Prolapse of the uterus is its unnatural position when the organ is below its anatomical and physiological border. This happens due to weakness of the pelvic muscles after pregnancy, as well as the uterine ligaments. Most clinical cases are accompanied by displacement or very low location of the organ, when it is as close as possible to the bottom of the vagina. Among the complications, the main one is the risk of prolapse of the uterus from the vaginal opening.
- Causes
- Symptoms
- Treatment
- Prevention
The pathology is characterized by the preservation of the cervix in its place. Another known name for the pathology is pelvic organ prolapse. As a rule, women of pre-retirement age, as well as girls who have undergone pregnancy, are at risk of its occurrence.
Typically, the reproductive organ is attached to the small pelvis with the help of ligaments, as well as muscles and fascia located in the pelvic floor. The reason for its lowering is a situation when the muscles holding the organ lose their tone.
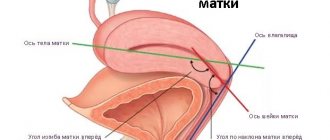
The structure and functioning of the pelvic organs in women is normal
The pelvic organs include the bladder, urethra, uterus, vagina, rectum, and the pelvic floor on which they are located (Figure 1).
Rice.
1. Pelvic organs in a woman (normal location): 1 – pubic symphysis (junction of the pubic bones), 2 – bladder, 3 – urethra (urethra), 4 – uterus, 5 – vagina, 6 – rectum.
About 50% of the human body weight is connective tissue. Its main function is to maintain a constant structure of the body and integrate all other tissues together, ensuring their constant and orderly arrangement. Ligaments and fascia are typical representatives of connective tissue.
The vagina has anterior and posterior walls that border the bladder and rectum (see Fig. 1). The bladder, vagina, and rectum are hollow organs and are not able to maintain their shape in space. The frame (supporting) function is performed by connective tissue films - fascia and ligaments, which fix them to the pelvic bones, muscles and tendons. In such a stable state, the bladder, vagina and rectum can fully perform their functions. On the contrary, failure of connective tissue leads to structural changes in the supporting apparatus, which cause disruption of the pelvic organs.
Rice. 2.
Schematic representation of the structures of a woman’s pelvic floor (normal). Red colors indicate the pelvic floor muscles (levators and sphincters), blue colors indicate fascia and ligaments. 1 – bladder, 2 – uterus.
Many ligaments, fascia and muscles surrounding the pelvic organs on all sides make up the pelvic floor
– a complex anatomical formation that ensures the functioning of the bladder, urethra, uterus, vagina and rectum (Fig. 2). The pelvic floor is in constant tone, maintaining the shape and position of the pelvic organs, and at certain moments (urination, defecation, coughing, increased intra-abdominal pressure, etc.) it changes its configuration in accordance with the situation (Fig. 3).
Rice. 3.
The interaction of ligaments, fascia and muscles allows you to maintain constant tone of the pelvic floor. Red arrows indicate the main vectors of muscle effort. At rest they are in equilibrium, and if necessary they decrease or increase. For example, when urinating, the posterior vector sharply prevails over the anterior one. 1 – bladder, 2 – uterus.
Stress urinary incontinence and pelvic organ prolapse are the result of damage to various ligaments and fascia of the pelvic floor. Next, we will look at the anatomical defects that lead to involuntary loss of urine and prolapse of the pelvic organs through the vagina.
Back to contents
Diagnostics
Since the first stage of prolapse is extremely difficult to determine on your own, a woman should visit a gynecologist systematically (at least once every six months). During the examination, the doctor usually immediately diagnoses the prolapse. If the gynecologist has doubts about the diagnosis, he sends the patient for an ultrasound. When a woman is diagnosed with a rectocele or cystocele, she is referred for examination to a specialist - a urologist or proctologist. They prescribe the optimal solution, the effectiveness of which directly depends on the stage of the disease. Typically, the presence of a rectocele is detected by palpation of the rectum, and a cystocele by catheterization of the bladder.
Additionally, the patient is prescribed smears for vaginal microflora, as well as a general urine analysis.
Pathogenesis of pelvic organ prolapse
The main supporting structure of a woman's pelvic floor is the ligaments and fascia. Damage to them leads to a condition that is commonly called pelvic organ prolapse or prolapse: bladder, uterus, rectum. The term “prolapse of the vaginal walls” is usually used, but it does not reflect the entire essence of the process, but only indicates external manifestations.
The vagina can be compared to a tent, which is held up by fixing the central part. In the ligamentous apparatus of the pelvic floor, the central part is the fibrous ring surrounding the cervix. The ring is woven into the uterosacral and cardinal ligaments, as well as the pubocervical and rectovaginal fascia - supporting structures for the walls and vaults of the vagina. (Fig. 4).
Rice. 4.
The ligamentous apparatus that fixes the cervix is the top of the pelvic floor. CMM – cervix, OFC – pericervical fibrous ring, SDT – arch of the pelvis. UCL – uterosacral ligaments, CL – cardinal ligaments, RVF – rectovaginal fascia.
The cervix is “suspended” in the middle of the pelvis by ligaments, like a parachutist on the lines of a parchute. When the ligaments are partially or completely destroyed, the cervix, under the influence of intra-abdominal pressure and gravity, begins to fall down and pull neighboring organs with it (Fig. 5). This situation is called apical (upper) prolapse.
Rice. 5.
Prolapse of the uterus is a consequence of damage to the ligamentous apparatus: the uterus “pulls” neighboring organs with it – the bladder and rectum.
Figure 6 shows the extreme form of POP - complete uterine prolapse. In this situation, the vagina is completely turned outward, like a bag, the contents of which can be the bladder, uterus, rectum, and loops of the small intestine. The reason for the situation is the total destruction of the ligamentous-fascial apparatus of the pelvic floor.
Rice. 6.
Complete prolapse of the pelvic organs (diagram and photo).
The pubocervical fascia is located between the bladder and the anterior wall of the vagina, and the rectovaginal fascia is located between the rectum and the posterior wall of the vagina. Damage to the first leads to prolapse (prolapse) of the bladder into the vagina, and damage to the second leads to prolapse (prolapse) of the rectum. This is how prolapse of the anterior and posterior walls of the vagina develops, or rather cystocele - prolapse of the bladder and rectocele - prolapse of the rectum (Fig. 7).
Rice. 7.
Supporting apparatus of the bladder and rectum.
a
– fascia holds organs in a physiological position;
b
– rupture of the pubocervical fascia leads to prolapse of the bladder (cystocele).
If the ligaments that hold the female urethra (urethra) in the correct position are damaged, stress urinary incontinence develops (coughing, sneezing, laughing, running, etc.).
Factors contributing to the development of pelvic organ prolapse
- Traumatic and prolonged labor (quick and protracted labor, delivery of a large fetus, surgical obstetrics) - cause injuries to the ligaments and fascia of the pelvic floor;
- Systemic connective tissue dysplasia is a congenital deficiency of connective tissue;
- Estrogen deficiency (decrease in general and local levels of female sex hormones) - leads to dystrophy of the connective tissue and muscles of the pelvic floor, skin and mucous membranes of the pelvic organs;
- Chronic diseases (bronchitis, asthma, constipation, etc.), physical work accompanied by increased intra-abdominal pressure - constant stress on the pelvic floor;
- Chronic inflammatory diseases of the pelvic organs - lead to disruption of the processes of microcirculation of blood and lymph in the pelvis, as a consequence to tissue degeneration;
- Obesity - increased abdominal pressure;
- A sedentary lifestyle (sedentary work) means constant stress on the pelvic floor.
Back to contents
Reasons for prolapse
The main reason for the displacement is a violation of the elasticity of the muscles and tissues of the pelvic floor. As a result, the ligaments and muscles cannot hold the uterus and intestinal loops in their typical position. The organs become increasingly heavy on the pelvis, putting pressure on it. As a result of weakening muscle tissue, the pelvis ceases to support the internal organs, so they begin to shift downward.
The following additional reasons for omission are identified:
- Consequences of childbirth. Prolonged or vice versa - too rapid labor, a large fetus, the use of obstetric forceps and other difficulties in the birth process may not have the best effect on the elasticity of the uterine tissue.
- Repeated births. Having a second child greatly increases the risk of prolapse.
- Age factor. Prolapse of the posterior wall of the uterus or the entire organ is often observed in old age, in women who have entered menopause.
- Sudden loss of excess weight. At the same time, body tissues lose elasticity and sag, just like organs.
- Excessive physical activity, frequent carrying of heavy objects.
- Disruption of the gastrointestinal tract. In case of defecation disorders, the overcrowded intestines put pressure on the uterus, causing its displacement.
- Consequences of surgery. The walls of the vagina may shift if a previous operation to remove the uterus took place without additional fixation of the vaginal dome.
Types and degrees of pelvic organ prolapse
The most common types of PTO are:
- Cystocele
– prolapse of the bladder and anterior vaginal wall (Fig. 8); - Rectocele
– prolapse of the rectum and posterior vaginal wall (Fig. 9); - Uterocele
– uterine prolapse or apical prolapse (Fig. 10); - Prolapse of the
vaginal dome (Fig. 11).
Cystocele
- prolapse of the bladder, often called prolapse of the anterior vaginal wall. This is not entirely accurate, since this term describes only the external manifestation of the problem - a visually detectable vaginal wall located lower than it should be, or even “peeking out” beyond the entrance to the vagina.
Cystocele is the most common type of POP in women. The most typical complaints with this pathology are: frequent urination, difficulty urinating, a feeling of incomplete emptying of the bladder, heaviness in the lower abdomen.
Rice. 8.
Prolapse of the bladder – cystocele (arrow).
Rectocele
- prolapse of the posterior vaginal wall. The most typical complaints with rectocele: constipation, difficulties in emptying the rectum (the need to “reduce the vagina”), urination disorders, sensation of a foreign body in the perineum.
Rice. 9.
Prolapse of the rectum – rectocele (arrow).
Uterocele
— prolapse, prolapse of the uterus is often combined with prolapse of the bladder (cystocele) and/or rectum (rectocele), so complaints will be characteristic of both diseases.
Rice. 10.
Prolapse of the uterus - uterocele.
Dropping out
The vaginal dome develops only after hysterectomy (complete removal, along with the cervix).
If the uterus was removed due to its prolapse, then the likelihood of developing the picture presented in Figure 11 increases 5 times.
This clearly indicates the inadvisability of removing the uterus as a therapeutic measure for prolapse!
Rice. eleven.
Prolapse (drawing) and prolapse (photo) of the vaginal dome after removal of the uterus.
Classification of uterine prolapse by severity
In the international literature, the Baden-Walker classification of pelvic organ prolapse is most often used (Fig. 12). It involves four stages:
- Stage 1
– the most prolapsing point reaches half the length of the vagina; - Stage 2
– the most prolapsing point of the vagina reaches the hymenal ring (entrance to the vagina); - Stage 3
– the most prolapsing point extends beyond the hymenal ring to half the length of the vagina; - Stage 4
– the vagina falls out completely.
Rice. 12.
Scheme of classification of PTO according to Baden-Walker and stages of uterine prolapse.
Back to contents
Symptoms
The initial stage is sometimes asymptomatic, and the patient often does not even realize that she has signs of displacement. The second and subsequent stages of loss are impossible not to notice. The following symptoms indicate prolapse problems:
- heaviness in the vagina, sensation of the presence of a foreign body;
- difficulty defecating and urinating, and the urge to do so, on the contrary, is more frequent;
- disruptions of the menstrual cycle, accompanied by heavy and painful menstrual bleeding.
- discomfort and pain for both partners during intimacy;
- atypical vaginal discharge (sometimes with blood clots).
Symptoms of prolapse, prolapse of the uterus and vaginal walls
Prolapse of the uterus and vagina leads to a marked deterioration in the quality of life and desocialization of a woman. Complaints are almost never limited to “sensation of a foreign body in the vagina.”
The abnormal position of the pelvic organs leads to severe disturbances in the functioning of the bladder and rectum, creates difficulties during sexual activity up to complete refusal of the latter, and is the cause of chronic pain syndrome.
Complaints from patients suffering from pelvic organ prolapse:
- A noticeable anatomical defect in the area of the vaginal opening, aching pain and a feeling of heaviness in the lower abdomen, a sensation of a foreign body in the vagina;
- Impaired urination (incomplete emptying of the bladder, difficulty urinating, frequent urge to the point of urinary incontinence, recurrent cystitis);
- Impaired defecation (constipation, difficulty defecating, incontinence of gas and stool);
- Violation of sexual function, up to refusal of intimate intimacy;
- Chronic inflammation and vaginal discharge.
Uterine prolapse is usually combined with other types of prolapse and has mixed symptoms.
Back to contents
Complications and consequences
If you start treatment at the initial stages of the disease, the prognosis will be favorable. A woman with grades 1 and 2 of cervical prolapse can restore muscle elasticity without resorting to surgery. The lack of timely therapy leads to rapid progression of the pathology. The patient’s condition is aggravated by increased physical activity, stress, and lack of personal hygiene.
Complications of the pathology include:
- complete loss of the cervix from the vagina, and with it the uterus and intestinal loop;
- infection of the urinary system leading to kidney failure;
- vaginal eversion;
- chronic pelvic pain;
- infertility.
To prevent cervical prolapse, it is recommended to regularly see a gynecologist. During the next examination, a specialist may suddenly identify a pathology. Women of reproductive age need to be examined at least once a year, and after menopause, visit a gynecologist every six months.
Surgical methods for treating prolapse of the uterus and vaginal walls
Connective tissue (dense fibrous) is designed in such a way that it is not able to adequately recover after damage (ruptures). This means that if the ligaments and fascia have been seriously damaged, then the only reliable way to restore their structure is surgery. Considering all of the above, pelvic organ prolapse (prolapse) can only be cured surgically.
There are only two ways to restore any frame: repair its parts or replace them with new ones. By analogy, there are two ways to reconstruct the pelvic floor, the first is to restore the fascia and ligaments with plastic surgery using your own tissues, the second is to strengthen the supporting apparatus using mesh prostheses (implants). As a rule, these methods are combined.
Colporrhaphy
Colporrhaphy
- vaginal plastic surgery using one’s own tissues, used only for the treatment of moderate median cystocele and rectocele, often in combination with levatoroplasty. The technique consists of suturing the defect and strengthening the vaginal wall with intact fascial tissue. With a correct diagnosis and patient selection, the effectiveness of the technique is up to 80%. Colporrhaphy is not effective for connective tissue dysplasia and severe forms of prolapse. Vaginoplasty is a stage of pelvic floor reconstruction surgery using mesh implants.
Rice. 13.
Anterior colporrhaphy. Scheme of plastic surgery of the anterior vaginal wall for cystocele.
Rice. 14.
Posterior colporrhaphy. Scheme of plastic surgery of the posterior vaginal wall for rectocele.
Pelvic floor reconstruction with mesh implants
As a method of treating pelvic organ prolapse in women, mesh implants have been used since the 80s of the last millennium, and today there is no alternative to them. Prosthetics are used when something needs to be replaced. Mesh implants are used to treat severe forms of pelvic organ prolapse (grade 3, 4), when the supporting apparatus is practically destroyed.
The essence of the method is to create artificial ligaments that fix the female pelvic organs in a normal anatomical position. Restoring the normal anatomy of the pelvic floor automatically leads to normalization of the function of the pelvic organs.
Rice. 15.
Reconstruction of the pelvic floor ligaments with a mesh prosthesis. The mesh implant is indicated in green.
I want to bring joy to all the women of our vast country who suffer from severe prolapse of the uterus and vaginal walls. Today you have the opportunity to undergo surgery QUALIFIEDLY AND FREE OF CHARGE AT THE EXPENSE OF COMPLIANCE MEDICAL FUNDS, although for this you will have to travel to the city of St. Petersburg to the North-Western Center for Pelvioperineology. This facility specializes in the treatment of pelvic organ prolapse and stress urinary incontinence.
There are center employees in many regions, I am a representative in Krasnoyarsk and the Krasnoyarsk Territory, I diagnose and select patients with pelvic organ prolapse for free surgical treatment under the compulsory medical insurance program. You can ask me questions by phone.
Examination for surgical treatment and expiration dates of tests
Valid for 6 months:
- Fluorography;
- Cervical smear for oncocytology.
Valid for 3 months:
- Blood test for HIV (AIDS);
- Blood test for RW (syphilis);
- Blood test for hepatitis B and C viruses;
- Ultrasound of the pelvic organs;
Valid for 1 month:
- Blood group and Rh factor.
- Clinical blood tests;
- General urine analysis;
- Biochemical blood tests (sugar);
- ECG;
- A certificate from a therapist with a detailed diagnosis and a conclusion about the absence of contraindications to surgical treatment.
Valid for 10 days:
- A smear to determine the degree of vaginal cleanliness (if infections and inflammation are detected, treatment is indicated).
Based on the results of the preoperative examination, a second consultation is carried out, the date of the operation and preoperative preparation are set.
Preparation for surgical treatment
- Stop sexual intercourse two days before surgery.
- The day before, cut or shave the hair on the pubic area, labia and perineum.
- On the eve of the intervention, go to bed no later than 22:00. You can take a sedative: tinctures of motherwort, peony, valerian, etc., according to the instructions included with the medications.
- In the morning, on the day of surgery, empty your bowels, take a shower and thoroughly clean the external genitalia, and put on clean knitted underwear.
- Hunger – last meal three hours before surgery.
- Immediately before the procedure, empty your bladder.
- HAVE WITH YOU:
- Referral for surgery, examination results (ultrasound and tests).
- A clean shirt (robe) and socks, sanitary pads, slippers. Leave jewelry (earrings, rings, etc.) at home.
Back to contents
Disease prevention
If there is a risk of developing prolapse of the anterior wall of the uterus due to hereditary characteristics, then preventive measures should be taken from an early age.
The attending physician prescribes a set of exercises to prevent the development of pathology. In addition to this, a special diet is prescribed to correct body weight.
If the disease does occur and the first signs of the disease appear, you should immediately avoid heavy physical activity and consult a doctor.
Like any disease, prolapse of the uterine wall can be prevented; for this you need to regularly visit the gynecologist, exercise, and also avoid obesity and heavy physical activity.
Conservative treatment of prolapse of the uterus and vaginal walls
Conservative treatment methods are used in the early stages of pelvic organ prolapse in order to prevent the progression of the disease, or in cases where surgical treatment is contraindicated, in order to alleviate the symptoms of the disease.
Unfortunately, neither pelvic floor muscle training, nor laser exposure, nor medications, nor reflexology can provide acceptable effectiveness. It is important to note that the pelvic floor muscles are not directly related to the development of pelvic organ prolapse; they are not even located in the areas where defects form.
Pelvic floor muscle training
Above, we examined the mechanism of development of pelvic organ prolapse, demonstrating that the ligaments and fascia of the pelvic floor are “to blame” for all the troubles, which after damage do not fully recover on their own. Therefore, training the pelvic floor muscles, which are not directly involved in the pathological process, is practically meaningless in the treatment of the pathology in question. Moreover, without qualified consultation, these exercises can lead to progression of prolapse and worsen the situation. Muscle training gives good results for incompetent pelvic floor muscles.
Vaginal pessaries
As a palliative measure, pessaries are used - devices that are installed in the vagina in the form of “spacers” and thereby prevent its loss. This kind of “crutch”, which helps a woman alleviate the symptoms of the disease and improve the quality of life, is an effective alternative to surgical treatment. (Fig. 16, 17).
Rice. 16.
Vaginal ring.
Rice. 17.
Various types of pessaries.
This approach does not lead to a cure, but it does improve the patient’s condition. Wearing pessaries is associated with the risk of developing an inflammatory reaction of the vaginal mucosa to a foreign body and requires compliance with certain rules and skills in using this device, which implies certain training.
Pessaries are selected by the gynecologist individually in size and shape, depending on the type and degree of prolapse. You can sign up for the selection of a pessary in Krasnoyarsk by calling 8 391 201-11-92.
Selection and rules for using vaginal pessaries
Physiotherapy
The use of physical factors is effective in the early stages of the disease, when there are still no complaints and the diagnosis is made only during examination on a gynecological chair.
There are various methods of influencing the vaginal walls and underlying tissues with physical factors (laser, magnetic field, etc.). This method can lead to a reduction in the degree of prolapse by improving tissue nutrition. There is no evidence base for these methods yet.
Physiotherapy is widely used as a recovery stage after surgical treatment and as a preventive measure for the development of prolapse in the postpartum period.
Volume-forming methods
The method is used mainly for the treatment of urinary incontinence in the early stages of the disease. It consists of creating additional support for the urethra during stress urinary incontinence through tissue tension by creating additional tissue volume under the urethra.
Hyaluronic acid fillers and your own fat (lipofilling) are used. With hyaluronic acid fillers, the effect is temporary - from 6 to 12 months. , for lipofilling long-lasting, almost permanent.
Back to contents
Degrees of the disease
Depending on the severity of the disease, uterine prolapse is divided into 4 stages:
- At the first stage of the disease, the uterus moves slightly downward, but the cervix remains in place.
- At the second stage, the cervix moves into the vagina, and the uterus is already in its vestibule. Often, when the muscles are tense, you can see the uterus through the genital slit, and therefore, a woman at the second stage can diagnose her own pathology.
- Incomplete prolapse occurs: the cervix and part of the uterine body protrude beyond the vagina.
- At the fourth stage, the uterus and cervix completely fall out of the perineum.
Prevention of pelvic organ prolapse
- Gentle delivery;
- Timely treatment of pelvic floor muscle failure - perineoplasty, sphinctero-levatoroplasty;
- Treatment of chronic diseases (bronchitis, asthma, constipation, etc.) accompanied by increased intra-abdominal pressure;
- Hormone replacement therapy for hormonal deficiency (perimenopause and menopause);
- Changing working conditions and lifestyle, combating obesity;
- The use of conservative treatment methods in the early stages of the disease.
Back to contents
Make an appointment
Surgical treatment
But surgery remains a radical measure for uterine prolapse. There is no “ideal operation” for this pathology. Any surgical intervention has its pros and cons. All types of surgical intervention are divided into several groups:
- operations that aim to strengthen the pelvic floor muscles - colpoperineolevatoplasty (this is usually the vaginal stage of a two-stage operation);
- operations on the uterine ligaments (shortening and suturing of the round ligaments to the anterior wall of the uterus);
- surgical strengthening of the ligaments that fix the uterus (cardinal, uterosacral) - the operation disrupts the patient’s reproductive function;
- rigid fixation of the uterus and vagina to the pelvic walls (sewn to the pubic symphysis, sacral bone, and others);
- operations using alloimplants (endoprostheses);
- operations that partially narrow the vagina;
- hysterectomy (if there are additional indications).
Surgical intervention can be performed through vaginal access, by transection or laparoscopically, simultaneously or in several stages. The percentage of recurrences of uterine prolapse remains high (reaches 30%). In the postoperative period, it is important to follow the doctor’s recommendations:
- restriction of carrying heavy objects (no more than 5 kg) for 1.5 months;
- sexual rest for 6 weeks;
- a ban on physical activity for 2 weeks, then minor physical activity is allowed.
Subsequently, you should monitor your bowel function, empty your bladder on time, promptly treat diseases of the bronchopulmonary system, avoid carrying heavy objects and engage in certain sports (cycling, rowing).
Author:
Sozinova Anna Vladimirovna obstetrician-gynecologist