Cardiac arrest is the equivalent of clinical death. As soon as the heart stops performing its pumping functions and pumping blood, changes in the body begin, called thanatogenesis or the onset of death. Fortunately, clinical death is reversible, and in a number of situations of sudden respiratory and cardiac arrest they can be restarted.
Actually, sudden cardiac arrest is precisely the cessation of its effective work. Since the myocardium is a community of many muscle fibers that must contract rhythmically and synchronously, their chaotic contraction, which will even be recorded on a cardiogram, can also refer to cardiac arrest.
Causes of cardiac arrest
- The cause of 90% of all clinical deaths is ventricular fibrillation. In this case, the same chaos of contractions of individual myofibrils will take place, but blood pumping will stop and the tissues will begin to experience oxygen starvation.
- The cause of 5% of cardiac arrests is complete cessation of heart contractions or asystole.
- Electromechanical dissociation is when the heart does not contract, but its electrical activity remains.
- Paroxysmal ventricular tachycardia, in which an attack of heartbeats with a frequency of more than 180 per minute is accompanied by the absence of a pulse in large vessels.
The following changes and diseases can lead to all of the above conditions:
Heart pathologies
- IHD (coronary heart disease) - angina pectoris, arrhythmias, acute oxygen starvation of the myocardium (ischemia) or its necrosis, for example, during myocardial infarction
- inflammation of the heart muscle (myocarditis)
- myocardiopathy
- heart valve damage
- pulmonary embolism
- cardiac tamponade, for example, compression by blood due to injury to the heart sac
- dissecting aortic aneurysm
- acute thrombosis of the coronary arteries
Other reasons
- drug overdose
- poisoning with chemicals (intoxication)
- overdose of drugs, alcohol
- obstruction of the respiratory tract (foreign body in the bronchi, mouth, trachea), acute respiratory failure
- accidents - electric shock (use of weapons for self-defense - stun guns), gunshots, knife wounds, falls, blows
- state of shock - pain shock, allergic, with bleeding
- acute oxygen starvation of the whole body due to suffocation or respiratory arrest
- dehydration, decrease in circulating blood volume
- sudden increase in blood calcium levels
- cooling
- drowning
Predisposing factors for cardiac pathologies
- smoking
- hereditary predisposition
- alcoholism
- age over 50 for men and over 60 for women
- heart overload (stress, intense physical activity, overeating, etc.).
Drugs that cause cardiac arrest
A number of medications can provoke cardiac catastrophe and cause clinical death. As a rule, these are cases of interaction or overdose of drugs:
- Anesthetics
- Antiarrhythmic drugs
- Psychotropic drugs
- Combinations: calcium antagonists and third class antiarrhythmics, calcium antagonists and beta blockers, you cannot combine some antihistamines and antifungals, etc.
Due to the fault of drugs, death occurs in approximately 2% of all cases, so it is strictly forbidden to take any drugs without indications. Any drug should be taken only as prescribed by a doctor in the indicated dosages, and you should also inform your doctor about the medications you are taking for the treatment of another disease (prescribed by another doctor), since the combination and overdose can lead to serious consequences (see also reasons pain in the heart area).
Signs of cardiac arrest
The appearance of the patient, as a rule, leaves no doubt that something is wrong. As a rule, the following manifestations of cessation of cardiac activity are observed:
- Lack of consciousness, which develops 10-20 seconds after the onset of an acute situation. In the first seconds, a person can still make simple movements. After 20-30 seconds, additional convulsions may develop.
- Paleness and bluishness of the skin, primarily the lips, tip of the nose, and earlobes.
- Rare breathing, which stops 2 minutes after cardiac arrest.
- Absence of pulse in large vessels of the neck and wrists.
- Absence of heartbeat in the area below the left nipple.
- The pupils dilate and stop responding to light - 2 minutes after stopping.
Thus, after cardiac arrest, clinical death occurs. Without resuscitation measures, it will develop into irreversible hypoxic changes in organs and tissues, called biological death.
- The brain lives for 6-10 minutes after cardiac arrest.
- As a casuistry, cases of preservation of the cerebral cortex after 20 minutes of clinical death when falling into very cold water are described.
- From the seventh minute, brain cells begin to progressively die.
And although resuscitation measures are supposed to be carried out for at least 20 minutes, the victim and his rescuers have only 5-6 minutes in reserve, guaranteeing the subsequent full life of the victim of cardiac arrest.
First aid for cardiac arrest
Given the high risks of death from sudden ventricular fibrillation, civilized countries equip public places with defibrillators that can be used by almost any citizen. The device comes with detailed instructions or voice guidance in several languages. Russia and the CIS countries are not spoiled by such excesses, so in the event of sudden cardiac death (suspected) you will have to act independently.
Increasingly, legislation limits even a doctor passing by someone who has fallen on the street in the ability to perform primary cardiopulmonary resuscitation. After all, now a doctor can do his work only during the hours allotted to him on the territory of his medical institution or subordinate territory and only in accordance with his specialization.
That is, an obstetrician-gynecologist resuscitating a person with sudden cardiac arrest on the street may receive very little due. Fortunately, such penalties do not apply to non-medics, so mutual aid still remains the victim’s main chance of salvation.
In order not to look indifferent or illiterate in a critical situation, it is worth remembering a simple algorithm of actions that can save the life of someone who has fallen or is lying on the street and preserve its quality.
To make it easier to remember the order of actions, let’s call them by their first letters and numbers: OP 112 SODA .
- O – assessing the danger
Approaching the person lying not too close, we ask loudly if he can hear us. People under the influence of alcohol or drugs usually mumble something. If possible, we pull the body off the roadway/passage, remove the electrical wire from the victim (if an electric shock has occurred), and free
- P – checking the reaction
From a standing position, preparing to jump away if something happens and quickly run away, we pinch the earlobe of the person lying and wait for a response. If there are no groans or curses, and the body is lifeless, move on to point 112.
- 112 - telephone call
This is a general emergency phone number that can be dialed from mobile phones in the Russian Federation, CIS countries and many European countries. Since there is no time to waste, someone else will take care of the phone, and it is you who must choose from the crowd, addressing the person personally so that he has no doubts about the assigned task.
- C - heart massage
Having placed the victim on a flat, hard surface, you need to begin chest compressions. Immediately forget everything you saw on this topic in films. Doing push-ups from the sternum with bent arms makes it impossible to get your heart going. Arms should be straight throughout resuscitation. The straight palm of the weaker hand will be placed across the lower third of the sternum. The stronger palm is placed perpendicularly on top of it. This is followed by five non-childish pressing movements with all the weight on outstretched arms. In this case, the chest should shift no less than five centimeters. You will have to work like in the gym, not paying attention to the crunching and grinding under your arms (the ribs will then heal, and the pleura will be sutured). 100 pushes should be made per minute.
- О – ensure airway patency
To do this, the person’s head is carefully tilted back a little so as not to damage the neck, with fingers wrapped in any scarf or napkin, dentures and foreign objects are quickly pulled out of the mouth, and the lower jaw is pushed forward. In principle, you can skip this point. The main thing is not to stop pumping your heart. Therefore, you can put someone else on this point.
- D - artificial respiration
For thirty pumping of the sternum, there are 2 breaths from mouth to mouth, previously covered with gauze or a handkerchief. These two breaths should not take more than 2 seconds, especially if one person is performing resuscitation.
- A is adies
Upon arrival at the scene of the ambulance or rescue services, you must prudently and promptly go home, unless the victim is your close friend or relative. This is insurance against unnecessary complications in your personal life.
First aid for a child
A child is not a small adult. This is a completely original organism, the approaches to which are different. Cardiopulmonary resuscitation remains especially relevant for children in the first three years of life. At the same time, you should not give in to panic and act as quickly as possible (after all, you only have five minutes left).
- The child is placed on the table, unswaddled or undressed, and the mouth is freed from foreign objects or impurities.
- Then, with the pads of the second and third fingers of the hand, located on the lower third of the sternum, pressure is applied at a frequency of 120 pushes per minute.
- The thrusts should be gentle, but intense (the sternum moves to the depth of a finger).
- After 15 compressions, take two breaths into the mouth and nose, covered with a napkin.
- In parallel with resuscitation, an ambulance is called.
First aid for cardiac arrest
Medical care depends on the cause of cardiac arrest. The most commonly used device is a defibrillator. The effectiveness of the manipulation decreases by about 7% every minute, so the defibrillator is relevant during the first fifteen minutes of the disaster.
The following algorithms for assistance in case of sudden cardiac arrest have been developed for ambulance teams.
- If clinical death occurs in the presence of the team, a precordial blow is applied. If cardiac activity is restored after it, then saline is injected intravenously, an ECG is taken, if the heart rhythm is normal, artificial ventilation is performed and the patient is taken to the hospital.
- If there is no heartbeat after a precordial stroke, the airway is restored using an airway, tracheal intubation, an Ambu bag, or mechanical ventilation. Then, closed cardiac massage and ventricular defibrillation are performed sequentially, and after the rhythm is restored, the patient is taken to the hospital.
- For ventricular tachycardia or ventricular fibrillation, I use defibrillator discharges of 200, 300 and 360 J sequentially or 120, 150 and 200 J with a biphasic defibrillator.
- If the rhythm is not restored, amiodarone and procainamide are used intravenously with a shock of 360 J after each drug administration. If success is achieved, the patient is hospitalized.
- In case of asystole confirmed by ECG, the patient is transferred to mechanical ventilation and atropine and epinephrine are administered. The ECG is re-recorded. Next, they look for a cause that can be eliminated (hypoglycemia, acidosis) and work with it. If the result is fibrillation, proceed to the algorithm for its elimination. If the rhythm stabilizes, hospitalization is required. If asystole persists, death is declared.
- For electromechanical dissociation - tracheal intubation. Venous access, search for a possible cause and its elimination. Epinephrine, atropine. In case of asystole as a result of measures, act according to the asystole algorithm. If the result is fibrillation, proceed to the algorithm for eliminating it.
Thus, if sudden cardiac arrest occurs, the first and main criterion that should be taken into account is time. The patient’s survival and the quality of his future life depend on the rapid start of assistance.
| Heart failure | |
| ICD-10 | I 46 46. |
| ICD-10-CM | I46 |
| ICD-9 | 427.5 427.5 |
| ICD-9-CM | 427.5 [1] [2] |
| OMIM | 115080 |
| DiseasesDB | 8695 |
| MeSH | D006323 |
Heart failure
- sudden and complete cessation of effective cardiac activity with the presence or absence of bioelectrical activity. The human heart is a unique organ consisting of a huge number of muscle fibers that work as a single mechanism. But sometimes the coordinated work of these muscles is disrupted, and cardiac arrest occurs.
Doctors' actions
After an ambulance arrives at the scene, doctors will resuscitate the patient using a defibrillator - a device that, using electrical impulses, resumes the work of the myocardium, injects saline solution intravenously, injects atropine and glucose.
If cardiac arrest occurs right when the ambulance arrives, an effective precordial beat method is used. It is delivered with a fist to the sternum. This method can instantly bring the patient out of a state of clinical death.
However, a precordial blow can only be performed by a trained specialist, otherwise there is a high risk of damage to the sternum.
If the airway is blocked, tracheal intubation is performed - a tube is inserted into the tracheal cavity to allow the victim to breathe.
Most often the patient can be saved. You can't panic, you need to act.
Reasons [edit | edit code ]
The causes of cardiac arrest vary, but the most common are:
Main factors [ edit | edit code ]
- Ventricular fibrillation - about 90% of all cases of cardiac arrest;
- Ventricular asystole - about 5% of all cases of cardiac arrest;
- Ventricular paroxysmal tachycardia with absence of pulse in large vessels;
- Electromechanical dissociation is electrical activity in the form of rhythmic QRS complexes without corresponding ventricular contractions.
Additional factors [edit | edit code ]
- ischemia;
- acute obstruction of blood circulation;
- myocarditis;
- cardiomyopathy;
- hypovolemia;
- hypoxia;
- metabolic changes;
- hypothermia;
- acute hypercalcemia.
Indirect factors [edit | edit code ]
- Smoking;
- Alcohol abuse;
- Excessive strain on the heart;
- Substance abuse;
- Age;
- Genetic.
Prevention
One of the common causes of cardiac arrest is alcohol addiction. The first preventative measure is to get rid of alcoholism. In addition to this you need:
- avoid physical overexertion;
- Avoid drinking drinks that contain alcohol;
- avoid emotional stress;
- stop smoking;
- do not eat foods high in fat;
- add fresh fruits and vegetables to your diet.
Several times a year you need to do an ECG procedure and take a general blood test. This will allow you to identify the problem at an early stage of development and promptly eliminate the occurrence of negative consequences. If the cardiologist has prescribed treatment, then follow it unquestioningly. If you experience any pain or suspicious symptoms in the chest area, you should contact a cardiologist.
Consequences[edit | edit code ]
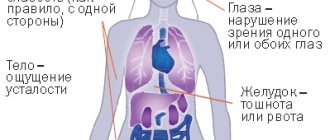
From the side of the central nervous system [edit | edit code ]
Loss of consciousness usually does not occur immediately, but after 10–20 seconds from the onset of ventricular fibrillation or asystole; for this reason, a person can still perform simple actions even after cardiac arrest.
From the respiratory system [edit | edit code ]
Rare agonal breathing stopping 2 minutes after loss of consciousness.
From the circulatory system [edit | edit code ]
Gradual cessation of blood circulation.
From the muscular system [edit | edit code ]
Tonic-clonic seizures may appear 15–30 seconds after loss of consciousness.
From the visual system [edit | edit code ]
Pupil dilation after 2 minutes with loss of reaction to light.
From the integumentary system [edit | edit code ]
A rapidly increasing change in skin color in the form of cyanosis or pallor.
General [ edit | edit code ]
After loss of consciousness and respiratory arrest, clinical death occurs and hypoxia develops in organs and tissues.
Agony
If a person has not lost consciousness, then he begins to experience agony. It includes symptoms of cardiac arrest such as disruption of the normal respiratory rhythm; Cheyne-Stokes breathing: convulsive and superficial. A person feels fear: he understands that death is approaching. Pain sensitivity is gradually lost.
The man's voice is hoarse. You may foam at the mouth. Breathing is also difficult due to the fact that the lungs swell during clinical death. Mucus accumulates in the lungs, and since the muscles of the chest are weakened, it is not removed from the lungs.
If after a couple of minutes the heart does not begin to work again, then breathing stops. The complexion becomes gray, thick sweat appears on the skin, and the face does not express any emotions. However, the reaction of the pupils to light remains. Convulsions may continue for half a minute, which is one of the signs of cardiac arrest.
Medical assistance [edit | edit code ]
- Indirect cardiac massage and emergency defibrillation. Its use without preliminary ECG control is justified by the fact that in more than 90% of cases the cause of cardiac arrest is ventricular fibrillation:
- adults
sequentially: 4.5-5.5-7.5 kV (200, 300 or 360 J); - children:
provided there is good contact with the surface of the chest, electrodes of the largest size are used (not only for children). First, defibrillation is carried out with a discharge of 2 J/kg, then it is increased to 4 J/kg.
- Mechanical ventilation (Ambu bag, mechanical breathing);
- 100% oxygen by mask or endotracheal tube;
- Central venous catheterization;
- Emergency drug therapy:
Preparations:
lidocaine, atropine and epinephrine - can be administered through an endotracheal tube with 10 ml of 0.9% sodium chloride solution or sterile water, or intravenously, it is better to inject into a central venous catheter, epinephrine 1 ml = 1 mg (at a dilution of 1:10,000 ) 0.1 ml = 0.1 mg (at a dilution of 1:1000).
Sequence of actions [edit | edit code ]
In case of paroxysmal ventricular tachycardia with absence of pulse in the central arteries and ventricular fibrillation, measures should be carried out in the following sequence:
- Defibrillation up to three times in succession 4.5-5.5-7.5 kV (200, 300 or 360 J, respectively);
- Check for electrical activity on the cardioscope;
- After each injection of the drug, indirect cardiac massage is performed for 30-60 s and defibrillation is repeated with a discharge of 7-7.5 kV (360 J);
- It is necessary to monitor the electrical activity of the myocardium and pulse after each subsequent event;
- Epinephrine - 1 mg IV bolus; if there is no effect, it should be re-administered every 3-5 minutes. Repeated epinephrine can be administered in medium (2-5 mg) or high (0.1 mg/kg) doses;
- Lidocaine - 1.5 mg/kg (bolus from 80 to 120 mg) IV, then IV drip over 5 minutes to a total dose of 3 mg/kg;
- Bretylium tosylate - 5 mg/kg IV in a bolus, then IV drip over 5 minutes to a total dose of 10 mg/kg;
- Magnesium sulfate - 1-2 mg IV for suspected tachycardia of the “pirouette” type, refractory ventricular paroxysmal tachycardia or fibrillation;
- Procainamide - 30 mg/min IV for refractory ventricular fibrillation or tachycardia (maximum dose - 17 mg/kg);
- Sodium bicarbonate - 1 mEq/kg only in case of previous metabolic acidosis, overdose of certain drugs (for example, TAD);
- Atropine - 1 mg IV bolus every 3-5 minutes to a total dose of 0.04 mg/kg. Can be administered every 1-2 minutes;
- In the absence of a pulse, but the presence of electrical activity (electromechanical dissociation, idioventricular rhythms, ventricular escape rhythms, bradysystolic rhythms, idioventricular rhythms after fibrillation);
- The presence of myocardial kinesis during echocardiography;
- Assessment of blood flow using Doppler ultrasound (if possible);
- Each subsequent stage is carried out if the previous one is ineffective;
- If the above measures are unsuccessful within 45 minutes, a decision should be made to stop resuscitation measures.
Further life after cardiac arrest [edit | edit code ]
Most people who experience cardiac arrest are delirious or lying as if dead. Treatment takes place in intensive care units. Patients survive if the heart can be started within 5-6 minutes after stopping. At the end of the resuscitation period, constant monitoring of the patient's condition is necessary. Cardiac activity and other functions may be impaired, and the patient often requires prolonged cardiac resuscitation. The patient is given an x-ray because the chest may have been damaged during cardiac arrest. In addition, biochemical tests are prescribed, diuresis is monitored, and other tests are carried out that can detect the development of dangerous complications. In case of prolonged heart failure, nootropic support is prescribed, which is necessary for the full restoration of the brain.
Cardiac arrest in the first few minutes leads to a state of clinical death. After a certain time, biological death occurs. If in the first case a person has minimal chances of survival, then the second option involves the development of disorders incompatible with life.
Which population groups are most likely to experience cardiac arrest?
Smokers and alcoholics are more likely to experience clinical death than people leading a healthy lifestyle. If a person’s mother, father or other relatives suffered from cardiac arrest, then the likelihood of clinical death increases.
The older a person is, the greater the likelihood of cardiac muscle failure - this is due to wear and tear of the entire body, including the myocardium. Stressful conditions, overeating, excessive physical stress on the body are important factors that should also be avoided.
Causes and risk factors
Emergency measures must be taken within the first seven minutes; it is almost impossible to survive after this period if the heart has stopped.
In extreme situations, survivors will remain disabled or fall into a coma. This happens because brain cells quickly collapse in the absence of oxygen, and behind them, other vital organs cease to function normally. First aid most often has to be provided to people who are far from medicine. But, unfortunately, they are rarely capable of self-control and do not always have sufficient knowledge in this area. Cardiac arrest is diagnosed when the organ stops pumping blood without making contractile movements. Most often, the myocardium ceases to function during diastole. Blood no longer circulates in the organs, they are left without oxygen and nutrients, all vital processes in them also stop, and irreversible death of cells and tissues begins.
Such a condition cannot arise on its own. There are reasons for everything. They may be associated with pathologies of the circulatory system and its main organ. This is the most common explanation for most cases of sudden death. There are other conditions that can lead to cardiac arrest and death.
Types of cardiac arrest:
- Quite rarely occur: asystoles (bioelectric activity and heart contractions are completely absent), electromechanical dissociative states (electrical impulses are generated, but do not cause contractile activity in the ventricles), paroxysms of ventricular tachycardia (frequent contractions of the chambers are present, but the pulse is not audible).
- The vast majority of cardiac arrests are associated with atrial fibrillation (individual groups of muscle cells of the ventricles contract in a chaotic manner, but the function of pumping blood is not performed).
Cardiac pathologies as the main cause of heart failure:
- Acute myocardial failure.
- Acute coronary syndrome or manifestation of coronary heart disease (associated with thrombosis, atherosclerosis, arterial stenosis)
- Extensive myocardial infarction.
- Heart defects associated with abnormalities of the valve apparatus and coronary vessels.
- Cardiomyopathy.
- Pulmonary embolism.
- Ruptured aortic aneurysm.
- Severe inflammatory process in the myocardium.
- Development of cardiogenic shock.
- Cardiac tamponade developing due to hydropericardium or hemopericardium.
- Brugada syndrome (a genetic metabolic disease that causes sudden attacks of ventricular tachycardia). This pathology is a common cause of cardiac arrest in young people (half of all incidents).
- Hypertensive crisis.
Chronic or acute conditions associated with damage to internal organs and the brain can also cause cardiac arrest:
- Brain disorders (hemorrhage and tissue necrosis).
- Kidney and liver dysfunction.
- Oncological diseases.
- Infections (eg meningitis).
- A severe form of diabetes mellitus that can lead to diabetic coma.
- Complications of pulmonary diseases (bronchial asthma attack).
Causes of sudden cardiac arrest not directly related to diseases:
- Significant blood loss (more than half the normal volume).
- Different types of shock (anaphylactic, traumatic, bacterial, burn, pain, dehydration).
- Toxic changes associated with an overdose or incorrect combination of certain dangerous substances (alcohol, drugs, certain medications taken without contraindications).
- Various life-threatening injuries (electrical trauma, closed or open wounds, consequences of an accident).
- Anesthesia during surgery.
- Critical exposure to low or high temperatures.
- Choking (intentional or due to negligence, when a foreign object enters the respiratory tract).
- Getting water into the lungs.
- Development of acute hypercalcemia.
Factors that increase the risk of sudden cardiac death:
- old age;
- bad habits (including regular overeating);
- severe emotional shock;
- physical overexertion (especially common in professional athletes);
- obesity;
- high cholesterol or blood sugar;
- hereditary factor.
Harbingers
It is extremely important to see threatening signs - harbingers of coronary death - while the patient is still alive. Timely treatment can save a person. Despite the fact that patients feel fine, subsequent questioning of relatives often reveals dangerous symptoms.
There is a high probability of death with frequent, polytopic, paired and group ventricular extrasystoles, especially in combination with signs of myocardial ischemia on the ECG. This can be detected by daily ECG monitoring.
When diagnosing such extrasystole, immediate antiarrhythmic treatment is required.
A sign that the patient himself can note is a sudden decrease in exercise tolerance. For example, a week ago he could climb to the 5th floor, but today he cannot walk even 100 meters. These phenomena are caused by silent ischemia. When they appear, it is necessary to call an ambulance, because a sharp decrease in exercise tolerance is interpreted as unstable angina and requires treatment in a hospital.
One of the frequent harbingers of coronary death is episodes of loss of consciousness. They occur during paroxysms of ventricular tachycardia, which is very difficult to register on a regular ECG. Other dangerous causes of fainting are unrecognized complete A-V block, sick sinus syndrome, and long QT syndrome. Timely 24-hour ECG monitoring will help diagnose these conditions and carry out treatment, for example, implantation of a pacemaker.
The risk of sudden death is higher in people who have similar cases in their family, especially younger relatives.
In most patients, retrospectively, within a few days or even weeks, it is possible to identify the symptoms that preceded sudden death:
- sudden weakness;
- unexpected chest pain;
- deterioration in health for an unknown reason;
- decreased emotional background, anxiety;
- episodes of pallor, palpitations, rapid breathing.
If these symptoms appear, it is important to consult a doctor in time, undergo daily ECG monitoring and other tests, and begin intensive treatment.
To learn about the causes of sudden coronary death and what methods will help avoid a fatal complication, watch this video:
Symptoms of cardiac arrest
Stopping the work of the heart muscle is accompanied by the following symptoms:
- Sudden fainting with falling and loss of consciousness. Develops in 10-20 seconds.
- Manifestation of convulsive syndrome after 20-30 seconds.
- Heartbeat cannot be heard.
- The pulse cannot be felt.
- There is no breathing (no movement of the chest). Or it becomes rare, convulsive, with wheezing.
- Changes on the cardiogram.
Cardiac arrest can also be determined by a person’s appearance:
- The skin turns pale, limbs, ears, nose, mouth turn blue.
- The pupils are wide and do not shrink when exposed to light.
- The man lies motionless, does not respond to shouts or slaps on the cheeks.
- An expression of fear on the face.
- Reflexive pressing of the hand to the heart.
- The body twitches unnaturally.
Other development mechanisms
Some scientists insist on identifying another form of cardiac arrest - electromechanical dissociation. This term stands for the absence of mechanical activity of the heart in the presence of electrical contractions.
There is an ECG on the monitor, but there is no blood circulation. Myocardial contractions continue, but the activity is insufficient to supply the vessels with blood.
With electromechanical dissociation, the pulse is not palpable and there is no blood pressure.
The ECG device records:
- Correct contractions with low frequency;
- Idioventricular ventricular rhythm is the intrinsic rhythm of the ventricles;
- Loss of sinus and atrioventricular node activity.
This condition is caused by weak impulse activity in the heart.
In the 70s of the last century, the term “obstructive sleep apnea syndrome” appeared. Cardiac arrest occurs at night during sleep. The condition is accompanied by temporary cessation of breathing. This pathology is called nocturnal bradycardia. A blood test reveals a lack of oxygen in the plasma.
According to statistics, heart function is disrupted during sleep for the following reasons.
- Stopping the rhythm and its disturbances – 49% of cases.
- Impaired conduction of electrical impulses from the atria to the ventricles – 27%.
- Atrial fibrillation - frequent and chaotic contractions of the atria - in 19%.
- Combinations of several types of bradyarrhythmia (conduction disturbances in the heart muscle) – in 5%.
Obstructive sleep apnea syndrome is diagnosed using a special device. When using the device, patients note that the heart stopped for a few seconds: from 3 to 13. During the waking period, patients with this syndrome do not experience fainting or respiratory arrest.
What causes cardiac arrest during sleep?
A person's breathing reflex is disrupted. The respiratory organs transmit impulses to the heart muscles through the vagus nerve. This causes the cessation of cardiac activity.
ECG study
Sudden infant death syndrome
Sometimes isolated cases of death of healthy infants at night in their sleep, for no apparent reason, at the age of 2 to 5 months are recorded. Cardiac arrest in a newborn is explained by the following reasons:
- insufficient physiological maturation of the newborn’s cardiovascular system;
- the birth of a child from multiple pregnancy;
- hypoxia suffered inside the womb is one of the common causes of sudden cardiac arrest in the fetus;
- oxygen deficiency during childbirth;
- early birth occurred, the baby was premature;
- infectious damage to an unborn embryo or baby in the first weeks of life;
- abnormal development of the fetus in the womb;
- pregnancy occurring with pathologies.
There are a number of factors that contribute to cardiac arrest in early childhood:
- smoky, stale, hot air in the room of a sleeping child;
- the baby sleeps on his stomach;
- the bed is very soft, the child falls into it, he is covered with a fluffy blanket, sleeps on a pillow;
- a young inexperienced mother puts her child to sleep next to her, she may accidentally crush him in his sleep;
- parents drink alcohol and cannot adequately monitor their infant.
What can cause the heart to suddenly stop beating?
Typically, myocardial arrest occurs due to pathologies of the cardiovascular system (so-called cardiogenic causes). But often the triggering factor is other acute or chronic diseases, as well as injuries and accidents (non-cardiogenic).
| Cardiogenic causes | Non-cardiogenic causes |
| Myocardial infarction | Stroke |
| Acute and chronic heart failure | Carrying out heart surgery (stenting, valve replacement) |
| Defects of heart structures | Oncological diseases |
| Cardiomyopathies | Infectious pathologies |
| Myocarditis | Complications of bronchopulmonary diseases (respiratory failure, respiratory distress syndrome) |
| Hypertensive crisis | Endocrine disorders (diabetic, hypothyroid, thyrotoxic coma) |
| Heart rhythm disturbances | Acute hypercalcemia and/or hypokalemia |
| Cardiogenic shock | Sepsis |
| Pulmonary embolism | Pancreatic shock |
| Aortic aneurysm | Acute renal and/or liver failure |
| Cardiac tamponade |
Isolated episodes that can cause cardiac arrest include:
- Anaphylactic shock (due to anesthesia, local anesthesia, taking antibiotics and other drugs, insect bites);
- Poisoning (including alcohol and drugs);
- Massive burns;
- Hypo- and hyperthermia;
- Electrical injuries;
- Suffocation.
Causes in children and young people
Most often, older people die from heart failure. However, there are reasons that can cause it in children or young people. They are usually caused by the above conditions associated with trauma and other damage, as well as serious arrhythmias. But there are also some specific pathologies.
So, before the age of one year, sudden infant death syndrome may occur. In such a case, a disturbance in the heartbeat and breathing develops against the background of absolute external well-being, most often at night and during sleep.
Risk factors for sudden infant death may include:
- sleeping on a bed that is too soft in an unventilated room on the stomach - in this case, the baby may simply suffocate;
- multiple pregnancy;
- prematurity;
- delivery by caesarean section;
- bad habits of the mother during pregnancy.
During pregnancy, for one reason or another, fetal cardiac arrest may occur. Most often this happens due to undiagnosed intrauterine developmental disorders of the embryo or genetic pathologies.
Athletes often experience sudden death due to Commotio Cortis syndrome. It occurs as a result of a sharp and strong blow to the heart at the time of diastole. Such an action can cause the reflex development of a dangerous arrhythmia, for example, ventricular fibrillation.
The following sports are considered dangerous in this regard:
- martial arts;
- baseball;
- American football;
- hockey.
Diagnostics
A person lying unconscious can find himself in this position for various reasons. They need to be installed as quickly as possible. Diagnosis of cardiac arrest (as opposed to transient fainting) involves the following:
- Call the fallen person, shake him, hit him in the face not too painfully, sprinkle him with cold water. Try to bring the victim to his senses in every possible way. If this does not help, cardiac arrest may be suspected.
- Check for pulsation in the carotid artery in the neck. Determine whether the person is breathing. To do this, it is often advised to bring a mirror to your mouth (it will fog up if there is breathing), observe the movement of the chest, listen to the heartbeat by leaning your ear to your chest. Another way is to put your cheek to the victim’s lips; you can feel how it becomes warm and moist if the air continues to circulate in the lungs.
- Direct a beam of light into the pupils; the normal reaction will be their narrowing.
- Assess the appearance of the skin. Note cyanosis and excessive pallor.
- If possible, take ECG readings.
Providing first emergency first aid
Sudden cardiac arrest is a critical condition that requires immediate action. This can happen anywhere, and most often clinical death overtakes a person outside a medical facility. Therefore, first aid should be provided by people nearby. You definitely need to call an ambulance, but you shouldn’t count on it too much. After all, the victim has only 7 minutes to return to life. Not every ambulance can rush to the scene of the incident so quickly.
The sooner resuscitation measures are started, the greater the chance of saving a person from sudden death. Late timing of such actions significantly reduces these chances. Every minute without oxygen, irreversible processes occur in the body, destroying, first of all, brain tissue. Serious damage also occurs in other vital organs. If a person can be revived after 7-10 minutes of clinical death, he will most likely remain disabled from subsequent complications.
How you can help in case of cardiac arrest before the doctor arrives:
- Perform artificial respiration. To do this, lay the person on his back; the surface should be as flat and hard as possible. The head is raised upward, the lower jaw is extended. Check the airways for vomit or other foreign objects, and clear the mouth and throat if necessary. Prevent tongue sinking. Next, draw in as much air as possible into the lungs and exhale it into the victim’s mouth (after covering it with a handkerchief to avoid infection). The nasal openings should be clamped with your hand. Two such injections are performed, then an indirect massage of the heart muscle is performed.
- Perform a heart massage. Place one hand on top of the other, extend your arms, place them on your chest (lower third of the chest). Press with force, sharply, five times in a row, if there is another assistant who then performs one artificial breath. Otherwise, do 15 presses and two blows, following each other. The shock speed should be approximately 100 per minute.
Resuscitation must be carried out until signs of life appear: spontaneous heartbeats or breathing. Press hard enough, but try not to break the victim’s ribs (which often happens in such situations). However, after half an hour has passed since the heart stopped, any manipulations to bring a person out of a state of clinical death are considered inappropriate. At this moment biological death is declared.
Reanimation
When performing chest compressions, it should be taken into account that the arms should be kept straight and not bent (this is how first aid is shown in most films, TV series, etc.).
It is necessary to place your weak hand (left for right-handers or right for left-handers) a few centimeters above the xiphoid process, and place your stronger hand on it. After this, you need to make a few pushes down into the center of the chest.
Try to push as often as possible and do not be afraid to damage the bones: breaking them is quite difficult, but incorrect indirect massage, which is the only method of salvation, can lead to final death.
Only two people can provide ideal first aid in case of cardiac arrest: one does chest compressions, and the other does artificial respiration. But if you have to provide first aid alone, then keep in mind that for every 30 pushes there should be two inhalations and exhalations.
If you are helping a stranger, be sure to use gauze or a handkerchief to avoid the risk of contracting infectious diseases.
Complications of cardiac arrest
According to the theory of pathological anatomy, after approximately the seventh minute of cardiac arrest, the brain begins to die. A time period of up to 3-4 minutes from the moment of clinical death is considered optimal for saving a life without critical consequences for mental and physical health. People rescued at the seventh minute or later develop complications of varying severity.
Brief cardiac arrest is characterized by mild to moderate disturbances in brain activity:
- Regular pain in the head that persists for a long time.
- Loss of visual function, up to blindness.
- Problems with memory, hearing, concentration.
- Convulsive seizures.
- A disorder of the psyche and consciousness, manifested by auditory and visual hallucinations
Severe brain damage includes:
- coma;
- complete incapacity for mental activity, loss of all brain functions, inability to care for oneself;
- paralysis of the entire body or individual parts of it.
Forecast
In general, the prognosis for cardiac arrest cannot be considered positive. Only a third of the victims can be saved. Moreover, only a tenth of survivors can count on full or partial restoration of the functions of vital organs.
The most favorable outcome is considered to be if the patient recovers from the state of clinical death in the first 3 minutes. The survival rate after a 10-minute cardiac arrest is one hundredth of all incidents.
Complete return of all brain functions is observed in 3-5% of people, about 15% of survivors suffer from moderate damage to brain tissue. The remaining percentage does not come out of a coma or becomes completely disabled for the rest of their lives.
People who returned “from the other world” in full consciousness and without any special health problems are considered “lucky”. Cardiac arrest can practically equate to biological death. The chances of saving life are too low. However, as long as there is hope to save a person, we must fight for him. Everyone needs to know how to do this correctly. Perhaps the skills of artificial respiration and indirect myocardial massage will be useful in helping your loved ones. To prevent such conditions, you should protect your heart from overload, promptly treat cardiac diseases, be careful and not get into life-threatening situations.
Signs of an imminent heart attack
In Denmark, studies have been conducted for a long time regarding sudden cardiac arrest. As a result of their implementation, they succeeded in the fact that a deceased person could remain alive if he reported a deterioration in health in time. Danish experts included the following signs of an imminent offensive:
- shortness of breath;
- cardiopalmus;
- darkening of the eyes;
- slight dizziness;
- feeling of heaviness in the upper and lower extremities;
- cardiac arrest is painful, and discomfort in the chest area may appear 4 days before the attack;
- pre-fainting state.
At these moments, a person is able to independently ask passers-by for help or call emergency help; only after these symptoms does he experience cardiac arrest and faint. Research has proven that after successful resuscitation measures, in 34% of cases the muscular organ stops working again within 1 hour. Therefore, the patient should be under the supervision of a cardiologist.