Pregnancy is a special period in the life of any woman. Regular examinations help to understand that something is starting to go wrong during pregnancy. A number of studies are mandatory for everyone, but there are also those that are prescribed individually, and the pregnant woman can refuse them. Optional tests include chorionic villus biopsy. As a rule, such medical manipulation is very frightening for expectant mothers. What is it? How long does it take to do it? And should we be afraid of such a procedure?
Chorionic villus sampling (CVS) is a test that provides a sample of placental ectopia that contains the same chromosome makeup as the embryo. Further study of the biomaterial allows us to find out at the chromosomal level the composition of the nuclei of the fetal cells without affecting the fetus itself. Unfortunately, this procedure cannot be considered a completely safe medical procedure. In addition, this is a fairly expensive study.
What is chorion and what does its study provide?
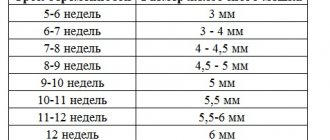
The chorion is the villous extra-embryonic outer membrane. It is formed 7-12 days after conception from the fusion of cells of the extraembryonic mesoderm and trophoblast. And from the end of the first trimester of pregnancy, the chorion gradually transforms into the placenta. At the same time, its tertiary well-vascularized villi form branches and form cotyledons (structural and functional placental units). In this case, direct contact between the maternal and fetal blood circulation finally ceases.
The main functions of the chorion include:
- Separation of the embryo from the tissues of the uterine wall. In this case, the chorion with its villous part is in contact with the decidua (formed from the endometrium). And its smooth part is the second layer of that part of the fetal sac, which is called the fetal membrane.
- Ensuring the exchange of substances and gases between the embryo and maternal blood (excretory and trophic functions). This is possible due to the growth of chorionic villi into the walls of the spiral arteries of the uterine wall.
- Protection of the embryo from infectious agents and toxins. This barrier begins to work fully from the 10th week of gestation, when the formation of the placenta begins. In the early stages of pregnancy, chorionic villi are not yet able to adequately filter substances contained in a woman’s blood. Therefore, this period is characterized by a fairly high probability of occurrence of disorders of embryogenesis of a toxic and infectious nature.
Chorion tissues are of embryonic origin. So their genetic material is basically the same as that of an embryo. And taking a small part of the chorion for research does not affect the process of organogenesis of the unborn child and in 97-99% of cases is not critical for prolonging pregnancy. This is exactly what is used when performing chorionic biopsy for the prenatal diagnosis of various hereditary anomalies.
How informative is chorionic villus biopsy?
Currently, chorionic villus biopsy followed by examination of the resulting material makes it possible to identify almost 3,800 different diseases. Moreover, the result obtained has a high degree of reliability.
The diagnostic capabilities of chorionic biopsy include identifying the following groups of diseases:
- Various chromosomal abnormalities (Down, Edwards, Turner, Klinefelter, Patau syndromes, etc.).
- Monogenic diseases with different types of inheritance.
- Enzymatic pathologies - for example, phenylketonuria, Lesch-Nyhan syndrome, citrulinemia, arginine succinic aciduria.
- Thalassemia and other hemoglobinopathies.
- Numerous lysosomal storage diseases. These include sphingolipidoses (Fabry, Crabbe, Landing, Tay-Sachs, Niemann-Pick diseases, adrenoleukodystrophy, etc.), carbohydrate metabolism disorders (glycogen storage diseases, Pompe disease), glycosaminoglycan metabolism disorders (various mucopolysaccharidoses), and glycoprotein metabolism disorders.
The reliability of identifying these diseases is very high. Diagnostic errors may be associated with technical errors when collecting material, when uterine tissue is also included in the chorionic villus biopsy. But this is rare. False-positive test results for mosaicism are also possible, when this chromosomal pathology occurs only in chorion cells.
Diagnostic errors occur in no more than 4% of cases. Moreover, they are usually associated with overdiagnosis, rather than false negative results. So the method as a whole has high accuracy. But it also has some limitations. For example, a chorionic villus biopsy will be uninformative if the embryo has defects in the formation of the neural tube that are not associated with pathology of the genetic material.
Of course, the diagnostic capabilities of the method depend on the technical equipment of the medical genetic center and the availability of certain reagents in it. Therefore, if a certain uncommon anomaly is suspected, the doctor must first clarify whether the necessary research can be carried out in this laboratory. If necessary, the material is sent to another region in compliance with the necessary transportation conditions.
When will the results be ready?
The results of chorionic villus biopsy are ready on average in 7-10 days. Laboratories with more modern equipment can conduct the test faster, and results should be expected within two days.
All this time, the biological material is multiplied under special conditions, isolated in an incubator. Analysis of the resulting cells shows the presence or absence of certain abnormalities in fetal development with 99% accuracy.
There are times when tissues lose their viability, and it becomes necessary to repeat the analysis.
The results are needed to:
- Make a decision to continue the pregnancy.
- Decide on the birthplace of your special baby.
- Decide on the type of birth: natural or caesarean section.
In what cases is research carried out?
Chorionic villus biopsy is not an ordinary test. It is carried out only if there are certain indications, if non-invasive diagnostic methods do not provide the necessary and reliable information. The decision on such manipulation is usually made by a medical commission and requires the mandatory informed consent of the woman. She has the right to refuse the proposed diagnosis, which is not the basis for any subsequent restrictions on the scope of the prescribed examination and treatment.
Indications for chorionic villus biopsy include:
- Previous birth of a woman with a child with disorders caused by any gene or chromosomal abnormalities. The fact of stillbirth or death of a newborn in the first few days is also taken into account.
- The presence of people in the family with hereditary diseases, even if they are not first-degree relatives. Confirmed carriage of a recessive pathological gene (including sex-linked) in at least one of the parents.
- An unfavorable result of the first mandatory prenatal screening (ultrasound and biochemical examination) with an identified high risk of certain chromosomal diseases in the embryo.
A relative indication is also the age of a woman over 35 years old. After all, this is associated with an increased likelihood of spontaneous critical mutations, especially in the presence of other factors predisposing to this.
Preparation
Invasive diagnostics during pregnancy causes concern for many women. In fact, today there are more modern studies of a non-invasive type. However, sometimes direct access to amniotic fluid or even the fetus itself may be required.
You need to understand that invasive studies are not always carried out. If there is a risk of harming the unborn child, the gynecologist will not prescribe this procedure. If we talk about preparatory activities, then first of all, doctors recommend not to bring yourself to a nervous state by reading scary stories on the Internet and how research is carried out.
If you need to get comprehensive information about the procedure, then you should talk to your doctor or get all the necessary data on specialized medical websites. Each situation is individual.
Before starting the research, it is necessary to do an ultrasound and pass the required tests. The doctor must make sure that the pregnant woman does not have hidden infections. Also, such procedures will help identify the presence of multiple births and assess the viability of the fetus. The gynecologist-obstetrician must accurately determine the gestational age. After this, he will prescribe a specific study.
4-5 days before the procedure, you must completely stop using acetylsalicylic acid (aspirin) and any analogues of this drug. The fact is that the drug thins the blood, which can negatively affect the quality of the examination.
Also, 24 hours before the event you need to stop taking anticoagulants (drugs that belong to the category of low molecular weight heparins). Such drugs reduce the level of blood clotting. Because of this, bleeding may occur during the procedure.
Additional advice on preparation should be obtained from your doctor. He may prescribe certain medications or a diet some time before the tests.
Contraindications
A planned chorionic villus sampling may be delayed or canceled in the following cases:
- high risk of threatened miscarriage - for example, with isthmic-cervical insufficiency, multiple myomatosis or the presence of a large fibroid node with significant deformation of the uterine cavity;
- already diagnosed threatened abortion (high uterine tone, appearance of bloody discharge from the genital tract);
- the woman has fever, a current acute infection, or a clinically significant exacerbation of a chronic infectious and inflammatory disease;
- features of the attachment of the chorion, which leads to its inaccessibility for biopsy;
- dermatitis or infectious lesion of the skin and subcutaneous tissue on the anterior abdominal wall diagnosed in a woman (with a planned transabdominal chorionic villus biopsy);
- vulvovaginitis of an infectious nature (in the case of transcervical chorionic biopsy);
- clinically significant deterioration in the general somatic condition of the pregnant woman.
Time frame for the study
The timing of chorionic villus biopsy is determined by the period when the embryo’s main organs and systems are already formed, its membranes are quite large, but the placenta has not yet fully formed. Therefore, the procedure is most often performed between 10 and 13 weeks of gestation.
In addition, during this period the risk of biopsy-provoked spontaneous abortions is significantly lower than in earlier periods. And the doctor usually already has the result of the first basic prenatal screening, which provides indicative information about the presence of signs of some of the most common chromosomal diseases.
At later stages, the chorion is gradually transformed into the placenta. Taking a sample (part) of this formation is also possible. But this is a different test called placentocentesis or placental biopsy.
A combination of several techniques is also possible. For example, sometimes chorionic villus biopsy and amniocentesis are performed using the same access (simultaneously). This makes it possible to significantly increase the information content and reliability of prenatal diagnosis, as it also makes it possible to obtain information about abnormal development of the fetus or its infection.
Can it be done during pregnancy?
Doctors try to avoid biopsies during pregnancy, so as not to additionally burden the female body. Usually it is postponed until childbirth and is recommended to be done 10-12 weeks after the birth of the baby. If the procedure is done too early, the results may be false. Samples are taken for analysis during pregnancy only when doctors have serious concerns about the health of the expectant mother. In such conditions, the procedure is prescribed for the second trimester, when the risk of negative consequences from it is minimal.
Find out how to treat ectopia, leukoplakia and cervical dysplasia.
If the test results of a pregnant woman show the presence of cancer cells, then most often a decision is made to terminate the pregnancy in order to save the woman. However, there are many cases when a pregnant woman carried and gave birth to a baby without problems, and treatment was carried out after. Each case is individual, so doctors weigh all the risks before offering a choice to the patient.
Types of research
Currently, 2 types of chorionic biopsy are practiced:
- Transabdominal, when access to the uterine cavity and fetal membranes is achieved by puncturing the anterior abdominal wall.
- Transcervical - through the cervical canal, without violating the integrity of the uterine wall.
Transabdominal chorionic villus biopsy can be single-needle or double-needle.
Currently, the transabdominal technique is most often preferred. In this case, the specialist gains access to the chorion located along the front or side walls at any level. But when attaching an embryo along the posterior surface of the uterus, it is advisable to use the transcervical technique.
How is chorionic villus sampling performed?
Before the procedure, the woman is given a preliminary examination. It includes general clinical blood and urine tests, analysis for major infections, and a vaginal smear to determine the degree of purity. Ultrasound is also a mandatory procedure, despite the first screening being recently performed. Often, sonography is performed on the day of the biopsy. In fact, the specialist first assesses the condition of the uterus and the position of the embryo, after which he begins the procedure for collecting biomaterial.
Although chorionic villus sampling is an invasive procedure, it is performed in the vast majority of cases without the use of anesthesia. In the case of the transabdominal technique, application anesthesia can be used, if necessary, to reduce discomfort at the time of skin puncture.
Chorionic villus biopsy is performed under mandatory ultrasound control of the position of the puncture needle. In this case, the free-hand method or a special puncture adapter can be used. 1-2 hours before the examination, the woman is recommended to drink several glasses of water, which will fill the bladder and thereby significantly improve visualization of the uterine cavity.
In general, the procedure (for the transabdominal option) includes:
- Antiseptic treatment of the area on the abdomen that is supposed to be used for puncture.
- Linear puncture of the tissues of the anterior abdominal wall and uterus with immersion of the tip of the puncture needle into the myometrium.
- Changing the position of the needle so that it is directed parallel to the chorionic membrane.
- Immersion of the needle into the chorionic tissue, removal of the mandrin and gentle aspiration of the sample. In this case, to collect the material, a syringe with a transport medium is attached to the outer contour of the needle. If a two-needle technique is used, only the inner needle of a smaller diameter is immersed into the chorion. A thicker guide needle acts as a trocar for the initial puncture of the abdominal wall and uterine wall.
- Removing the needle, covering the puncture site with an aseptic bandage, ultrasound monitoring of the embryo's heartbeat and the condition of the uterine wall.
During transvaginal chorionic biopsy, material is collected using a flexible thin catheter with a mandrel. In this case, the cervix is fixed by grasping it with bullet forceps. The tip of the catheter is also inserted into the chorion parallel to the uterine wall under ultrasound guidance.
Usually the entire procedure takes no more than 30 minutes. Although, when the chorion is located on the side walls of the uterus or in its corners, technical difficulties with access are possible, which will increase the duration of the biopsy.
For a full diagnosis, it is necessary to obtain at least 5 mg of chorionic tissue. The optimal biopsy volume is 10-15 mg. This will allow you to conduct several types of research if necessary.
Possible risks of the procedure
The invasiveness of this technique is the main risk factor for the development of possible complications and consequences. True, they occur infrequently and are not always associated with technical errors in the biopsy performed or insufficient experience of the doctor. In general, according to medical statistics, no more than 4-5% of patients experience serious complications.
Possible negative consequences of chorionic villus sampling include:
- Spontaneous abortion (miscarriage) during the first 5-7 days after the procedure. Diagnosed in 2–2.5% of cases. The risk of induced miscarriage is higher with transcervical chorionic villus biopsy.
- Bloody discharge from the genital tract, which occurs mainly in women after transcervical chorionic villus biopsy. They may be associated not so much with damage to the chorion itself, but with injury to the cervix from bullet forceps. Nevertheless, the patient's complaints of bleeding require clarification of the source of bleeding with the obligatory exclusion of a threatened abortion. About 20-25% of women after transcervical chorinobiopsy experience this phenomenon. And in most cases, it stops on its own and without any negative consequences.
- Formation of retrochorial hematoma. It is considered a factor that increases the likelihood of abortion. But in most cases, such a hematoma resolves by the 16th week of gestation and does not affect the development of the fetus. And when it breaks into the uterine cavity, a woman may experience brownish-bloody, light discharge from the genital tract.
- Development of chorioamnionitis. It is a rare complication. Many authors point out that there are no significant differences between the frequency of post-biopsy and spontaneous chorioamnionitis.
- Violation of the integrity of the fetal membranes, which is most likely with transcervical chorionic villus biopsy. It is fraught with leakage of amniotic fluid and the development of infectious complications.
- When performing chorionic biopsy in the early stages of gestation, congenital transverse amputations of the limbs are possible due to trophic disorders in the area of intervention. By the end of the 1st trimester, the risk of developing this complication is leveled out. That is why, since 1992, chorionic villus biopsy has been performed no earlier than the 8th week of gestation, preferably from the 10th week.
- Increased serum α-FP levels. It is transient in nature, does not require drug correction and usually resolves by 16-18 weeks of gestation. However, it is necessary to take into account the risk of such a consequence when prescribing biochemical screenings in the 2nd trimester in order to exclude false-positive results for the likelihood of defects.
- Alloimmune cytopenia in the fetus, which is possible during Rh-conflict pregnancy. To prevent this, it is practiced to administer anti-Rhesus immunoglobulin to previously non-sensitized women with Rh-negative blood, if the father of the child is Rh-positive. The drug is usually administered in the first 48-72 hours after chorionic villus biopsy.
In general, despite its invasiveness, this diagnostic technique rarely leads to the development of truly severe complications. Of course, a lot depends on the doctor’s skills and the pathology present in the woman and/or embryo.
Possible complications
Since the procedure is invasive, there is a risk of complications:
- miscarriage. It can happen 5–7 days after the procedure;
- bleeding from the vagina. They can appear due to damage to the chorion and injury to the cervix. Bleeding is observed in about a quarter of women after the procedure. Light discharge goes away on its own as the wound heals. But if the bleeding is quite severe, you should immediately consult a doctor to prevent abortion;
- retrochorial hematoma. Its occurrence increases the likelihood of abortion. However, it may resolve on its own by the end of the 4th month of pregnancy. The hematoma does not affect the development of the fetus. But it can break into the uterine cavity, which will lead to light brownish discharge from the vagina;
- Chorioamnionitis. This is a fairly rare complication of chorionic villus sampling. The fetal membranes become inflamed and the amniotic fluid becomes infected;
- damage to the membranes of the fetus. This can lead to leakage of amniotic fluid, which can lead to an infectious process;
- congenital amputations of limbs. This can happen due to the biopsy being performed very early in pregnancy - before the 10th week. Atrophic changes may begin in the area of intervention. This complication does not appear if the procedure is carried out within the permitted time frame;
- alloimmune cytopenia in a child. This complication can occur if there is a Rh conflict during pregnancy. Therefore, it is recommended that anti-Rhesus immunoglobulin be administered to all women with a negative Rh factor if the father is positive. It is advisable to administer the drug within 24 hours after chorionic villus biopsy.
Such complications are observed only in 4–5% of cases. To avoid their occurrence, you need to contact a qualified specialist with extensive experience and take into account all contraindications.
Chorionic villus biopsy is a very informative prenatal study. But it is prescribed only if there are serious indications, since the likelihood of complications developing is quite high.
Chorionic biopsy or chorionic villus biopsy is one of the modern invasive methods of direct prenatal diagnosis. It is intended for collecting tissue samples of embryonic origin with their subsequent molecular genetic, cytogenetic, and biochemical studies. Chorionic biopsy is performed strictly according to indications and only at certain times of gestation by specialists who have the appropriate certificate and experience.