- lack of appetite.
Infants are also susceptible to developing an inflammatory disease, since due to their age they cannot indicate a painful ailment. Parents should be alert to the following behavior changes in their infants:
- tearfulness;
- refusal to go to the toilet because the baby experiences pain when urinating;
- grunting or redness during urination;
- frequent regurgitation;
- a significant increase in temperature levels;
- sleep disturbance;
- the appearance of foam, clots or other foreign impurities in the urine.
Individual symptoms may indicate the presence of a certain form of inflammatory process. For example, with pyelonephritis, children suffer from frequent regurgitation, nausea, often vomiting, acute and paroxysmal pain. With glomerulonephritis, swelling appears, blood pressure increases, and laboratory tests of urine reveal the presence of protein and blood.
The appearance of at least one of the above signs in a child is a good reason for an emergency visit to the doctor. Self-medication or inadequate treatment of the inflammatory process can lead to serious complications.
Diagnostics
A number of diagnostic methods are used to confirm the diagnosis:
- visual examination of a small patient;
- collecting the necessary medical history (blood, urine);
- measuring body temperature;
- blood pressure measurement;
- palpation in the kidney area.
To make a more accurate diagnosis, the following is carried out:
- Ultrasound of the kidneys.
- CT or MRI.
After receiving the results of the study, the doctor determines the method of therapy.
Treatment
Treatment of mild forms of nephritis is allowed at home; in all other cases, the child is placed in a hospital. The main goal of therapy is to eliminate the inflammatory process, normalize kidney function, stimulate regenerative processes, and also prevent possible complications.
Drug therapy
Medicines are prescribed by the doctor in each case individually. The basis of therapy includes the use of the following medications:
- Antibacterial drugs (Augmentin, Ceftriaxone) - suppression of bacterial activity and treatment of infection that provoked the inflammatory process.
- Diuretics (Furosemide) - normalization of kidney function, washing out infectious agents. In case of increased swelling, diuretics are not recommended.
- Anti-inflammatory drugs (Ibuprofen, Nurofen) - relief of general symptoms of the disease - fever, acute headache, chills, etc.
- Antihistamines (Suprastin) - removal or reduction of allergic manifestations when treated with basic medications.
- Immunostimulating drugs (Viferon) - enhancing the effectiveness of prescribed therapy.
Proper nutrition
One of the signs of the inflammatory process is loss of appetite, as well as nausea and vomiting. In order not to aggravate the painful situation, the child’s usual diet should be changed.
- Strictly limit the consumption of salty foods, fatty and smoked foods.
- Limit consumption of canned foods, herbs, and spices.
- Increase the volume of fluid consumed (clean water). If there are no allergic reactions, then cranberry juice can be introduced into the diet. The berry has a number of medicinal properties - bactericidal, anti-inflammatory, immunostimulating.
Prophylaxis of this pathology
As part of the prevention of this disease, it is advisable to follow the following recommendations:
- Drinking plenty of fluids.
- Complete avoidance of long-term use of medications that are potentially harmful to the kidneys.
- Conducting regular urine tests.
- Implementation of sanitation of any chronic foci of infection.
- It is very important to try to avoid hypothermia. Thus, compliance with the thermal regime is necessary.
- It is very important to conduct a urine test against the background of each disease. Among other things, this should be done before and after various preventive vaccinations.
- A person must monitor the condition of his body and avoid excessive fatigue and frequent fatigue. Therefore, excessive exercise should be avoided.
In the event of any symptoms that may indicate the appearance of interstitial nephritis, it is necessary to urgently consult a physician, and also such specialists as a nephrologist or urologist. If treatment is not started in a timely manner, it may turn out to be ineffective, as a result of which all vital renal functions will be disrupted, while the development of failure of this organ cannot be ruled out, which means there is a direct threat to the patient’s life.
Preventive actions
To prevent kidney inflammation, doctors recommend following simple rules:
- Drink at least two liters of water throughout the day.
- Don't get too cold.
- Unnecessarily, do not take a lot of analgesics, antispasmodics and other synthetic drugs.
- Don't overexert yourself, especially when it comes to physical activity.
- Eliminate foci of infection in the body in a timely manner.
How long do people live with pathology? When the disease is detected at the initial stage and therapy is prescribed correctly, many patients are able to fully recover. Any changes in the urine test should be closely monitored. At the first suspicious signs, consult a urologist or nephrologist and undergo the necessary examination.
Interstitial nephritis is one of those diseases that is relatively easy to treat, but if untimely treatment can lead to coma and even death of a person. Today, specialists have in their arsenal a sufficient number of methods for accurately diagnosing the disease. If you consult a doctor in a timely manner, the prognosis is favorable.