What to do if placental abruption occurs
This dangerous condition requires therapy. To begin treatment for placental abruption, you should consult a specialist. Treatment in a hospital setting is often required.
Treatment
In some cases, a decision is made to refuse emergency delivery:
- If the condition does not worsen, there is no progression of detachment.
- There is no dangerous condition when oxygen is not supplied to the child.
- There is no discharge, the volume of blood lost is not dangerous.
- The woman is being observed by doctors in the hospital.
In case of detachment, medications can be prescribed to stop bleeding, prevent spasms, as well as hormonal medications and drugs to treat anemia.
It is possible to reduce the likelihood of a pathological condition occurring. So, you need to undergo a comprehensive examination to make sure that there are no chronic pathologies that can be cured before conception.
All medications are taken with the doctor's permission
Pregnant women should stop smoking and drinking alcohol, and it is important to eat right
Uncontrolled use of medications can increase the risk of miscarriage, leading to complications for the mother's body. Do not despair, since emotional peace is an integral part of the treatment of retrochorial hematoma. You cannot take measures on your own at home, regardless of the severity of symptoms and other factors, you need to consult your doctor.
At the appointment, the gynecologist will use an ultrasound machine to determine the size of the hematoma and prescribe the appropriate treatment. There is no treatment algorithm for mild forms. The scope of assistance boils down to observation and the prescription of general strengthening drugs - multivitamins, ascorbic acid, vitamins E and group B.
In severe cases, emergency hospitalization will be required. Uterine bleeding is an indication for surgical treatment of hematoma. It is possible to terminate a pregnancy in order to save the woman’s life. Self-medication with drugs and folk remedies is contraindicated in this situation - there is a high risk of developing complications, often incompatible with life.
General recommendations:
- gentle regime of work and rest;
- inclusion of cereals, fruits, vegetables in the diet;
- avoidance of products that cause gas formation;
- abstinence from sexual intercourse;
- psycho-emotional peace.
If a woman finds it difficult to control her emotions, then sedative teas based on mint and chamomile, as well as Valerian tablets, are prescribed.
Consequences
The consequences depend on the condition of the mother’s body and her timely actions - identifying symptoms, contacting a gynecologist and starting treatment in a hospital. Directly depend on the severity and shape of the hematoma. In mild forms, it resolves or comes out completely quickly. Having seen the discharge, the woman goes to the doctor, but the ultrasound shows no complications - the danger to termination of pregnancy and the life of the mother has receded.
In moderate and severe forms, the following complications may occur:
- uterine bleeding;
- termination of pregnancy (miscarriage);
- pelvic inflammation - infection with secondary infections in the presence of chronic lesions.
In order to prevent the development of complications and adverse consequences, it is recommended to undergo repeated diagnostics after treatment.
What to do?
If brown discharge appears, a pregnant woman should under no circumstances engage in self-diagnosis. All of the above is nothing more than material for self-education for reference purposes, and not a guide for making any diagnoses for yourself.
There are not many variants of the physiological norm for this type of vaginal secretion, but there are more than enough variants of pathologies. For this reason alone, a woman should immediately see a doctor. An ultrasound scan, a vaginal smear, as well as blood and urine tests will help find an accurate answer to the question of why blood appeared in the secretions of the genital tract.
If the discharge is scanty and not accompanied by pain, you should consult a doctor at the antenatal clinic at your place of residence. If the brown discharge is abundant, with clots, and pain, then you should go to bed, avoid standing or walking, and wait for an ambulance to be called immediately.
Visiting doctors must be told the duration of pregnancy (from the first day of the last menstruation), describe in detail all the symptoms, including even the most insignificant ones, in your opinion, and also tell about all previous pregnancies and their outcome. All this information will help doctors quickly guess the cause of the bleeding and take you to a gynecological hospital or the emergency department of a maternity hospital with the most accurate formulation of the problem. Every minute can be decisive; it is necessary to help doctors understand you correctly.
If brown discharge recurs sporadically, you should tell the observing obstetrician-gynecologist about this so that he can give the most complete and accurate recommendations regarding the expectant mother’s lifestyle, daily routine, work and rest, the ability to have sex, and also prescribe the necessary supportive treatment depending on the condition. causes.
If there is a threat of miscarriage due to low placentation, antispasmodics are prescribed that relax the muscles of the uterus and prevent its tone, as well as vitamins, drugs to improve uteroplacental blood flow and light herbal sedatives. After hospital treatment, a woman may be prescribed hemostatic drugs. For hormonal problems and a lack of progesterone, certain dosages of hormonal drugs are recommended that completely compensate for the deficiency in the body.
Causes
Depending on the period at which the hematoma appeared, 2 types are distinguished in obstetrics. Retrochorial - formation is typical for early stages, diagnosed before 14-16 weeks. The fertilized egg detaches from the uterus, resulting in a space filled with fluid or blood clots.
Retroplacental - accordingly, occurs after 16 weeks, when the placenta is fully formed and performs vital functions for the fetus. Detachment of the baby's place can lead to the onset of premature birth, disruption of nutrition and oxygen supply, and intrauterine growth retardation.
Both obstetric and non-obstetric factors can provoke a dangerous pathology. Therefore, the physical and mental health of the expectant mother at the time of conception is of decisive importance; the planning stage will reduce the risks of deviations during the pregnancy process.
Causes of hematoma:
- hormonal disorders, diseases of the endocrine system;
- autoimmune diseases that affect blood flow;
- congenital anomalies of the uterus;
- inflammatory processes;
- diseases of the pelvic organs;
- injuries;
- pregnancy immediately after an abortion;
- age after 35 years;
- toxicosis, gestosis;
- stress, depression, nervous shock;
- embryo development abnormalities;
- multiple pregnancy;
- A woman’s lifestyle is smoking, drinking alcohol, working in hazardous industries, living in an environmentally unfavorable area.
Hormonal deficiency
Monthly menstrual bleeding is controlled by hormones. In the second half of the cycle, progesterone gradually decreases, the concentration of estrogen increases and menstruation begins. Do not think that menstrual-like discharge during pregnancy is normal. As a rule, this happens in the first months after conception due to a lack of progesterone.
Of course, there are rare situations in which menstrual bleeding during pregnancy can be considered normal. This happens if a woman produces two eggs in the current cycle instead of one, and ovulation occurs twice with a difference of several days. In this case, the first egg was not fertilized, it died and dropped into the uterus, and the second was fertilized and went to the uterus for implantation.
Bloody discharge will come on the day of the expected menstruation, but such periods will differ significantly. First of all, there will be little discharge. In a few days, scanty and incomprehensible periods will stop and will not recur over the next 9 months. People used to say about this phenomenon that “the fruit is washed,” but in practice this rarely occurs.
With hormonal deficiency or imbalance of hormones in the body, the discharge resembles slight pale brown marks on underwear or a thin sanitary panty liner. They may intensify slightly or disappear completely, after which they appear again.
How to recognize pathology?
There are several characteristic signs, when they appear, a girl can be sure that she has developed this pathology:
- The state of health worsens - a feeling of vomiting appears, which is easily confused with toxicosis, headache and weakness.
- The most obvious symptom is discharge during pregnancy. The clot constantly accumulates, causing bruising.
- You can feel a nagging pain in the lower abdomen, which does not stop when you change position.
- The woman begins to feel anemia in the extremities.
- The patient becomes short of breath.
At the earliest stage of hematoma development, no associated symptoms may appear. The expectant mother feels well and is enjoying her pregnancy. The presence of this pathology can only be recognized by doing an ultrasound.
Related and recommended questions
Discharge during pregnancy is beige-brown Dear doctors! Pregnancy 19 weeks...
Beige light brown discharge I am pregnant, exactly 6 weeks pregnant. This night…
Brown discharge at 8 weeks I'm 8 weeks and 1 day pregnant. Yesterday morning…
Brown discharge after orgasm during pregnancy Hello. I'm 10 weeks...
I don’t know what to think, is there pregnancy and fibroids? Help me please! I live sexually...
Hypertonicity Pregnancy 11 weeks. Periodically there are pains in the lower abdomen and brown...
Pregnancy 10 weeks, brown discharge Pregnancy 10 weeks, registered...
Dark discharge after placental abruption On September 25, slight bleeding began….
Stomach aches at 7 weeks of pregnancy. I would really like to hear your opinion! I am pregnant….
Discharge after a hematoma At 5 weeks of pregnancy I was admitted to the hospital with severe detachment...
Brown discharge in early pregnancy Dear doctor! Pregnancy…
Pregnancy, discharge, stomach ache. I’m pregnant, hCG is 3 weeks. Tell me please,…
Threat of miscarriage My pregnancy period from the day of conception is 4 weeks. A couple...
Delayed menstruation brown discharge I started having sex on June 10th of this year...
Discharge, pain in the right side. The right side hurt and radiated to the lower back, then the same...
Brown discharge after hematoma detachment My name is Svetlana, I’m pregnant 9-10...
Brown discharge during pregnancy I am 12 weeks pregnant. At 5 weeks she went to bed...
VERY URGENT! Is brown discharge dangerous during pregnancy? I'm pregnant for a short time...
Scanty dark brown discharge instead of menstruation. March had unprotected sex, which...
Bloody discharge and abdominal pain after menstruation I have the following situation: After...
Diagnostic measures
If such a negative phenomenon as a hematoma is detected, the patient must consult a gynecologist. To confirm the diagnosis, a specialist will prescribe the following diagnostics:
- A repeat ultrasound examination will be required to confirm the diagnosis. It is advisable to do this in a paid clinic where there is high-quality equipment. This will allow you to better determine the presence and size of a hematoma during pregnancy.
- During the examination, the obstetrician-gynecologist will take a smear on the flora and determine the nature of the discharge during pregnancy.
- It is mandatory to take the necessary tests (feces, urine, blood from a finger, blood from a vein).
Based on the results of this diagnosis, it is possible to determine whether there is a pathology that may threaten the full development of the fetus. If necessary, urgent treatment will be prescribed.
Hematoma. Description, reasons
Hematoma. What exactly is this? This is an accumulation of blood/bruising/bruising due to damage to soft tissues, disruption of the integrity of blood vessels. Bruises, blows, physical injuries are the root cause.
A hematoma in the uterus is a potential risk to the life of the child and the health of the mother. There may be several reasons for its formation:
- the phenomenon of severe toxicosis;
- inflammatory processes;
- infectious lesions of the genitourinary system;
- inflammatory processes of the uterus, diseases of the endometrium (inner mucous membrane of the uterus);
- stress;
- pathological changes;
- hormonal “changes”;
- thrombophilia (risk of thrombosis, impaired coagulation - the result of poor blood clotting);
- arterial hypertension;
- addiction to alcohol, drugs, tobacco;
- high surges of noise, vibration;
- genital infantilism (underdevelopment of the genital organs).
Consciously follow the recommendations of specialists; you should be attentive to sensations; do an ultrasound in a timely manner; provide honest information about yourself and your partner; not hiding the presence of genetic diseases is a mandatory, important step for a pregnant woman.
Causes
The reasons for the formation of retrochorial hematoma are similar to the factors that cause the threat of miscarriage:
- mechanical impact on the uterus (injuries, bruises);
- hormonal disorders (lack of progesterone);
- genetic abnormalities of the fetal egg (gross malformations);
- stress;
- heavy physical activity;
- inflammatory and tumor diseases of the uterus (endometritis, endometriosis, fibroids);
- sexually transmitted infections;
- occupational hazards (noise, vibration, radiation);
- early and late toxicosis;
- sudden jumps in blood pressure;
- infantilism and abnormalities of the genital organs;
- drinking alcohol and drugs, smoking;
- systemic diseases (systemic lupus erythematosus, collagenosis and others);
- chronic somatic diseases (diabetes mellitus, cardiovascular pathology and others);
- diseases of the blood coagulation system;
- disturbed ecology.
They also include diseases associated with vascular pathology, including the vessels of the uterus.
Other gynecological problems
Inflammatory diseases of the reproductive and genitourinary system during pregnancy are not at all uncommon. The expectant mother's immunity is significantly reduced (and this is also due to progesterone!), which is why any fluctuations in the balance of microflora can cause local inflammation.
If a woman had chronic diseases of the genital organs or organs of the urinary system before the onset of the “interesting situation,” then during the period of maximum decrease in immunity, by the middle of pregnancy, they may well make themselves felt. Many inflammatory processes of non-infectious origin occur with the release of vaginal secretion of a yellow, light brownish hue.
Diseases of infectious origin cannot be excluded. These can be sexually transmitted infections, as well as sexually transmitted diseases. Many of them have a fairly long incubation period, so at the time of registration, the examination may not reveal pathology, and real symptoms will appear later.
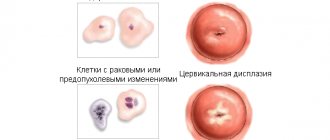
The most dangerous are brown and brown discharges, which have greenish purulent impurities, as well as an unpleasant and pungent odor. They indicate the bacterial origin of the problem, which, if not treated in a timely manner, can result in intrauterine infection of the fetus and even its death. Brown spotting discharge may indicate problems with the cervix and inflammation of the cervical canal.
After IVF
If a couple has had to resort to assisted reproductive techniques, such as IVF, they should be prepared for the discharge to be significantly different from that normal for a natural pregnancy. So, after transferring embryos for almost two weeks, brownish ones are considered a normal variant. This is the reaction of the female body to hormonal therapy, which she underwent before embryo transfer and continues after it.
Brown spotting vaginal discharge may also indicate successful implantation. If they are a sign of implantation, then usually brown streaks or scanty daubing appears 5–6 days after hatching. In a third of women, a change in the color of the vaginal secretion appears only 8–10 days after replantation.
But there is no need to despair, because after analyzing the concentration of the hCG hormone in the blood, treatment will be prescribed that will help maintain the pregnancy and bear a healthy baby, maybe several babies. In the worst case, brown discharge after two weeks from the moment of replanting may indicate that the embryos have stopped developing and their rejection has begun. After treatment, the IVF attempt can be repeated.
Bruises on the skin in pregnant women
Subcutaneous and intramuscular bruises are not so dangerous for the health of expectant mothers, but they should also be shown to a doctor. Stages of development of subcutaneous or intramuscular hemorrhage:
- painful sensations appear at the site of injury;
- the injured area of skin swells slightly;
- the color of the skin first becomes blue, then purple, greenish shades or yellowness appear.
It is useful to know how to take Femoston 2-10 for pregnant women.
Note: how Time Factor works and why it is recommended to take it when planning a pregnancy.
Bruising does not appear as a result of bruises. This is a consequence of a lack of vitamins and minerals that affect the condition of blood vessels. Weak and brittle capillaries are injured on their own, forming small hemorrhages in the subcutaneous layer. If measures are not taken, the problem will spread to large vessels, which will increase the risk of developing varicose veins or internal bleeding.
Photo of cyanosis on the belly of a pregnant woman around the navel.
Causes of bruises during pregnancy:
- the age of the expectant mother (the older the woman, the weaker her blood vessels);
- lack of vitamin C (the walls of blood vessels become like a sieve);
- lack of vitamin K (blood clotting decreases);
- there is not enough calcium, selenium and cobalt, on which the elasticity and strength of the walls of blood vessels depends.
In addition, there are various diseases that provoke the formation of bruises:
- blood clotting disorder;
- hemophilia;
- liver diseases;
- taking certain medications (Aspirin, Analgin, Nurofen).
Only a doctor, after examination and tests, can determine the exact cause of hemorrhages. Do not delay your visit to the gynecologist.
Abdominal muscles and pregnancy
When preparing for conception, women sometimes forget about the need to normalize their abdominal muscles. In people who are far from sports, the abdominal muscles are unevenly developed and in some places are greatly weakened. There is an area around the navel that has virtually no connective tissue. This is where a hernia can form - a protrusion of internal organs through weak muscles of the abdominal wall.
In the case when a bruise on the abdomen is accompanied by pain, the formation of a hernia can be suspected. If vomiting, flatulence, constipation appear, the heart rate increases, and a painful bulge forms on the abdomen, you should call an ambulance and call your gynecologist. In this case, no independent actions can be taken. Only consultation with a specialist, and immediately.
Also, a blue spot around the navel may signal that, under the influence of the growing fetus, the muscles in this place are diverging. To prevent bruising on the abdomen during pregnancy, it is recommended to wear a carefully selected bandage that fits the body.
Important! You cannot tighten the bandage too much, it should only support the tummy. You also can’t loosen it too much - the bandage will stop performing its functions. Ideally, a pregnant woman should feel comfort and relief; there should be no pressure or other unpleasant sensations.
How to treat hematoma during pregnancy
/sineaki_i_gematomi/gematoma-pri-beremennosti-kakie-byvayut-podvidy-kak-lechit.html
- Doctors recommend reducing physical activity. Lifting heavy objects can cause bleeding in the uterus. Such women are advised to remain in bed.
- Nutrition should be balanced. Be sure to include vegetables and fruits in your diet.
- To stop bleeding, the patient is prescribed vikasol, ascorutin and dicinone.
- Means designed to relieve spasms help relieve pain from a hematoma. Such drugs include paraverin and no-shpu.
- The lack of vitamins in the body of the expectant mother can be compensated by taking special vitamin complexes.
- It is necessary to ensure the outflow of blood from the female genital area. When lying down, a pregnant woman's pelvis should be higher than her head. This can be done by placing an additional pillow on it.
- To relieve spasms in the uterus and relax tense muscles, you can use Magne B6. However, it should not be taken by patients who have kidney problems.
- Actovegin helps with poor circulation in the area of the hematoma. Before taking it, be sure to consult your doctor. It is contraindicated in heart failure, pulmonary edema and kidney disease.
- Curantil helps normalize blood circulation and eliminates the lack of oxygen in fetal tissues. The drug thins the blood and prevents the formation of blood clots.
- With a hematoma, the risk of miscarriage increases. Hormonal drugs are designed to combat this threat. After treatment with duphaston, the likelihood of premature birth can be reduced.
How to prevent hematoma - preventive measures
The appearance of this unpleasant complication can be avoided if the expectant mother leads a healthy lifestyle and is attentive to her new condition.
Main preventive measures:
- Rejection of bad habits. If a woman smoked before conception, then during the period of bearing the baby and feeding him, you should forget about smoking.
- Timely treatment of infectious viral diseases. Gestation is not the time to experiment with your health.
- Maximum compliance with the doctor’s instructions if there is a risk of developing retrochorial pathology. In this case, you need to stay in bed and avoid physical and emotional stress. It is recommended to lie with a bolster or pillow under the pelvic area to drain the blood.
- Avoid bruises, injuries and falls.
- Do not lift or carry heavy objects.
- Monitor your diet. It is necessary to consume foods rich in vitamins that stabilize the functioning of the gastrointestinal tract and cardiovascular system. It is advisable to exclude foods that cause constipation and gas formation in the intestines.
- Do not delay registration. The earlier the pathology is identified, the easier it will be to overcome it without consequences.
Watch an informative video on the topic of miscarriage:
How quickly does it resolve?
The size of the bruise and the severity of the pathology are diagnosed using ultrasound, Doppler, blood and urine tests. Inpatient treatment may be recommended at the earliest stages (5-6 weeks) and throughout the entire gestation period.
Complex therapy is aimed primarily at stopping bleeding, reducing the size of the hematoma and eliminating tension in the tone of the uterus. The doctor may prescribe hemostatic drugs (Vikasol, Ascorutin, Dicynon, vitamin C) and antispasmodics (Papaverine, Metacin or No-shpa).
Vitamin and mineral supplements, Magne B6 and sedatives (Novopassit, infusions of valerian, peony or motherwort herb) help strengthen the nervous system.
To reduce the hematoma, it is necessary to normalize the functional state of the endometrial mucosa; the most effective medications are Duphaston and Utrozhestan.
The homeopathic remedy Wobenzym promotes the resorption of hemorrhages in the uterine cavity.
Antithrombotic drugs (Clexane and Actovegin) help fight hypoxia and improve fetal nutrition.
If the attending physician recommends bed rest, it is important to arrange the correct position of the body - with the lower part elevated (a bolster under the legs and a pillow under the pelvic area). It is better to abstain from intimate relationships for the entire period of treatment
Physical activity, overwork and stressful situations are contraindicated. You should organize a rational daily routine and adhere to healthy eating rules
It is better to refuse intimate relationships for the entire period of treatment. Physical activity, overwork and stressful situations are contraindicated. You should organize a rational daily routine and adhere to the rules of a healthy diet.
How long it will take for the hematoma to resolve depends on the degree of pathology and compliance with the recommendations of the attending physician.
Diagnostics
The main diagnostic method for retrochorial hematoma is ultrasound of the uterus and ovum.
During this procedure, the following signs are detected:
- local thickening of the uterine wall, which indicates an increase in uterine tone (short-term hypertonicity is possible when performing an ultrasound with a vaginal sensor, in which case it is necessary to repeat the ultrasound with a transabdominal sensor, that is, through the anterior abdominal wall. Continued muscle tone indicates a threat of termination of pregnancy);
- change in the shape of the fetal egg due to pressure on it from a thickened area of the myometrium (the fertilized egg takes on a scaphoid or teardrop shape);
- detection of retrochorial hematoma, clarification of its size, location and increase or decrease during repeated examination.
In addition, the following laboratory tests are required:
- general blood and urine tests;
- blood for clotting (platelets, bleeding time, fibrinogen, prothrombin and other factors);
- vaginal smear for flora;
- blood chemistry;
- screening for sexually transmitted diseases;
- hormone research (according to indications);
- CTG and Dopplerometry of the fetus in late pregnancy.
How, besides miscarriage, is a hematoma dangerous?
The consequences of the formation of gaps between the feeding organ and the wall of the uterus are different. If it is mild, it may only slightly slow down the child's growth and development. The situation is sometimes revealed only after childbirth in the form of bruises on the placenta.
With moderate severity of hematoma in the 1st trimester, the anomaly can seriously alter the normal formation of organs. The embryo does not receive enough nutrition, but also oxygen, which greatly affects the functioning and formation of the brain.
Extensive hematomas, the contents of which exceed 20 ml, can lead to developmental abnormalities. With a “bruise” that separates the uterus and placenta by 40% or more, the child noticeably lags behind in intrauterine development. Thus, one of the parameters - CTR (size from the coccyx to the crown) may lag by 10 or more days.
With severe pathology, uteroplacental apoplexy sometimes develops—Kuveler's uterus. This is a condition in which the hematoma extends into the myometrium. The muscles of the organ lose their contractile abilities, the wall becomes covered with cracks. In this case, the bleeding is directed into the abdominal cavity, and the vaginal discharge is spotting. The patient feels severe pain. In such a situation, an emergency caesarean section is prescribed, and the uterus can only be saved in some cases. If you do not seek medical help, the woman will die from bleeding.
In some cases, partial placental abruption with the formation of a hematoma leads to intrauterine death of the child. In this case, a woman may notice a lack of movement in the later stages, as well as brown spotting.
How much does it cost?
Retrochorial hematoma appears in the early stages of pregnancy - about 5-8 weeks of embryogenesis. There are 3 forms:
- light;
- average;
- heavy.
In a mild form, the hematoma can resolve on its own or come out during the day in the form of brown discharge (the woman sees coagulated blood). Also, the discharge may be spotting and observed for about 2 weeks in small portions. If discharge accompanies pregnancy for a long time, but there are no other symptoms, then you should seek medical help.
In the moderate form, nagging pain appears in the lower abdomen and the amount of discharge will be significantly greater than in the mild form. Sometimes it is even possible to confuse the release of a hematoma with menstruation, given the presence of nagging pain in the lower abdomen, which can be dangerous in an undiagnosed pregnancy. Here the release time is longer - up to 5 weeks. The pain is intense, so women often take painkillers or antispasmodics, often without a doctor’s prescription, which is fraught with the development of complications for both mother and child.
Important information: Instructions for using ointment (cream) for bruises and contusions Ambulance
In a severe form, if the hematoma has come out of the uterus, but heavy scarlet discharge appears, indicating bleeding, you need to urgently seek medical help. General weakness, malaise, and dizziness may appear due to the sudden loss of a large amount of blood. The condition is urgent and requires hospitalization under medical supervision.
Norm
A small amount of blood in the discharge in the very early stages may be the norm when a fertilized egg is implanted into the uterine cavity. This phenomenon is called implantation bleeding. It occurs due to a violation of the integrity of the endometrium during the attachment of the blastocyst. One of the options for such natural bleeding may be light brown discharge in a small amount approximately 8-9 days after the expected conception (or after ovulation - for ease of calculation).
Brownish spotting on panty liners or underwear is not long-lasting. Usually within a day or two there is no trace left of them. There is nothing alarming about this phenomenon.
In addition, such an early sign of pregnancy does not appear in every woman. You should know that the appearance of dark brown discharge with clots before the delay can hardly be considered a sign of implantation. Rather, we are talking about a hormonal imbalance that began ahead of schedule. During the first 2–3 months of pregnancy, yellow-brown, moderate or scanty discharge may be a consequence of global hormonal changes.
Progesterone raging in the body of the expectant mother usually gives the vaginal secretion a yellowish tint; brown “notes” in it can appear due to high or low levels of progesterone, due to the vulnerability of the genital tract due to looseness under the influence of hormones. Normally, such discharge occurs without pain, it does not contain inclusions or impurities, or streaks of blood, and does not bother the woman. They usually stop after the expectant mother’s body has fully adapted to the new situation and circumstances.
In the later stages (a week or two before the expected date of birth), a woman may notice the appearance of brown, streaked discharge. They are usually accompanied by the release of mucus in small quantities or a rather impressive clot.
In this case, we are talking about the removal of the mucous plug, which during pregnancy closed the cervical canal and prevented the penetration of anything foreign and dangerous into the uterine cavity where the baby grew.
Small brown discharge after sex or a doctor’s examination is also normal. Their reason lies in the extreme vulnerability of the pregnant woman’s genital tract. Under the influence of progesterone, they become loose and vulnerable to even minor mechanical stress.
Such discharge usually does not last long - no more than a day, and is not accompanied by any unpleasant sensations or additional symptoms. There are no clots in them, they do not intensify, their number changes in a descending manner. These are the three main reasons why brown discharge can be considered normal. All other situations, alas, relate exclusively to pathological ones.
Consequences of the disease
From the moment a blood clot appears until delivery, the woman is under close medical supervision. If she strictly follows all the recommendations, the prognosis is positive. In most cases, with adequate and timely treatment, the blood clot comes out on its own or resolves without harming the growing baby.
Without timely medical assistance, a retrothecal hematoma during pregnancy leads to:
- intrauterine fetal death;
- uterine bleeding;
- miscarriage;
- abnormalities in child development;
- placental abruption at 8-9 months.
If no measures are taken, the bleeding will not stop, which means the tumor will increase in size, threatening the safety and normal course of the gestation period.
Signs and symptoms
Signs of hematoma formation in the uterus during pregnancy can manifest themselves as follows:
- constant weakness and fatigue;
- periodic pain that appears in the lumbar region;
- a feeling of discomfort in the lower abdomen, as during menstrual bleeding.
With a retrochorial hematoma, a woman may experience uncharacteristic vaginal discharge. They can be spotting or moderate. Intense bleeding most often indicates an incomplete or complete miscarriage.
The scarlet color of the discharge is considered a dangerous symptom, because... it characterizes the formation of a blood clot and an increase in its size. Dark red, brown or black vaginal secretions are an indication that gravid hemorrhage is decreasing.
Some women find out what a retrochorial hematoma is only after childbirth, when the doctor examines the placenta and identifies an area on its wall where there was hemorrhage. Most often, the pathology is not diagnosed during pregnancy due to its small size and the absence of symptoms of the disease.
Symptoms
There are no characteristic symptoms confirming that a retrochorial hematoma emerges during pregnancy. The condition is similar to uterine bleeding, menstruation. Clinical manifestations largely depend on the severity of the pathological process. The severity of the condition can only be reliably determined using ultrasound diagnostics. Symptoms of hemorrhage in the uterus can be mild or intense, but even slight suspicions of pathology are a reason to seek qualified medical help.
Important information: Instructions for using badyagi in the form of gel powder for bruises (contusions) and how often to apply ointment (cream) to the face
With a hematoma, you may notice the following symptoms:
- nagging pain in the lower abdomen;
- discomfort in the pelvic area;
- periodic sharp and cramping pain in the suprapubic region;
- temperature increase;
- bloody, red or brown discharge (depending on how old it is and the presence of bleeding vessels at the site of amniotic sac detachment).
Vaginal discharge appears when the hematoma is emptied, when blood begins to gradually come out. A sign of improvement in the condition is precisely the appearance of dark discharge, while the presence of scarlet blood indicates an increase in the area of detachment. All these processes can be detected using ultrasound.
A hematoma during pregnancy may resemble the symptoms of menopause. Often occurs in women after 45 years of age, when pregnancy becomes unplanned, and its symptoms, including pregnancy, are perceived as manifestations of premenopause. Brown spotting, weakness, drowsiness, mood swings, nausea, discomfort and pain in the pelvic area should not be left unchecked by a specialist.
How is placental abruption treated?
If a small hematoma is detected, the woman will be prescribed sexual and household rest, as well as vitamins. The gynecologist monitors such a patient more vigilantly.
When multiple small formations or detachment that threatens the development of the fetus are diagnosed, analogues of female progesterone are usually prescribed. These are the drugs Utrozhestan or Duphaston.
In case of bleeding and serious hematoma, hemostatic agents are prescribed - Tranexam, Vikasol, Dicynon, as well as antispasmodics to relieve the tone of the uterus - Papaverine, No-shpa.
In each case, medications are selected individually. If there is even the slightest threat to the state of pregnancy or the life of the mother and child, then the woman is hospitalized, undergoing treatment and observation in a hospital setting.
After discharge, the ban on too active life, sexual relations and hard work remains. During this period, it is very easy to provoke a relapse of the pathology.
Treatment of hematoma
When brown discharge appears, the doctor evaluates the condition of the placenta using diagnostics. It also finds out the causes of the pathology. In case of mild severity, a woman is prescribed Utrozhestan or Duphaston, which replenish progesterone in the body and will help save the child. Vitamin C, E, group B, Ascorutin, complexes are also prescribed.
If the patient’s condition threatens serious consequences, then she is sent to the hospital. The woman is prescribed bed rest and complete rest. The hospital administers injections with No-shpa, Papaverine, Dicynon, Vikasol, Tranexam and others, depending on the situation. These drugs relieve the tone of the uterus and stop bleeding.
To establish normal blood circulation in the brain and prevent oxygen starvation of the fetus, Curantil and Actovegin are used.
Attention! The necessary drugs are selected individually. Self-medication in this case is dangerous.
It is equally important to avoid straining during emptying, as well as increased gas formation. Therefore, the patient is recommended to eat a diet that prevents constipation and flatulence. Staying on the toilet for a long time and straining can increase bleeding and increase the hematoma. You can use safe laxatives, such as microenemas, to make bowel movements easier. Sexual relations are excluded during the period of threat due to the mechanical impact on the organs.
Forms of hematomas
In general, the concept of hematoma implies the accumulation of blood, bruising or bruising resulting from soft tissue bruising or disruption of the integrity of blood vessels. A hematoma in the uterus is a hemorrhage in this organ.
Retrochorial hematoma is a mild form of the disease, which is usually not characterized by specific symptoms and most often goes unnoticed. Retrochorial hematoma during pregnancy involves detachment of the fertilized egg from the chorion.
At the 16th week of gestation, the stage of placenta formation is completed, which is why this type is called uterine hematoma during pregnancy in the first trimester. Only a specialist can diagnose the disease, based on the symptoms, medical history and test results. To clarify, it is useful to know about the existence of such a term as subamniotic hematoma in pregnant women. This disease is not so common in practice, but is characterized by spontaneous resorption, without requiring specific treatment.
Therefore, it is so important to know the differences between the above-mentioned diagnoses.
It is also useful to have an idea of the term retroplacental hemorrhage. This is an advanced form of the disease, when the stage of detachment of the fertilized egg from the placenta has already begun. In this case, the degree of risk and adverse consequences for the pregnant woman and child increases.
Diagnosis and recovery of hematoma
Ultrasound examination is the only way to reliably diagnose hemorrhage inside the uterus. After all, the disease is not always detected by the symptoms that appear. Based on this procedure, you can also determine the severity of the disease, and then choose the right treatment. Retrochorial hematoma during pregnancy, detected in the first trimester and at the conception stage, is treated quickly and, as practice shows, will go away by the third trimester.
This disease is accompanied by brownish, sometimes even dark, vaginal discharge. You may also experience pain in the lower abdomen. If the clot is located at the bottom of the organ, then the symptoms may not bother you. In such cases, only an ultrasound can show the presence of the disease.
When a woman's hematoma is accompanied by brown discharge, there is no need to worry, because doctors do not classify this as a bad symptom. At first, the discharge will be lighter, and a few days later it will begin to darken. Since blood collects in the cavity between the membranes of the chorion and the fetus, coagulating there and acquiring a characteristic shade, brownish discharge, on the contrary, can be a signal that the clots are beginning to come out, i.e., the resorption of the hematoma will not take much time.
You should worry when the discharge is scarlet or dark red. These are the first signs that the hematoma is growing, and the fertilized egg is still exfoliating, which means that the clot has not yet come out. If the required measures are not taken in a timely manner, a woman may lose her child, since in such cases premature termination of pregnancy occurs. At this stage, in addition to ultrasound, the specialist should prescribe monitoring of fibrinogen levels.
Possible consequences
In many ways, the course of the disease depends on the parameters of uterine hematomas. A hematoma that occupies about 50% of the total area of the embryo membrane and has a volume of more than 20 ml is considered dangerous. Such formation can inhibit the growth and full development of the fetus in a few days and provoke an unexpected pregnancy failure.
Adverse consequences may depend on how long the slowing of growth in the coccygeal-parietal dimension occurs. Braking for more than 10 days is a reason to worry. Premature detachment of the placenta can lead to the endometrium filling with blood and necrosis cores forming in it, which already indicates complete cutting off of the uterus.
During gestation, there is a high probability of heavy brown discharge due to hematoma, the consequences of which are not easy to determine. It is possible that such a bruise could result in death for both the mother and the child.
However, if a pregnant woman promptly identified the disease during an ultrasound examination or by paying attention to characteristic symptoms and underwent the necessary treatment, then the chances of normal development of the baby are much increased. After completing the course of treatment, a repeat ultrasound will be scheduled to confirm or refute the presence of a hematoma and assess the general condition of the fetus for the current day
Forecasts and reviews
Many patients have encountered a similar problem. According to reviews of hematoma during pregnancy, in most cases an unfavorable outcome was avoided and everything ended with the long-awaited birth of the baby. Almost all patients took care of their health in time and turned to a specialist at the moment when the blood clot occupied less than 40 percent of the size of the fetal egg. When this indicator exceeds the norm, the chances of saving the embryo practically disappear.
Hematoma during pregnancy is a complex pathology that many patients have to deal with in the first trimester of pregnancy. You should be very attentive to every change in your body, do not hesitate to talk about your problems to your doctor, and also adhere to the correct treatment. Only in this case can we hope for a favorable outcome - the birth of a healthy baby and the rapid recovery of the mother’s body.
So, now you know how a hematoma comes out during pregnancy.
source
Placenta previa or abruption
If a woman’s placenta (or chorion, its predecessor) is located low, then brown spotting or discharge of all shades of brown may be a sign. The most dangerous are brown intense discharge that occurs with complete and incomplete placenta previa.
With complete presentation, the “baby spot” is located at the bottom of the uterus and completely blocks the entrance to the cervical canal. If incomplete, the entrance to the cervical canal is closed by approximately two-thirds or less. Any negative impact and even the most ordinary stress can cause severe bleeding in a woman with such a pregnancy pathology.
If a diagnosis such as low placentation has already been made and confirmed by ultrasound data, the woman should be very careful. If there is no such diagnosis and the placenta is located normally, the woman still runs the risk of experiencing abruption
This becomes possible with a fall, especially with an abdominal injury, a sharp jump in hormone levels, severe emotional shock, heavy lifting, or taking certain medications prohibited during pregnancy.
Vaginal discharge during detachment is usually quite profuse, although there may be no pain. The age of the problem can be judged by the shade of the discharge. Fresh blood that has just separated and come out is always bright, scarlet. If, after detachment, the blood did not come out for some time and was in the space between the “baby place” and the wall of the uterus, then it will have brown shades of varying intensity.
How to detect the problem?
The presence of even a couple of drops of blood in a pregnant woman’s discharge is a high risk. Therefore, the help of doctors is needed.
Signs for an unscheduled visit to the gynecologist:
- Brown daub;
- Pulls the bottom in the pubic area;
- Lower back pain;
- My stomach gets tense.
Symptoms to immediately call an ambulance:
- Bloody discharge of any intensity for up to 12 weeks;
- Sharp and cutting pains;
- Weakness and dizziness;
- Nausea and vomiting;
- Reduced blood pressure;
- Fainting.
Diagnostics
At any stage of pregnancy, an ultrasound is immediately performed to assess the condition of the fetus and placenta. This test can also check for heartbeat, hypoxia, and many possible abnormalities. It is to identify a hematoma and its severity that only ultrasound is required.
To determine the cause, a comprehensive diagnosis is carried out:
- Smear for infections;
- Extensive blood tests;
- Coagulogram - for clotting;
- Doppler measurements of placental vessels;
- Hormone level analysis;
- Biochemistry;
- And others.
The only method to detect a hematoma is ultrasound. Therefore, a woman with scanty brown discharge can undergo an examination on her own if the condition does not require emergency help. This will speed up the timely identification of the problem.
Consequences and complications
This pathology has two development scenarios:
- A hematoma that occupies a small area usually resolves on its own, without medical help or unpleasant symptoms. With this pathology, pregnancy continues to develop normally without consequences for the child.
- A large hemorrhage, in which blood loss is more than 20 ml, can threaten spontaneous abortion (miscarriage), fetal death, or pathologies of the child’s development. If pregnancy continues with this type of hematoma, complications such as placental insufficiency (in 25% of women), premature birth (in 15% of cases), gestosis or late toxicosis in 8% of cases, growth retardation in 7% of fetuses can develop.
In addition, in cases of severe pathology with uterine ruptures, a woman may experience difficulties in repeated attempts to become pregnant.
What is retrochorial hematoma
Ultrasound can detect hematoma during pregnancy. In the photo taken by an ultrasound diagnostic device, the characteristic darkening, as well as the deformation of the fertilized egg, is clearly visible.
A retrochorial hematoma develops during a singleton pregnancy at 5-7 weeks and in cases where a woman is pregnant with twins. Pathology can be suspected by the appearance of nagging pain in the lower abdomen, brownish or scarlet discharge. If a woman discovers these symptoms, she should immediately consult a doctor.
In addition to retrochorionic pathology, there are:
- subchorionic -
it poses a serious threat to the fetus, surrounding the placenta; - retroamniotic
- timely detected formation, subject to adequate therapy, does not pose a threat to the developing baby; - retroplacental
- it is formed after the formation of the placenta, after 16 weeks of pregnancy; - subamniotic
- its presence is not dangerous for the baby, but requires regular monitoring; - intrauterine
- the presence of such a hematoma carries a serious risk to the fetus and requires urgent treatment.
Yellow bruises on the body for no reason
Bruises on the body for no reason, treatment and cause of the problem
Why do bruises appear on the body for no reason? Are they a symptom of a disease or were they placed due to negligence? In this article we will try to answer all these questions.
Bruises on the body for no reason appear quite suddenly. This is a symptom that requires immediate medical attention. The appearance of such bruises on the body may indicate the presence of a disease. Moreover, most diseases with such symptoms are quite serious and unpleasant. Bruises on the body for no reason signal the possible presence of diseases in the patient such as vasculitis, varicose veins, fragility of blood vessels, impaired blood circulation, decreased blood clotting and a lack of platelets. Bruises can appear due to hormonal imbalances and long-term use of various medications. Medicines such as antidepressants, analgesics, anti-inflammatory drugs and anti-asthma drugs can cause these symptoms. This is due to their ability to reduce blood clotting, which subsequently leads to bruising.
There is a hypothesis that bruises on the body for no reason may be the result of a lack of vitamins C, P and K in the body. Due to their low content, vascular fragility occurs, which further causes the formation of causeless bruises on the body.
Whatever the reason for the appearance of blue spots, urgently seek help from a doctor, because it is impossible to diagnose at home, and the reasons can be either trivial or quite serious. The doctor will prescribe all the necessary tests and, based on them, make conclusions about the further method of treatment.
how to increase the level of protein in the blood during pregnancy Protein is the most important element in the cells of the body of both an adult and a child. Hair, skin, nails, muscles - everything consists mainly of protein. If its level in the body is below normal, then symptoms appear
To determine the reasons for the formation of bruises on the body, a coagulogram and a clinical blood test are performed. Treatment and
Source
Types and forms
There are the following types of hematomas that occur in pregnant women:
- Retrochorial. Characterized by the accumulation of blood between the chorion and the wall of the uterus. The chorion is the capsule surrounding the embryo. It is formed 7-10 days after conception. As the embryo develops, the chorion degenerates into the placenta. Retrochorial hematoma is detected in the first trimester. It is the result of damage to the uterine vessels or detachment of the fertilized egg. With early initiation of therapy, hemorrhage disappears on its own and does not affect the course of pregnancy.
- Retroamniotic. This type of hematoma is also diagnosed in the first trimester of pregnancy. Blood accumulates between the amniotic membranes and the uterine wall. The membrane produces amniotic fluid, protects the fetus from injury and penetration of infectious agents. A retroamniotic hematoma does not pose a danger to the development of the fetus. A woman may complain of bloody discharge and deterioration in health. Nausea, dizziness and general weakness appear. With proper treatment, the hematoma completely dissolves.
- Retroplacental. Hemorrhage develops in the second or third trimester after the placenta has formed. The cause of blood accumulation is complete or partial separation of the placenta. The formation of a hematoma is accompanied by uterine bleeding. This type of hematoma is dangerous for both the health of the mother and the fetus. In some cases, premature birth cannot be avoided.
- Intrauterine. It occurs against the background of severe trauma to the uterus - partial or complete rupture of the walls. A hematoma forms in the third trimester of pregnancy with rapid growth of the fetus and stretching of the uterus. This is the most dangerous type of pathology, but maintaining pregnancy is possible even in the presence of intrauterine hemorrhage.
Important information: How to treat a hematoma of the paraorbital region
Depending on the severity of the pathology, the following forms of hematoma are distinguished:
- mild (characterized by an asymptomatic course, detected during examination of the patient);
- moderate (characterized by the appearance of pain and bleeding of moderate intensity);
- severe (accompanied by severe pain, drop in blood pressure, severe bleeding, impaired consciousness).
Why do they arise?
There can be several reasons that can cause damage:
- The most common cause is fainting. During pregnancy, the pregnant woman experiences low blood pressure and dizziness, which can cause loss of consciousness. The situation is worse when she loses consciousness on public transport or on the street. The impact can lead to bruises and even broken limbs. It can have an irreversible effect on the life of the fetus.
- Car crashes. In this case, blunt trauma is most often observed. Damage to the uterus, rupture of the placenta, and then premature birth may occur.
- Household damage. These include burns, sprains and dislocations. In the summer, when playing with older children, blows with a ball and other objects may occur.
It is important to understand that a blow to the stomach during pregnancy can be prevented by treating yourself with due care.
Danger for the expectant mother and baby
If a dangerous condition is detected on time, the woman has a great chance of recovering and saving the baby. With the normal further course of pregnancy and adequate therapy, the blood clot that has collected behind the membrane resolves within a month and is not detected on a subsequent ultrasound. This applies to pathologies whose blood clot volume does not exceed twenty milliliters.
The greatest danger comes from retroamniotic hematoma, or retroamniotic hematoma, as it is called. This is hemorrhage between the amniotic sac and the wall of the uterus. It is dangerous because it is accompanied by bleeding and threatens the mother with blood loss.
Any unpleasant sensations in the lower abdomen or spotting during pregnancy require attention from the woman and specialists. They may be a sign of retrothecal hematoma. To diagnose the condition, a blood test is ordered and one or more ultrasound examinations are performed.
If the hemorrhage occupies about half the surface of the separation of the uterine wall and the chorion, and the volume of blood accumulated in it exceeds twenty milliliters, there is a high probability of a frozen pregnancy.
Even if the disease was stopped at an early stage and the blood clot has resolved, the risk to the fetus still remains. The subsequent formation of placental insufficiency, its premature “aging”, a reduction in the amount of nutrients supplied to the baby, the development of hypoxia, as well as the birth of a low-weight baby are possible.