As we grow up, we learn what vaginal discharge is and how to deal with it. Menstruation and leucorrhoea during the intermenstrual period are normal; if unusual discharge appears, you will make an appointment with a gynecologist and receive recommendations. However, if you have entered such a wonderful period as pregnancy, discharge takes on special significance.
At each visit to the antenatal clinic, the obstetrician-gynecologist will ask you:
- is there any discharge? — what color and quantity are they (abundant, scanty, smearing, etc.)? — is the discharge accompanied by itching in the perineum, pain in the lower abdomen, changes in fetal movements?
...and other clarifying questions. He may also ask to show the discharge on the pad (pad) or invite you to be examined on a chair.
Fetus
At week 22, the fetus continues to develop systematically and is actively gaining body weight. His height is 27-30 centimeters, the child’s weight is 450-500 grams.
External features include the following:
- The crumb becomes noticeably thicker, a subcutaneous fat layer appears;
- The child's eyes open;
- The first layer of hair (lanugo) grows on the head, which protects the baby from constant exposure to liquid. Subsequently, a lubricant is formed, which, thanks to lanugo, is not washed off from the skin. Later, most of the hair falls out before birth.
- The brow ridges, eyelashes, and toenails and fingernails are formed.
- The heart increases in size. Pulse is about 160-170 beats per minute.
- Improvement of the intestines and genitals continues.
- Sweat glands are formed, which are already able to function.
Physical and psycho-emotional development of the fetus at 6 months from the moment of conception:
- The baby is able to control his feelings and emotions and express discomfort.
- The brain cells are fully formed, its weight is 100 grams. The central nervous system is strengthened.
- The child actively moves and reacts to stroking the abdomen, light, and loud sounds.
- The baby is able to suck his finger, touch his face, grab and feel, and can tap the walls of the placenta.
Fetus at 22 weeks of pregnancy
Help! Restless behavior of a child can become the starting point of intrauterine hypoxia. If you suspect a pathology, consult a doctor.
What is important to know about your baby's movements?
The baby has grown significantly and is now expressing himself by resting his legs or palms on his mother’s belly. The bulging of the abdomen is now clearly visible visually.
At 26 weeks of pregnancy, the baby’s movements become even more noticeable and clear. Sometimes, by resting his legs against the mother’s ribs, the baby can even cause pain to the woman.
Don't forget to monitor your child's activity.
A woman during this period of pregnancy feels at least 1 shock every 10 minutes. If your baby at 26 weeks of pregnancy does not move or kick for more than a day, rush to the doctor immediately!
But frequent movements and excessive activity of the baby can signal that the child does not receive enough oxygen.
Condition of the expectant mother
The powerful restructuring of the body, which began from the moment of conception, directly controls the change in weight and general well-being of a pregnant woman. At week 22, body weight grows much faster than at week 10.
The mother experiences the following changes:
- The skin, nail plate, and hair improve due to changes in hormonal levels.
- The mood and psychological state of the pregnant woman becomes much better.
- Stretch marks appear on the stomach and thighs, which can be removed with special creams. Sport will have a positive effect in the fight against them.
- Painful sensations in the lower abdomen associated with an enlarged uterus. Adequate rest will help you cope with this.
- Due to a lack of calcium, seizures may occur.
Feel
Many changes occur in a woman's body at 22 weeks. The mother develops trembling feelings, which are associated with the fact that a stirring inside the abdomen is clearly felt. Now the baby is able to push and push against the walls of the uterus.
Among the negative points it is worth highlighting:
- Increased sweating . This problem can be solved by drinking plenty of fluids and buying things made from natural materials (cotton, linen).
- Discomfort in the abdomen , which is associated with prolapse of the uterus. Talk to your doctor about purchasing a drain that will support your uterus and relieve pressure on your lower back.
- Heartburn and burning in the stomach . It can only be eliminated by following a proper diet.
- Swollen legs that prevent you from enjoying this wonderful period of life. This is due to the increase in weight, which increases the stress on them.
- Bladder diseases are caused by the growing uterus, so don’t be patient and visit the toilet as soon as possible.
Reference! It is recommended to consult a doctor if you notice that the fetus has not moved for quite some time (1 day or more).
Stomach
The volume of the abdomen at 22 weeks of pregnancy is quite decent, so you need to buy comfortable clothes that will not restrict movement. Although the interesting position is already quite noticeable to others, a woman can bend over, sit quietly, and also tie her shoelaces.
The growth rate of the belly begins faster, so the belly will become more noticeable every week.
For some, this process is accompanied by unpleasant itching. Try to moisturize and nourish delicate skin with special creams that have a smoothing effect and will eliminate aesthetic imperfections on the body after the birth of a child.
Discharge
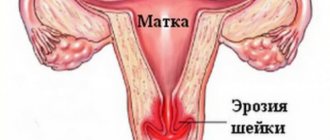
At the 22nd week of pregnancy, moderately mucous, light-colored discharge with a slight sour odor is considered normal. Deviations from the norm at the threshold of the 6th month of gestation are the following characteristics:
- A yellowish or greenish tint to the discharge indicates the presence of a sexually transmitted infection. You need to visit a doctor.
- Cheesy clots with lumps or mucus on underwear are a common symptom of an infectious process. A visit to the doctor will definitely solve this problem.
- Bloody discharge is a clear sign of premature birth. A woman in labor urgently needs to call emergency services. Another cause of vaginal bleeding is placental abruption.
- The extreme location (previa) of the placenta may be accompanied by blood-streaked discharge. Such pathology is detected during a routine examination.
- You should immediately consult a doctor if the discharge becomes watery and clear. Most likely, the process of leakage of amniotic fluid is developing. Be careful, the amount of fluid may be so small that it can be confused with normal secretions or urine.
Pregnancy 21 weeks spotting
I'm 21 weeks pregnant, I'm 29, this is my first pregnancy. In the evening I noticed a small brownish discharge, which continued a little at night. At 10 weeks of pregnancy there was spotting, she was kept in storage and took utrozhestan. At week 18 I had an ultrasound, everything was fine, the doctor said I didn’t see anything wrong. A week later they did an ultrasound scan of the hot canal, everything was also fine. At week 19, my stomach began to harden, and the gynecologist prescribed Buscopan suppositories. I read about the contraindications and did not take them; later she recommended papaverine. I feel the tone quite often, but nothing hurts, I try to relax, it goes away after a while. I put papaverine on at night a couple of times for peace of mind.
Today was a busy day, I didn’t sleep much, and then I began to have brown discharge with cheesy inclusions. Tomorrow I will go to the doctor, but I want to ask in advance: is it worth doing an ultrasound now (3 weeks after the last one), if they are campaigning for a hospital, should I agree or is it better at home?
What is an “ultrasound circus of the hot channel?” Did you mean ultrasound, which measures the length of the cervix? Buscopan is NOT used in modern obstetrics; its effectiveness, much less its safety, has NOT been tested. Papaverite is also not used in obstetrics in any country in the world (except for post-Soviet ones). If you have placental abruption, then the use of antispasmodics can end in disaster - severe bleeding and loss of pregnancy. You are using papaverine not to help your child, but as a psychotropic drug that nourishes your psyche - nothing more. Don't play with fire!
Most likely, you do not have tone, but normal uterine contractions, which is typical for the second half of pregnancy. First, go for an ultrasound. It is necessary to carefully look where the placenta is located and especially its edge, whether there is placental abruption, what
Source
Difficulties in pregnancy
Premature birth
The survival rate of such babies is very low due to physical immaturity and underdevelopment of the body. This period is dangerous due to spontaneous abortion, i.e. miscarriage. The cause of the pathology can be damage to the membranes, infection of the fetus, placental insufficiency, genetic disorders, and inflammatory diseases.
Frozen pregnancy
It is one of the types of abortion, in which the child in the womb stops developing and growing, and then dies completely, and his expulsion from the uterus did not occur. This pathology is detrimental to the female body, since after the decomposition of the tissues of a deceased baby, peritonitis and generalized sepsis occur. Possible causes associated with this include: complications during development, previous abortions, and advanced age of women in labor.
Low water
The anomaly, which is accompanied by a decrease in the level of amniotic fluid, is usually diagnosed at 22-23 weeks of pregnancy. Such a “deficiency” negatively affects intrauterine development and can be fatal.
Polyhydramnios
The opposite pathological phenomenon caused by excess amniotic fluid. Possible reasons lie in disruptions in the functioning of the mother’s body (infectious processes, colds). Moderate polyhydramnios requires special attention from doctors; severe polyhydramnios requires urgent hospitalization.
Symptoms that indicate a threat
A woman should be extremely careful and attentive if she notices discharge in later stages of pregnancy, because this may indicate a threat of miscarriage. Especially if such discharge is abundant and comes with mucus. But even with scanty discharge, you need to be careful if, in addition to it, the woman feels a nagging pain that does not go away, but on the contrary, intensifies.
You need to urgently seek help and call an ambulance, or visit your doctor. Please note that discharge and pain may be accompanied by severe vomiting.
If you see a small amount of discharge, and there is no pain or nausea, then you still need to take action: go to the doctor, limit activity and reduce any stress as much as possible, no sports and bags of groceries. If you consult a specialist in time, then even if there is a threat of miscarriage, there is a chance to maintain the pregnancy and give birth to a healthy baby on time.
If the doctor has identified a threat of amniotic sac detachment, the pregnant woman is prescribed a special drug that contains a hormone such as progesterone. In this case, to maintain pregnancy, it is important to complete the full course of treatment and maintain bed rest.
Medical examination
Screening
Screening is a comprehensive examination that includes ultrasound and blood donation to identify pathologies in the baby.
The second ultrasound screening is carried out to assess the general condition of the fetus: the progress of development of internal organs, the thickness of the collar space, the presence and size of the nasal bone. In addition, the condition of the uterus, placenta, amniotic fluid, and umbilical cord of the pregnant woman is examined for abnormalities.
A blood test is also taken to evaluate B-hCG and plasma protein-A - PAPP-A.
The obtained research data is entered into a special program (PRISCA or ASTRAIA).
The doctor must take into account additional factors:
- height and weight of the woman in labor;
- gestational age;
- past illnesses;
- bad habits;
- heredity;
- the presence of IVF, miscarriages, abortions.
Visit to the gynecologist
At the 22nd obstetric week of pregnancy, a woman should regularly visit a gynecologist after a second ultrasound screening.
The doctor examines the abdomen, measures blood pressure and pulse, listens to the baby’s heartbeat and looks at the results of ultrasound screening. Thus, the general condition of mother and child is assessed.
The gynecologist issues a referral for blood and urine tests and blood sugar levels. The list of special studies for a young mother at this stage also includes:
- HCG (human chorionic gonadotropin) is the most important indicator of the presence and successful development of the fetus.
- Free estriol is the level of female hormones (estrogens) that are produced during pregnancy.
- AFP (alpha fetoprotein) is a specific protein that is produced by embryonic tissue.
In addition, the doctor individually prescribes the following research methods after identifying potential problems in the woman in labor:
- Dopplerography is a study of blood flow, fetal vessels, and uterine arteries. The doctor identifies the nature of blood flow, as well as the likelihood of oxygen starvation - intrauterine hypoxia.
- Cardiotocography is one way to find out the baby's heart rate. The results obtained are displayed on paper in the form of a diagram. If the doctor has concerns, the procedure is re-prescribed.
- Cardiointervalography is a rare research tool that is prescribed when a heart defect is suspected or in other controversial situations.
Norm or pathology
Under no circumstances should you give in to panic right away. It is important to understand that the body is now under the influence of a huge, as yet unfamiliar, load. Therefore it may be broken.
The imbalance most often occurs due to a lack of progesterone in the body.
. In this case, during pregnancy, light brown discharge is not pathological.
Another reason for the appearance of small brown mucous discharge during pregnancy, which does not pose a danger to either the expectant mother or her child, is the so-called “false”
.
Even after conception, the body of pregnant women “remembers” about the menstrual cycle and in the early stages, namely, in the first month of pregnancy, around the day when menstruation would have started, had there not been a successful conception, a woman may have light brown discharge, the so-called daub. Its shade can vary from yellowish to light brown.
In any case, if it is detected, consultation with a competent specialist is mandatory!
Recommendations
Try to follow our tips to help you adapt to the new state:
- Show sensitivity to your child. After all, it is at this stage of development that communication between mother and child begins with the help of pushes. The baby hears everything and reacts to the outside world.
- Maintain proper sleep patterns and take half-hour breaks after lunch. For proper rest, a pregnant woman should purchase a special pillow and a hard mattress that will help her fully relax.
- Choose comfortable shoes and clothes that do not restrict your stomach. Otherwise, it will lead to disruption of normal blood circulation.
- Healthy eating is the key to success for a young mother. Monitor your blood pressure and weight.
Nutrition
The expectant mother should adhere to a balanced diet, which will have a positive effect on the baby’s health:
- To strengthen bones and teeth, the child takes calcium, so it is necessary to eat foods rich in this microelement (for example, dairy products, fish, nuts, greens).
- To protect your baby from anemia, eat foods high in iron: parsley, dried fruits, apples, liver, seafood and legumes.
- Give preference to fresh vegetables and fruits.
- Alcohol, carbonated drinks, and black coffee are contraindicated for a pregnant woman in any quantity.
Physical activity
At 22 weeks of pregnancy, it is recommended to lead an active lifestyle: maintain a toned figure and train various muscle groups. Fitness has a positive effect on preparation for the upcoming birth.
List of permitted exercises for the expectant mother at this stage:
- swimming is the safest sport during pregnancy;
- exercises to strengthen the pelvic floor muscles;
- Pilates and yoga will help strengthen the tone of the whole body and relieve tension;
- Dynamic dance exercises are encouraged ;
- general physical activity in the form of dumbbells should be no more than 500 grams. or 1 kg.
Pay attention to vaginal Kegel exercises, which will help strengthen the muscles of the perineum and avoid tearing during childbirth.
Intimate life
Sex at 22 weeks of pregnancy is even recommended if there are no individual medical contraindications for the mother. The intimate proximity of the parents will not cause concern to the baby, since he is protected by amniotic fluid and the membrane.
A woman’s sexual desire and sensitivity receptors increase significantly during this period due to increased blood flow to the genitals.
Sexologists note that the percentage of receiving the body for the female sex increases several times.
Naturally, if pain occurs during sexual intercourse, then you should consult a gynecologist.
Causes of abdominal pain in women
Sometimes a pregnant woman experiences brown discharge during the period corresponding to the onset of her period. This is due to low levels of progesterone, which is also called the pregnancy hormone.
https://www.youtube.com/watch?v=9wprcyG66Ww
It turns out that the body does not notice pregnancy and continues to live according to its usual schedule. On the one hand, this phenomenon does not pose a serious threat to the fetus, but low levels of progesterone can be dangerous for pregnancy.
Despite the fact that for some women such discharge continues almost until childbirth, it is advisable to observe bed rest during these days or exercise a minimum of physical activity. Depending on the level of progesterone, treatment of the pregnant woman may continue in the hospital.
Often brown discharge is pathological in nature, you should be especially alarmed if the pad has to be changed every hour, and the bleeding is accompanied by pain. In this case, immediately call an ambulance or go to the hospital yourself.
Even minor discharge without odor or pain is a serious reason to consult a gynecologist - it’s better to be safe than to lose your child. Timely medicine increases the chances of maintaining pregnancy and re-conception.
Very rarely, a chromosomal malfunction occurs, as a result of which connective tissue covered with vesicles is formed instead of the placenta. This phenomenon is called “skid”; it can be hollow or partial.
With a partial pregnancy, there is a chance to save the pregnancy, because part of the placenta forms normally, but with a complete pregnancy, the fetus dies at an early stage of development, so it is important to carry out curettage in time to preserve the possibility of re-conception.
Symptoms of the pathology are brown discharge, dizziness, and abdominal pain.
Does brown discharge in the early stages mean an ectopic?
Although dark spots on panties in the first weeks are quite normal, a problem such as an ectopic pregnancy cannot be ruled out. Therefore, a woman who already knows about her situation must definitely visit a doctor and have an ultrasound done to rule out this diagnosis. After all, this is very dangerous for a woman’s life. Without timely measures, an ectopic can cause death.
After all, the fertilized egg is not attached inside the uterus, as it should be, but on the fallopian tube. As a result, the fetus enlarges and compresses the tubes, which leads to their rupture and internal bleeding. Note that the main symptom of an ectopic pregnancy is a fairly strong nagging pain below. In this case, you cannot hesitate, because this is extremely dangerous for a woman’s life and her reproductive function.
Brown discharge in the first period may be a sign of a pathology such as hydatidiform mole. At the moment, experts cannot establish the exact reasons for the development of this problem. But it is known for sure that hydatidiform mole affects the normal chromosome complement of the fetus, which leads to a number of abnormalities and problems in the future. If a complete hydatidiform mole develops, there is a high probability of fetal death in the early stages of pregnancy.
Therefore, when visiting a doctor, it is important to exclude such pathology for your own peace of mind. If such a problem is detected, the fetus must be removed. In very advanced and difficult cases, in order to save the mother’s life, the doctor removes the uterus. Therefore, if you see dark yellow or brown discharge during pregnancy, don’t wait, it’s better to make an appointment to avoid serious problems with your health. But most importantly, don’t be nervous, because, as you know, severe stress can cause a miscarriage, especially in the early stages.
A normal pregnancy does not cause the expectant mother much concern. However, today fewer and fewer women can boast of a high level of reproductive health, which leads to various problems during the gestational period. One of the symptoms of trouble is brown discharge during pregnancy.
Sometimes they can actually become a dangerous signal. We will talk about the reasons why brown discharge occurs and the threats associated with this phenomenon in this article. To do this, let's look at the questions asked on various forums for expectant mothers and try to answer them.
Pelvic inflammatory processes
Dark discharge at 12 weeks of pregnancy may occur due to an inflammatory process. It is worth noting that most often the pathology spreads to the reproductive organ. As a result, involuntary contractions occur. In some cases, this may pose a risk of miscarriage.
Pathology should always be treated individually. There is no one medicine that suits everyone. In most cases, the inflammatory process in the uterus is eliminated with the help of antimicrobial compounds, vaginal tampons, suppositories and immunomodulatory drugs. However, not all of the listed medications are approved for use by expectant mothers. Often the inflammatory process causes abortion.