Incomprehensible terms from doctors often frighten pregnant women, because not every one of them has a medical education or has read additional literature related to pregnancy. On ultrasound, many people hear the diagnosis of “cephalic presentation of the fetus.”
What does it mean? Is this a pathology or a normal condition that does not threaten the mother and child? Without knowing the exact information, there is no need to panic or worry. It is better to check with your doctor for details or find answers to your questions yourself.
What does cephalic presentation of the fetus mean?
This position of the baby in the uterus is the most common and most desirable for natural birth. By cephalic presentation we mean the position of the baby's head at the entrance to the pelvis.
In 95-97% of cases, the baby is located head down in the uterus. The remaining 3-5% occurs in breech presentation of the fetus, during which childbirth is considered pathological.
Experts distinguish several options for the longitudinal cephalic position of the fetus. The tactics of childbirth and the prevention of complications during delivery depend on them.
Variants of cephalic presentation of the fetus
Obstetricians and gynecologists distinguish several different options for cephalic presentation of the baby:
The most optimal option in gynecology and obstetrics is considered to be occipital presentation . The baby's neck, passing through the birth canal during delivery, turns out to be bent. The back of the baby's head appears first at birth. About 90-95% of births proceed this way. Occipital presentation allows the mother to give birth without ruptures, and the baby to be born without injury.
What does cephalic presentation of a fetus of facial type ? This variety is characterized by maximum extension of the head. The baby emerges from the birth canal with the back of its head. In most cases, with this presentation, the baby is born by caesarean section. However, independent childbirth is not excluded.
Frontal presentation is very rare. The fetal forehead serves as a guiding point through the birth canal. With this type of presentation, a caesarean section is necessary. Natural childbirth is excluded.
The anterior cephalic variant is also called the anterior parietal. During the period of exile, the large fontanel serves as a wire point. With anterior cephalic presentation, the baby can be born either naturally or through cesarean section, but with independent birth there is a high risk of injury to the baby. A mandatory measure during delivery is the prevention of fetal hypoxia.
The location of the fetus is also characterized by position. Position 1 of the cephalic presentation of the fetus means that the back of the baby is facing the left uterine wall. It occurs quite often. The position of the child, in which his back is facing the right uterine wall, is called by obstetricians and gynecologists the 2nd position of cephalic presentation of the fetus.
The baby's back is not always facing the left or right uterine wall. It is usually turned posteriorly or anteriorly. In this regard, the type of position is distinguished. In the anterior view, the back is facing anteriorly, and in the posterior view, the back is facing backwards.
All incorrect presentations and fetal positions can be caused by the following reasons:
Low cephalic presentation of the fetus
Pregnant women usually learn about the low position of the fetus at 20-36 weeks of pregnancy. Fetal descent should occur around 38 weeks. Having heard such a diagnosis, do not panic.
Of course, due to low presentation of the fetal head, premature labor may begin, so doctors should closely monitor the progress of pregnancy, and expectant mothers should follow all doctor’s instructions and perform any actions with extreme caution.
In most cases, childbirth goes well. There are no negative consequences for the baby and his mother.
For low cephalic presentation of the fetus, experts recommend:
- use a special prenatal bandage;
- not to run;
- refuse physical activity;
- rest more often.
Incorrect presentation of the fetus: their features, birth options
The cephalic presentation of the occipital type is the most common and correct position in which babies are born. All other types of presentation are incorrect.
Childbirth with various types of breech presentation is considered pathological. During delivery, serious complications may occur (for example, hypoxia of the child, pinching and extension of his head, throwing back of his arms). Most often, childbirth is carried out by caesarean section, especially if the baby is male. However, natural childbirth is not excluded.
The specific option for delivery with mixed, leg, or breech presentation of the fetus is selected by the doctor depending on various factors.
Childbirth with an extensor presentation of the fetus (anteroparietal, frontal, facial) rarely occurs naturally. With the anterior parietal form, delivery tactics are expectant. A caesarean section is performed when there is a threat to the health and life of the mother and baby.
Independent childbirth with a frontal cephalic presentation is undesirable, since rupture of the uterus and perineum, asphyxia and death of the child are possible.
With a facial presentation, the fetus can be born either through natural birth or through surgery. The first option is chosen only if the female pelvis is of normal size, labor is active, and the size of the fetus is small.
Diagnosis of cephalic presentation of the fetus
At about 28 weeks, an obstetrician-gynecologist, upon examination, can tell about the presentation of the fetus. To determine its type, external obstetric examination techniques are used. With cephalic presentation, the head is palpated above the entrance to the pelvis.
Ultrasound is necessary to make an accurate diagnosis. The doctor can even determine cephalic presentation at 22 weeks. However, before giving birth the situation may change several times. As a rule, the fetus changes its position several times before the 32nd week, since there is enough space in the uterus for its movements.
The presentation of the fetus (breech or cephalic) can be determined by the woman independently. To do this, you need to lie on your back, bend your knees and place one hand on your lower abdomen. If the baby's head can be felt with gentle pressure, the presentation will be cephalic.
It is much more difficult to establish the cephalic presentation variant. Here a woman cannot determine anything on her own. Only an ultrasound can show an accurate diagnosis.
Fetal presentation: concept and classification
The fetus grows and develops in the uterus throughout pregnancy. From a tiny embryo, it gradually turns into a little person. In the first half of pregnancy, it can change its position quite often.
As labor approaches, the activity of the fetus decreases, since it is already very difficult to change position, because it is growing, and there is less and less free space in the uterus.
After about 32 weeks, you can already find out the presentation of the fetus, that is, determine which part of the baby’s body (head or buttocks) is located at the entrance to the pelvis. Sometimes doctors talk about what position the baby is in the tummy before 32 weeks.
Some pregnant women are given this information at 20-28 weeks of pregnancy. However, it should not be taken seriously at such an early stage, because the baby can change a position that is unfavorable to him several times.
There are the following types of fetal presentation:
1. Pelvic (the pelvic end of the child lies at the entrance to the woman’s pelvis):
- gluteal The fetus is located in the uterus with its head up. The legs are extended along the body. The feet are almost at the head;
- foot presentation of the fetus. One or both of the baby’s legs may be located at the entrance to the pelvis;
- mixed (gluteal-leg). The buttocks and legs are present at the entrance to the pelvis of a pregnant woman.
Features of childbirth with various types of cephalic presentation of the fetus
Childbirth is considered correct and favorable if it occurs with an anterior view of the occipital cephalic longitudinal presentation of the fetus. The baby's head bends as it leaves the pelvis. The chin is pressed against the chest. When passing through the birth canal, the role of the leading wire point is played by the small fontanel. The head, moving forward, rotates inside. The face turns out to be facing the sacrum, and the back of the head is facing the pubic symphysis. The head, showing itself to the light, unbends. Next, the shoulders unfold on the inside, and the head on the outside. Now the baby's face is turned towards his mother's thigh. Following the head and shoulders, the remaining parts of the body emerge without difficulty.
When giving birth in the posterior form of the occipital cephalic presentation in the longitudinal position, some difficulties arise. The head turns inside to face the pubic symphysis. The back of the head faces the sacrum. The advancement of the head is delayed. Labor weakness may occur, which can lead to complications. Doctors perform stimulation in such a situation. Obstetric forceps are applied when asphyxia develops.
With a facial presentation, a woman can give birth under the following conditions:
- normal pelvic size;
- small fruit;
- active labor;
- The baby's chin is facing anteriorly (anterior type of facial presentation).
During childbirth, a wait-and-see attitude is adopted. The condition of the woman in labor and the dynamics of labor are under control. Using phonocardiography and cardiotocography, the fetal heartbeat is monitored. If the baby's chin is turned posteriorly in a facial presentation, a caesarean section is performed.
Transverse or oblique presentation of the fetus
During pregnancy, presentation can change repeatedly, depending on the activity of the baby and the anatomical structure of the woman’s body. With an oblique presentation, there is a possibility that during active labor the baby will change position, but doctors advise not to risk it and give birth by caesarean section.
Delivery with a transverse presentation of the fetus is impossible naturally. In such cases, the intersection of the axis of the child and the axis of the woman’s uterus occurs at a right angle, with large anatomical parts of the fetus located above the iliac crests. It is extremely rare that doctors can turn the baby around, but this can lead to injury to the fetus.
What is cephalic presentation of the fetus?
Pregnant women often hear this formulation from gynecologists during examinations from the 30th week of pregnancy. Not all expectant mothers understand this complex medical phrase, so they begin to worry about the condition of the baby developing in the stomach. What is fetal presentation, is the cephalic position normal or a dangerous pathology?
When a doctor talks about presentation, he means the position of the baby’s body from the back of the head to the sacrum relative to the uterus. That is, cephalic presentation of the fetus is the longitudinal position of the fetus with the head placed in the pelvic area. This position of the baby is correct and is observed in 97% of mothers preparing for childbirth. In about 3% of women, babies sit with their butts on the mother’s pelvis, or they can even lie horizontally. In such a situation, childbirth is complex and pathological.
Changes in fetal positions before birth
It is impossible to accurately determine the reasons why the baby occupies a certain position in the uterus. Until the end of the second trimester of bearing the baby, he is constantly in motion, changing his position ten times a day. This suggests that he is very comfortable in his mother’s womb. As the baby grows, the mother’s belly already becomes a little cramped, and therefore, closer to childbirth, he takes a certain position.
Why is the head, in a longitudinal position, located precisely at the bottom of the uterus? Doctors say that the head moves under the influence of the weight of the fetus. But this is only an assumption, and usually the position of the fetus directly depends on the uterus, its contractions and the size of the pregnant woman’s pelvis.
What is cephalic presentation of the fetus?
Gynecologists distinguish four types of head position of the child:
- Occipital. Obstetricians consider this position to be the most comfortable and safe. When the baby moves along the birth canal during childbirth, his neck is bent. The back of the baby's head emerges first from the mother's vagina. More than 95% of births occur in the manner described above. With an occipital presentation, most babies are born without injury, and mothers are usually not diagnosed with ruptures.
- Facial. In this position, the baby's head is tilted very far back. During the birth process, the baby's face is the first to emerge from the mother's genital tract. Usually, with facial placement of the fetus, doctors send patients for cesarean section to prevent complications. Although many women successfully give birth naturally.
- Frontal. This type of presentation is recorded extremely rarely. During childbirth, the baby's forehead is the first to emerge from the mother's vagina. In this position of the fetus, surgical intervention is mandatory; natural childbirth is not allowed.
- Forecephalic. This type of presentation is also called anterior parietal. The first thing to appear from the vagina is the baby's fontanel, located on the top of the head. If the fetus is placed anteriorly, you can give birth either by cesarean section or naturally. But during a natural birth, the baby is likely to get injured. There is also a high risk of baby hypoxia during the birth process.
The position of the baby in the womb is also determined by two positions. When the baby is in the first position, his back is adjacent to the left side of the uterus. Most babies develop in this position. If the child leans his back against the right side of the uterus, then he is in the second position. Sometimes babies press their backs against the anterior or posterior mucous surfaces of the uterus.
What to do if the fetus is in low cephalic presentation?
Typically, doctors tell women about low cephalic presentation of the fetus at 20 weeks of pregnancy. This is too early; normally, the child, in preparation for birth, should descend into the pelvic cup at 38 weeks. Due to the low cephalic presentation of the fetus at 20 weeks, there is a high risk of premature birth. But there is no need to worry: gynecologists closely monitor the condition of patients with an unfavorable diagnosis. Young mothers who have a low cephalic presentation of the fetus in the womb should listen to all the advice of medical specialists and move with extreme caution. Doctors recommend that women with low placement of the child:
- wear special support bandages;
- exclude intense physical activity;
- often rest lying down;
- do not run, do not make sudden and rapid movements.
In the vast majority of cases, childbirth with a low position of the baby takes place at a normal time and is not accompanied by complications.
What are the reasons for fetal malposition?
Sometimes gynecologists diagnose pregnant women not with a cephalic presentation of the fetus, but with a breech presentation. That is, the baby is not placed in the uterus upside down, but sits in the mother’s pelvic bowl with his legs or butt. The following factors provoke the child’s incorrect position:
- mother's narrow hips;
- myoma;
- polyhydramnios, which increases fetal activity;
- oligohydramnios, which interferes with the baby’s mobility;
- placenta previa;
- abnormal structure of the uterine walls;
- low contractility of the uterine muscles;
- genetic predisposition;
- constant compression of the abdomen during daytime rest and night sleep;
- wearing uncomfortable and tight clothing.
If the child is in a pelvic or transverse position, the gynecologist decides which method of delivery will be used. With pelvic placement of the fetus, both normal childbirth and surgical intervention are allowed. Obstetricians perform a caesarean section if the woman in labor has too narrow hips or if the baby is large. In case of transverse presentation, when the baby is located horizontally in the uterus, obstetrics are carried out exclusively by cesarean section. Natural childbirth is contraindicated.
Causes
The causes of malpresentation of the fetus are very diverse. The following factors lead to this pathology:
- polyhydramnios or oligohydramnios;
- a woman’s pelvis is quite narrow;
- placenta previa (location) is too low;
- double or triple wrapping of the umbilical cord around the neck;
- very short umbilical cord;
- tumors in the uterus (fibroids, fibroids);
- the presence of a postoperative scar on the uterus;
- abnormal development of the uterus;
- hypotonicity of the uterus (decreased tone);
- multiple pregnancy or repeat pregnancy;
- myometrial dystrophy;
- saddle or bicornuate uterus.
All of the above reasons are predisposing factors to breech or transverse presentation.
How is fetal cephalic presentation diagnosed?
How is fetal cephalic presentation detected during pregnancy? At about 30 weeks of gestation, the expectant mother will learn from the gynecologist detailed information about the location of the baby in the uterine cavity. Diagnosis of breech presentation is usually made through a standard gynecological examination. The gynecologist plunges his fingers into the patient’s vagina and feels the crown of the fetus’s head above the pelvic bowl. With a pelvic position, the doctor’s fingers come across the baby’s legs or butt. To confirm the diagnosis, the patient is sent for ultrasound monitoring.
A medical specialist can determine the cephalic presentation of the fetus as early as 20 weeks. But it is still not advisable to carry out diagnostics before the 30th week, since before this period the baby does not yet occupy the entire space of the uterus, and therefore is able to roll over several times. The mother herself can find out the location of the baby in the womb at home. To do this, she should lie on her back, spread her legs slightly, bend her knees, and place her palm on the lower abdomen. Lightly pressing on the abdomen with her hand, the woman feels for a hard and round object when the fetus is in a longitudinal cephalic presentation. This is the baby's head. To reassure overly excited and confused young mothers who understand little about anatomy, some gynecologists show them the cephalic presentation of the fetus in photos or schematic illustrations. After all, women who understand the physiological characteristics of childbirth worry little.
Causes of incorrect position of the baby in the uterus and pathological presentation
There may be several reasons for the pathological phenomena under consideration, but they are all conditionally divided into 2 large groups:
Those caused by errors in the structure of the uterus
- The presence of fibrous or myomatous nodes in the cavity or cervix . The presence of tumors in this area does not allow the baby to take the correct position.
- Narrow pelvis: from the 2nd stage. and more.
- Anomalies in the structure of the uterus that are congenital in nature: uterine septum, bicornuate uterus, etc.
- Disorders associated with the location of the placenta : presentation or prolapse.
Pathological phenomena that provoke an increase or decrease in fetal motor activity:
- Errors in fetal development. Absence of the brain, hydrocele of the brain can lead to the fact that the baby takes an oblique position in the womb.
- The presence of several fetuses in the uterus. This phenomenon significantly limits the mobility of children.
- Hypertonicity of the uterus. Such a pathological condition can be provoked by curettage of the uterus, inflammation of the cervix/uterine body, or abortion. In addition, frequent overwork, stress, neuroses, etc. can lead to an increase in uterine tone.
- Much or little water. In the first case, the uterus increases in size, which creates conditions for active movements for the baby. If the amniotic fluid is below normal, the child is simply not able to take the correct position.
- The weight of the fetus is very large (from 4 kg and above) or very small . In the latter case, the child is able to freely and regularly change position in the uterine cavity.
- Weakness of the abdominal muscles. This is especially true for women who have a history of 4 births or more. The muscles lose their elasticity and are unable to restrain the movements of the fetus.
How is childbirth carried out with different types of cephalic presentation of the fetus?
Obstetricians call births safe when there is a longitudinal occipital position of the fetus and a cephalic presentation of the fetus. When the baby walks outwards through the vagina, he tilts his head, his chin presses against his neck. The head, pushing forward, makes a turn. The child's face faces the mother's sacrum, and the back of the head faces the pubic symphysis. When the head finally emerges from the vagina, it extends, then the baby's shoulders straighten, and the face turns towards the mother's thigh. The shoulders and head are the hardest to come out; the torso and limbs leave the birth canal without difficulty.
With an occipital position, childbirth often occurs with complications. The baby's head turns incorrectly in the birth canal: the face looks at the pubic symphysis, and the back of the head looks at the maternal sacrum. As a result, the exit of the head to the outside is delayed. There is also a risk of weakening labor, which is very dangerous for the newborn child. In this situation, obstetricians are forced to subject the woman to stimulation. The use of obstetric forceps is indicated when the baby experiences asphyxia due to prolonged exposure to the genital tract.
With a facial position, natural childbirth is allowed only if the woman has wide enough hips, the fetus is small, and labor is intense. During the birth process, obstetricians carefully monitor the physical condition and well-being of the mother in labor and, using cardiotocography, calculate the heart rate of the newborn baby.
With the frontal position of the fetus, natural childbirth is allowed in extremely rare cases, since it is almost always accompanied by severe complications: ruptures of the vagina and cervix, the formation of vaginal fistulas and even the death of an unborn baby. To correct the position of the head, the obstetrician may gently turn the baby around. If the reversal is impossible, then the doctor decides to perform the operation.
In the anterior cephalic position, childbirth is often carried out naturally. But if the obstetrician understands that the health of the mother and the life of the child are in danger, then he prescribes a caesarean section.
The location of the baby in the mother's tummy is an important factor in pregnancy. After all, the severity of labor, its course and the final result depend on the position of the fetus. If the baby lies normally, then there should be no problems. In this case, delivery takes place naturally. If the child’s position is not the way nature intended it, then a caesarean section cannot be avoided. Most likely, doctors will offer this option to a woman after an ultrasound scan performed in the last weeks of pregnancy. On the screen of the ultrasound diagnostic device, the baby’s tiny body, its position, and position are clearly visible. The appearance of the fetus will tell both doctors and the woman the right decision.
Measures to prevent abnormal fetal positions
In fact, there are no special specific measures to prevent the risks of malpresentation of the fetus. Everything is natural, and the correct position of the child in the womb is inherent in nature; you just need to ensure the normal course of pregnancy throughout its entire period.
It is advisable for a pregnant woman to maintain a favorable psychological mood, eat a nutritious and varied diet, and observe a work and rest schedule. You shouldn't overeat either, especially in the last weeks of pregnancy. After all, a large and post-term fetus can be a risk factor for malpresentation. You should also strictly follow your doctor’s recommendations and take vitamins or medications as prescribed by specialists. If necessary, it is possible to perform special gymnastic exercises suggested by the obstetrician-gynecologist.
Communicate more with your baby, ask him to take the correct position in his tummy - this will help both you and the baby tune in to a positive wave before giving birth.
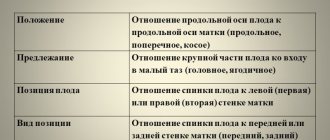
Position and presentation: what is the difference?
Many expectant mothers often confuse the terms. Therefore, before talking about the specific positions of the fetus in the womb, it is necessary to explain the meaning of these words. So, first things first. The position of the fetus is the relationship between the axes of the uterus itself and the posture of the baby. When determining it, doctors are guided by a conventional line that runs from the baby’s head to the pelvis. If the axes coincide, then we can talk about a longitudinal position. When they are perpendicular to each other, the little one lies in a transverse position. The middle option between the two above indicates an oblique position.
Presentation is determined by that part of the body that is in close proximity to the cervix. Accordingly, it can be head or pelvic. If the baby is positioned obliquely or transversely, the presentation cannot be recorded. In addition, the baby’s position is determined based on the rotation of the baby’s back in relation to the sides of the uterus. If it is facing the left wall, they speak of its first variety. The second position is called the reverse pose. Sometimes the back faces the front or back wall of the uterus. In this case, we are already talking about the type of fruit. The types of fruit are called respectively: anterior and posterior. By the way, up to the 34th week of pregnancy, the baby can change its position in the womb. After this period, the situation remains stable, since the baby can no longer “walk around” in a cramped space.
Transverse and oblique position of the fetus: clinical picture, diagnosis, tactics of pregnancy and childbirth.
EPIDEMIOLOGY
Abnormal fetal position is detected with a frequency of 1:200 births (0.5–0.7%), and in multiparous women it is 10 times more likely than in primiparous women.
CLASSIFICATION
Incorrect positions of the fetus include transverse and oblique positions.
Transverse position (situs transversus ) is a clinical situation in which the axis of the fetus intersects the axis of the uterus at a right angle, and large parts of the fetus are located above the iliac crests.
Oblique position (situs obliquus) is a clinical situation in which the axis of the fetus intersects the axis of the uterus at an acute angle, and the underlying large part of the fetus is located in one of the iliac cavities of the large pelvis. The oblique position is considered a transitional state: during childbirth it turns into longitudinal or transverse.
The position of the fetus in case of incorrect positions is determined by the head: if it is located to the left of the midline of the pregnant woman’s body - the first position, if on the right - the second. The view, as with the longitudinal position of the fetus, is determined by the back: if it is facing anteriorly - anterior view, posteriorly - posterior. The location of the fetal back in relation to the fundus of the uterus and the entrance to the pelvis is important.
ETIOLOGY
The causes of transverse or oblique position of the fetus are varied. This includes decreased tone of the uterus and sagging muscles of the anterior abdominal wall. Other causes of abnormal fetal positions: polyhydramnios, in which the fetus is excessively mobile, multiple pregnancy, bicornuate uterus, placenta previa, tumors of the uterus and appendages located at the level of the entrance to the pelvis or in its cavity, narrow pelvis.
CLINICAL PICTURE
The transverse and oblique position of the fetus is determined based on data from examination of the pregnant woman, palpation of the abdomen, and vaginal examination. When examining, pay attention to the unusual transversely stretched shape of the abdomen. The uterus is not elongated oval, but spherical in shape, as it is stretched transversely. Upon palpation, the presenting part of the fetus cannot be determined; the head can be felt to the left or right of the midline of the pregnant woman’s body. With multiple pregnancy, polyhydramnios, or severe uterine tension, it is not always possible to determine the position and position of the fetus.
DIAGNOSTICS
The final diagnosis is made on the basis of ultrasound. Vaginal examination during pregnancy and in the first stage of labor does not give clear results. The study should be carried out very carefully, since the opening of the membranes and the rupture of water with incomplete opening of the uterine pharynx significantly worsens the prognosis of childbirth. During a vaginal examination, after the discharge of water and the opening of the pharynx by 4 cm or more, the side of the fetus (ribs, intercostal spaces), the shoulder blade, the armpit, and sometimes the elbows or hand are palpated. If the handle falls out of the genital slit, the diagnosis of the transverse position is beyond doubt.
EXAMPLES OF FORMULATION OF DIAGNOSIS
·Pregnancy 36 weeks. Transverse position of the fetus. I position, front view.
·Pregnancy 39–40 weeks. Premature rupture of water. Oblique position of the fetus.
·First stage of term labor. Transverse position of the fetus. II position, rear view.
COURSE OF PREGNANCY AND CHILDREN
Pregnancy proceeds without any peculiarities, but premature births occur more often. In the absence of medical care, childbirth is accompanied by a number of serious and extremely life-threatening complications for the mother and fetus (early rupture of water, prolapse of small parts of the fetus, the occurrence of neglected transverse position of the fetus, uterine rupture, death of the mother and fetus). Early rupture of water occurs as a result of excessive tension of the lower pole of the ovum, which is due to the lack of separation of the OB into anterior and posterior. With early rupture of water, labor takes a long time.
Rapid rupture of water often leads to prolapse of the umbilical cord or fetal arm, loss of fetal mobility (neglected transverse position). Prolapse of the umbilical cord in a transverse position of the fetus can lead to infection, the development of chorioamnionitis, and fetal hypoxia. Handle prolapse increases the risk of ascending infection during childbirth. The neglected transverse position of the fetus is often accompanied by the impact of the fetal shoulder into the entrance of the pelvis. Thus, most of the fetus is located in the cavity of the distended lower uterine segment and cervix. The fetus is completely motionless in the uterus; A very dangerous situation arises - neglected transverse position of the fetus.
If the transverse position of the fetus is advanced and labor continues, uterine rupture is possible. The death of a woman in labor can occur due to diffuse peritonitis or sepsis. Generalized infection occurs as a result of a prolonged course of labor, caused by secondary weakness of labor forces, early rupture of water; the fetus dies from hypoxia.
It is extremely rare that childbirth with a transverse position of the fetus ends spontaneously through self-twisting (evolutio foetus spontanea), or the birth of a fetus with a double body (partus conduplicatio corporis). Such a birth outcome is possible as an exception in the case of strong contractions, a very premature or dead macerated fetus. The mechanism of self-inversion is as follows: the fetal head is retained above the boundary line of the pelvis, one shoulder is driven into the pelvic cavity; the neck of the fetus sharply stretches and a shoulder is born from the genital slit, followed by it, sliding past the head, the torso, pelvis and legs of the fetus and, finally, the head. When giving birth with a double torso, the shoulder is born first, then the torso and head, pressed into the stomach, and then the fetal pelvis and legs.
MANAGEMENT OF PREGNANCY IN IMPROPER POSITIONS OF THE FETAL
Pregnancy management is aimed at timely prevention and elimination of complications that may arise with the transverse position of the fetus. At 35–36 weeks of pregnancy, the position of the fetus becomes stable, therefore, when a transverse position is diagnosed, it is necessary to make a decision on the further management of the pregnant woman and inform her about this. A pregnant woman should be hospitalized in a maternity hospital no later than 36–37 weeks of pregnancy; she needs to be explained that timely hospitalization contributes to a favorable outcome of childbirth. In the maternity hospital, the pregnant woman is thoroughly examined and given psychoprophylactic preparation for childbirth; it is necessary to warn the woman that the onset of contractions or the rupture of water must be immediately reported to the doctor on duty (midwife). The operation of correcting the transverse position of the fetus using external techniques (external rotation onto the head), previously widely used at the 35–36th week of pregnancy, is now rarely used. The effectiveness of such an operation is low; the fetus often returns to a transverse position, since the cause of the pathology has not been eliminated. In some cases, the rotation operation leads to serious complications (placental abruption, uterine rupture, fetal hypoxia).
CORRECTIVE GYMNASTICS
At a gestational age of 29–34 weeks, the pregnant woman should be prescribed a set of special exercises to promote the rotation of the fetus into a cephalic presentation. Corrective exercises are performed in the absence of contraindications (uterine scar, signs of miscarriage, fibroids, bleeding, decompensated heart defects, etc.) under the direct supervision of a doctor at the antenatal clinic. You can use the scheme proposed by I.F. Dikanem (a pregnant woman, lying down, turns alternately on her right and left side, lies after each turn for 10 minutes; the procedure is repeated 2-3 times, classes are carried out 3 times a day). A number of authors successfully use the system of corrective exercises developed by I.I. Grishchenko and A.E. Shuleshova. The system consists of exercises that provide rhythmic contraction of the abdominal and torso muscles in combination with rhythmic and deep breathing. If the result is positive, classes are stopped. To secure the created cephalic presentation, longitudinal bolsters are attached to the bandage. The pregnant woman wears a belt with bolsters until the cephalic presentation is completely stabilized (the head is pressed against the entrance to the pelvis). If the exercises are unsuccessful, the hospital doctor decides on the issue of external rotation, if there are no contraindications.
MANAGEMENT OF LABOR IN IMPROPER POSITIONS OF THE FETAL
Childbirth in a transverse position cannot complete spontaneously (self-rotation and self-twisting are observed very rarely. In a transverse position of the fetus, only abdominal-wall CS in a planned manner should be considered a reasonable method of delivery. With an oblique position of the fetus, the woman in labor is placed on her side, corresponding to the location of the large part in the iliac region. With lowering, the pelvic end of the fetus often takes a longitudinal position. If the position of the woman in labor “on her side” does not correct the oblique position of the fetus, the issue should also be resolved in favor of a CS. Conducting a natural birth in a transverse position and the operation of turning the fetus on its leg are permissible only for a very premature fetus or during the birth of twins, when the second fetus lies in a transverse position.
Head presentation
It dominates the overall statistics, as it is typical for approximately 95% of cases. It is ideal if the baby is positioned with the back of the head towards the cervix. In this case, his chin is pressed to his chest and his head is tilted. The first point that passes through the birth canal is the small fontanelle, located at the junction of the parietal and posterior bones of the skull. In this case, there are two types of position of the baby. So, 1st position of the fetus is called anterior occipital presentation. It is characterized by the fact that the baby's face is turned back (in relation to the mother's body). The position is observed in 90% of pregnancies. It is the most optimal for a successful delivery.
There is also a 2nd position of the fetus, called posterior occipital presentation. In this case, in relation to the parent’s body, the face is turned forward. This makes the process much more difficult. During childbirth, the baby can get into the correct position, but this often takes a long time. The process may take a long time.
Types of cephalic presentation
These are not all forms of cephalic presentation. Among other things, it is divided into so-called extension types, when the toddler’s head is raised to a certain extent:
- Anterocephalic presentation. It has a slight degree of extension. The leading point is the large fontanelle, which is located at the junction of the frontal and parietal bones. In this case, it is possible to give birth naturally, but the process is much more difficult and longer. The thing is that the fetus's head enters the mother's pelvis with its largest part. In fact, this position of the baby is an indication for a caesarean section.
- Frontal position. Occurs in 0.5% of cases. If the baby is normal or large in size, its passage through the birth canal is impossible. Surgery is prescribed.
- Facial presentation is the maximum degree of extension of the fetal head. This situation is recorded in only 0.05% of births. The natural birth of a baby is possible, but it can be traumatic for both mother and child.
Head presentation and fetal positions
The anterior view of the occipital presentation in the first position of the baby is the most convenient option for normal childbirth. And fortunately, the most common. As already mentioned, in the first position the baby’s back is facing the left side of the uterus. In this situation, he moves “towards the exit” with the smallest diameter of his head. That is, it can easily transform, stretch and narrow in order to pass through the birth canal easier and faster.
If the baby's back is turned towards the right side of the uterus, this is already an occipital presentation in the second position. The situation is not so exemplary. In this case, the chances of developing the so-called clinically narrow pelvic syndrome increase. A woman experiences strong but unproductive contractions that suddenly slow down or stop altogether. In order for the baby to take a comfortable position - the first position, the woman needs to relax. This will make it easier for the baby to go down without colliding with the placenta if it is on the left or on the upper wall. The doctor will suggest the correct positions that will help the baby rise in the womb, turning the head and face to the right, and the back to the left.
Breech presentation
It occurs in 5% of cases. The position of the fetus in this case does not affect the birth process. Breech presentation can be different:
- The first position of the fetus is legs forward. In this case, the limbs are born first. To avoid this, the obstetrician delays the birth of the baby: he prevents his free movement with his hand. The limbs do not fall out. The toddler has the opportunity to turn his buttocks forward. If this happens, the birth will be less dangerous.
- The second position of the fetus during breech presentation is breech. It is more favorable for both the baby and his mother. Despite this, breech presentation itself is unnatural. In this case, the doctor recommends a cesarean section to many expectant mothers in order to protect the mother and her baby from unnecessary injuries and pain.
Is a caesarean section necessary?
Breech presentation is not a direct indication for surgery. The position of the fetus in this case is an additional, and not the main factor influencing the decision of the medical staff. Doctors consider the situation as a whole, taking into account other points:
- The age of the expectant mother, the size of her pelvis.
- The course of the woman’s previous pregnancies, characteristics of childbirth.
- Baby size. With a breech presentation, a fetus whose weight exceeds 3.5 kilograms is already large. With conventional ones, this figure is 4,000 kg.
- Gender of the baby. Oddly enough, but it is very important. It turns out that breech presentation is not dangerous for girls. But boys may have their genitals damaged during childbirth.
What to do in this situation?
If an ultrasound showed a breech presentation, a woman can change the situation before the 34th week. Having learned about the incorrect position of the fetus, she is obliged to perform some exercises:
- You need to lie on your right side and spend about 10 minutes in this position, then quickly turn to your left side. The exercise must be repeated 4 times in a row. It should be done several times a day before meals.
- It is recommended to stand in a knee-elbow position once a day for 15 minutes.
Swimming in the pool helps the baby turn over in the womb. Therefore, if you have the opportunity to buy a subscription, you need to take advantage of it. When the baby turns over on its head, be sure to wear a bandage for several weeks to fix its position. If this does not happen, the expectant mother is sent to the hospital two weeks before giving birth. There, doctors make decisions about how the process will proceed. By the way, doctors used to try to manually turn the baby over while massaging the pregnant woman’s belly. But then this method was abandoned due to the high risk of complications: premature birth, placental abruption, and disruption of the baby’s condition.
Exercises to correct abnormal types of baby presentation
If, after thirty-two weeks, a pregnant woman is found to have an abnormal position of the baby, doctors may recommend performing useful exercises that will encourage the fetus to assume a normal position for childbirth. However, it is worth remembering that sometimes there are individual characteristics of the female body or child that can prevent the baby from turning into the correct position, despite the quality of the exercises performed by the woman.
There are also restrictions on performing gymnastics by a pregnant woman:
- risk of untimely birth;
- placenta previa.
If there are no restrictions, a woman can try doing simple exercises:
- Lie on your side on a hard surface. Lie down for 12–15 minutes on one side, then turn over to the opposite side and lie down for the same amount of time. You should roll over from one side to the other at least three times in one approach. It is worth performing these manipulations two to three times a day. The effectiveness of simple actions is often high and the result appears already in the first 5–7 days.
- Lie on your back, place blankets under your legs and lower back so that your legs are 25–30 cm higher than your head. You need to lie in this position for 20–25 minutes, 1–2 times a day.
- Take a knee-elbow position on the floor and stay in this position for 20–25 minutes. The exercise should be performed 3-4 times a day.
It is recommended to stay in this position for at least 20 minutes per approach. - Exercise “Cat”, for which you initially also need to take a knee-elbow position. While in the starting position, bend your back up in the lumbar region, then straighten your back without bending down. The exercise must be performed 15–20 times in one approach, 2–3 times a day. “Kitty” is useful for all pregnant women who have no contraindications; when performing this exercise, the uterus is saturated with oxygen.
- Stay in a standing position or slightly leaning forward for longer than usual.
- Try to sleep on the side where your baby's head is.
- Swim on your stomach and back.
Swimming helps turn the fetus head down - Starting position: standing, feet shoulder-width apart, hands on the belt. Perform slow bends forward and backward. Inhale while standing, exhale while bending over. It is recommended to perform 10–20 smooth bends in one approach.
- The starting position is the same. Perform smooth bends to the side. As you inhale, be in a horizontal position and raise your arms up; as you exhale, lower your arms and tilt to one side. It is worth performing 10 bends in each direction at a time.
When performing any of the exercises, a pregnant woman should not experience discomfort, severe physical exertion or pain. To achieve the best effect, it is recommended to perform gymnastics no earlier than 2-3 hours after eating. Movements help increase the tone of the uterus and stimulate the baby's motor activity.
People say that you can help your baby roll over using a headphone with music or a light source placed on the lower abdomen. They say that the baby, even in the womb, begins to pick up sounds and changes in lighting and, out of curiosity, can turn towards an external stimulus.
If the mother’s efforts were not in vain and the child, with the help of physical exercises, nevertheless took the necessary position, it is worth helping him remain in a natural presentation. First of all, for this you need to wear a bandage. The bandage should be put on while lying down and worn for at least half a day. It also makes sense to do a couple of simple exercises:
- sit on the floor, bend your knees and bring your feet together. Press your knees to the floor as much as possible and sit in this position for 5-15 minutes;
- sit on a chair, press your feet to the floor. Slowly raise your bent legs up 20–30 cm, and then lower them to the starting position. It is recommended to perform 20–30 repetitions in one approach.
It also happens that the baby independently turns over into a natural position for childbirth in the last weeks of pregnancy. Still, nature takes its toll and there is no need to panic ahead of time.
That's what happened to my friend. After 32 weeks, she was informed that the baby was in a breech position. She began to do physical exercises to make the child turn over, but they did not bring results. And a week later, after the girl stopped doing gymnastics, at the next ultrasound she was pleased that the fetus had turned head down.
Oblique or transverse arrangement
In this situation, it is impossible to determine the presentation of the fetus. The position is a direct indication for cesarean section. Oblique or transverse position of the baby in the womb occurs in 0.4% of cases. And if earlier during childbirth doctors tried to grab the baby by the leg and turn him over, today this method is not used. The technique turned out to be quite traumatic for both the baby and his mother. Sometimes a revolution is performed during the delivery of twins. But only in the case when the first child was already born, and the second suddenly took on a transverse position.
The reasons for the oblique or transverse position of the fetus may be different. Among the main factors are tumors in the uterus and fibroids. The formations prevent the toddler from lying in a natural position. Sometimes this happens when the child is very large or a short umbilical cord is wrapped around his neck: it limits his movements. Another reason is the multiple births a woman has had, when her uterus suffered from numerous stretches. With an oblique or transverse position, a woman needs to perform all the same exercises as with a breech presentation. In this case, it is also recommended to lie more time on the side towards which the baby’s back is turned. The woman is hospitalized 3 weeks before the expected birth. And if the situation has not changed, she is prepared for surgery.
Indications for caesarean section
The presence of disorders or diseases in both the woman and the fetus can lead to delivery by cesarean section. Indications for women: genital cancer or herpes, myopia, severe symphysitis, narrow or deformed pelvis, severe scars on the uterus or vagina, tumors in the uterus, severe diseases of the heart, kidneys, lungs, the presence of transplanted organs, eclampsia.
From the side of the fetus or placenta: malformations of the child (omphalocele, gastroschisis), chronic hypoxia, developmental delay, transverse or pelvic presentation of the fetus, as well as malformation of the head, Siamese twins or twins, triplets, etc., large fetus, etc. complete or incomplete placental abruption.
If gynecologists have recommended that a woman give birth not naturally, but by caesarean section, then she needs to go to the maternity hospital several weeks before the expected due date.
Position of fetuses in twins
The position and appearance of the fetus are determined during routine ultrasound diagnostics. Sometimes, during such research, future parents learn about a surprise prepared for them by nature: they will have twins! After the euphoria, they begin to think about whether natural delivery is possible in this situation. Of course, this is quite possible, but only in two cases: if both babies are in a cephalic presentation or the baby who is closer to the cervix has this position, and the other is positioned with his buttocks forward. When the leading baby has a “pelvic position,” a cesarean section is recommended. The thing is that during the birth of the buttocks of the first-born, children in the womb can get their heads caught, which is fraught with injury. It is clear that in an oblique or transverse position, surgical intervention cannot be avoided. And even if twins are in the correct position in the womb, the decision on the method of delivery is made by the medical staff, taking into account many factors.