Types of cardiac excitability disorders
Taking into account the place of occurrence of electrical excitation, extrasystoles are:
- atrial,
- ventricular,
- atrioventricular.
Atrial extrasystole – the zone of excitation is the atria. The cardiogram changed in such cases differs from the normal one in the reduced size of the P wave. If an extraordinary impulse appears in the area of the atrioventricular node, the excitation wave has an unusual direction. A negative P wave appears.
Ventricular extrasystole - additional impulses occur only in one of the ventricles and cause an extraordinary contraction of this particular ventricle. This type of extrasystole on the ECG is characterized by the absence of the P wave, prolongation of the interval between the extrasystole and the normal contraction of the heart. The interval before the extrasystole, on the contrary, is shortened. Extraordinary contraction of the ventricles does not affect the functioning of the atria.
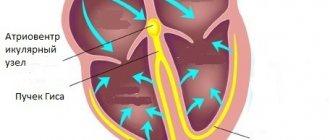
Atrioventricular extrasystole - the atrioventricular node is considered the zone of excitation. In this case, the excitation wave in the atrium has the opposite direction to the usual one. But excitation through the trunk of the His bundle, through the conduction system of the ventricles, is carried out in the usual way. Atrioventricular extrasystoles are characterized by a negative P wave, recorded in different parts of the node.
Supraventricular extrasystole is another name for extraordinary ectopic contractions of the heart that occur in the atria and atrioventricular node. All types of extrasystoles that appear in the upper parts of the heart, that is, above the ventricles, are supraventricular extrasystoles.
Extrasystoles that appear in different foci and are characterized by a polymorphic ECG are polytopic. According to the number of extrasystoles, they can be single, paired, or group. When an extrasystole occurs after a normal heart contraction, bigeminy develops.
Prevention and prognosis
You can avoid the occurrence of extraordinary contractions of the ventricles by following the following preventive recommendations:
- complete renunciation of addictions;
- limiting the consumption of strong coffee;
- avoiding physical and emotional fatigue;
- rationalization of the work and rest regime, namely full, long sleep;
- use of medications only under the supervision of a physician;
- complete and vitamin-enriched nutrition;
- early diagnosis and elimination of pathologies leading to ventricular extrasystole;
- Regularly undergoing a complete preventive examination by clinicians.
The outcome of the disease depends on its course. For example, functional extrasystole has a favorable prognosis, and pathology developing against the background of organic heart damage has a high risk of sudden cardiac death and other complications. However, the fatality rate is quite low.
The mechanism of occurrence of extraordinary contractions of the heart
In many ways, cardiac extrasystole is associated with nervous factors. The fact is that the ventricles of the heart are under the influence of the parasympathetic nervous system. If the heart is weakened, the amplifying nerve not only increases the strength and frequency of heart contractions. It simultaneously increases the excitability of the ventricles, which leads to the appearance of extrasystole.
An important role in the mechanism of arrhythmias is played by disturbances in electrolyte metabolism of a local or general nature. When the concentration of potassium, sodium, magnesium changes inside and outside the cell, it affects intracellular excitability and contributes to the occurrence of arrhythmias.
Why does rhythm disturbance occur?
The cause of extrasystole is a violation of the excitability of the heart. Extrasystole accompanies many diseases, such as myocarditis, ischemic heart disease, cardiosclerosis, rheumatism, heart defects and other diseases. But in half the cases it is not connected with them in any way. Other reasons:
- reflex effects from internal organs (for cholecystitis, diseases of the genital organs, stomach);
- overdose of cardiac glycosides, abuse of diuretics, antiarrhythmic drugs;
- imbalance of electrolytes sodium, potassium, magnesium;
- consumption of stimulants - large amounts of coffee, alcohol, energy drinks;
- high physical activity;
- neuroses, psychoneuroses, labile cardiovascular system;
- endocrine diseases – thyrotoxicosis, hypothyroidism;
- chronic infections.
The causes of supraventricular extrasystole, as one of the supraventricular arrhythmias, are the same as those listed above.
Extrasystole with osteochondrosis has recently become a common occurrence. Its appearance is associated with degenerative-dystrophic changes in the thoracic spine. The nerve roots and plexuses located in this area can be pinched and disrupt the innervation of the heart and other organs.
Extrasystole during pregnancy occurs in half of expectant mothers 2–3 months before birth. During this period, the woman’s body experiences the highest stress. Treatment of cardiac extrasystole in pregnant women is impossible without finding out the cause, and they can be different. And the treatment should not have a negative effect on the fetus. Therefore, immediately see a cardiologist.
Etiology
Ventricular extrasystole in children and adults is considered one of the most common types of arrhythmias. Among all types of the disease, this form is diagnosed most often, namely in 62% of situations.
The causes are so diverse that they are divided into several groups, which also determine the course of the disease.
Cardiac disorders leading to organic extrasystole are presented:
- ischemia;
- myocardial infarction;
- myocarditis;
- cardiosclerosis formed against the background of a previous heart attack;
- pericarditis;
- malignant course of hypertension;
- dilated and hypertrophic cardiomyopathy;
- chronic course of heart failure;
- pulmonary heart syndrome;
- mitral valve prolapse;
- congenital or secondary heart defects.
The functional type of ventricular extrasystole is determined by:
- long-term addiction to bad habits, in particular, smoking cigarettes;
- chronic stress or severe nervous tension;
- drinking large amounts of strong coffee;
- neurocirculatory dystonia;
- osteochondrosis of the cervical spine;
- vagotonia.
In addition, the development of this type of arrhythmia is influenced by:
- hormonal imbalance;
- overdose of drugs, in particular diuretics, cardiac glycosides, beta-agonists, antidepressants and antiarrhythmic substances;
- the occurrence of VSD is the main cause of ventricular extrasystole in children;
- chronic oxygen starvation;
- electrolyte disturbances.
It is also worth noting that in approximately 5% of cases, such a disease is diagnosed in a completely healthy person.
In addition, specialists from the field of cardiology note the occurrence of such a form of the disease as idiopathic ventricular extrasystole. In such situations, arrhythmia in a child or adult develops for no apparent reason, i.e., the etiological factor is established only during diagnosis.
How to react to an extraordinary contraction of the heart
One category of people does not feel extrasystole at all. Arrhythmia is discovered accidentally during auscultation, taking a cardiogram when visiting a doctor for another reason. Some patients perceive it as freezing, cardiac arrest, a blow, jolts to the chest. If group extrasystoles occur, symptoms of arrhythmia may be accompanied by slight dizziness and a feeling of lack of air.
In most cases, single extrasystoles are harmless. Short, frequent (6–8 per minute), group and polytopic extraordinary contractions of the heart can have adverse consequences. Why is extrasystole of these types dangerous?
It is sometimes preceded by more severe types of arrhythmias - paroxysmal tachycardia with a number of contractions up to 240 per minute and atrial fibrillation. The latter is accompanied by uncoordinated contractions of the myocardium. A serious heart rhythm disorder, such as extrasystole, can provoke ventricular fibrillation.
Therefore, if you experience any discomfort in the heart area, you should seek medical help.
How to restore heart rhythm
How to treat extrasystole, and by what means? You need to start by going to the doctor. First you need to get examined. Identify and, if possible, eliminate the factors causing arrhythmia.
Antiarrhythmic drugs for extrasystole are the main stage of treatment. They are selected individually. The same remedy may help one patient, but simply will not work for another. Single rare extrasystoles not associated with heart disease do not need to be treated. Patients with early polytopic extrasystoles are hospitalized.
For ventricular extrasystoles, novocainamide, lidocaine, diphenine, and ethmozine are indicated. Supraventricular extrasystole is treated using verapamil, quinidine, propranolone and its analogues - obsidan, anaprilin, inderal. Cardarone and disopyramide are active in both types of arrhythmia.
Diagnosis and treatment of extrasystole
Heart rhythm disturbances (in particular extrasystole) can occur both against the background of organic heart diseases and in the absence of any structural changes in the coronary arteries, myocardium or valve apparatus. Extrasystoles are premature excitations and contractions of the entire heart or its parts. Depending on this, they are divided into atrial, ventricular and extrasystoles emanating from the atrioventricular junction.
The disease caused by structural pathology of the heart has a more severe prognosis. The development of arrhythmia can be facilitated by the presence of coronary heart disease, congestive heart failure, arterial hypotension, hypoxemia, electrolyte imbalance (potassium, calcium, magnesium), drug intoxication, excessive consumption of coffee and alcohol.
NIMARMEDIC cardiologists successfully treat this type of arrhythmia using conservative (medicinal) treatment and also determine the need for possible surgical intervention. High-tech diagnostic equipment and high professionalism of doctors are a guarantee of effective treatment of the disease in the clinics of the NEARMEDIC network.
To make an appointment with a cardiologist, call or fill out a request on the website.
Once ventricular extrasystoles are detected in a patient, treatment should be selected taking into account the symptoms and the presence of dangerous types of extrasystoles.
The tactics for managing patients with ventricular extrasystole are as follows:
- observation without prescribing medications for patients with benign PVC, which is subjectively well tolerated (it is recommended to change lifestyle, eat a balanced diet, eliminate factors that provoke arrhythmia, adjust physical activity, etc.);
- in case of functional ventricular extrasystole (extrasystole caused by non-cardiac diseases) and extrasystole associated with heart pathologies, drug therapy is prescribed aimed at treating the underlying disease;
- treatment with antiarrhythmic drugs;
- the use of surgical treatment (radiofrequency ablation of the arrhythmogenic area of the myocardium, heart transplantation).
There are several main areas of treatment depending on the course, form and severity of PVCs.
1. If a person has no complaints, and the study reveals rare single monomorphic premature ventricular complexes that do not cause hemodynamic disturbances, no special therapy is required. In this case, the patient should give up caffeine-containing and alcoholic drinks, eliminate smoking, establish a daily routine, and ensure adequate sleep and rest. If there are any dysfunctions of the body associated with insufficient mobility, you need to increase physical activity in accordance with the body's capabilities. At the same time, it is necessary to exclude excessive physical activity (weight lifting, weightlifting). Your diet should include foods rich in potassium and magnesium: they have a beneficial effect on the cardiovascular system.
| Products containing potassium | Products containing magnesium |
| ⠀•⠀dried apricots; ⠀•⠀cocoa powder; ⠀•⠀wheat bran; ⠀•⠀raisins; ⠀•⠀sunflower seeds; ⠀•⠀nuts (pine nuts, almonds, peanuts, walnuts); ⠀•⠀legumes (peas, lentils, beans); ⠀•⠀jacket potatoes; ⠀•⠀avocado; ⠀•⠀ceps; ⠀•⠀bananas; ⠀•⠀citrus fruits; ⠀•⠀Brussels sprouts and kohlrabi; ⠀•⠀milk and fermented milk products; ⠀•⠀cereals (oatmeal, buckwheat, pearl barley, rice); ⠀•⠀fruits (peaches, pears, watermelon, apples, prunes, apricots, melon); ⠀•⠀chicory; ⠀•⠀vegetables (carrots, spinach, green onions, eggplant, cucumbers); ⠀•⠀chicken eggs; ⠀•⠀fish and meat; ⠀•⠀apple juice. | ⠀•⠀oil (sesame, flaxseed, peanut); ⠀•⠀cheese (Dutch, Poshekhonsky, goat, with mold); ⠀•⠀cottage cheese (low-fat and low-fat, curd cheese); ⠀•⠀bitter chocolate; ⠀•⠀almost all types of meat; ⠀•⠀fish (halibut, sturgeon, perch, haddock, cod, saury); ⠀•⠀duck eggs; ⠀•⠀cereals (rolled oats, chickpeas, peas, buckwheat, brown rice, lentils); ⠀•⠀fruits and berries (cherries, kiwi, pineapple, feijoa, raspberries, pears, peach, persimmon); ⠀•⠀many varieties of tea (for example, “Ivan-tea”) and juices; ⠀•⠀ginger; ⠀•⠀mustard; ⠀•⠀vanilla. |
2. When attacks of extrasystole are detected, which are accompanied by clinical symptoms, but do not disturb hemodynamics and have a benign course, beta-blockers (Bisoprolol, Metoprolol) are first prescribed. Sometimes, especially with functional ventricular arrhythmia against the background of vegetative-vascular dystonia and stressful conditions, drugs with sedative (Valemidin, Valerian) and anti-anxiety effects (Stresam, Adaptol), magnesium preparations (Magnerot) help in complex treatment , "Magne B6 forte"). It must be emphasized that the number of PVCs is taken into account when determining the degree of its malignancy. Frequent (up to 1000 or more per day) ventricular extrasystole in itself, even in the absence of obvious heart disease, is an indication for antiarrhythmic therapy.
Frequent PVCs and the appearance of paired, polytopic extrasystoles disrupt the movement of blood through the vessels, therefore, to reduce the risk of ventricular fibrillation and cardiac arrest, antiarrhythmic drugs are prescribed. It is preferable to use class I antiarrhythmics, and only if they are ineffective - Amiodarone or Sotalol. In parallel, drugs must be used to treat the underlying disease that caused the extrasystole[10]. To assess the results of treatment, as a rule, daily ECG monitoring is performed. A decrease in the number of PVCs by 75-80% indicates the effectiveness of therapy.
3. For PVCs of a malignant nature, it is necessary to prescribe highly effective drugs, such as Amiodarone and Sotalol. Sometimes they are combined with maintenance doses of beta-blockers. Treatment is usually carried out in a hospital setting, under ECG monitoring. In the hospital there are more opportunities to adjust hemodynamics and significantly reduce the risk of death in patients with cardiac arrhythmias.
Class I antiarrhythmics should not be taken if the patient has the following pathologies:
- severe signs of heart failure (low ejection fraction according to echocardiography);
- acute forms of coronary heart disease (acute infarction, progressive angina);
- previous myocardial infarction (especially if it was less than 6-12 months old);
- angina pectoris of functional classes III and IV (especially with proven coronary atherosclerosis);
- severe hypertrophy of the left ventricle with a thickness of more than 14 mm and/or the right ventricle (according to echocardiography);
- chronic heart failure class III-IV according to NYHA (New York Heart Association) and/or left ventricular ejection fraction less than 35%;
- pronounced dilatation (expansion of the chamber) of the left ventricle, cardiomegaly;
- active myocarditis;
- bundle branch block;
- severe bradycardia, etc.
If the patient does not have these contraindications and has moderately severe heart pathology, then the use of class I drugs can be considered [10]. It should be noted that antiarrhythmic drugs can have a proarrhythmic effect, i.e. cause a more dangerous arrhythmia, so only a doctor can prescribe them and only with appropriate indications.
Work has appeared that has shown the possibility of a beneficial effect of Omacor on ventricular arrhythmia, in particular in patients with coronary heart disease and chronic heart failure [6]. The addition of this drug to antiarrhythmics increases the effectiveness of treatment of ventricular arrhythmias. If the problem is associated with an electrolyte imbalance, then the patient is prescribed Magnesium sulfate or Potassium chloride.
The question of the duration of antiarrhythmic therapy is practically important. In patients with malignant ventricular arrhythmias, antiarrhythmic therapy should be continued indefinitely, in most cases for life. For less malignant rhythm disturbances, treatment should continue for up to several months with the possibility of gradual (due to the danger of rebound syndrome) its withdrawal. After stopping continuous therapy, the patient is advised to always carry a successfully used antiarrhythmic with him and take it in case of resumption of cardiac dysfunction.
4. For ventricular extrasystole, surgical treatment is possible. Indications for surgical intervention are:
- frequent (from several thousand to 20-30 thousand per day) ventricular extrasystole with an identified arrhythmogenic focus;
- ineffectiveness or impossibility of long-term use of antiarrhythmics in combination with poor tolerability or poor prognosis.
The high activity of the lesion makes it possible to detect it when drawing up a map of the electrical activity of the heart and perform radiofrequency ablation (RFA) of this myocardial zone[11]. The essence of the RFA technique is that a catheter is inserted into the patient through a large-caliber vessel, which is guided under the control of equipment to the very heart. First, using a special technique, the focus of pathological impulses is diagnosed, and then the site of ectopic excitation is exposed to a radiofrequency pulse, which leads to its destruction.
It is also possible to install an electrical pacemaker (ECS). The pacemaker is a device with electrodes that are attached to the ventricle and atrium during surgery. The electrodes create electronic impulses that cause the myocardium to contract. A pacemaker essentially replaces the sinus node, which is responsible for rhythm. It relieves a person from extrasystole and allows him to return to a full life.
In acute and chronic coronary heart disease, the development of ventricular arrhythmia is directly related to myocardial ischemia. In this regard, surgical myocardial revascularization (stenting, coronary artery bypass grafting) can improve electrical stability and reduce the likelihood of developing ventricular arrhythmias.
In patients with a high risk of sudden death and congestive heart failure, heart transplantation remains the main treatment option.
Key benefits of treatment at NEARMEDIC
Highly accurate diagnostic methods
NEARMEDIC cardiologists use a unique cardiac screening program, which includes effective clinical and instrumental examinations and laboratory tests. Using an ECG, functional disorders are examined, ultrasound of the heart allows you to detect changes in blood vessels and tissues, daily Holter ECG monitoring reveals changes in heart rhythm, laboratory tests in your own laboratory allow you to identify concomitant diseases and assess the patient’s health in general.
Comfort and convenient location
All NEARMEDIC branches are located very conveniently and cover almost the entire capital. You do not have to go to the other end of Moscow for treatment of ventricular extrasystole or other cardiac disease. Our clinics are located both in the business center and in residential areas of the capital.
Treatment
In situations where such a disease has developed without the occurrence of cardiac pathologies or VSD, specific therapy for patients is not provided. To relieve symptoms, it is enough to follow the clinical recommendations of the attending physician, including:
- normalization of the daily routine - people are advised to rest more;
- maintaining a proper and balanced diet;
- avoidance of stressful situations;
- performing breathing exercises;
- spending a lot of time outdoors.
In other cases, it is first necessary to cure the underlying disease, which is why therapy will be individualized. However, there are several general aspects, namely the treatment of ventricular extrasystole by taking the following medications:
- antiarrhythmic substances;
- omega-3 drugs;
- antihypertensive drugs;
- anticholinergics;
- tranquilizers;
- beta blockers;
- herbal medicines - in cases of the disease in a pregnant woman;
- antihistamines;
- vitamins and restorative medications;
- drugs aimed at eliminating the clinical manifestations of such heart disease.
Surgical intervention for ventricular or ventricular extrasystole is carried out only according to indications, including the ineffectiveness of conservative treatment methods or the malignant nature of the pathology. In such cases, resort to:
- radiofrequency catheter ablation of ectopic foci;
- open intervention, which involves excision of damaged areas of the heart.
Treatment methods for ventricular extrasystole
There are no other ways to treat such a disease, in particular folk remedies.
Extrasystole - causes, symptoms, diagnosis and treatment at NEARMEDIC
In most cases, the cause of the disease is cardiovascular diseases, such as myocardial infarction, cardiosclerosis, pericarditis, mitral heart defects and others. Ventricular extrasystole can be the result of increased automaticity of the cells of the conduction system of the heart beyond the boundaries of the sinus node.
Among the possible causes of the atrial (supraventricular) form of the disease are instability of a person’s emotional sphere, neuropsychic disorders, deep emotions, excessive physical activity, professional sports, and regular stress. Heart disease is also preceded by bad habits such as smoking, alcohol and excessive consumption of spicy foods.
Causes
Extrasystole of the heart can be caused by a number of reasons, which can be divided into two sources.
The first and most basic is diseases of the cardiovascular system. Extrasystole can occur against the background of disturbances in the functioning of the heart, which are accompanied by organic damage to the myocardium. The second block is external:
- pathology of the thyroid gland;
- electrolyte disturbances;
- external influences. For example, being in a stuffy room where there is a lack of oxygen;
- excessive caffeine consumption. This factor causes tachycardia.
Symptoms of the disease
Subjective sensations with this disease are not always expressed. Sometimes the symptoms practically do not manifest themselves, but more often the person talks about the “turning and tumbling” of the heart and feels interruptions in its work. Vigorous contraction of the ventricles after a compensatory pause causes a sensation of a blow, a push into the chest from the inside.
Patients suffering from cerebral atherosclerosis report dizziness. An attack can provoke cerebral circulatory disorders (paresis, aphasia, fainting) in them, and in people with coronary artery disease - angina attacks.
Discomfort, weakness, hot flashes and anxiety, lack of air - these symptoms are characteristic of functional extrasystole. Frequent attacks reduce cardiac output, causing coronary, renal and cerebral circulation to decrease by 10-25%.
It should be noted that patients with organic heart damage tolerate atrial extrasystole and other types of illness more easily than those suffering from vegetative-vascular dystonia.
Symptoms and causes of pathology
Arrhythmia has several forms, and one of them is extrasystole. By the way, quite often patients do not even suspect that they have such a problem. To determine the presence of pathology, it is necessary to examine the heart. The norm is 30 pulses per hour. If the number of impulses per hour is approximately 40 impulses, then the patient has polymorphic type electrosystoles. To know how many extrasystoles are permissible per day, you can make calculations. If a person has had myocardial contractions more than 50 times a day, then it is necessary to treat tachycardia. In general, the daily rate of supraventricular extrasystoles is approximately 20-30 times, which can occur even in healthy people.
Sensations of a subjective nature are not always fully expressed during extrasystole. It is much more difficult for those people who suffer from vegetative-vascular dystonia to endure the disease. But if a person has organic damage to the heart muscle, then, on the contrary, tolerance will be easier.
Most often, a person feels ventricular extrasystoles as beats or jolts inside the chest from the heart. This is explained by a sharp and strong contraction of the ventricles after a compensatory pause has passed. In addition, patients claim that the heart feels like it is tumbling or turning over. It feels like it is freezing, or interruptions in functioning occur.
Symptoms of functional extrasystole are sudden changes in temperature, a feeling of heat, weakness, lethargy, and discomfort. The person sweats heavily. There is a lack of air. A state of panic appears.
Frequent extrasystoles of the group and early type lead to a decrease in cardiac output. As a result, this negatively affects the renal, cerebral and coronary blood flow. In these areas, blood circulation is reduced by approximately 9-26%. In the future, this provokes the appearance of dizziness, sometimes there are fainting, paresis and aphasia. Signs of atherosclerosis of blood vessels in the brain appear. Patients may experience symptoms of angina pectoris, as attacks occur periodically.
If a patient has a group-type extrasystole, this can lead to more dangerous heart rhythm disturbances. Firstly, there is a risk of paroxysmal tachycardia. Secondly, atrial flutter may occur. If the atria are heavily overloaded, then the pathology transforms into atrial fibrillation. Ventricular extrasystole is considered the most dangerous, as it can cause sudden death.
Depending on the etiology, pathology can be toxic, organic and functional. The causes of extrasystole are different. For example, functional extrasystole develops in a healthy person. This is caused by frequent stress, drinking strong coffee and alcohol, drugs, and smoking. Often a similar pathology is found in people with osteochondrosis, neuroses, and vegetative-vascular dystonia. Sometimes it is also found in women during menstruation.
If the disease is organic in nature, then the causes may be heart attacks, cardiosclerosis, ischemic heart disease, heart defects, hemochromatosis, heart surgery, circulatory failure (and chronic), etc.
The causes of toxic extrasystole are often fever and thyrotoxicosis. Sometimes certain medications cause these side effects. For example, this applies to ephedrine, caffeine, proserine, a group of diuretics, glucocorticoids, and some antidepressants.
Extrasystole
The most common type of arrhythmia, which is based on premature contraction of the heart muscle (extrasystole), resulting from heterotopic excitation of the myocardium. This rhythm disorder is diagnosed in 60-70% of patients, and most often these are completely healthy people. According to scientific studies, among people over 50 years of age, the frequency of its registration reaches 90%.
For a healthy person, up to 200 extraordinary contractions per day are allowed. Occurring against the background of complete health due to stress, smoking, drinking alcohol, strong tea or coffee, extrasystole can be functional in nature. Sometimes it occurs against the background of severe physical activity, with vegetative and psycho-emotional disorders. If premature contraction occurs against the background of heart disease (myocarditis, coronary heart disease, valve defects, cardiomyopathy, etc.), it is usually pathological. Extracardiac diseases that have an adverse effect on the heart muscle can also cause: allergic reactions, intoxication due to infections, thyrotoxicosis, poisoning, neoplastic processes, etc.
Classification
There are several options for classifying ventricular extrasystole. The need to know all possible options for dividing them into groups is due to differences in symptoms, prognosis and treatment options for the pathology.
One of the most important criteria when classifying such extrasystoles is the frequency of occurrence of extrasystoles . Extrasystole (ES) is understood as a single extraordinary contraction. Thus, we distinguish:
- Rare (up to 5 per minute).
- Less rare (medium frequency ES). Their number can reach 16 per minute.
- Frequent (more than 16 within one minute).
An equally important option for dividing ES into groups is the density of their occurrence . This is sometimes called "ECG density."
- Single extrasystoles.
- Paired (two ES following each other).
- Group (three or more).
Depending on the place of occurrence , there are:
- Left ventricular.
- Right ventricular.
Division by the number of pathological foci of excitation :
- Monotopic (one focus).
- Polytopic (several foci of excitation, which can be located in one ventricle or in both).
Classification by rhythm :
- Allorhythmic - periodic extrasystoles. In this case, instead of every second, third, fourth, etc. During normal contraction, ventricular extrasystole occurs:
- bigeminy - every second contraction is an extrasystole;
- trigeminy – every third;
- quadrigeminy - every third, etc.
- Sporadic - irregular extrasystoles, independent of normal heart rhythm.
Based on the results of interpretation of Holter monitoring, several classes of extrasystoles are distinguished:
- 0 class – no ES;
- class 1 – single rare monotopic ES, not exceeding 30 per hour;
- class 2 – similar to class 1, but with a frequency of more than 30 per hour;
- class 3 – single polytopic ES;
- class 4A – polytopic paired ES;
- class 4B – any group ES with periods of ventricular tachycardia;
- class 5 – the appearance of early extrasystoles, occurring at the moment of relaxation of the muscle tissue of the heart. Such ES are extremely dangerous, because may be precursors to cardiac arrest.
This Wolf-Lown classification was developed for a more convenient assessment of the degree of risk and prognosis of the disease. Class 0 – 2 poses virtually no threat to the patient.
When choosing a treatment method, doctors rely mainly on classification depending on the degree of benignity of the extrasystole . There are benign, potentially malignant and malignant courses.
Classification depending on the degree of benignity of ventricular extrasystole
Symptoms of extrasystole
Extrasystole does not always have a clear clinical picture. Its symptoms depend on the characteristics of the body and the various forms of the disease. Most people do not feel discomfort and are unaware of this arrhythmia until it is accidentally detected on an ECG. But there are patients who tolerate it very hard. As a rule, extrasystole manifests itself in the form of strong heartbeats, sensations of its fading or a short-term stop followed by a strong push to the chest. Extrasystoles can be accompanied by both pain in the heart and various vegetative and neurological symptoms: pallor of the skin, anxiety, the appearance of fear, a feeling of lack of air, increased sweating.
Diagnostics
The diagnosis of extrasystole is established by a cardiologist or therapist based on the patient’s complaints, information about existing heart diseases and examination. The patient is prescribed electrocardiography. If the ECG does not immediately confirm the disease, daily ECG monitoring is performed.
Treatment methods for extrasystole depend on the etiology, form and severity of the disease. If this rhythm disorder does not cause concern, does not have severe symptoms and does not reduce performance, it does not need to be treated. For patients who experience particularly unpleasant sensations, it is recommended to use sedatives and antidepressants in doses selected by the doctor. Under the influence of tranquilizers, extrasystole may disappear or the patient will no longer feel it.
In case of arrhythmia, patients are advised to avoid heavy physical exertion, sudden turns and bending of the body. Meals should be frequent and small, overeating and eating before bed should be avoided, since an overfilled stomach can also provoke an attack of extrasystole. Carbonated drinks and foods that contribute to flatulence and constipation should be excluded from the diet.
Extrasystole is a disease in which it is imperative to monitor the level of potassium ions in the blood, since with low potassium concentrations even the strongest antiarrhythmic drugs may be ineffective. Regular consumption of dried fruits (dried apricots, raisins, prunes), vegetables and fruits (bananas, apples), and in some cases taking medications will help maintain the level of potassium in the body at the desired level.
Treatment tactics
Treatment of cardiac extrasystole must be carried out immediately. Before selecting the optimal therapy, it is necessary to determine the shape and location of the pathology.
If the patient has single extrasystoles and they are not caused by pathologies of the cardiac type, then therapy will not be needed. If the development of the disease is associated with disturbances in the functioning of the organs of the endocrine, digestive, circulatory system and heart, then it is necessary to first treat the primary disease. If extrasystole is caused by taking medications, then their use should be stopped.
If the disease has a neurogenic etiology, it is recommended to consult a neurologist. He will prescribe medications with sedative properties. For example, Relanium and Rudotel are suitable. Decoctions of peony, lemon balm and motherwort are very useful. They also have sedative properties.
Drug therapy is prescribed when the number of extrasystoles per day exceeds 200 times, and the patient has subjective complaints and cardiac pathologies. Drugs are selected depending on the type of pathology and the number of heart contractions. In some cases, it is used with medications containing antiarrhythmic drugs. The doctor may prescribe Mexilen, Diltiazem, Sotalol, Cordarone, Quinidine, Lidocaine, Novocainamide and other drugs. When the number of extrasystoles decreases or they completely disappear, and this condition persists for a couple of months, then it is allowed to reduce the dosage of drugs or completely cancel them. But as a rule, therapy will be long-term, so it is best to prevent the development of such a pathology in advance.
Extrasystoles in the heart are strong and sharp beats, after which the heart stops. This condition is not considered normal. If such a symptom appears, you should immediately go to the hospital or conduct a detailed examination to select the appropriate therapy. Complications of extrasystole are dangerous, so do not ignore the symptoms. Otherwise, the risk of developing angina pectoris, atrial fibrillation, and even death is possible.
Prevention
For prevention it is necessary:
- treat concomitant cardiac and non-cardiac diseases;
- promptly report any side effects of medications;
- strictly follow the doctor’s instructions and recommendations.
In the event of an attack of arrhythmia, the patient must:
- calm down, take a comfortable position, if you feel dizzy, lie down;
- unbutton or remove clothing that makes breathing difficult, provide free access to fresh air;
- to eliminate interruptions that arise due to a stressful situation, tension, anxiety, you can take 40 drops of Corvalol or other sedatives;
- if the condition worsens, call an ambulance.
It must be remembered that any drug for the treatment of extrasystole should be taken only after consultation with the attending physician, who will select it taking into account the individual situation and prescribe the necessary dosage.
Extrasystole is characterized by a recurrent course. Complete treatment of the underlying disease will help eliminate the disease. It is necessary to undergo a heart examination periodically. It should be remembered that extrasystoles in most cases do not reduce a person’s performance, but the disease can be complicated by other, more serious types of arrhythmias.
Treatment and assistance for extrasystole at home
Extrasystole is a rhythm disturbance in which after each normal contraction of the heart another pathological one occurs from an additional source. In most cases, this condition does not manifest itself in any way, but is detected on the ECG, and is caused by the action of stress factors or chemicals.
Due to the frequent functional nature of the arrhythmia, it is quite possible to treat extrasystole at home. However, with repeated and severe attacks, it is better to consult a specialist.
How to determine extrasystole at home using improvised means?
Unfortunately, there are no specific manifestations of this type of arrhythmia. An accurate diagnosis can only be established by an ECG study. However, there are many signs by which it is possible to suspect the presence of ventricular or supraventricular extrasystole. Perhaps many of you have already felt similar symptoms:
- feeling that the heart is not working properly;
- sudden slowing or rapid heartbeat;
- a feeling of cardiac activity fading, pauses occur between contractions;
- dyspnea.
All this may be accompanied by vegetative disorders:
- nausea, dizziness;
- the appearance of anxiety, fear;
- increased sweating;
- pale skin;
- fainting.
In addition to the signs themselves, you should pay attention to what preceded the attack. Extrasystole often appears after drinking alcohol, large amounts of coffee, smoking and overeating. It can be provoked by significant physical activity or emotional stressful situations. Finally, abnormal heartbeats often accompany pregnancy.
Very often, extrasystoles appear before bedtime when a person lies on his side.
What needs to be done to provide assistance?
It is quite possible to relieve an attack of extrasystole at home. However, it should be remembered that if this arrhythmia is accompanied by other symptoms of damage to the cardiovascular system (pain in the heart area, significant shortness of breath, swelling), then it is better not to delay contacting a cardiologist. Such a combination may indicate the organic nature of the pathology.
First of all, the effect of the etiological factor should be removed. It is necessary to stop physical activity, stop drinking alcohol or coffee.
Take a short break and relax. Open the window to eliminate hypoxia. Take valerian tincture or tablets. For the same purpose, calendula preparations may be suitable, which will help stop severe group extrasystoles.
In most cases, these measures will be quite enough to eliminate an attack of extrasystoles at home. If the abnormal heartbeat does not stop, it is better to consult a doctor immediately.
Features of treatment with folk remedies
It is not always necessary to use antiarrhythmic medications. Treatment of extrasystole with folk remedies also gives good results. There are many medicinal plants that help fight arrhythmias:
calendula – contains large amounts of magnesium and potassium, antioxidants. Calendula infusion brings the rhythm back to normal, improves blood supply to the myocardium;- lemon balm – rich in microelements, has calming, restorative properties, reduces blood pressure;
- hawthorn – contains a large amount of magnesium, has tonic and antiarrhythmic properties, improves coronary blood flow;
- Adonis (Adonis) – contains many cardiac glycosides, due to which it has a cardiotonic effect and restores normal heart rhythm. Contraindicated for gastrointestinal diseases.
- cornflower – has pronounced antiarrhythmic and antispasmodic effects, which makes it good at relieving attacks of extrasystole.
In any case, before using any medicines, even traditional ones, consult your doctor. After all, even herbal medicines can have contraindications.
Prevention
There is no point in treating extrasystole if the main causes of its occurrence are not removed. This is precisely what prevention is aimed at. To this end, it is recommended to follow the following tips:
- avoid stressful situations, get enough rest;
- Get a good night's sleep - this is an important factor in the body's recovery;
- Despite the fact that heavy physical activity can cause attacks, complete adynamia also negatively affects the heart. Moderate exercise is a good preventive measure;
- limit the consumption of alcoholic beverages, coffee, strong tea;
- stop smoking;
- practice massage and breathing exercises;
- Eat foods high in potassium (banana, avocado, baked potatoes, dried apricots, spinach) and magnesium (wheat bran, cocoa, buckwheat, cashews and almonds).
Following these simple rules will help not only get rid of extrasystoles, but also improve your overall health.
conclusions
Treating both ventricular and supraventricular extrasystole at home is a completely feasible task. There are many effective medications that are good at restoring normal heart rhythm. Equally important is following preventive recommendations that help neutralize etiological factors.
However, you should never neglect medical help in such a matter as the treatment of heart disease.
The following sources of information were used to prepare the material.
Treatment of extrasystole
As a rule, antiarrhythmic therapy may be needed for frequent ventricular extrasystoles. Extrasystole most often has a benign course, but in some cases it can adversely affect the prognosis of the underlying disease and, most importantly, in some patients it can significantly worsen the quality of life. Treatment of extrasystoles can completely eliminate interruptions and significantly improve the quality of life, but may also have side effects. Therefore, the decision to prescribe an antiarrhythmic drug or any other therapy is made solely by the doctor.
Currently, the following approaches to the treatment of patients with extrasystole are accepted:
- Impact on the etiology of arrhythmia
- Impact on factors that provoke arrhythmia
- Impact on the mechanisms of arrhythmia
- Impact on patient tolerance to arrhythmia
Medicines for the treatment of patients with ventricular extrasystole
First-order drugs (more than 70% effective)
propafenone (Propanorm), amiodarone (Cordarone)
Second-order drugs (effectiveness 50-70%)
group of beta-blockers: atenolol, metoprolol, bisoprolol, etc.
Tertiary drugs (effectiveness less than 50%)
verapamil, diltiazem, Panangin, diphenylhydantoin, carbamazepine, omega-3 PUFAs
Long-term intermittent use of antiarrhythmic therapy in patients with ventricular extrasystole effectively affects the mechanisms of arrhythmia, is safe and improves the quality of life of patients. In any case, the drug and an individual treatment regimen are prescribed by a cardiologist or arrhythmologist.
Diagnosis of ventricular extrasystole
To determine this type of extrasystole, three main types of diagnostics are sufficient: questioning and examination of the patient, some laboratory and instrumental types of research.
First, complaints are examined. If they are similar to those described above, the presence of an organic pathology affecting the heart should be suspected or determined. The dependence of symptoms on physical activity and other provoking factors is clarified.
When listening (auscultating) the heart, the sounds may be weakened, muffled or pathological. This occurs in patients with hypertrophic cardiopathology or heart defects.
The pulse can be irregular, with different amplitudes. This is explained by the occurrence of a compensatory pause after an extrasystole. Blood pressure can be anything. With group and/or frequent ventricular ES, it may be reduced.
In order to exclude pathology of the endocrine system, hormone tests are prescribed and biochemical blood parameters are studied.
Among the instrumental studies, the main ones are electrocardiography and Holter monitoring. By interpreting the ECG results, one can detect an extended, altered ventricular QRS complex, in front of which there is no atrial P-wave. This indicates contraction of the ventricles, before which there are no atrial contractions. After this deformed extrasystole, a pause is observed, followed by a normal sequential contraction of the cardiac chambers.
ECG with left ventricular and right ventricular extrasystoles
Echocardiography detects signs of ischemia or hypertrophy of the left ventricle only in the presence of concomitant myocardial damage.
In cases of the presence of an underlying disease, the ECG reveals signs of myocardial ischemia, left ventricular aneurysm, hypertrophy of the left ventricle or other chambers of the heart, and other disorders.
Sometimes, to provoke ventricular extrasystole and study the characteristics of the heart muscle at this moment, stress ECG tests are performed. The occurrence of ES indicates the appearance of arrhythmia due to coronary pathology. Due to the fact that this study, if performed incorrectly, can be complicated by ventricular fibrillation and death, it is carried out under the supervision of a physician. The testing room must be equipped with an emergency resuscitation kit.
Coronary angiography is performed to exclude the coronary origin of extrasystole.
Extrasystole of the heart: what are the causes and treatment
What is this:
– premature contraction of the heart, the source of which lies outside the sinus node (the main source of electrical impulses). Most often divided by localization:
– atrial (supraventricular, supraventricular);
– ventricular (right and left ventricular);
– from AV connections or nodes (AV connection is an additional source of impulses, located between the atria and ventricles. It exists just in case of emergency if the sinus node suddenly “passes out”).
– polytopic (from different places).
What's the point:
– extrasystoles, like all rhythm disturbances, irritate patients, but even more so – the doctors themselves; especially if it is impossible to redirect to a cardiologist. The first thing that needs to be decided is whether the extrasystole in a given patient is dangerous or not. Secondly, if yes, what to prescribe. Third, if it is not dangerous, but the patient is bothered, how to calm it down and what to treat then?
Causes of extrasystole
Extrasystoles are the most common subtype of arrhythmia, which periodically occurs in 65% of absolutely healthy people. With a normal heart rhythm there should be about 200 ventricular and 200 supraventricular extrasystoles per day. At moments of failure, up to tens of thousands of extrasystoles are recorded.
The nature of extrasystole can be organic (there are cardiac pathologies) or neurogenic (functional). Functional extrasystole develops when:
- Stress.
- Neuroses.
- Taking medications.
- Cervical osteochondrosis.
- Neurocirculatory dystonia.
- Intense physical activity.
- Abuse of nicotine, alcohol, caffeine-containing drinks.
An episodic increase in the number of daily extrasystoles does not pose a danger to healthy people; such surges in medicine are called “cosmetic arrhythmias.” Heart rhythm disturbances must be monitored and corrected in patients with organic heart pathologies.