What is vasculitis
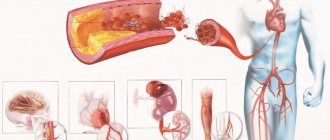
A group of autoimmune processes in which inflammation of the arterial or venous walls of human blood vessels occurs is vasculitis. As the disease progresses, it disrupts the blood flow to some organs, which is fraught with the development of complications. Taking into account the cause of development, vasculitis is divided into the following types:
- Primary. Their etiology has not yet been clarified, but autoimmune disorders are considered the triggering factor.
- Secondary. They develop against the background of other diseases - acute or chronic.
These factors, and especially a combination of several at once, can change the antigenic structure of the own walls of blood vessels. As a result, the immune system begins to perceive them as foreign. For this reason, the production of antibodies begins, damaging the vascular walls. This phenomenon triggers inflammatory and degenerative processes in target tissues. Secondary vasculitis is not only immunological disorders. Possible causes of vascular inflammation include the following:
- injuries of different localization and genesis;
- skin burns, including sunburns;
- overheating or hypothermia of the body;
- the body's individual reaction to vaccines or medications;
- contact with biological poisons or chemicals;
- hereditary predisposition;
- previous viral hepatitis;
- long-term fungal diseases, including candidiasis.
Symptoms of meningitis
1. Meningeal group:
- Intracranial pressure increases.
- Acute hydrocephalus appears.
- When tested, Kernig's sign is detected.
- The tone in the muscles of the back of the head increases.
2. Infectious group:
- Tachycardia appears.
- Sweating increases.
- There is increased weakness.
- The feeling of anxiety worsens.
- The temperature often rises and there is a fever.
- The skin tone becomes sallow, and sometimes the skin turns blue.
3. General cerebral group:
- You can observe vomiting, which appears completely suddenly, without nausea and is in no way related to meals.
- Headaches are localized at the temples and in the frontal region.
- A previously unknown fear of sharp sounds and light is felt.
The appearance of secondary meningitis is associated with the presence of one or more of these pathologies:
- Otitis acute or chronic.
- Boils in the neck or face. The most dangerous are those located above the lips.
- Abscess of one or two lungs.
- Frontit.
- Osteomyelitis of the skull bones.
Moreover, meningitis can be caused not only by the presence of all these above-mentioned ailments, but also by inappropriate or incorrect treatment of them, which, as a complication, causes inflammation of the cerebral cortex.
If your suspicions about the presence of meningitis are justified, the doctor will immediately refer you to the neuroinfectious department. There, after passing all the tests, the first stage of treatment will begin - antibiotics. Antibiotic therapy is the most important method of treatment; the drug is prescribed by the attending physician and is selected by him depending on the suspected causative agents of the disease. The time for taking medications is also determined by the doctor.
If there is cerebral edema, diuretics are prescribed, sometimes they are prescribed even when there is no edema, simply for preventive purposes. After outpatient treatment is completed, the patient switches to home treatment.
But with meningitis there are also accompanying ailments, such as vasculitis, which was already discussed earlier. Its treatment is purely individual, it depends on how severely the vessels are affected.
We suggest you read: Intestinal inflammation in an 8-year-old child: symptoms and treatment
In no case should you self-medicate, since this is not a disease that can be cured with medicinal herbs alone. A drug called Prednisolone is often prescribed. This is a hormone of synthetic origin, it helps to inhibit the influence of the immune system on the walls of blood vessels, then there is less stress on the vessels and their inflammation weakens a little. The main thing you should do is consult a doctor and continue to follow his instructions.
Signs
Vasculitis has many varieties, so the clinical picture and severity of symptoms of a particular form of the disease may differ. A typical symptom is hemorrhages in a small area with primary localization on the skin of different parts of the body. As the disease progresses, they appear in muscle tissue, areas of nerve endings and joint cavities. Doctors also identify several other common signs that indicate inflammation of the vascular walls:
- decreased visual acuity;
- bloody stools;
- stomach ache;
- joint pain, arthritis;
- rash;
- fever, headache;
- weight loss;
- sleep disorders;
- prolonged bronchitis, eosinophilic pneumonia, bronchial asthma;
- headache;
- pleurisy;
- neuropsychiatric disorders;
- seizures;
- changes in psycho-emotional state;
- pale skin;
- periodic loss of consciousness;
- nausea, vomiting;
- swelling in the temporal region.
Symptoms and signs of cerebral vasculitis
Cerebral vasculitis of the brain, the symptoms of which are often similar to stroke, is quite difficult to diagnose. Primary cerebral vasculitis develops suddenly, followed by regression of symptoms, followed by a new wave of exacerbation.
- Speech impairment;
- Dysphagia (difficulty swallowing);
- Acute headache;
- Decreased performance;
- Emotional swings;
- Mental disorders.
The progression of the disease leads to structural changes in brain areas with a deterioration in the general condition of the patient.
Signs of secondary vasculitis:
- Decreased hearing acuity;
- Dizziness;
- Fainting;
- Convulsive syndrome;
- Increased blood pressure;
- Personality disorders;
- Disorientation in space;
- Involuntary muscle contractions;
- Coma;
- Dementia.
Symptoms increase gradually, the initial stage of the disease is asymptomatic.
Classification of vasculitis
In medicine, there are several classifications of this disease. One of the criteria for determining its types is the caliber of the vessels. Taking this factor into account, vasculitis disease is divided into the following forms:
- Capillaritis. It involves damage to small vessels (capillaries). This may cause: Dego's disease, urticarial vasculitis (urticaria), Schamberg's purpura pigmentosa, Wegener's granulomatosis.
- Arteriolitis. It is an inflammation of medium-sized vessels (arteries and arterioles). It manifests itself as lepromatous arteritis, polyarteritis nodosa, Kawasaki disease, familial Mediterranean fever, and striatal vasculopathy.
- Arteritis. This is a lesion of large vessels (artery walls). These include giant cell arteritis, Takayasu's disease, Kogan's syndrome, sarcoidosis, and tropical aortitis.
- Phlebitis. With this form of vasculitis, inflammation of the vein walls occurs.
- Vasculopathy. With this disease, there are no clear signs of inflammatory cell infiltration of the vascular wall.
Due to its development, the disease is divided into two forms: primary (formed as an independent pathology) and secondary (formed against the background of other diseases). Depending on the degree of vascular damage, vasculitis occurs:
- mild degree - with a mild rash, burning and itching;
- moderate - with pronounced spots ranging in size from a few millimeters to 1-2 cm, weakness, loss of appetite, joint pain;
- severe - with numerous rashes, intestinal and pulmonary bleeding, significant changes in joints and internal organs.
Neurovasculitis
Neurovasculitis may develop under the influence of cold or nervous conditions. This disease is a reversible inflammation of the vessels of the extremities, associated with a disorder of reflex neurogenic reactions to irritation. The reason is the regular effect of temperatures in the range from -2 to +12 degrees against the background of high humidity or single frostbite.
Neurovasculitis occurs in adults over 25 years of age who work in damp, cold environments. Depending on the stage of the disease, a person experiences the following symptoms:
- First. Accompanied by chilliness of the feet, pallor and cyanosis, but without swelling of the extremities.
- Second. At the end of the working day, swelling appears, cyanosis and hyperesthesia of the skin, and pain in the feet when compressed are noted.
- Third. Swelling at this stage does not go away, the pain becomes burning, ulcers develop, and ascending thrombophlebitis.
Rheumovasculitis
This is one of the types of rheumatoid arthritis. The mechanism of development of rheumovasculitis is associated with immune processes that take part in the development of arthritis. In almost all patients, such vascular inflammation is accompanied by general inflammatory manifestations: fever, severe weight loss. Clinical manifestations of rheumatoid arthritis are included in the group of extra-articular symptoms of rheumatoid arthritis. These include the following signs:
- peripheral gangrene;
- scleritis;
- mononeuritis;
- pericarditis;
- impaired lung function;
- damage to the skin of the periungual bed.
Perivasculitis
All vasculitis is classified into types depending on the location of inflammation. If the inner vascular layer is affected, then it is endovasculitis, if the middle one is mesovasculitis. When the tissue adjacent to a blood vessel becomes inflamed, the disease is called perivasculitis. With it, the arterial wall is completely destroyed. As a result, it ruptures, and inflammation of the outer layer of blood vessels and connective tissue begins.
As the disease progresses, it can lead to gangrene or necrosis. A more common type of perivasculitis is polyarteritis nodosa. It affects the following small and medium vessels:
- brain;
- renal;
- hepatic;
- coronoids;
- mesenteric.
Autoimmune vasculitis
This type of vasculitis has many different causes. One of the provoking factors is genetic predisposition. Vessels of certain sizes are affected by different types of autoimmune vasculitis:
- large – giant cell and Takayasu arteritis;
- medium - nodular and microscopic polyarteritis, Kawasaki disease, Wegener's disease, Behçet's disease.
Articles on the topic
- Omnik - instructions and mechanism of action, contraindications, side effects, dosage regimen and analogues
- Polyhydramnios during pregnancy - signs and why it occurs, diagnosis, drug therapy and nutrition
- What are antibodies in the blood - why are they produced and what do they affect in the body, determination test
The clinical picture is determined by the type of autoimmune vasculitis. Primary signs manifest themselves in skin damage: its sensitivity increases or decreases. Against this background, the following are observed: incomplete paralysis of the arms and legs, insomnia, chronic fatigue syndrome, fever, poor appetite. The disease has an undulating course, i.e. periods of remission are replaced by exacerbations. The latter occur mainly in the cold season. Depending on the type of illness, a person may experience the following symptoms of vasculitis:
- Hematological. Causes chest pain, cough with copious sputum, shortness of breath, weakness, and kidney failure.
- Rheumatoid. Accompanied by pain in the limbs, fainting, and mental disorders. May lead to stroke.
- Takayasu arteritis. It is observed mainly in women 15-20 years old. Symptoms of the disease: elevated body temperature, headache, dizziness, weight loss. After 5-10 years, the pathology can lead to a heart attack.
- Wegener's disease. It is indicated by cough, shortness of breath, prolonged rhinitis, sinusitis or sinusitis, runny nose and mucus mixed with blood from the nose, deformation of the saddle and nasal septum, impaired renal function, and protrusion of the eyeballs. Half of the patients develop conjunctivitis or optic nerve ischemia.
- Behçet's disease. Accompanied by stomatitis, ulcers and erosions on the genitals, and inflammation of the eyes.
Hemorrhagic vasculitis
This type of vascular inflammation occurs more often in children than in adults. Boys aged 4-12 years are especially prone to developing this disease. The pathology is an aseptic (non-infectious) inflammation of the capillaries caused by the damaging effect of immune complexes. The main signs of the disease are hemorrhages (bleeding), disorders of blood circulation in small vessels and a violation of its intravascular coagulation. Depending on the clinical course, the pathology is:
- renal;
- abdominal (from the stomach);
- cutaneous;
- articular;
- combined.
The disease often develops after influenza, acute tonsillitis or scarlet fever. Causes may include drug allergies, hypothermia, and genetic predisposition. Distinctive signs of hemorrhagic vasculitis are:
- a purple rash on your legs, knees, hands, or stomach;
- pain in the ankle joints, leading to difficulty in motor function;
- stomach ache;
- kidney damage.
Allergic
The main cause of this type of vascular inflammation is an allergy to various external or internal factors: regular use of medications (sulfonamides, barbiturates, analgesics), chemical industry products, infections. Due to the reaction of the immune system to them, allergic vasculitis develops. It often occurs without involving internal organs in the pathological process. Depending on the caliber of the affected vessels, allergic vasculitis is divided into the following types:
- Surface. It affects small venules and arteries of the skin, capillaries. Inflammation is manifested by hemosiderosis, Ruter's allergic arteriolitis, and nodular necrotizing vasculitis.
- Deep. The pathological process involves arteries and veins of medium and large caliber, located in the subcutaneous fatty tissue and at its border with the dermis. The pathology manifests itself as acute and chronic erythema nodosum.
Necrotizing
This type of disease is rare, especially in children. The pathology is accompanied by extensive skin necrosis, fever, chills, weight loss and fatigue. Sometimes there are enlarged cervical lymph nodes, bilateral purulent conjunctivitis, swelling of the hands and feet. Necrotizing vasculitis develops more often as a complication of other forms of this disease. The following signs are observed on the skin:
- small papules on the skin - each bubble with transparent contents;
- redness of the skin;
- blueness of fingers or toes;
- non-healing wounds and ulcers;
- joint pain;
- numbness, tingling in the limbs;
- speech disorders;
- blood in urine or stool.
ANGITIS NODOLOUS
Angiitis nodosum includes various variants of erythema nodosum, differing from each other in the nature of the nodes and the course of the process.
Erythema nodosum acute is a classic, although not the most common, variant of the disease. It manifests itself as a rapid rash on the legs (rarely on other parts of the extremities) of bright red, swollen, painful nodes the size of a child’s palm against the background of general swelling of the legs and feet. There is an increase in body temperature to 38-39 oC. general weakness, headache, arthralgia. The disease is usually preceded by a cold or a sore throat. The nodes disappear without a trace within 2-3 weeks, successively changing their color to bluish, greenish, yellow (“bruise bloom”). There is no ulceration of the nodes. No relapses are observed.
Erythema nodosum chronic is the most common form of cutaneous angiitis. It is characterized by a persistent recurrent course, usually occurring in women of mature age, often against the background of general vascular and allergic diseases, foci of chronic infection and inflammatory or tumor processes in the pelvic organs (chronic adnexitis, uterine fibroids). Exacerbations are more often observed in spring and autumn, and are characterized by the appearance of a small number of bluish-pink dense, moderately painful nodes the size of a hazelnut or a walnut. At the beginning of their development, the nodes may not change the color of the skin, may not rise above it, and can only be determined by palpation. The almost exclusive localization of nodes is the lower leg (usually their anterior and lateral surfaces). There is moderate swelling of the legs and feet. General phenomena are inconsistent and poorly expressed. Relapses last several months, during which some nodes may resolve and others may appear to replace them.
Ulcerative nodular angiitis in a broad sense can be considered as an ulcerative form of chronic erythema nodosum. The process from the very beginning has a torpid course and is manifested by dense, rather large, slightly painful bluish-red nodes, prone to decay and ulceration with the formation of sluggish scarring ulcers. The skin over fresh nodes may have a normal color. Sometimes the process begins with a bluish spot, which transforms over time into a nodular compaction and ulcer. After the ulcers have healed, flat or retracted scars remain, the area of which can again thicken and ulcerate during exacerbations. The typical location is the back surface of the legs (calf region), but the nodes can also be located in other areas. Pastyness of the legs is characteristic. The process has a chronic, recurrent course, observed in mature women, and sometimes in men. The clinical picture of nodular-ulcerative angiitis sometimes completely simulates erythema induratum of Bazin, with which the most careful differential diagnosis should be carried out. Diagnosis of skin angiitis is based on clinical and anamnestic data, confirmed in doubtful cases by histological examination. Differential diagnosis is often made with skin tuberculosis.
Treatment is based on a clear understanding of the form, stage of the process and the degree of its activity, the concomitant pathology and pathological process that may underlie cutaneous angiitis, as well as the factors favoring its development. Patients with degree II of process activity are subject to examination and treatment in a hospital setting; in some cases, bed rest at home is allowed. At stage 1 of activity, hospitalization or home stay are necessary in the progressive stage of the disease, especially in the presence of unfavorable professional conditions. Of primary importance in all cases of exacerbations of cutaneous angiitis with the main foci on the lower extremities is bed rest, since in such patients orthostasis is usually pronounced. At the same time, gymnastics in bed is useful to improve blood circulation. Bed rest should be observed until the transition to the regressive stage. Patients, especially during an exacerbation, must follow a diet with the exception of irritating foods (alcoholic drinks, spicy, smoked, salty and fried foods, canned food, chocolate, strong tea and coffee, citrus fruits). In all cases of cutaneous angiitis, it is necessary to provide therapy aimed at eliminating the cause of the disease (remediation of a focal infection, treatment of mycosis of the feet or the underlying general disease). It is necessary to exclude exposure to factors that provoke an exacerbation of the disease (hypothermia, smoking, prolonged walking and standing, bruises, heavy lifting, etc.). It is necessary to ensure, with the help of appropriate specialists, the correction of identified concomitant diseases that can support and worsen the course of cutaneous angiitis (primarily hypertension, diabetes mellitus, chronic venous insufficiency, uterine fibroids, etc.). In acute cases, plasmapheresis is pathogenetically indicated. In all cases of cutaneous angitis, treatment should not end with the disappearance of the clinical manifestations of the disease. It should be continued in a reduced volume until laboratory parameters are completely normalized, and in the next six months to a year, patients should be left on maintenance treatment, for which angioprotectors are usually used that improve microcirculation and rheological properties of the blood, protecting the vascular wall from adverse effects (Prodectin, Parmidine or Doxium - 0.25 g 2-3 times a day), disaggregants (curantil - 0.025 g 2-3 times a day, complamin - 0.15 g 3 times a day), peripheral hemokinators (cinnarizine - 0.025 g per night) or adaptogens (Eleutherococcus extract - 25 drops 2 times a day before meals). Patients should be warned about the need to follow preventive measures that exclude exposure to risk factors (hypothermia, physical and nervous overload, long walking, bruises). If necessary, patients should be employed, and sometimes transferred to temporary disability. Patients are recommended to have a healthy lifestyle (morning exercises, hardening, walks in the fresh air, swimming, adequate sleep). After clinical recovery, spa treatment is recommended to consolidate the results obtained. Resorts for cardiovascular patients using sulfur, carbon dioxide and radon baths, dosed walking, and sea bathing are shown.
Read also: Systemic vasculitis symptoms
Diagnostics
The first step in diagnosing the disease is a careful examination of the patient by a doctor. The difficulty lies in the fact that not all patients immediately turn to a rheumatologist, and the disease sometimes goes into remission, which creates the illusion of recovery . If vasculitis is suspected, the doctor prescribes a number of laboratory, instrumental and morphological studies:
- Serological. The blood is examined for antineutrophil cytoplasmic antibodies, which helps to identify microscopic polyangiitis, Wegener's granulomatosis, and Churg-Strauss syndrome. Additionally, rheumatoid factor is examined to exclude rheumatic disease and cryoglobulins to differentiate vascular inflammation from Goodpasture's syndrome.
- Visceral angiography. Before the procedure, a contrast agent is injected intravenously to study the blood flow through the vessels. The study itself is carried out using X-rays.
- Doppler ultrasound. This procedure evaluates the intensity of blood flow in the vessels, which makes it possible to judge its violations.
- Computed and magnetic resonance imaging. Help visualize changes in the structure of internal organs.
- Detailed blood test. Inflammation is indicated by an increase in erythrocyte sedimentation rate and an increase in the number of leukocytes.
- Analysis of urine. The pathology is confirmed by an excess of the normal amount of C-reactive protein in urine and the presence of blood elements.
- Aortography. This is an x-ray examination of the aorta, based on obtaining an image after filling it with a contrast agent.
Why is it dangerous to neglect treatment?
When the disease is not detected on time, there is a high risk that it will develop into a chronic form. Then relapses are possible, in which treatment will be resumed again and again. In addition, complications after meningitis include:
- Development of strabismus.
- Progressive mental retardation.
- Epileptic seizures.
- Possibility of complete or partial loss of vision and hearing.
- Paralysis of the upper or lower limbs.
- Kidney or liver failure.
But even these terrible consequences cannot be compared with the worst thing - death. Sometimes there are even cases of death on the 7th day of the disease. Meningitis and vasculitis are two very terrible diseases in which the cortex and blood vessels of the brain become inflamed.
Related Posts
- Fainting, collapse, shock: causes and how to treat
- Death of brain cells in the elderly: what is it and what to do
- Brain hypoxia: symptoms and treatment
- What is hemiparesis (right-sided and left-sided) and how to treat it
- What to do if a person faints
- Why do you feel nauseous, wobbly and dizzy in the morning?
- Herbs for dilating blood vessels in the brain (list and description)
- Dizziness in older people: causes and treatment
Treatment of vasculitis
The goal of treating the disease is to reduce the aggression of a person’s own immune system. This is necessary to achieve remission and prevent subsequent relapses. Additionally, measures are taken to prevent irreversible damage to tissues and organs. In general, the treatment regimen includes the following activities:
- Taking medications. The patient is prescribed medications that reduce antibody synthesis and tissue sensitivity. Abnormal activity of the immune system is suppressed using glucocorticoids. If they do not have an effect, then chemotherapy with cytostatics is used. When using them, the prognosis is favorable: 90% of patients live after treatment with these drugs for more than 5 years. If the disease is bacterial in nature, the patient is prescribed antibiotics. For mild cases, non-steroidal anti-inflammatory drugs are indicated.
- Carrying out extracorporeal hemocorrection. This includes blood purification techniques, such as hemosorption, plasmapheresis, and immunosorption.
- Diet food. The diet is selected taking into account the reasons that led to vascular inflammation. Additionally, the possibility of developing allergies is excluded. The patient must follow a diet during an exacerbation and for some time after it.
During the acute stage, the patient is prescribed bed rest. This helps the skin rash disappear and blood circulation stabilize. A week after the first rash appears, a gradual expansion of the regimen begins. Treatment can be carried out at home or in a hospital. The main indications for hospitalization are moderate and severe forms of the disease. Inpatient therapy is also necessary in the following cases:
- hemorrhagic form of the disease;
- development of vascular inflammation during pregnancy;
- exacerbation of the disease or its first appearance;
- childhood.
Drug therapy
Certain medications for vasculitis are prescribed only by a doctor, taking into account the severity of the disease and the patient’s examination data. In case of a recurrent form of the disease, drugs must be taken in courses of 4-6 months . For mild cases, treatment lasts 8-12 weeks, for moderate cases – about a year . Depending on the form of the pathology, the doctor may prescribe the following groups of drugs:
- Nonsteroidal anti-inflammatory drugs: Ortofen, Piroxicam. Relieves joint pain, reduces swelling and the severity of skin rashes.
- Antiplatelet agents: Aspirin, Curantil. They thin the blood by inhibiting platelet adhesion processes, which helps prevent the formation of blood clots.
- Glucocorticosteroids: Prednisolone. It is the first-line drug of choice and has an immunosuppressive effect. Additionally, Prednisolone has a pronounced anti-inflammatory effect, so it is always prescribed for severe cases of the disease.
- Anticoagulants: Heparin. By slowing down blood clotting, they eliminate the risk of developing blood clots.
- Cytostatics: Azathioprine. Prescribed when corticosteroids are ineffective, there are contraindications to their use, or the rapid progression of the pathology. The function of Azathioprine is to suppress cellular immune responses.
- Enterosorbents: Nutriclins, Thioverol. They bind and remove toxins formed during illness from the body.
- Antihistamines: Suprastin, Tavegil. Their use is rational only at the initial stage of the disease in children if they have food or drug allergies.
Gravity blood surgery
This method of treatment includes techniques for purifying the blood of substances that cause the disease or aggravate its course. Among these procedures are the following:
- Immunosorption. It involves passing venous blood through a device filled with immunosorbent. This is a special drug that binds antibodies and immune complexes that damage blood vessels.
- Hemosorption. The blood is passed through a device with a sorbent, which also cleans it of antibodies, immune complexes and antibodies. This helps eliminate toxins, stimulate blood circulation and improve tissue nutrition.
- Plasmapheresis. Blood from a peripheral vein is passed through a centrifuge, where the liquid is separated into red blood cells and plasma. The blood cells are then returned back into the bloodstream with donor plasma or plasma replacement solutions. This is how antibodies, antigens and immune complexes are removed from the blood.
Diet food
The diet for vasculitis should be hypoallergenic. This is necessary to exclude factors that provoke vascular inflammation. The patient should give up fried foods and switch to stewed foods. It is recommended to include fresh fruits and vegetables, dairy products, dried fruits and cereals in the menu. The following foods should be removed from your diet:
- citrus fruits – tangerines, oranges, lemons;
- red apples, wild strawberries, strawberries;
- baked goods;
- eggs;
- salty dishes;
- alcohol;
- strong tea;
- coffee, chocolate;
- chips, crackers, flavor enhancers;
- honey, pollen;
- mushrooms;
- industrial canned food.
Content
Definition and general information [edit]
Synonym: vasculitis with marbled skin, livedoangiitis
Nonspecific inflammation of the walls of dermal and hypodermal blood vessels of various sizes.
Etiology and pathogenesis[edit]
Clinical manifestations[edit]
It is observed almost exclusively in women, usually in the summer. Bluish spots of different sizes and shapes form a looping pattern on the skin of the lower extremities, sometimes on the torso, upper extremities and face. Painful lumps may appear on the skin of the ankles and dorsum of the feet, which subsequently necrotize and turn into deep ulcers that are difficult to treat. After their healing, scars remain with a zone of hyperpigmentation along the periphery. Subjectively, nagging pain in the extremities and severe throbbing pain in nodes and ulcers are felt.
Vasculitis with marbled skin: Diagnosis[edit]
Differential diagnosis[edit]
Differential diagnosis is carried out with livedo reticularis (reaction of blood vessels to the effects of heat or cold in the form of marbling of the skin, disappearing after a short time or with pressure), congenital livedo (a type of hemangiomas), livedo pampiniform (late onset, often a symptom of a systemic disease).
Vasculitis with marbled skin: Treatment[edit]
Bed rest, discontinuation of oral contraceptives. Indomethacin 0.025 g 3 times a day or ibuprofen 0.2 g 3 times a day, plaquenil 0.2 g 2 times a day, pentoxifylline 0.4 g 3 times a day, sodium heparin 5000-7500 IU 2 once a day subcutaneously, acetylsalicylic acid 0.1 g per day. Externally - bandages with heparin ointment or diclofenac emulsion gel.
Prevention[edit]
Other [edit]
Skin atrophy white Miliana
Synonyms: capilaritis alba (Milian, 1929)
Definition and general information
A disease caused by chronic and recurrent capillaritis of the lower extremities.
Etiology and pathogenesis
Thinning and atrophy of the epidermis, disappearance of melanin pigment, capillaritis, endothelitis, elastorexis. Small changes in collagen and hemosiderosis are detected around the circumference of the lesions.
The elements are usually localized on the skin of the lower third of the legs in the form of porcelain-white or yellowish small spots of atrophy with a diameter of 2-5 mm, often surrounded by a halo of hyperpigmentation. The spots may merge into larger plaques. The skin over the lesions is thin, ivory-colored, the center resembles wrinkled parchment or old scar, and the periphery remains smooth and shiny. There are no subjective sensations, but upon palpation local pain in the lesion is noted. This atrophy does not tend to ulcerate, which is different from varicose dermatitis.
Read also: Cutaneous vasculitis symptoms
Compressive atrophy of the skin as a result of prolonged external pressure on it (for example, with a plaster cast for a bone fracture) is excluded by anamnesis and the symmetry of changes on both legs. Capillaritis, manifested by purpura (Shamberg's disease, Majocchi's disease, etc.), does not result in skin atrophy. Capillaritis in the acute form of systemic lupus erythematosus may be accompanied by similar skin changes on the legs and feet, but in addition to them, it also has other signs of the underlying disease.
Acetylsalicylic acid up to 1 g per day, non-steroidal anti-inflammatory drugs, agents that improve microcirculation (pentoxifylline 400 mg per day). Externally - troxevasin gel. In case of relapses and resistance to treatment, prednisolone is prescribed at a dose of 30-40 mg per day with a gradual decrease until complete cancellation after the acute phenomena have subsided.
Prevention of vasculitis
Since the primary form of the disease does not have a clearly defined cause, its prevention is difficult. In this case, it is only rational to strengthen the immune system by taking immunomodulator drugs. Additionally, it is necessary to harden the body with cold douches, swimming, and winter swimming. Proper nutrition combined with regular physical activity also helps strengthen the immune system.
Prevention of the secondary form of the disease has more principles. It is important to eliminate factors from your life that cause vasculitis. With this in mind, you need to adhere to the following recommendations:
- eliminate long-term stress;
- carry out sanitation of chronic foci of infection;
- Healthy food;
- maintain a sleep and rest schedule;
- Avoid prolonged exposure to allergens and environmental factors associated with occupational hazards on the body.