Normal sternum shape and deviations
The chest is a shield that covers the internal organs. These include the heart and lungs, as well as large trunks of blood vessels. All these elements of the body must be closed and protected.
The normal shape of the chest is an irregular cone. It should have four sides.
Breast shapes are divided into several subtypes. They depend on the constitution of the person. The types of chest are divided into:
- Normosthenic – conical chest. The diameter of the anteroposterior sides should be less than the lateral one. This distinguishes the normosthenic form of the chest from other types. The spaces between the ribs are almost invisible. The shoulders are at an angle of 90 degrees relative to the neck. The muscles of the peri-shoulder zone are developed. All indicators of such a chest are normal,
Hypersthenic. Feature: cylindrical shape. The lateral and anteroposterior dimensions are almost equal. The size indicators in this case will be larger than the norm. A hypersthenic chest involves straight and broad shoulders, horizontally positioned ribs, with narrow gaps. The cylindrical chest is quite wide, the muscles are also quite developed.- Asthenic. An asthenic has a flat, narrow and slightly elongated sternum. The anteroposterior and lateral dimensions will be smaller than in any of the described types. The collarbones and the pits above and below them stand out well. The asthenic chest is characterized by very large intercostal spaces. The shoulders are usually drooped and the muscular system is weak.
Reasons for changes and their types
During the deformation of the chest, its shape changes, which has a negative impact on the functioning of internal organs - the heart, lungs.
In medicine, a distinction is made between congenital and acquired deformities.
Acquired deformity is a curvature of the shape of the chest due to some diseases, for example, diseases of the respiratory organs, rickets, bone tuberculosis. Burns in the chest area and various injuries can deform the sternum.
Acquired deformities are divided into the following types:
- Emphysematous - occur as a result of inflammatory processes in the lungs and respiratory tract, emphysema. In this case, the front part of the chest increases in size.
- Paralytic - a prerequisite for such a change is diseases of the lungs and pleura. The paralytic chest is characterized by reduced parameters.
- Scaphoid – boat-shaped indentations appear in the upper and middle parts of the chest. The scaphoid chest appears due to inflammatory processes in the spinal cord.
- Kyphoscoliotic - observed in cases of changes in the structure of the spine (asymmetry of the chest is formed, or a crooked spine appears).
The main reasons for such changes:
atrophied bone tissue,- changes in bones due to age,
- rupture of intervertebral discs,
- spinal fractures,
- neoplasms (tumors),
- damage, damage
- osteoporosis,
- deformation of the structure of the spine and vertebrae.
Congenital pathologies
Congenital chest deformity is the most common and dangerous phenomenon. Among the changes in this case, several types of deformations are distinguished:
- Funnel-shaped. Atypical costal cartilage or diaphragm can have a deforming effect. This type is characterized by the central part of the chest pressed towards the spine. This creates a funnel. This pathology reaches its greatest development by the child’s third birthday. If in the early stages it can be treated with gymnastics, then in the later stages only surgical intervention is used.
More than 20 types of operations are used in the world to correct this type of deformity. - Keel-shaped, or chicken-shaped. In this situation, the costal cartilage grows. This causes the sternum to move forward.
The shape of this deformation of the chest in a child resembles a keel. If this disrupts the functioning of internal organs (heart and lungs), then at the age of 5 years surgical treatment – thoracoplasty – is allowed. In the initial stages, chest deformity involves exercise, swimming, and the use of physical therapy. May occur as a result of rickets.
The following factors influence the development of the chest:
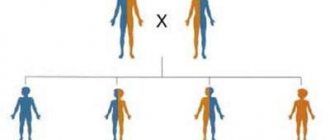
- Genetic predisposition - if one of your relatives has had such deformities, then there is a risk of passing them on as an “inheritance” to children, grandchildren and great-grandchildren,
- Developmental defects - if there are many developmental abnormalities, a child may develop a similar pathology.
Pectus excavatum (sunken chest)
This pathology is accompanied by noticeable retraction of individual zones. These are, in particular, the anterior parts of the ribs, cartilage or sternum. This is a fairly common developmental defect. Pectus excavatum often occurs due to the presence of serious genetic changes in the structure of cartilage and connective tissue.
Pectus excavatum (sunken chest) is by far the most common chest deformity and occurs in 1 in 400 newborns. Pectus carinatum, the second most common form of deformity, is 5 times less common than pectus excavatum.
There are several theories explaining the development of this deformity, but the etiology remains unclear. Some authors believe that the development of pectus excavatum may be associated with excessively rapid growth of the costal cartilage, which displaces the sternum posteriorly. Abnormalities of the diaphragm, rickets, or increased intrauterine pressure are also thought to contribute to posterior sternum displacement.
The frequent association of pectus excavatum with other diseases of the musculoskeletal system, such as Marfan syndrome, suggests that to a certain extent the deformity is caused by connective tissue abnormalities. Genetic determination also occurs in 40% of patients with carinatum deformity.
Pectus excavatum can appear either as a small defect or as a severe defect in which the sternum extends almost to the vertebrae. The occurrence of the defect is the result of 2 factors: (1) the degree of posterior angulation of the sternum and the degree of posterior angulation of the costal cartilage in the area of attachment of the ribs to the sternum.
Pectus excavatum usually occurs at birth or shortly after birth. The deformity often progresses, and the depth of the depression increases as the child grows. Sunken breasts are more common in men than women, with a ratio of 6:1 Sunken breasts can be associated with other congenital anomalies, including anomalies of the diaphragm.
There are several methods to quantify the severity of pectus excavatum deformity, which usually involves measuring the distance from the sternum to the spine. Perhaps the most commonly used method is the Haller method, which uses the ratio of transverse distance to anteroposterior distance derived from CT scans. In the Haller system, a score of 3.25 or higher indicates a severe defect that requires surgical intervention.
Pectus excavatum does not have much of a physiological effect on infants or children at all. Some children experience pain in the sternum or rib cartilage, especially after intense exercise. Other children may have palpitations, which may be due to mitral valve prolapse, which usually occurs in patients with sunken chests.
Sometimes asthma occurs in patients with pectus excavatum, but it is noted that the deformity does not have a clear effect on the clinical course of asthma. Funnel deformity affects the cardiovascular system and observations have shown that after surgical correction of the deformity there is a significant improvement in the functions of the cardiovascular system.
Dysplasia and risks of deformation
At the moment, medicine has come to the conclusion that pathological forms of the chest are a consequence of disturbances in the structure of the collagen protein. This causes connective tissue dysplasia and, as a result, chest deformation in children. Such changes are the external expression of dysplasia. But there are other dangers associated with this phenomenon.
After the chest, the next area at risk is the heart. To prevent negative consequences, an examination by a cardiologist is prescribed. When the very first signs of dysplasia appear, you should seek help from a doctor. Only a highly specialized specialist will prescribe effective treatment.
And only he knows how to correct this negative phenomenon. Typically, treatment for such a disease takes a long time. Both drug treatment and surgical intervention are carried out. Relapses are prevented with the help of medications.
Deformity is an abnormality in the development of the chest. There are a number of dangerous consequences of such changes. They relate to organs that are located in the frame:
- Respiratory. A sunken chest can lead to lung and breathing problems. Often the lungs become smaller and shrink.
- Cardiovascular. A severely deformed thoracic region leads to compression of the heart and provokes its displacement. Large blood vessels also undergo changes. In most cases, rapid heartbeat is observed and blood flow is impaired.
Such negative aspects of chest deformation also affect the overall development of children and adolescents. They become less active, physical health decreases, and surgical correction of the pathology is required. Most operations are performed after 7 years. But complications may arise after surgery. The most common are:
- hemothorax - blood begins to accumulate in the pleural cavity (lungs),
- processes of suppuration of the skin at the wound site,
pneumothorax – the lungs fill with air (in the pleura),- injuries under the skin contribute to the appearance of hematomas,
- pneumonia – often occurs after breast surgery,
- sepsis is an infection that spreads through the bloodstream,
- intestinal paresis - appears due to disturbances in water and electrolyte balance,
- inflammation of the heart muscle.
You must be prepared for all such consequences of deformation.
Because in most cases, pathological development of the chest is not just a cosmetic defect, but a serious disease.
Symptoms of keeled chest
Disturbances in any circulatory and respiratory functions do not make themselves felt at the birth of a child, but over time the chest begins to stretch anteriorly. In adolescence, patients complain of palpitations, frequent shortness of breath when playing sports, and fatigue when performing household chores.
During puberty, patients develop depression, increase in aggressiveness, and isolation due to dissimilarity with peers. Such dissimilarity from peers makes social adaptation difficult, because children are afraid that they will be ridiculed, teased, given bad labels and given nicknames.
During a detailed examination, the orthopedist reveals the following disorders due to narrowing of the chest: - decreased oxygen consumption coefficient - increased minute breathing volume - decreased vital capacity of the lungs
Features of the course of the disease at an early age
Modern specialists in traumatology identify only three of them:
- First degree. In this case, the depth of the funnel does not exceed 2 cm. In this case, no displacement of the heart is noted.
- Second degree. It is characterized by the following depth of the funnel: 2-4 cm. In this case, a displacement of the heart is noted (up to 3 cm).
- Third degree. In this case, the depth of the funnel is 4 cm or more. At the same time, the displacement of the heart exceeds 3 cm.
With subsequent development of the deformity, the chest becomes fixed. In this case, the depth of the funnel can increase to 8 cm. The child begins to develop scoliosis. In some cases, thoracic kyphosis appears. There is a decrease in respiratory excursion by approximately three to four times when compared with age norms.
There are serious disturbances in the functioning of the cardiovascular and respiratory systems. Many children suffering from this pathology are asthenic. In most cases, the vital capacity of the lungs is reduced by 30%. Manifestations of cardiac and respiratory failure are often observed. Gas exchange in the blood is very difficult. Children often complain of fatigue and chest pain.
Keeled chest classification according to ICD-10
Q 67.7 Keeled chest.
All possible variants of this pathology are divided into two main groups. As mentioned earlier, chest deformation can be either congenital (dysplastic) or acquired. The latter are much more common. Their development often occurs under the influence of the following factors:
- Bone tuberculosis.
- Scoliosis.
- Severe injuries and burns to certain areas of the sternum.
- Rickets.
- Chronic lung diseases.
Any deformity of the chest (congenital) implies the presence of serious anomalies or underdevelopment of the following areas:
- Blades.
- Sternum.
- Spine.
- Chest muscles.
- Ribs
The most severe chest deformity is less common. The reasons lie in the presence of a significant disturbance in the development of bone structures.
Diagnostics
Today there is a large stock of methods for studying disorders of the musculoskeletal system. One of the most common is radiography. It gives a complete picture of the disorders and, with the correct description of the images, can contribute to the effectiveness of treatment. Using radiography, you can obtain data on the degree and shape of the chest deformation.
Another instrumental method is CT scan of the sternum. It allows you to determine the degree of disorders that affect the heart and lungs, as well as the degree of displacement of internal organs. Along with CT, another hardware method is used - MRI. It provides complete and detailed information about bone and connective tissues, their condition and the degree of development of the disease. There are also additional methods that can describe the clinical picture. These include ECG, echocardiography and spirography. They make it possible to determine the condition of internal organs.
Carinatum deformity
Keeling deformity is the second most common congenital chest wall deformity. Pectus carinatum accounts for approximately 7% of all anterior chest wall deformities. It is more common in boys than girls (4:1 ratio). As a rule, this deformity is already present at birth and tends to progress as the child grows.
A keelbone deformity is a protrusion of the chest wall and is actually a spectrum of deformities that includes the costochondral cartilage and the sternum. Changes in osteochondral cartilage can be either unilateral or bilateral. In addition, bulging of the sternum can be either large or minor. The defect may be asymmetrical, causing rotation of the sternum with depression on one side and protrusion on the other side.
Etiology
The pathogenesis of keeled deformity, as well as funnel-shaped deformity, is not clear. It has been suggested that this is the result of excessive growth of the ribs or osteochondral cartilage. There is a certain genetic determination of keeled deformity. Thus, in 26% of cases, a family history of this form of deformity was noted.
Another type of thoracic deformity is keeled. It is also called rachitic. Symptoms of this pathology are a fairly noticeable protrusion of the chest part forward. This deformation can be compared to the keel of a ship. This visual defect is otherwise called “chicken breast.” Very often, such a pathology can relate to congenital forms of the disease.
- From 20 mm – mild;
- From 20 to 40 mm – average degree;
- From 40 mm and above – severe.
For the most part, the keeled deformity has a pronounced defect, due to which the child experiences discomfort, difficulties and a depressed, depressed state, which can greatly affect his psycho-emotional state.
Treatment options
Therapeutic tactics for chest pathology are determined based on the degree of deformation and existing dysfunction of vital organs. Some pathological conditions can be corrected using conservative treatment methods. Exercise therapy, massage, special gymnastics and physiotherapeutic procedures help with small funnel-shaped and keeled deformities of the chest.
With moderate and severe degrees of sternum deformation, the child needs surgical treatment. After the operation, normal function of the chest organs is restored.
The hypotonic muscle with keeled, pectus excavatum and other types of chest deformity reacts poorly to the dynamic load of the antagonist movements, which leads to compensatory hyperactivity of other muscles. With the help of special gymnastic exercises (see the video for more details), massage and physiotherapy, it is possible to solve this problem and prevent further deformation of the bones. Gymnastics normalizes breathing and helps restore the natural functions of internal organs.
The doctor may also prescribe hormonal medications, vitamin-mineral complexes and a special diet high in calcium and vitamin D to the small patient. This will strengthen the child’s musculoskeletal system in case of deformities caused by metabolic disorders.
In some cases, special corsets are used to eliminate pathology. Orthoses fix the chest in the correct position. Such devices must be worn for a long time. Their help is resorted to in case of slight curvature of the sternum.
If the deformation of the chest leads to aggravation of disturbances in the functioning of vital organs, this is a direct indication for surgery. Sometimes surgical correction is performed to eliminate a pronounced cosmetic defect.
In children, the chest is more elastic than in adults, so surgery is less traumatic for them. In total, there are more than 100 methods of surgical intervention for chest pathologies. Of these, operations are distinguished:
- with the introduction of implants;
- using clamps;
- with a 180 degree inversion of the sternum;
- without fixation.
Causes of acquired disorders
Why does acquired chest deformity appear in a child? The reasons that provoke it are listed below:
- Diseases of the musculoskeletal system.
- Tumors.
- Chondrosis.
- Inflammatory and purulent diseases of soft tissues.
- Various injuries.
- Unsuccessful surgical operations.
- Excessive physical activity.
- Metabolic disease.
- Achondroplasia.
- Anomalies of bone tissue.
- Down syndrome.
- Asthma.
- Ankylosing spondylitis.
- Inflammatory diseases.
- Syndrome Wife.
All these diseases lead to serious consequences, and ultimately deform the chest.