Post-infarction cardiosclerosis is a form of coronary artery disease, the course of which is characterized by partial replacement of the muscle tissue of the heart with connective tissue as a result of myocardial infarction. Post-infarction cardiosclerosis - ICD 10 code I25.1.
Post-infarction cardiosclerosis is manifested by cardiac arrhythmias and symptoms of heart failure (edema, shortness of breath, increased fatigue, cyanosis, exercise intolerance).
Treatment of the disease can be either conservative or surgical. If the development is unfavorable, the outcome of a disease such as post-infarction cardiosclerosis is instant death.
Kinds
There are two main types of post-infarction cardiosclerosis:
- finely focal (scattered);
- large-focal post-infarction cardiosclerosis.
The latter type is less treatable and has a poor prognosis. An aneurysm can occur in this area, so large-focal post-infarction cardiosclerosis is often the cause of death of the patient.
Fine-focal PICS occurs with dystrophy or atrophy of heart tissue and appears as small whitish foci or stripes on the myocardium. The cause of the disease is often hypoxia, in which the heart tissue is poorly supplied with oxygen.
There is also diffuse cardiosclerosis, in which the stroma of the heart muscle becomes thicker, coarser, and the connective tissue seems to envelop the myocardium in a network.
The need for preventive measures and lifestyle adjustments
A person diagnosed with post-infarction cardiac cardiosclerosis, when prescribing treatment, must follow the doctors’ recommendations for maintaining a new lifestyle, the full implementation of which can significantly improve the quality of the patient’s subsequent life.
It is necessary to change the intensity of physical activity, while eliminating hard work and serious sports from the patient’s life. Hiking and a simple complex of physical therapy are shown.
It is recommended to follow a certain diet and nutrition regimen. Ready-made menus are offered for the day, week, and a list of permitted and strictly prohibited foods and drinks is provided.
Only joint actions of the doctor and the patient, constant monitoring of health status will help to avoid possible complications of the disease and its further development.
You can learn more about the disease by watching the video:
Symptoms
IHD post-infarction cardiosclerosis is manifested by the following symptoms:
1. Shortness of breath. At the initial stage of the disease, shortness of breath occurs only after significant physical exertion, but as it progresses, it can appear even at rest. It is also possible to experience nocturnal shortness of breath, which appears when a person goes to bed and disappears a few minutes after falling asleep. The danger of such shortness of breath is that if you do not take a horizontal position in time, then pulmonary edema may develop, followed by death.
2. Chest pain. The patient feels pain in the chest region, on the left, which can radiate to the left arm and shoulder blade.
3. Edema. They can lead to liver enlargement, swelling of the neck veins, and ascites. If the disease is caused by high blood pressure, then pulmonary edema may develop. Most often, with PICS, severe swelling of the lower extremities is observed.
4. Lack of appetite.
5. High blood pressure.
6. Tachycardia.
7. Decreased ability to work.
8. Cardiac arrhythmias.
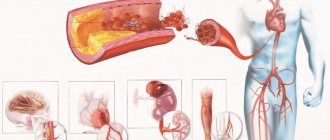
Auscultation reveals a dull heart sound, murmurs, and rhythm disturbances. A very bad sign of post-infarction cardiosclerosis is the formation of a chronic aneurysm in the left ventricle. This increases the likelihood of blood clots and thromboembolism, as well as aneurysm rupture. In this case, the outcome of the disease is post-infarction cardiosclerosis - the death of the patient.
Deadly complications
The replacement of muscle tissue with connective tissue provokes the occurrence of numerous disorders of the heart, which can lead to death.
Dangerous complications of post-infarction cardiosclerosis:
- paroxysmal tachyarrhythmia (tachycardia);
- ventricular fibrillation;
- cardiogenic shock.
Paroxysmal tachycardia is manifested by attacks of rapid heartbeat, which are accompanied by dizziness, nausea, and sometimes fainting.
During one of the paroxysms, ventricular fibrillation may develop - their chaotic contraction with a very high frequency (more than 300 beats per minute). Such a complication in 60% of cases leads to the death of the patient.
Cardiogenic shock occurs due to large-focal cardiosclerosis of the left ventricle. This is a sharp deterioration in its contractility, which is not compensated by the corresponding vascular reaction. This leads to a lack of blood supply to all human tissues and organs. Manifestations of cardiogenic shock are as follows: drop in blood pressure, pale and moist skin, pulmonary edema, stupor. In 81–95% of cases (depending on the age of the patient), this condition leads to death.
Diagnostics
The diagnosis of PICS is made automatically if the patient has suffered a myocardial infarction. But in rare cases, it happens that the patient is unaware of the development of this pathology for a long time. In this case, the following diagnostic methods are used to make a diagnosis:
1. Interview and examination of the patient. During the interview, the doctor asks about the patient’s past illnesses and listens to the patient’s complaints. During the examination, the specialist notes the symptoms of the disease, after which he performs auscultation, during which he detects a weakening of the first heart sound, and sometimes systolic murmur and gallop rhythm.
2. Electrocardiogram. Post-infarction cardiosclerosis can manifest itself on an ECG. Post-infarction cardiosclerosis on ECG, signs:
- myocardial defects;
- focal changes that are characteristic of a heart attack;
- hypertrophy of both ventricles of the heart;
- bundle branch block;
- diffuse changes in the heart.
3. Ultrasound of the heart. In addition to the ECG, post-infarction cardiosclerosis is diagnosed using ultrasound. This study allows you to assess how impaired the contractile function of the heart is. In addition, ultrasound reveals the presence of scars on the heart, and also determines how much the size and shape of the myocardium has changed.
4. Radiography. It is used to detect an increase in heart volume.
5. Coronary angiography. Conducted to assess blood circulation.
6. Angiography. Helps identify the degree of narrowing of the coronary arteries.
7. Echocardiography. It is one of the most informative for PICS. Allows you to identify contractile dysfunction, chronic aneurysm, determine the volume and location of damaged myocardial tissue.
8. Positron emission tomography. Allows you to differentiate tissue lesions from healthy tissue.
Causes
The main cause of PICS is myocardial infarction. However, in some cases, against the background of coronary heart disease, muscle tissue is gradually replaced by connective tissue, which causes diffuse cardiosclerosis. Often this fact is discovered only at autopsy.
Other diseases of the cardiovascular system (myocarditis, dystrophic processes, injuries of coronary vessels) can also lead to the development of cardiosclerosis, but this happens much less frequently.
Treatment
Conservative treatment of post-infarction cardiosclerosis is aimed at slowing the development of heart failure, preventing the proliferation of connective tissue in the myocardium and relieving disturbances in heart rhythm and conduction.
First of all, the patient must change his lifestyle, daily routine and diet. It is necessary to significantly limit emotional and physical stress, follow a special diet and take medications prescribed by your doctor.
For the treatment of PICS use:
- metabolic agents;
- ACE inhibitors;
- diuretics;
- nitrates;
- disaggregants;
- beta blockers.
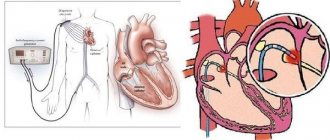
In case of severe conduction and heart rhythm disturbances, surgical intervention is possible, the essence of which is to install an pacemaker or defibrillator.
If angina persists after a heart attack, this is an indication for stenting or angioplasty of the coronary arteries. If an aneurysm develops, its resection is performed, followed by coronary artery bypass grafting.
Development of post-infarction cardiosclerosis in adults
Not everyone knows what PICS is. Post-infarction cardiosclerosis is a chronic cardiac pathology that develops mainly against the background of an acute form of coronary artery disease. In such people, the number of muscle cells decreases. This contributes to impaired myocardial contractility and circulatory disorders. In a healthy person, the heart works by contracting muscle cells and generating nerve impulses.
With IHD, oxygen starvation of tissues is observed. Cardiosclerosis is most dangerous against the background of an acute infarction, since in this case an area of necrosis is formed. Subsequently, it is replaced by connective tissue and is disabled. In severe cases, such people need to have a pacemaker installed. The ventricles and atria dilate with cardiosclerosis. The organ itself increases in volume. Often, with cardiosclerosis, valves are involved in the process.
What is cardiosclerosis? Types and classification
The following types of post-infarction cardiosclerosis are distinguished:
- Focal;
- Widespread (diffuse);
- Involving valves.
An experienced cardiologist knows that the focal form of the disease most often develops. It is characterized by the presence of a limited area of connective tissue, next to which functioning cardiomyocytes are located. The lesions can be single or multiple. This pathology can be no less serious than diffuse cardiosclerosis. Cardiosclerosis is most dangerous in the area of the left ventricle of the heart, since the systemic circulation begins there. Less commonly, diffuse cardiosclerosis develops against the background of a heart attack. With it, the connective tissue is distributed evenly. The cause may be a massive heart attack.
Main etiological factors and causes
Large-focal post-infarction cardiosclerosis develops against the background of an acute form of coronary heart disease. Other causes of the development of this pathology include bruise and injury to the heart, myocardial dystrophy, rheumatism, and myocarditis. The following risk factors are identified:
- atherosclerosis of the coronary arteries;
- poor nutrition;
- blood lipid disorder;
- diabetes;
- hypertonic disease;
- obesity;
- nervous tension;
- addiction to alcohol and cigarettes.
A common cause of heart attack is atherosclerosis. With it, plaques form in the lumen of the coronary arteries that supply the heart. They impede blood flow, leading to acute ischemia. A heart attack can also develop against the background of thrombosis, when the lumen of the vessel is blocked. This pathology is detected mainly in people over 40 years of age.
After a heart attack, scars are formed consisting of connective tissue. These are areas of sclerosis. This tissue is not capable of contracting and conducting impulses. The consequence of all this is a decrease in cardiac output. Subsequently, rhythm and conduction are disrupted.
How does cardiosclerosis occur?
This form of chronic ischemic heart disease is manifested by the following symptoms:
- shortness of breath;
- a feeling of interruptions in the work of the heart;
- cough;
- increased heartbeat;
- swelling;
- dizziness;
- weakness;
- decreased performance;
- sleep disturbance;
- chest pain.
The most consistent symptom of the disease is shortness of breath. It is more pronounced if there is an atherosclerotic process. It does not appear immediately, but several years after the start of the growth of connective tissue. Shortness of breath has the following distinctive features:
- accompanied by cough;
- appears in a lying position, during stress and physical activity;
- disappears when sitting;
- progresses over time.
Patients often experience nocturnal attacks of cardiac asthma. When cardiosclerosis and arterial hypertension are combined, there is a high probability of developing left ventricular failure. In this situation, pulmonary edema develops. If, against the background of a heart attack, foci of necrosis have formed in the area of the right ventricle and a violation of its function is observed, then the following symptoms occur:
- liver enlargement;
- swelling;
- pulsation and swelling of the veins in the neck;
- acrocyanosis.
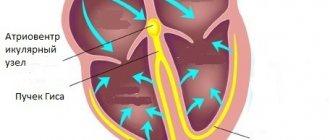
Fluid may accumulate in the chest and pericardial sac. Stagnation of blood in the lungs against the background of cardiosclerosis leads to coughing. It is dry and paroxysmal. Damage to the nerve fibers of the pathways leads to heart rhythm disturbances. Cardiosclerosis causes atrial fibrillation and extrasystole. The most dangerous consequences of this disease are complete blockade and ventricular tachycardia.
Forecast
With PICS, the prognosis depends on the severity of the disease and the location of pathological changes in the heart muscle.
With such a severe pathology as post-infarction cardiosclerosis, the prognosis for survival is as follows. If the left ventricle of the heart is affected and blood flow is reduced by more than 20%, the patient’s quality of life deteriorates significantly. With such pathological changes, conservative therapy can no longer lead to a complete cure; it only maintains the current state of the body. Without a heart transplant, the patient will live no more than five years.
It is also worth noting that the more scars have formed on the heart, the more difficult it is to eliminate the source of pathology and symptoms and the more unfavorable the prognosis.
Treatment after diagnosis is aimed at preventing recurrent heart attacks. If the necessary treatment is not carried out, then most often post-infarction cardiosclerosis is the cause of death of the patient.
Causes of cardiosclerosis and methods of its treatment
Cardiosclerosis is a disorder of the tissue structure of the heart. It occurs in two forms: small-focal cardiosclerosis and large-focal cardiosclerosis. What is it? As many remember from school biology courses, our body consists of organs, and organs are made of tissues. Tissue is a system of homogeneous cells that perform a single function. Each tissue in the body has its own purpose and takes its place in the “design” of organs.
Epithelial tissue serves as the outer covering of both the entire human body and individual organs. Nervous tissue “works” as a conductor of signals between the brain and external “sensors” - receptors (in fact, the brain itself is a “clump” of nervous tissue). Muscle tissue has the property of contracting, obeying signals-impulses coming from the brain and is the basis for the muscles of the body. Connective tissue functions as a support, a “framework” of the body, both internal (bones and cartilage) and external (dermis - the top layer of skin).
Types of muscle tissue
The basis for the structure of the heart is muscle tissue, but not ordinary one. The heart muscle has a special fibrous structure and a characteristic structure, due to which the muscle tissue of the heart is called striated muscle tissue. Cross-striped cardiac tissue, which almost entirely consists of the myocardium, the main part of the heart, has the most important property, without which the work of the heart would be impossible. The heart muscle can contract under the influence of signals originating in its own cells of the heart tissue.
In addition to cardiac tissue, the heart has in its “construction” the integumentary tissue of the endocardium, the inner surface of the heart wall, and connective tissue - a thin film no more than half a millimeter thick, of which the epicardium consists. Anyone who has dealt with raw meat can visualize this film; the characteristic film covering individual muscles and veins of meat has a similar structure.
Read also: Ischemic cardiosclerosis
Prevention
The most effective method of prevention is to prevent myocardial infarction. Therefore, patients who are at risk for this disease should undergo regular examinations by a cardiologist for the timely detection of possible pathological processes in the myocardium.
An important step in preventing PICS is diet. The patient should give up strong tea, cocoa, chocolate, coffee, alcoholic beverages, fatty and fried foods, which contain large amounts of cholesterol.
In addition, it is necessary to give up bad habits, normalize your daily routine, lead a healthy lifestyle, and spend more time in the fresh air.
Physical activity (moderate, without overexertion) and sanatorium-resort treatment in cardiac clinics and sanatoriums will be useful.