What is chorion during pregnancy?
After fertilization and implantation of the fertilized egg, the fertilized egg requires nutrition and respiration.
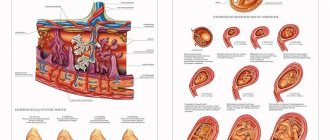
All necessary substances enter through the mother’s blood, initially through the chorion, and later through the placental membrane. Thus, the chorion during pregnancy is, first of all, a temporary organ that guarantees the normal development of the embryo. The appearance of the chorion is the membrane of the embryo with a large number of elongated villi that penetrate the wall of the uterus. Due to the growth of the fetus, the temporary organ also thickens, gradually transforming into the placenta, with the final changes occurring at 12-13 weeks.
In addition to its main function (nutrition and respiration), the chorion during pregnancy produces female hormones and protects the fetus. This means that the temporary body is designed to fully ensure the viability of the child.
Chorionic thickness by week of pregnancy: table
The first ultrasound examination is carried out at approximately 12 weeks. During the examination, the attachment of the organ is assessed, which may differ and is not pathological. In this case, presentation is diagnosed along the posterior or anterior wall of the uterus, less often a low chorion is recorded, and subsequently migration of the organ to the side walls often occurs.
Additionally, the chorion structure and thickness are assessed. Initially, the most thickened section of the chorion, which is approximately equal to the number of weeks of gestation in millimeters, is subject to measurement by ultrasound. The table shows the normal limits for membrane thickness in early pregnancy:
Causes of presentation, diagnosis and treatment
The true reason for the development of such situations has not yet been found. Background factors for the occurrence of presentation are:
The only method for diagnosing chorionic attachment and presentation is ultrasound! It is carried out in the early stages, when it is already possible to diagnose abnormalities and prevent the development of complications.
Pregnant women with central chorionic presentation must be hospitalized in a specialized hospital. It is impossible to cure this condition! The actions of doctors are aimed at preventing the development of complications. Therapy for all patients is comprehensive. It includes general recommendations and prescription of medications. A positive result largely depends on the pregnant woman herself.
Drug therapy is aimed at reducing uterine tone, pressure, and treating stress. Antispasmodics include No-shpa in tablets, Papaverine in rectal suppositories, Magne B6, and ginipral. The dose, duration of use and specific medicine are selected by the doctor!
It is possible to carry and give birth to a child with different localizations of the chorion. Many girls give birth naturally without any complications. If placenta previa persists, delivery is carried out by planned cesarean section. This is done to prevent complications during childbirth and preserve the life of the mother and baby.
Sonographic markers of miscarriage in the first trimester
Ultrasound scanner RS80
A benchmark for new standards!
Unparalleled clarity, resolution, ultra-fast data processing, and a comprehensive suite of advanced ultrasound technologies to solve the most challenging diagnostic problems.
Among the most important problems of practical obstetrics, one of the first places is miscarriage. Premature birth is the most common complication of pregnancy, and prematurity is one of the main causes of perinatal morbidity and mortality.
Despite certain advances achieved in diagnosis, therapy, and prevention of this complication, the incidence of premature birth has increased by 9% in the last five years [1]. Perinatal mortality during premature births is 25 times higher than during timely births, stillbirth rates reach 50%, and early neonatal mortality rates reach 70% [1, 2].
The frequency of spontaneous miscarriages in the first trimester remains stable for many years and accounts for 15-20% of all wanted pregnancies. In the structure of obstetric complications, this pathology ranks second [3]. In this regard, it is necessary to create a diagnostic algorithm for patients with miscarriage for timely optimization of management tactics in the first trimester. The ultrasound method occupies a leading place in the structure of complex diagnostics of this complication, being a highly informative, non-invasive, safe diagnostic test [4-6].
The purpose of this work is to determine the most informative echographic markers of miscarriage in the first trimester to predict pregnancy outcome.
Materials and methods
The main group consisted of 128 women with threatened and incipient spontaneous miscarriage at a period of 8-13 weeks, who were in the miscarriage department of the Perinatal Center of Krasnodar. The studies were conducted before the start of complex therapy.
In the first trimester of pregnancy, ultrasound diagnostics were carried out using two standard techniques, the most informative of which was transvaginal echography, as well as transabdominal scanning techniques with a full bladder. All studies were carried out on modern ultrasound machines using a 6.5 MHz transvaginal probe and 3.5 and 5 MHz convex probes in two-dimensional echo mode; Doppler examination was also used in pulsed and color modes.
Research results
For the first trimester of pregnancy, the following main echographic criteria for threatened and incipient spontaneous miscarriage were used, which were conditionally divided into three groups:
Sonographic signs of pathology of extraembryonic structures
- Amnion hypoplasia was detected in 6 (4.7%) pregnant women. Hypoplasia was considered to be the diameter of the amniotic cavity less than 10-12 mm; the measurement was carried out in two mutually perpendicular planes during longitudinal scanning.
- Chorionic hypoplasia was detected in 8 (6.25%) pregnant women. Normally, the maximum thickness of the chorion corresponds to the gestational age or lags behind it by 2-4 mm. A lag in chorion thickness of more than 5 mm was considered hypoplasia. The measurement was carried out three times in the middle third of the chorion (Fig. 1).
- Fragmented chorion was detected in 2 (1.56%) pregnant women. In the structure of the fragmented chorion, anechoic structures of irregular shape, 5-10 mm in size, are visualized (Fig. 2).
- Branched chorion presentation was detected in 14 (10.9%) pregnant women. In this case, the chorion partially or completely covers the area of the internal pharynx (Fig. 3).
- Leveling of the echogenicity of three extraembryonic cavities (chorionic, amniotic and yolk sac cavity) was detected in 2 (1.56%) pregnant women. Normally, due to differences in biochemical and cellular composition, the contents of the chorionic, amniotic cavities and the yolk sac cavity have different echogenicity [5]. During primary infection, as a result of a pronounced proliferative-exudative reaction of the amniotic membrane and yolk sac, the echogenicity of these cavities increases.
Rice. 1.
Pregnancy 8-9 weeks. Chorionic hypoplasia. The maximum thickness of the chorion is 5 mm.
Rice. 2.
Pregnancy 12 weeks. Fragmented chorion.
Rice. 3.
Pregnancy 10 weeks. Chorionic presentation.
Sonographic signs of pathology of the embryo and ovum
- Deformed ovum, this sign was detected in 35 (27.3%) pregnant women.
- Low position of the ovum occurred in 2 (1.56%) pregnant women. The low percentage of detection of this sign is associated with gestation periods of 8-13 weeks, at which the fertilized egg occupies most of the uterine cavity.
- Retrochorial hematoma was detected in 12 (9.4%) pregnant women. The nature of the localization of the hematoma (polar or parietal) and the time of its formation (echographic signs of hematoma organization) are important (Fig. 4 a, b).
- Fetal bradycardia (heart rate less than 90 beats per minute) was detected in 2 (1.56%) pregnant women. The fetal heart rate was determined using spectral Doppler.
- Early oligohydramnios was detected in 4 (3.1%) pregnant women. Inconsistency between the diameter of the fetal egg and the gestational age. The measurement was carried out in three mutually perpendicular planes, along the internal contour of the fetal egg.
- Impaired differentiation of the main anatomical structures of the embryo according to gestational age was detected in 6 (4.7%) pregnant women (Fig. 5, 6).
- A lag in the growth rate of the coccygeal-parietal size (CPD) was detected in 4 (3.1%) pregnant women. Normally, from 8 weeks of pregnancy, the increase in CTE is 10-12 mm per week.
Ultrasound in the first trimester of pregnancy
Observation of a pregnant woman in the antenatal clinic is carried out according to a certain scheme. What does it include and why are all these numerous examinations, tests and examinations needed?
Ultrasound has been used in obstetrics for a relatively short time, since the mid-1960s. And, despite this, today it is no longer possible to imagine examining a pregnant woman without an ultrasound. During this time, doctors have accumulated vast practical experience in using this research method, ultrasound scanners have been repeatedly improved, three- and four-dimensional ultrasound has appeared, and most importantly, more than one generation of healthy children has grown up.
How does ultrasound work?
Ultrasound is the name given to sound waves propagating in space at high frequencies (above 20 kHz). Ultrasound scanner sensors are both a source and receiver of ultrasonic waves. An ultrasound wave, passing through various tissues in the body, changes its speed and is reflected; all these changes are recorded and converted into an image on the monitor of an ultrasound scanner. Currently, when examining pregnant women, two types of sensors are used: transabdominal - TA (with the help of which the study is carried out through the anterior abdominal wall) and transvaginal - TV (the study is carried out through the vagina). In the first trimester, both types of sensors can be used, but transvaginal ultrasound is more informative, because the TV sensor is brought closer to the uterus and has a higher frequency of ultrasound waves, which gives a clearer image on the ultrasound scanner monitor. From the second trimester, transabdominal ultrasound is mainly used.
Ultrasound of pregnant women is performed three times - at 10-14 weeks, 20-24 and 30-34 weeks. If necessary, an obstetrician-gynecologist can prescribe an additional ultrasound, and even more than one.
Ultrasound examination of the fetus (ultrasound, echography) is the only sufficiently informative and safe research method that allows assessing the development of pregnancy from the very beginning until birth. The expectant mother will have her first visit to the ultrasound room at the beginning of her pregnancy.
You need to prepare for a transabdominal ultrasound by filling your bladder. To do this, you need to drink approximately 300-500 ml of liquid without gas 30 minutes before the test. You should take a clean diaper or towel with you to the examination. During the examination, a special transparent gel, colorless and odorless, is applied to the abdomen and the sensor. No special preparation is required for transvaginal ultrasound. You just need to empty your bladder before the test. During the examination, a special protective cover or condom is put on the sensor and gel is applied.
The study lasts on average 10-30 minutes. After this, the doctor fills out a special protocol in which he records in detail all the ultrasound results.
In the first trimester of pregnancy, an ultrasound is performed to:
- establishing the localization (location) of the fertilized egg (in the uterine cavity or outside it);
- diagnosis of single or multiple pregnancy;
- assessment of the size and growth, structure of the fetal egg and embryo;
- assessment of the vital activity of the embryo or fetus;
- studies of the structure of the embryo or fetus;
- studies of extraembryonic structures (yolk sac, chorion, amnion);
- diagnosis of pregnancy complications (threatened or in progress abortion, etc.);
- diagnosis of diseases and malformations of the internal genital organs (uterine fibroids - a benign tumor of the uterus, cysts and tumors of the ovaries, bicornuate uterus, intrauterine septum, etc.).
Establishment of intrauterine pregnancy by ultrasound
With early diagnosis of pregnancy, an ultrasound examination will identify the fertilized egg as a round or oval formation of dark gray (almost black) color, located, as a rule, in the upper half of the uterine cavity. In case of multiple pregnancy, in the very early stages you can see two or more fertilized eggs located separately. Diagnosis of intrauterine pregnancy using TA scanning is possible at an obstetric period of 5-6 weeks, i.e. when the delay of menstruation with a regular menstrual cycle is 1 week or more. The average diameter of the ovum at this time is approximately 5-7 mm. With transvaginal ultrasound, visualization of the fetal egg in the uterus is possible a little earlier - if menstruation is delayed by 3-6 days, which corresponds to 4-5 weeks of pregnancy. In this case, the size of the fertilized egg is 2-4 mm. The embryo is determined from the 5th week of pregnancy during a TV study and from the 6th - during a TA study in the form of a white linear formation in the cavity of the fetal egg. At the same time or a little later, heart contractions can be determined.
Normally, in the presence of a regular menstrual cycle, it is necessary to determine the presence of an embryo in the fertilized egg at 6 weeks of pregnancy using a TV scan. It is not necessary to do an ultrasound at this time, but if it is performed (at the woman’s request, in case of recurrent miscarriage), then at 6 weeks the embryo should be detected. And if the cycle is irregular, then the period of menstruation cannot be accurately determined. Then the period is determined by ultrasound and, if there is no embryo, they are looked at again.
If any deviation from the norm is detected, it is recommended to conduct a control ultrasound scan after a week.
When the fertilized egg is localized outside the uterine cavity, i.e. with an ectopic pregnancy, visualization of the ovum is difficult and not always possible. A reliable sign of an ectopic pregnancy is the detection of the heartbeat of the embryo outside the uterine cavity.
Assessment of the size and growth of the fertilized egg and embryo
To assess the size and growth of the ovum and embryo/fetus, indicators such as the average internal diameter of the ovum (AVD) and the coccygeal-parietal size of the embryo/fetus (CTR) are used.
To determine the SVD of the fetal egg, the length, width and anteroposterior dimensions of the ovum are measured along the internal contour, then the resulting measurements are summed up and the sum is divided by 3. For each stage of pregnancy in the first trimester, the dimensions of the SVD of the ovum are determined. These data are entered into special tables and into the ultrasound scanner program, which makes it possible to approximately determine the gestational age based on this indicator. The average error in determining the gestational age using the ovum SVD is ± 6 days.
The first dimension measured during embryo imaging is the coccygeal-parietal dimension (CPR). Essentially, this is the length of the embryo from the head to the tailbone. It should be noted that the CTE of the embryo is less subject to individual fluctuations than the average internal diameter of the ovum, so using this size to determine the gestational age gives more accurate results. The error in this case is ± 3 days. The absence of an echographic image of the embryo when the ovum SVD is greater than 14 mm is a reliable sign of a non-developing pregnancy in which the embryo is absent.
Assessment of the vital activity of the embryo and fetus
The vital activity of the embryo (fetus) in the first trimester is assessed by cardiac and motor activity.
Normally, with transvaginal ultrasound, cardiac activity in the embryo is recorded from 5-6 weeks of pregnancy. In this case, the correct rhythm of heart contractions is observed. The heart rate (HR) of the embryo during uncomplicated pregnancy gradually increases from 110-130 beats per minute at 6-8 weeks to 190 beats per minute at 9-10 weeks, after which it decreases to 140-160 and remains at this level until birth . The heart rate of the embryo in the first trimester is important for predicting the course of pregnancy. Thus, a decrease in heart rate to 85-100 beats per minute and an increase over 200 are unfavorable prognostic signs and indicate a high probability of termination of pregnancy. The absence of visualization of heartbeats with a CTE of the embryo greater than 8 mm is a sign of a non-developing pregnancy. For final confirmation of a non-developing pregnancy, it is necessary to conduct a control ultrasound scan a week later, based on the results of which a final diagnosis is made.
The motor activity of the embryo is determined from 7-8 weeks of pregnancy. At the beginning these are weak, isolated, barely noticeable movements. Then - flexion and extension of the torso. After this, as the embryo grows and develops, limb movements appear. But it should be noted that episodes of motor activity can be replaced by long periods of rest, so recording heartbeats is a more important criterion for assessing the vital activity of the embryo.
Study of the structure of the embryo and fetus
During ultrasound, special attention is paid to the anatomy of the developing embryo, since at the end of the first trimester gross malformations can be detected, such as anencephaly (absence of the brain), spinal cord herniation, skeletal anomalies, etc. The head of the embryo is determined as a separate round formation from 8-9 weeks of pregnancy. Most organs of the chest and abdominal wall are identified after 10-11 weeks of pregnancy.
Particular attention should be paid to the echographic marker of chromosomal disorders - nuchal translucency (NT). The nuchal space is measured on the back of the neck at 10-14 weeks of pregnancy with a fetal CTE of 45-84 mm. Normally, the size of the collar space should not exceed 3 mm. An increase in this indicator allows up to 80% of chromosomal disorders to be diagnosed at the end of the first trimester.
As ultrasound equipment improves, data is accumulating on the possibility of diagnosing malformations of the cardiovascular system, central nervous system (CNS), gastrointestinal tract (GIT), and urinary system up to 12 weeks of pregnancy.
Study of extraembryonic structures
In addition to the embryo, ultrasound evaluates the yolk sac, chorion and amnion.
During physiological pregnancy, the yolk sac (an extraembryonic structure that performs nutritional and hematopoietic functions in the first weeks of pregnancy) is determined when the ovum SVD is more than 10 mm (pregnancy period is more than 5 weeks) in the form of a white ring with a diameter of 2 mm (5 weeks) to 7 mm (10 weeks). A sign of an undeveloped pregnancy is also the absence of a yolk sac when the ovum is larger than 10 mm. After 12 weeks of pregnancy, the yolk sac is normally not detectable. There is a relationship between the size of the yolk sac and pregnancy outcome. An increase of more than 7 mm and a decrease of less than 2 mm, irregular shape and thickening of the walls of the yolk sac are prognostically significant only when combined with other disorders, such as changes in the thickness of the chorion (villous membrane), or delayed embryonic growth. An isolated discrepancy between the size of the yolk sac and the norm does not significantly affect the incidence of pregnancy complications.
The chorion is the outer villous membrane of the fertilized egg. The fetal part of the placenta is formed from the chorion. During ultrasound, the chorion is visualized as a white ring with wavy contours, located along the outer edge of the fertilized egg. The thickness of the chorion in the first trimester in millimeters is approximately equal to the gestational age in weeks. Underdevelopment of the chorion (hypoplasia) or changes in its structure often leads to spontaneous abortion. The chorionic villi are interconnected with the inner (decidua - falling off) lining of the uterus. If this interaction is disrupted, detachment of the fertilized egg occurs. As a result, a retrochorial (located behind the chorion) hematoma (a limited collection of blood) is formed. Retrochorial hematoma is an ominous sign indicating an incipient miscarriage.
Amnion is a water membrane, which is a closed sac in which the embryo/fetus is located, surrounded by amniotic fluid. The amnion is adjacent to the chorion from the inside. Hypoplasia (underdevelopment) of the amniotic cavity leads to a non-developing pregnancy. In such cases, the diameter of the amniotic cavity does not exceed 10-12 mm for more than 6 weeks of pregnancy. An increase in the size of the amnion, characteristic of early polyhydramnios, and its heterogeneous contents (suspension in the amniotic fluid) are often associated with the presence of infection. Early polyhydramnios is an unfavorable sign.
Diagnosis of pregnancy complications based on ultrasound results
The most common pathology in the first trimester is the threat of miscarriage. The main echo sign of the threat of interruption is local thickening of the uterine muscles (hypertonicity of the myometrium). Several areas of hypertonicity can be detected. At the same time, the shape of the fetal egg changes: from round or oval it becomes irregular, sometimes severely deformed. The most unfavorable situation is when the area of increased tone is located at the site of placenta formation: in this case, detachment of the ovum and termination of pregnancy are possible.
In most cases, myometrial hypertonicity is accompanied by pain in the lower abdomen. In this case, treatment aimed at maintaining pregnancy is necessary. In the event that the fertilized egg loses contact with the wall of the uterus and exfoliates from its bed, a retrochorial hematoma is formed (a limited accumulation of blood between the fertilized egg and the uterine wall). This is typical for an incipient miscarriage. With significant detachment, deformation and reduction in the size of the fertilized egg occurs, and the death of the embryo occurs. Clinically, bleeding of varying intensity is usually observed. The threat of termination of pregnancy is also indicated by a shortening of the cervix to 2.5 cm (normal 3.5-4 cm) and a funnel-shaped expansion of the internal os.
If, against the background of bloody discharge from the genital tract, ultrasound reveals an expansion of the uterine cavity and the presence of heterogeneous contents in it, and the fertilized egg is not visible, then an incomplete miscarriage is diagnosed. In this case, hospitalization in the gynecology department is necessary to scrape out the remains of the fertilized egg and stop the bleeding.
A non-developing pregnancy is characterized by smaller sizes of the fetal egg for a given period of pregnancy, its deformation, blurred contours, a decrease in the thickness of the chorion, and the absence of heartbeats of the embryo.
Localization of the fertilized egg in the cervical canal (cervical canal) is characteristic of cervical pregnancy. In this case, better visualization is achieved with transvaginal ultrasound. In this situation, urgent hospitalization in a hospital is necessary, since the likelihood of heavy bleeding is very high.
Quite often during pregnancy, a corpus luteum cyst occurs in one of the ovaries, which is a formation with a diameter of 3 to 8 cm with thick walls and a heterogeneous internal structure. This is the norm. A characteristic feature of this cyst is a gradual decrease in its size and disappearance by the end of the first trimester.
Hydatidiform mole is a rare complication observed in 1 case in 2000-3000 pregnancies, associated with chorion pathology, in which the chorion transforms into grape-shaped formations that destroy all other structures of the fetal egg. In this case, the uterus fills with many bubbles with fluid. An ultrasound visualizes a uterus larger than normal in size for a given stage of pregnancy, with an enlarged cavity filled with heterogeneous contents (the so-called “snow storm” picture).
Diseases and defects of the internal genital organs on ultrasound
When performing an ultrasound of the pelvic organs, the size of the uterus and ovaries is assessed, as well as the presence of pathological changes (uterine fibroids - a benign tumor of the uterus, cysts and tumor diseases of the ovaries) and congenital malformations (saddle uterus, bicornuate uterus, duplication of the uterus, septum in the uterine cavity and etc.). The most unfavorable situation is when the placenta is located above the myomatous node. In this case, there is a high risk of premature placental abruption.
Currently, three-dimensional ultrasound examination, which produces a “three-dimensional picture,” is becoming increasingly popular. Three-dimensional ultrasound makes it possible to diagnose some developmental defects at an earlier stage (for example, facial defects: cleft lip, etc.). But 3D scanning is a longer study, and, unfortunately, it is not always possible to obtain the necessary image. And the experience in three-dimensional ultrasound examination has not yet been accumulated. Therefore, most likely, this method is the future, and at present, three-dimensional ultrasound is just an additional research method.
So, ultrasound examination of the fetus and pelvic organs in the first trimester of pregnancy is one of the most important and irreplaceable diagnostic methods, allowing one to assess the development of pregnancy from the earliest stages and choose the right tactics for its management.
All about children
06/13/2019 admin Comments No comments
Interpretation of ultrasound during pregnancy is carried out by two doctors - an ultrasound diagnostic specialist and the attending obstetrician-gynecologist. The first gives a conclusion about the duration of pregnancy and the detected features and pathology, the second compares them with family history, the characteristics of the course of pregnancy specifically for this woman.
Based on all this, a conclusion is made whether everything is in order, whether measures need to be taken to correct the condition of the fetus, uterus or other organs. The study is carried out according to a specific protocol, which is slightly modified depending on the stage of pregnancy. The doctor examines the fetus, placenta, umbilical cord, amniotic fluid, cervix and uterine body, takes certain measurements and enters them into the pregnancy ultrasound form.
How are the results of an ultrasound scan of pregnant women interpreted?
Based on all the data provided, at the end of the study a conclusion is drawn and recommendations are made. Here the sonologist writes when, in his opinion, it is worth undergoing the next examination, and how soon after the ultrasound you need to visit the antenatal clinic doctor.
The important ultrasound findings during pregnancy differ in the first trimester from those that will be assessed later - in the second and third trimesters. This is due to the fact that the child does not immediately turn out the way he is born.
It develops from a “disc” (this is how ultrasound sees it until the 10th week), passing through the embryonic stage (visible on a monitor that looks like a fish), and only then does it develop full-fledged arms, legs, torso and head, which are measured using ultrasound .
First trimester study
The first ultrasound examination protocol during pregnancy includes the following data:
- Woman's passport details
- Obstetric gestational age (calculated based on the last menstrual period)
- Number of fetuses in the uterus
- Coccygeal-parietal (CP) size of the fetus (this indicator is the “predecessor” of the indicator “height” or “body length”): indicated in millimeters
- Heartbeats (here they write whether they are present (s/b +) or not (s/b -)), their frequency
- Collar thickness (mm)
- Presence or absence of a yolk sac, if present - its average diameter
- Location of the chorion (future placenta): it can be located on any wall of the uterus, as well as in the area of its fundus or internal os. The last option is called “chorion or placenta previa”
- The structure of the chorion: normally should not be “changed”
- Uterine appendages: their size, presence of cysts, developmental anomalies are assessed
- Features of the structure of the uterus: tumors, fibroids, developmental anomalies.
After the doctor has written down specific measurement numbers, he needs to compare them with ultrasound standards during pregnancy. They are assessed depending on the gestational age. Moreover, it should be noted that research conducted before the 8th week gives the most accurate results about the timing of pregnancy, since at this time the embryos do not yet have individual characteristics.
Parameter table
Thus, normal fetal ultrasound parameters by week of pregnancy can be presented in the form of a table, where all parameters, except for the term, are presented in millimeters:
Screening and first scheduled ultrasound
At 12 weeks, the woman must register with the hospital and undergo the first ultrasound examination.
Photo 1. Typical protocol for the first screening ultrasound examination.
The first ultrasound gives the mother the opportunity to see her baby and ask the doctor all her questions. During this ultrasound, the specialist determines the size of the fetus and the approximate timing of the birth of the child. In addition, the tone of the uterus, the correct location of the placenta and the number of developing fetuses are analyzed.
There is a table of normal values with which the data obtained from an ultrasound examination of the fetus are compared. Pregnancy proceeds satisfactorily if the results are normal.
A method that is considered significant and more informative than fetal ultrasound is screening at the 12th week of pregnancy. It has several components: the ultrasound examination itself and a biochemical blood test, which shows two markers - free b-hCG and PAPP-A, which can identify the risk of chromosomal abnormalities of the fetus.
Causes and consequences of deviations
Deviations from the norm are of two types: thick placenta or very thin. Both are risk factors, because anomalies in the structure of the “children’s place” disrupt its functions, on which the well-being and development of the baby directly depend. It is worth considering both situations in detail.
Placental hyperplasia is said to occur when the thickness of the “baby place” is above the upper limit of the permissible range of normative values. The greater the difference, the more serious the situation. A thick placenta worries doctors much more than a thin placenta, because with hyperplasia, the temporary organ ages and matures faster, and this is fraught with premature birth, fetal hypoxia, fetoplacental insufficiency and delayed development of the baby.
If the placenta ages prematurely, the baby in any case does not receive enough oxygen, vitamins and nutrients. He may exhibit symptoms of intoxication of the body, because the placenta copes worse and more slowly with the removal of waste products.
There are many reasons that can cause hyperplasia of the “children’s place”. This is, for example, diabetes in an expectant mother. With it, not only the thickness, but also the structure of the placenta is disrupted - an additional lobule may be present.
The thickness may be increased due to chronic anemia, which some pregnant women begin to experience in the early stages of pregnancy.
If a woman has suffered a viral disease (for example, influenza or acute respiratory viral infection) in the early stages, the likelihood that placental hyperplasia will occur is very high. By thickening the “baby spot” can respond to genital tract infections, sexually transmitted diseases, as well as “winged” infections (chlamydia, ureaplasmosis and others).
At any stage of pregnancy, the thickness of the placenta can begin to increase due to Rh conflict if an Rh negative mother is carrying a Rh positive baby, resulting in sensitization. In the later stages, hyperplasia of the “baby place” threatens pregnant women with gestosis, edema, high blood pressure and excess weight.
The functions of the placenta with thickening deteriorate significantly, especially the protective function. If hyperplasia is caused by infection, such a placenta will not be able to protect the baby; he will most likely become infected and may die in utero. The early stages of thickening do not make themselves felt. Only by undergoing ultrasound diagnostics is it possible to determine such a violation.
But in later stages, the woman will be “informed” about the development of the pathology by the baby’s movements: he will begin to show pronounced anxiety, and then episodes of physical activity will become more rare. CTG may reveal abnormalities in the condition of the fetus; uteroplacental blood flow will also be disturbed by ultrasound.
Treatment is prescribed only after determining the exact cause of the anomaly. If this is an infection, the woman is prescribed a course of antimicrobial or antiviral therapy; for diabetes mellitus, a standard course of treatment by an endocrinologist is prescribed; for gestosis, hospitalization may be required, as well as a diet and normalization of blood pressure. Unfortunately, there are no medications that could reduce the thickness of the placenta.
Fertilized egg on ultrasound: sizes by week of pregnancy
The fertilized sac is a round or ovoid (egg-shaped) formation that surrounds the embryo, usually located in the upper half of the uterine cavity.
In the early stages of pregnancy (in the first trimester), an ultrasound examination is performed to determine the localization (location) of the fetal egg. On an ultrasound, the fertilized egg looks like a small dark gray (almost black) spot with clear contours.
The presence of a fertilized egg in the uterine cavity eliminates the possibility of an ectopic pregnancy. In a multiple pregnancy, you can see two separately located fertilized eggs.
How does ultrasound work?
Ultrasound is the name given to sound waves propagating in space at high frequencies (above 20 kHz). Ultrasound scanner sensors are both a source and receiver of ultrasonic waves. An ultrasound wave, passing through various tissues in the body, changes its speed and is reflected; all these changes are recorded and converted into an image on the monitor of an ultrasound scanner. Currently, when examining pregnant women, two types of sensors are used: transabdominal - TA (with the help of which the study is carried out through the anterior abdominal wall) and transvaginal - TV (the study is carried out through the vagina). In the first trimester, both types of sensors can be used, but transvaginal ultrasound is more informative, because the TV sensor is brought closer to the uterus and has a higher frequency of ultrasound waves, which gives a clearer image on the ultrasound scanner monitor. From the second trimester, transabdominal ultrasound is mainly used.
Ultrasound of pregnant women is performed three times - at 10-14 weeks, 20-24 and 30-34 weeks. If necessary, an obstetrician-gynecologist can prescribe an additional ultrasound, and even more than one.
Ultrasound examination of the fetus (ultrasound, echography) is the only sufficiently informative and safe research method that allows assessing the development of pregnancy from the very beginning until birth. The expectant mother will have her first visit to the ultrasound room at the beginning of her pregnancy.
You need to prepare for a transabdominal ultrasound by filling your bladder. To do this, you need to drink approximately 300-500 ml of liquid without gas 30 minutes before the test. You should take a clean diaper or towel with you to the examination. During the examination, a special transparent gel, colorless and odorless, is applied to the abdomen and the sensor. No special preparation is required for transvaginal ultrasound. You just need to empty your bladder before the test. During the examination, a special protective cover or condom is put on the sensor and gel is applied.
The study lasts on average 10-30 minutes. After this, the doctor fills out a special protocol in which he records in detail all the ultrasound results.
In the first trimester of pregnancy, an ultrasound is performed to:
- establishing the localization (location) of the fertilized egg (in the uterine cavity or outside it);
- diagnosis of single or multiple pregnancy;
- assessment of the size and growth, structure of the fetal egg and embryo;
- assessment of the vital activity of the embryo or fetus;
- studies of the structure of the embryo or fetus;
- studies of extraembryonic structures (yolk sac, chorion, amnion);
- diagnosis of pregnancy complications (threatened or in progress abortion, etc.);
- diagnosis of diseases and malformations of the internal genital organs (uterine fibroids - a benign tumor of the uterus, cysts and tumors of the ovaries, bicornuate uterus, intrauterine septum, etc.).
At what stage of pregnancy can you see the fertilized egg?
Approximately two and a half weeks after conception, if menstruation is delayed by 3-5 days or more, that is, in the fourth to fifth obstetric week of pregnancy from the last day of the last menstruation, an ultrasound diagnostician can already see the fertilized egg in the uterine cavity using transvaginal ultrasound. The diagnostic level of hCG in the blood serum, at which the fertilized egg should be visible in the uterine cavity during transvaginal ultrasound, is from 1000 to 2000 IU.
The fertilized egg looks like a rounded black (anechoic or echo-negative, that is, not reflecting ultrasonic waves) formation, the diameter of which is very small and ranges from 2-3 mm. The embryo and extra-embryonic organs still have a microscopic structure and therefore are not yet visible using ultrasound. The use of such a parameter as the average internal diameter of the ovum is most appropriate in the first 3-5 weeks of pregnancy from conception, when the embryo is not yet visible or is difficult to detect. The error when using the measurement usually does not exceed 6 days.
Chorion 3 mm period 5 weeks
anonymous, Female, 30 years old
Good afternoon. I am 29 years old, my cycle is 24-25 days, regular. At exactly 4 obstetric weeks I took a hCG test - 554.9 MIU/ml. A week later I went for the first ultrasound (5 obstetric weeks). The ultrasound doctor wrote in the conclusion: “The average internal diameter of the gestational sac is 3.4 mm. The embryo and yolk sac are not visualized due to timing. Short-term intrauterine pregnancy." I was told that usually at such stages there should be more than five, and in some cases even the fetal heartbeat can be heard. Is it so? I am very worried that this is a frozen pregnancy, because the previous one also ended in miscarriage in the early stages. Are these sizes normal at 5 obstetric weeks? Can everything return to normal and catch up in size in a week or two? It felt like there was a late implantation, because... A little anointed right before the start of the expected menstruation. Thanks in advance for your answer.
Consultation on the topic “Fetal sac 3–4 mm at 5 obstetric weeks” is given for informational purposes only. Based on the results of the consultation received, please consult a doctor, including to identify possible contraindications.
About the consultant
Details
Education: Graduated from the Russian National Research Medical University named after N. I. Pirogov (formerly RSMU) in 2006, residency in the specialty “Obstetrics and Gynecology” at the Department of Obstetrics and Gynecology of the Pediatric Faculty of RSMU at the Center for Family Planning and Reproduction in 2008.
She completed the course “Ultrasound research in obstetrics and gynecology” at the Scientific Center for Obstetrics, Gynecology and Perinatology named after V.I. Kulakova in 2008, “Endocrinology in gynecological practice” on the basis of the Department of Obstetrics and Gynecology of the Russian Academy of Postgraduate Education (RMAPO) in 2009.
She completed advanced training courses in obstetrics and gynecology at the Department of Obstetrics and Gynecology of the Moscow Medical Academy. I. M. Sechenov in 2013
Professional skills: Infertility treatment: intrauterine insemination, IVF, donor programs, surrogacy programs, surgical manipulations (follicle puncture, embryo transfer, endometrial tube biopsy, HSG). Has a specialist certificate and experience in Ultrasound diagnostics.
Experience: More than 8 years
Becoming a mother is a woman’s natural desire, but pregnancy is not always planned. Therefore, if you celebrate 3-5 days, and there is a possibility of fertilization, then it is quite advisable to undergo a transvaginal ultrasound examination. Most likely, it will show that your uterus already has a new “resident” - a 3 mm fertilized egg, your unborn child.
He has already gone through a long and difficult path, which began with the process of fertilization and passage through the fallopian tubes. You are unlikely to feel any signs of pregnancy, but a 3 mm fertilized egg is already inside, is developing with all its might and has every right to life. On the monitor screen of an ultrasound machine you can see a drop-shaped or round formation that does not reflect ultrasonic waves. At a period of approximately 2 or 5 weeks, the diameter of the fertilized egg is 3-5 mm, it continues to constantly divide its cells and grow. Itself and its embryonic organs are still so small that they cannot be seen in any way. At 3 weeks, the fertilized egg, as a rule, is attached to the right tubal corner of the uterus, but there are cases of its “low” location, which is not a pathology at all. It’s just that your baby has been moving around in the uterus for some time in search of shelter.
Size of fertilized egg and gestational age
The ultrasound machine automatically calculates the most accurate gestational age based on the size of the embryonic chamber. It takes into account the time that was necessary to achieve such parameters and sets the date for the fusion of the male and female eggs. However, in obstetrics a slightly different calculation technique is used, which involves calculating the gestational age from the first day of the last menstruation. As a rule, the error is 2-2.5 weeks and is hidden in subsequent studies.
If you were told on an ultrasound that the size of the fertilized egg is 3 mm, then this means that you have time to think about whether this baby will be born or not. Take this dilemma as seriously and responsibly as possible.
Observation of a pregnant woman in the antenatal clinic is carried out according to a certain scheme. What does it include and why are all these numerous examinations, tests and examinations needed?
Ultrasound has been used in obstetrics for a relatively short time, since the mid-1960s. And, despite this, today it is no longer possible to imagine examining a pregnant woman without an ultrasound. During this time, doctors have accumulated vast practical experience in using this research method, ultrasound scanners have been repeatedly improved, three- and four-dimensional ultrasound has appeared, and most importantly, more than one generation of healthy children has grown up.
How does ultrasound work?
Ultrasound is the name given to sound waves propagating in space at high frequencies (above 20 kHz). Ultrasound scanner sensors are both a source and receiver of ultrasonic waves. An ultrasound wave, passing through various tissues in the body, changes its speed and is reflected; all these changes are recorded and converted into an image on the monitor of an ultrasound scanner. Currently, when examining pregnant women, two types of sensors are used: transabdominal - TA (with the help of which the study is carried out through the anterior abdominal wall) and transvaginal - TV (the study is carried out through the vagina). In the first trimester, both types of sensors can be used, but transvaginal ultrasound is more informative, because the TV sensor is brought closer to the uterus and has a higher frequency of ultrasound waves, which gives a clearer image on the ultrasound scanner monitor. From the second trimester, transabdominal ultrasound is mainly used.
Ultrasound of pregnant women is performed three times - at 10-14 weeks, 20-24 and 30-34 weeks. If necessary, an obstetrician-gynecologist can prescribe an additional ultrasound, and even more than one.
Ultrasound examination of the fetus (ultrasound, echography) is the only sufficiently informative and safe research method that allows assessing the development of pregnancy from the very beginning until birth. The expectant mother will have her first visit to the ultrasound room at the beginning of her pregnancy.
You need to prepare for a transabdominal ultrasound by filling your bladder. To do this, you need to drink approximately 300-500 ml of liquid without gas 30 minutes before the test. You should take a clean diaper or towel with you to the examination. During the examination, a special transparent gel, colorless and odorless, is applied to the abdomen and the sensor. No special preparation is required for transvaginal ultrasound. You just need to empty your bladder before the test. During the examination, a special protective cover or condom is put on the sensor and gel is applied.
The study lasts on average 10-30 minutes. After this, the doctor fills out a special protocol in which he records in detail all the ultrasound results.
In the first trimester of pregnancy, an ultrasound is performed to:
- establishing the localization (location) of the fertilized egg (in the uterine cavity or outside it);
- diagnosis of single or multiple pregnancy;
- assessment of the size and growth, structure of the fetal egg and embryo;
- assessment of the vital activity of the embryo or fetus;
- studies of the structure of the embryo or fetus;
- studies of extraembryonic structures (yolk sac, chorion, amnion);
- diagnosis of pregnancy complications (threatened or in progress abortion, etc.);
- diagnosis of diseases and malformations of the internal genital organs (uterine fibroids - a benign tumor of the uterus, cysts and tumors of the ovaries, bicornuate uterus, intrauterine septum, etc.).
Establishment of intrauterine pregnancy by ultrasound
With early diagnosis of pregnancy, an ultrasound examination will identify the fertilized egg as a round or oval formation of dark gray (almost black) color, located, as a rule, in the upper half of the uterine cavity. In case of multiple pregnancy, in the very early stages you can see two or more fertilized eggs located separately. Diagnosis of intrauterine pregnancy using TA scanning is possible at an obstetric period of 5-6 weeks, i.e. when the delay of menstruation with a regular menstrual cycle is 1 week or more. The average diameter of the ovum at this time is approximately 5-7 mm. With transvaginal ultrasound, visualization of the fetal egg in the uterus is possible a little earlier - if menstruation is delayed by 3-6 days, which corresponds to 4-5 weeks of pregnancy. In this case, the size of the fertilized egg is 2-4 mm. The embryo is determined from the 5th week of pregnancy during a TV study and from the 6th - during a TA study in the form of a white linear formation in the cavity of the fetal egg. At the same time or a little later, heart contractions can be determined.
Normally, in the presence of a regular menstrual cycle, it is necessary to determine the presence of an embryo in the fertilized egg at 6 weeks of pregnancy using a TV scan. It is not necessary to do an ultrasound at this time, but if it is performed (at the woman’s request, in case of recurrent miscarriage), then at 6 weeks the embryo should be detected. And if the cycle is irregular, then the period of menstruation cannot be accurately determined. Then the period is determined by ultrasound and, if there is no embryo, they are looked at again.
If any deviation from the norm is detected, it is recommended to conduct a control ultrasound scan after a week.
When the fertilized egg is localized outside the uterine cavity, i.e. with an ectopic pregnancy, visualization of the ovum is difficult and not always possible. A reliable sign of an ectopic pregnancy is the detection of the heartbeat of the embryo outside the uterine cavity.
Assessment of the size and growth of the fertilized egg and embryo
To assess the size and growth of the ovum and embryo/fetus, indicators such as the average internal diameter of the ovum (AVD) and the coccygeal-parietal size of the embryo/fetus (CTR) are used.
To determine the SVD of the fetal egg, the length, width and anteroposterior dimensions of the ovum are measured along the internal contour, then the resulting measurements are summed up and the sum is divided by 3. For each stage of pregnancy in the first trimester, the dimensions of the SVD of the ovum are determined. These data are entered into special tables and into the ultrasound scanner program, which makes it possible to approximately determine the gestational age based on this indicator. The average error in determining the gestational age using the ovum SVD is ± 6 days.
The first dimension measured during embryo imaging is the coccygeal-parietal dimension (CPR). Essentially, this is the length of the embryo from the head to the tailbone. It should be noted that the CTE of the embryo is less subject to individual fluctuations than the average internal diameter of the ovum, so using this size to determine the gestational age gives more accurate results. The error in this case is ± 3 days. The absence of an echographic image of the embryo when the ovum SVD is greater than 14 mm is a reliable sign of a non-developing pregnancy in which the embryo is absent.
Assessment of the vital activity of the embryo and fetus
The vital activity of the embryo (fetus) in the first trimester is assessed by cardiac and motor activity.
Normally, with transvaginal ultrasound, cardiac activity in the embryo is recorded from 5-6 weeks of pregnancy. In this case, the correct rhythm of heart contractions is observed. The heart rate (HR) of the embryo during uncomplicated pregnancy gradually increases from 110-130 beats per minute at 6-8 weeks to 190 beats per minute at 9-10 weeks, after which it decreases to 140-160 and remains at this level until birth . The heart rate of the embryo in the first trimester is important for predicting the course of pregnancy. Thus, a decrease in heart rate to 85-100 beats per minute and an increase over 200 are unfavorable prognostic signs and indicate a high probability of termination of pregnancy. The absence of visualization of heartbeats with a CTE of the embryo greater than 8 mm is a sign of a non-developing pregnancy. For final confirmation of a non-developing pregnancy, it is necessary to conduct a control ultrasound scan a week later, based on the results of which a final diagnosis is made.
The motor activity of the embryo is determined from 7-8 weeks of pregnancy. At the beginning these are weak, isolated, barely noticeable movements. Then - flexion and extension of the torso. After this, as the embryo grows and develops, limb movements appear. But it should be noted that episodes of motor activity can be replaced by long periods of rest, so recording heartbeats is a more important criterion for assessing the vital activity of the embryo.
Study of the structure of the embryo and fetus
During ultrasound, special attention is paid to the anatomy of the developing embryo, since at the end of the first trimester gross malformations can be detected, such as anencephaly (absence of the brain), spinal cord herniation, skeletal anomalies, etc. The head of the embryo is determined as a separate round formation from 8-9 weeks of pregnancy. Most organs of the chest and abdominal wall are identified after 10-11 weeks of pregnancy.
Particular attention should be paid to the echographic marker of chromosomal disorders - nuchal translucency (NT). The nuchal space is measured on the back of the neck at 10-14 weeks of pregnancy with a fetal CTE of 45-84 mm. Normally, the size of the collar space should not exceed 3 mm. An increase in this indicator allows up to 80% of chromosomal disorders to be diagnosed at the end of the first trimester.
As ultrasound equipment improves, data is accumulating on the possibility of diagnosing malformations of the cardiovascular system, central nervous system (CNS), gastrointestinal tract (GIT), and urinary system up to 12 weeks of pregnancy.
Study of extraembryonic structures
In addition to the embryo, ultrasound evaluates the yolk sac, chorion and amnion.
During physiological pregnancy, the yolk sac (an extraembryonic structure that performs nutritional and hematopoietic functions in the first weeks of pregnancy) is determined when the ovum SVD is more than 10 mm (pregnancy period is more than 5 weeks) in the form of a white ring with a diameter of 2 mm (5 weeks) to 7 mm (10 weeks). A sign of an undeveloped pregnancy is also the absence of a yolk sac when the ovum is larger than 10 mm. After 12 weeks of pregnancy, the yolk sac is normally not detectable. There is a relationship between the size of the yolk sac and pregnancy outcome. An increase of more than 7 mm and a decrease of less than 2 mm, irregular shape and thickening of the walls of the yolk sac are prognostically significant only when combined with other disorders, such as changes in the thickness of the chorion (villous membrane), or delayed embryonic growth. An isolated discrepancy between the size of the yolk sac and the norm does not significantly affect the incidence of pregnancy complications.
The chorion is the outer villous membrane of the fertilized egg. The fetal part of the placenta is formed from the chorion. During ultrasound, the chorion is visualized as a white ring with wavy contours, located along the outer edge of the fertilized egg. The thickness of the chorion in the first trimester in millimeters is approximately equal to the gestational age in weeks. Underdevelopment of the chorion (hypoplasia) or changes in its structure often leads to spontaneous abortion. The chorionic villi are interconnected with the inner (decidua - falling off) lining of the uterus. If this interaction is disrupted, detachment of the fertilized egg occurs. As a result, a retrochorial (located behind the chorion) hematoma (a limited collection of blood) is formed. Retrochorial hematoma is an ominous sign indicating an incipient miscarriage.
Amnion is a water membrane, which is a closed sac in which the embryo/fetus is located, surrounded by amniotic fluid. The amnion is adjacent to the chorion from the inside. Hypoplasia (underdevelopment) of the amniotic cavity leads to a non-developing pregnancy. In such cases, the diameter of the amniotic cavity does not exceed 10-12 mm for more than 6 weeks of pregnancy. An increase in the size of the amnion, characteristic of early polyhydramnios, and its heterogeneous contents (suspension in the amniotic fluid) are often associated with the presence of infection. Early polyhydramnios is an unfavorable sign.
Diagnosis of pregnancy complications based on ultrasound results
The most common pathology in the first trimester is the threat of miscarriage. The main echo sign of the threat of interruption is local thickening of the uterine muscles (hypertonicity of the myometrium). Several areas of hypertonicity can be detected. At the same time, the shape of the fetal egg changes: from round or oval it becomes irregular, sometimes severely deformed. The most unfavorable situation is when the area of increased tone is located at the site of placenta formation: in this case, detachment of the ovum and termination of pregnancy are possible.
In most cases, myometrial hypertonicity is accompanied by pain in the lower abdomen. In this case, treatment aimed at maintaining pregnancy is necessary. In the event that the fertilized egg loses contact with the wall of the uterus and exfoliates from its bed, a retrochorial hematoma is formed (a limited accumulation of blood between the fertilized egg and the uterine wall). This is typical for an incipient miscarriage. With significant detachment, deformation and reduction in the size of the fertilized egg occurs, and the death of the embryo occurs. Clinically, bleeding of varying intensity is usually observed. The threat of termination of pregnancy is also indicated by a shortening of the cervix to 2.5 cm (normal 3.5-4 cm) and a funnel-shaped expansion of the internal os.
If, against the background of bloody discharge from the genital tract, ultrasound reveals an expansion of the uterine cavity and the presence of heterogeneous contents in it, and the fertilized egg is not visible, then an incomplete miscarriage is diagnosed. In this case, hospitalization in the gynecology department is necessary to scrape out the remains of the fertilized egg and stop the bleeding.
A non-developing pregnancy is characterized by smaller sizes of the fetal egg for a given period of pregnancy, its deformation, blurred contours, a decrease in the thickness of the chorion, and the absence of heartbeats of the embryo.
Localization of the fertilized egg in the cervical canal (cervical canal) is characteristic of cervical pregnancy. In this case, better visualization is achieved with transvaginal ultrasound. In this situation, urgent hospitalization in a hospital is necessary, since the likelihood of heavy bleeding is very high.
Quite often during pregnancy, a corpus luteum cyst occurs in one of the ovaries, which is a formation with a diameter of 3 to 8 cm with thick walls and a heterogeneous internal structure. This is the norm. A characteristic feature of this cyst is a gradual decrease in its size and disappearance by the end of the first trimester.
Hydatidiform mole is a rare complication observed in 1 case in 2000-3000 pregnancies, associated with chorion pathology, in which the chorion transforms into grape-shaped formations that destroy all other structures of the fetal egg. In this case, the uterus fills with many bubbles with fluid. An ultrasound visualizes a uterus larger than normal in size for a given stage of pregnancy, with an enlarged cavity filled with heterogeneous contents (the so-called “snow storm” picture).
Diseases and defects of the internal genital organs on ultrasound
When performing an ultrasound of the pelvic organs, the size of the uterus and ovaries is assessed, as well as the presence of pathological changes (uterine fibroids - a benign tumor of the uterus, cysts and tumor diseases of the ovaries) and congenital malformations (saddle uterus, bicornuate uterus, duplication of the uterus, septum in the uterine cavity and etc.). The most unfavorable situation is when the placenta is located above the myomatous node. In this case, there is a high risk of premature placental abruption.
Currently, three-dimensional ultrasound examination, which produces a “three-dimensional picture,” is becoming increasingly popular. Three-dimensional ultrasound makes it possible to diagnose some developmental defects at an earlier stage (for example, facial defects: cleft lip, etc.). But 3D scanning is a longer study, and, unfortunately, it is not always possible to obtain the necessary image. And the experience in three-dimensional ultrasound examination has not yet been accumulated. Therefore, most likely, this method is the future, and at present, three-dimensional ultrasound is just an additional research method.
So, ultrasound examination of the fetus and pelvic organs in the first trimester of pregnancy is one of the most important and irreplaceable diagnostic methods, allowing one to assess the development of pregnancy from the earliest stages and choose the right tactics for its management.
Size of fertilized egg by week of pregnancy
The size of the ovum by week is a very important indicator during pregnancy. For example, a gestational sac diameter of 3 mm corresponds to a gestational age of 4 weeks, and a gestational sac diameter of 6 mm corresponds to a gestational age of 5 weeks. An increase in the average diameter of the ovum occurs in the early stages of pregnancy at a rate of approximately 1 millimeter per day.
Most standard indicators for the average internal diameter of the ovum are limited to a period of 8-10 weeks. This is due to the fact that after 6–7 weeks of pregnancy, the size of the fertilized egg cannot reflect the growth of the embryo. With its advent, the coccygeal-parietal size of the embryo (CTE) is used to estimate the gestational age.
The dimensions of the average internal diameter of the ovum by week are given in the calculator .
Study of extraembryonic structures
In addition to the embryo, ultrasound evaluates the yolk sac, chorion and amnion.
During physiological pregnancy, the yolk sac (an extraembryonic structure that performs nutritional and hematopoietic functions in the first weeks of pregnancy) is determined when the ovum SVD is more than 10 mm (pregnancy period is more than 5 weeks) in the form of a white ring with a diameter of 2 mm (5 weeks) to 7 mm (10 weeks). A sign of an undeveloped pregnancy is also the absence of a yolk sac when the ovum is larger than 10 mm. After 12 weeks of pregnancy, the yolk sac is normally not detectable. There is a relationship between the size of the yolk sac and pregnancy outcome. An increase of more than 7 mm and a decrease of less than 2 mm, irregular shape and thickening of the walls of the yolk sac are prognostically significant only when combined with other disorders, such as changes in the thickness of the chorion (villous membrane), or delayed embryonic growth. An isolated discrepancy between the size of the yolk sac and the norm does not significantly affect the incidence of pregnancy complications.
Advertising
The chorion is the outer villous membrane of the fertilized egg. The fetal part of the placenta is formed from the chorion. During ultrasound, the chorion is visualized as a white ring with wavy contours, located along the outer edge of the fertilized egg. The thickness of the chorion in the first trimester in millimeters is approximately equal to the gestational age in weeks. Underdevelopment of the chorion (hypoplasia) or changes in its structure often leads to spontaneous abortion. The chorionic villi are interconnected with the inner (decidua - falling off) lining of the uterus. If this interaction is disrupted, detachment of the fertilized egg occurs. As a result, a retrochorial (located behind the chorion) hematoma (a limited collection of blood) is formed. Retrochorial hematoma is an ominous sign indicating an incipient miscarriage.
Amnion is a water membrane, which is a closed sac in which the embryo/fetus is located, surrounded by amniotic fluid. The amnion is adjacent to the chorion from the inside. Hypoplasia (underdevelopment) of the amniotic cavity leads to a non-developing pregnancy. In such cases, the diameter of the amniotic cavity does not exceed 10-12 mm for more than 6 weeks of pregnancy. An increase in the size of the amnion, characteristic of early polyhydramnios, and its heterogeneous contents (suspension in the amniotic fluid) are often associated with the presence of infection. Early polyhydramnios is an unfavorable sign.
Irregularly shaped ovum (deformed ovum)
If the fertilized egg is located in the uterine cavity, then such a pregnancy is called a physiological uterine pregnancy. A fertilized egg up to 5-6 weeks normally on ultrasound has a round or drop-shaped shape, surrounded by a thin membrane. By 6-7 weeks, it completely fills the uterine cavity and acquires an oval shape in a longitudinal scan, and a round shape in a transverse scan. If on an ultrasound the doctor sees a deformation of the fertilized egg (it is elongated, flattened on the sides, looks like a bean), then this may indicate uterine tone . A change in the shape of the fertilized egg is also possible with partial detachment. Significant deformation with unclear contours is observed during frozen pregnancy.
Timely diagnosis of deformation of the ovum during pregnancy makes it possible to save the child.