Dear readers, situations sometimes happen in life, such as anaphylactic shock. Delay and ignorance of the principles of emergency assistance can lead to the most tragic consequences. Of course, medical workers know this like twice two. But if there are no doctors nearby, and the ambulance is still on the way, what should you do if a person dies before your eyes? What is emergency care for anaphylactic shock? The most important thing is not to get confused and correctly follow the instructions that I will talk about here.
Anaphylactic shock is...
Anaphylactic shock is a type of allergic reaction that occurs instantly and immediately puts a person in a serious condition. It can be fatal.
It develops after the allergen re-enters the body, which entails spasm of muscles and bronchi, decreased blood pressure, and dysfunction of the central nervous system.
Substances that can provoke anaphylactic shock are divided into 4 groups:
- food products (wheat, peanuts, chocolate, milk, citrus fruits, soybeans, corn, eggs, dyes and additives);
- plant origin (poplar fluff, flowers with a pungent odor);
- poison (after the bite of a snake, bees, wasps);
- medications (anti-inflammatory drugs, analgesics, antibiotics, muscle relaxants, radiocontrast agents, blood substitutes, immune serums, penicillin group).
For example , a person is allergic to oranges, but he doesn’t know about it yet. Trying citrus for the first time, and there is no reaction. When he buys and eats for the second time, the antibodies in his blood begin to fight the antigens (allergen).
Due to this reaction, active substances are released : serotonin (what is it?), histamine, bradykinin. They increase the permeability of vascular walls and cause muscle spasms.
Blood accumulates on the periphery of the arms and legs, which is why blood pressure drops. Liquid, nutrients and oxygen do not enter the cells of organs, including the brain. This provokes loss of consciousness.
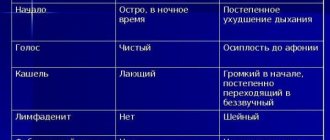
How to determine the severity of anaphylactic shock?
| Criterion | 1st degree | 2nd degree | 3rd degree | 4th degree |
| Arterial pressure | Below the norm by 30-40 mmHg (Normal 110-120/ 70-90 mmHg) | 90-60/40 mmHg and below | Systolic 60-40 mmHg, diastolic may not be determined. | Not determined |
| Consciousness | Conscious, restless, excited, fear of death. | Stupefaction, possible loss of consciousness | Possible loss of consciousness | Immediate loss of consciousness |
| Effect of antishock therapy | Good | Good | Treatment is ineffective | Virtually absent |
Main symptoms of anaphylactic shock
When it occurs, symptoms are divided into 2 categories, depending on the stage.
The first stage is characterized by:
- temperature increase;
- burning;
- itching;
- the skin turns red or pale;
- arms, legs, face become numb and tingling;
- lips and tongue become swollen;
- running from the eyes and nose;
- sneezing;
- it is difficult to breathe, you can hear a whistle;
- feeling of a lump in the throat;
- abdominal pain, nausea.
Already having such symptoms of precursors, it is worth immediately providing assistance to the person .
If this does not happen, the second stage of anaphylactic shock occurs :
- severe weakness;
- dizziness;
- loss of consciousness;
- pallor;
- dyspnea;
- cold sweat;
- ringing and noise in the ears;
- feeling of fear of death;
- convulsions.
Depending on which system of the body the allergen affects more, the symptoms are classified into :
- Respiratory – suffocation due to swelling of the mucous membrane.
- Cardiac – acute myocardium and infarction may occur.
- Cerebral – convulsions, nausea, headache, possible involuntary urination.
- Skin - itching, Quincke's edema, urticaria.
Help with allergies
Allergy is a chameleon disease. Either it will appear on the skin as a plaque or rash, or it will begin its march with a banal itch. Seasonal runny nose? Also about her. And these are just minor pranks. And sometimes an allergy turns into a real evil monster: if it wants, it will start to choke, but if it wants, it will turn off the light of consciousness. How to resist this scourge?
It’s not always possible to pacify such a chameleon; sometimes we don’t even have time to administer drugs to save a person, death occurs in a matter of minutes...
Anaphylaxis in my practice
More than ten years ago, a man with a duodenal ulcer was treated in the therapeutic department of our hospital. On the first day they administered quamatel - there seemed to be no reaction. And on the second day the patient died, literally, as they say, on the needle. And no amount of resuscitation could save him.
And about five years ago, a guy came on my shift with a blunt abdominal injury. An ultrasound revealed that he had a ruptured spleen and fluid in his abdomen, a condition that required immediate surgery. With some technical difficulties, the spleen was removed; blood loss amounted to more than a liter. We decided to give him three doses of fresh frozen plasma.
The operation was successful, the surgeons took off their gowns and left... All that remained were the operating nurses, me and the anesthetist. They called a gurney and were already preparing to transfer the patient to the intensive care unit. They shifted the guy who had not yet woken up, and I was about to disconnect him from the ventilator and connect him to a breathing bag, when I suddenly noticed that his skin had become an unusually bluish color. They measured my blood pressure and it dropped to 80/40. We tried it again - 60/0. Pulse 48 per minute.
The patient was dying. From what? There is no blood through the drainage from the abdominal cavity, his breathing is not affected - he is on a ventilator. What's happened? — thoughts rushed through my head like bullets. The sisters, hardly hiding their horror, waited for decisions from me.
Lifting the sheet, I saw red plaques on my stomach. — Adrenaline cube quickly! Blood pressure is 40/0, pulse has become arrhythmic. Solutions flowed into the veins into two rivers. - Another cube of adrenaline! — at that moment my own adrenaline was going through the roof, the guy was not even twenty years old. - Prednisolone, all that we have, quickly into a vein!
Then a total of twenty ampoules of prednisolone were administered! Five cubes of adrenaline!
The pressure was finally stabilized at one hundred and forty, provided that it was maintained by constant administration of adrenaline. The guy's body was completely covered with red plaques.
The next day the patient was weaned off the respirator. Everything ended well, he survived without any negative consequences.
Why did this happen? He had no previous symptoms of allergies. We sinned on plasma, but who knows, because during the operation anesthetics, hemostatic agents, and other drugs were administered. Very often the allergen is never detected, even in allergy tests.
Who is guilty?
So what is an allergy? This is a complex of symptoms (itching, redness, swelling, loss of consciousness and many others) caused by the pathologically high sensitivity of the body's immune system, previously sensitized by a foreign substance (allergen).
Sometimes an allergy to the body's own tissues occurs, which causes severe autoimmune diseases (glomerulonephritis, rheumatism, etc.).
It is interesting that allergies themselves appeared and are developing in parallel with our progress, the development of the chemical industry, and the improvement of the quality of life. The immune system began to malfunction and incorrectly determine what is good and what is bad.
For the development of a true allergy, it is necessary that the human body encounters and becomes familiar with a certain substance (later the allergen). The first meeting will be harmless, but in response, the body will produce antibodies, and at the next contact, these antibodies will rush to the place of contact with the allergen (antigen) and form an antigen-antibody union. There will be a release of aggressive substances (histamine, cytokines, etc.) from special cells. This will manifest itself as a runny nose, lacrimation, itching, redness, etc.
Moreover, allergens often have not only a local effect, but also affect the body as a whole. That's when trouble can happen - Quincke's edema (swelling of the upper half of the body) with suffocation (as a result of swelling of the oropharyngeal mucosa), anaphylactic shock, a sharp drop in blood pressure and death.
I won’t go into the details of the pathogenesis, but there is also an anaphylactoid reaction. It is very similar to the classical reaction, but in pathogenesis there is a stage when antibodies are formed in response to the initial meeting of the allergen and the person. Here, immediately in response to contact, there is a release of biological substances that trigger the body’s reaction, or excess histamine comes from food (honey, fish), which is manifested by a certain reaction of the body. But clinically everything happens identically, and the treatment is the same. Therefore, we, clinicians, do not bother with such subtleties.
Allergies are so diverse that a separate specialist, an allergist, was appointed to treat this condition. And, of course, it is impossible to describe all the diversity of this disease in one article. People who are familiar with this scourge firsthand, I think, even without me, can already imagine what and how. Therefore, with your permission, I will omit such common and non-threatening symptoms as hay fever and lacrimation. And I will continue to write for those who have not yet properly understood allergies, but with the obligatory amendment that if necessary, you will immediately contact a specialist to determine the allergen and undergo a specialized course of treatment.
...and what to do?
How to independently understand that you have an allergy?
After all, sometimes there is no specialist nearby, and we go to the doctor when the whole body is already covered with plaques or it has become completely bad.
Most often, allergies begin to manifest themselves with minor symptoms, and if you start treatment at this stage, then it may not come to an emergency. But it can get there - because, starting with ordinary diathesis, allergies sometimes develop into more formidable forms: bronchial asthma and even anaphylactic shock.
But again, I repeat - definitely see an allergist! Only he will help you so that in the future you will not suffer from this misfortune. In particular, the allergist will explain what to do with the diet, because life when you can’t eat either spicy or smoked foods, and you can only eat porridge, is not life!
How does an allergy begin? First of all - with itching. They scratched there, they scratched here, more often under the armpits, in the groin. Itching, of course, is not a 100% indicator. It can also itch from unwashed skin, scabies, liver disease, and a lot of other things. For example, if it itches often and in one place, look at the place where you scratched, maybe you will find the entry and exit points of the scabies mite. But if you find a rash or plaques and notice that under certain circumstances they disappear (appear at home, disappear at work), then it is most likely an allergy to something. Take an antihistamine (for example, Zyrtec), if the itching decreases and the plaque disappears, it means you definitely have an allergy.
Needs treatment. How? First of all, it is necessary to eliminate the allergen.
And if it is not known, then you will have to go on a strict diet (the diet is posted on many sites, so I will not repeat it). In general, during an exacerbation of allergies, the body reacts to many possible allergens. Therefore, a diet is mandatory!
If the allergen is plant pollen, then windows should not be opened during flowering. Ventilate the apartment after rain. After washing, you cannot hang things outside. The cleanliness of the house should be perfect.
Allergies to medications usually manifest themselves immediately and quite violently, so the new drug, a possible allergen, should be immediately discontinued.
To relieve symptoms, take an antihistamine
(it is histamines that are released from mast cells in response to the introduction of an allergen), the second or third generation is better. These drugs are convenient, taken once a day and do not have a hypnotic effect.
You need to drink a lot of water, but always bottled, purified water.
(You can’t use it from the tap - there are too many nasty chemicals, which can also cause a reaction.) Histamine and other biologically active substances responsible for allergies will be eliminated through the kidneys in the urine. This way you will be doing a home detox. Sorbents are also good in this case (activated carbon).
At night, you can give an injection of suprastin (allergists recommend suprastin, not chloropyramine, but if suprastin is not available, then chloropyramine will do).
If after a day or two nothing helps, be sure to go to the doctor, don’t risk it! Anaphylactic shock is no joke!
Allergy sufferers should have adrenaline along with a syringe in their first aid kit. At the moment, adrenaline is the most powerful and effective remedy for anaphylactic shock, combining antihistamine, anti-shock (stimulating the work of the heart and blood vessels) effects, it is the first-line drug for this life-threatening condition. However, if used rashly, it can lead to hypertensive crisis or arrhythmia. It is administered during anaphylactic shock, when the victim experiences dizziness, loss of consciousness, and a sharp drop in blood pressure. Subcutaneous routes of administration are questionable: necrosis may appear at the injection site, and, given the impaired microcirculation, the drug is unlikely to act properly. Therefore, the intravenous route is optimal - probably someone from your environment is able to give you an injection. Adrenaline is administered slowly, 0.3 milliliters at a time, constantly measuring blood pressure and pulse.
Allergy hormones, like dexamethasone or prednisolone, can also be kept in your medicine cabinet. They do not act immediately, but after 4-6 hours, but these drugs will help stabilize blood pressure by releasing their own endogenous adrenaline.
Be sure to inform others about your allergy and explain to them what to do if your condition becomes dangerous. Take care of yourself!
Vladimir Shpinev
Photo thinkstockphotos.com
Products by topic: adrenaline, dexamethasone, prednisolone, Zyrtec, Suprastin, chloropyramine, activated carbon
Urgent Care
If there is a person in front of you who is having anaphylactic shock, emergency care means urgently calling an ambulance .
Over the phone, calmly and clearly explain what the symptoms are so that the medical staff is prepared for the situation.
After this, the patient needs to be transferred to a flat, hard surface, turn his head to the side and raise his legs .
Since vomiting often occurs during shock, in this position a person will not be able to choke on the masses. If the attack occurs indoors, you need to open the windows to access oxygen.
Remember to constantly check your pulse and breathing, as these functions are often impaired. To take your pulse, place two fingers firmly against the carotid artery or wrist.
Normally, the pulse should be smooth, full, from 60 to 90 beats per minute.
If the pulse is very weak or absent, you need to do chest compressions. If there is no breathing - the chest does not rise up and down - we proceed to artificial .
You can mouth-to-nose or mouth-to-nose using a damp cloth or napkin.
In parallel with these actions, you need to take a look at the skin . Perhaps the reason for this condition will be noticeable.
For example, a stuck wasp sting. It needs to be pulled out carefully. And pull the bandage tightly above the bite site so that the allergen does not spread through the bloodstream throughout the body.
Such actions will not improve a person’s health, but will help gain time and wait for an ambulance. Only qualified medical personnel can completely correct the situation.
What to do if a child has anaphylactic shock?
If anaphylactic shock is suspected, only a doctor can make an accurate diagnosis; parents can only suspect this reaction if the child already had an allergy, and try to stop the dangerous symptoms. Actions in case of anaphylactic shock or suspicion of it should be clear and consistent, and the first thing to do is call an ambulance.
First aid for anaphylactic shock in children
While waiting for a doctor, emergency care for anaphylactic shock in children is carried out by parents - this is important so as not to waste time. Actions for anaphylactic shock:
- Place your baby on a flat surface with a pillow under his feet to elevate them.
- Provide the child with free breathing - remove the scarf, unbutton the collar, open the window.
- The child's head should be turned to the side to prevent the tongue from retracting. If there are mouth guards in your mouth, they need to be removed.
- If the child vomits, vomit must be removed with a napkin.
- By phone, ask your doctor about which allergy medication is best to give to your child. Keep the doctor informed of all actions, be sure to write down what was given and in what dosages.
To stop the reaction, you need to stop or slow down the flow of the allergen:
- If the cause of anaphylactic shock is pills or foods, you need to rinse the stomach and give the baby a sorbent (activated carbon).
- If you are bitten by an insect, you need to remove the sting (if it remains in the wound) and apply ice to the bite site for 20 minutes.
- If the reaction began during the injection, the administration of the medicine should be stopped, ice should be placed on the injection site for 20-25 minutes, and a tight bandage should be applied above the injection site (if the injection site allows).
- If the reaction was provoked by the drug in the form of drops, rinse the eyes or sinuses (depending on where the drug was dropped).
Adrenaline for children with anaphylactic shock - dosage
The drug adrenaline for anaphylactic shock is the first aid, which doctors call the “drug of choice”, a medicine that is usually used as a priority for this problem. Adrenaline during anaphylactic shock eliminates the symptoms of an attack literally in moments, which is very important. If a child has already had an attack of anaphylactic shock, he should have an auto-injector with the required dosage. In all other cases, the dosage should be taken based on the patient's age.
How to administer adrenaline for anaphylactic shock in children?
Adrenaline (or Epinephrine - a synthetic analogue) is an emergency aid for anaphylactic shock in children. This hormone:
- constricts blood vessels;
- stimulates breathing and heartbeat;
- eliminates the effect of histamine on vascular walls.
Adrenaline for children with anaphylactic shock is administered intramuscularly - using an auto-injector, if the child already has one. In other cases, Adrenaline is administered intramuscularly with a regular syringe, after reaching the required (by age) dose.
Anaphylactic shock in children - clinical recommendations
Drug treatment of anaphylactic shock in children in a hospital includes many drugs that are administered by injection or droppers with a solution:
- antihistamines - Suprastin, Diphenhydramine, Tavegil;
- bronchodilators (to relieve bronchospasm) – Eufillin;
- steroids – Hydrocortisone, Prednisolone;
- to raise blood pressure – Norepinephrine;
- for the breakdown of penicillin and cephalosporin - the enzyme penicillinase.
Parents are advised to keep in their home medicine cabinet all the necessary medications that will help relieve allergies or anaphylactic shock:
- Adrenalin;
- Prednisolone;
- antiallergic drugs in the form of tablets and injections (Tavegil, Zodak);
- syringes, alcohol wipes for disinfection;
- saline solution
First aid
If anaphylactic shock is diagnosed, then first aid is the administration of adrenaline . Only he is able to counteract the allergen and the body’s acute reaction with lightning speed. If the patient can barely breathe, you need to give an injection under the root of the tongue.
When an allergic reaction is caused by a bite, the drug is injected into the vicinity of this red dot so that the poison does not spread further. If the affected area is on one arm, then adrenaline is also injected into the other.
Manipulation with the syringe must be done slowly so as not to cause a disturbance in the heart rhythm, or even a complete stop.
The drug should quickly relieve swelling of the airways. If this does not happen, then intubation or tracheotomy is performed - a hole is made through the neck and larynx, a tube is inserted so that the person can breathe through it.
After the patient’s condition has stabilized, doctors are restoring health with the help of suprastin and diphenhydramine - antihistamines that do not affect blood pressure and do not cause drug allergies.
Specialists cannot immediately send the patient home without diagnosis in order to prevent recurrence of shock. To do this, you need to establish the type of allergen , because this is not always an obvious bee sting.
The allergen could be some component from a complex dish, or a smell on the street.
Examined using:
- blood test for immunoglobulin E;
- provocative tests;
- Patch test is a patch test with chemical allergens.
After the diagnostic result, we can say with high accuracy what caused it and prescribe treatment aimed at restoring the body.
Treatment
Help for anaphylactic shock should be provided immediately. Doctors make a tourniquet above the bite or injection of the drug to stop the flow of the allergen. Then they give an injection of adrenaline and an antiallergic drug.
The person is placed on his back and his head is tilted to the side to prevent him from suffocating. Provide oxygen flow. If necessary, use an oxygen cushion.
Subsequent treatment is aimed at bringing cardiovascular activity and breathing back to normal, as well as preventing possible complications.
Consequences of anaphylactic shock
If a person was provided timely emergency assistance, which was successful, after which the patient still underwent additional treatment, there may still be chronic disorders :
- since during anaphylactic shock blood did not flow to the heart, it may hurt for a long time after the situation;
- chronic low blood pressure;
- constant fatigue and slowness.
Anaphylactic shock can also cause :
- irregular nausea and vomiting;
- pain in the joints, abdomen and chest;
- myocarditis;
- neuritis;
- diffuse damage to the central nervous system.
Therefore, it is important to see a doctor , even if you managed to survive a seizure on your own. All consequences are removed with the help of well-chosen therapy.
Symptoms
The development of symptoms begins almost at lightning speed, which is the danger of this reaction. After an allergen enters the body, anaphylactic shock can occur within 10-30 minutes; with insect bites, the reaction begins to appear within 2 minutes after the insect attack.
Such reactions may manifest themselves very slightly, for example, itching of the skin, swelling or redness of the skin. However, in particularly acute reactions, suffocation may occur due to swelling of the respiratory tract, cardiac arrest, stiffness, and convulsions.
The most common reactions are:
- The skin may become covered with red spots and blisters may appear on it. The rash is accompanied by severe itching and burning.
- The mucous membranes are susceptible to changes, resulting in severe swelling of the mucous tract and eyes, and lacrimation begins.
- Breathing is impaired due to severe swelling, cramps and spasms.
- Neck compression or a feeling of a lump due to swelling constricting the throat.
- Vomiting and abdominal pain may occur if the allergen comes from food.
- Metallic or bitter tastes may appear in the mouth.
- Panic, neurasthenia, hysterical states that can be caused by confusion.
- The victim may faint or experience severe dizziness. Blood pressure rises.
Signs of anaphylactic shock and emergency assistance
There are several stages in the course of this dangerous condition:
- Lightning fast . The patient rapidly develops vascular, respiratory and heart failure. Despite the measures taken, in 90% of cases it is not possible to save the lives of patients.
- Lingering . Shock in allergy sufferers develops against the background of the administration of drugs prohibited for them. In this case, intensive therapy is carried out, the duration of which is several days (it all depends on the condition of the patient, who must be under the supervision of specialists at all times).
- Abortive . With the development of this variant of allergic shock, there is no threat to the life of patients. This condition can be quickly relieved with special medications.
With the development of recurrent anaphylactic shock, patients may experience a repeat of the pathological condition, since their body is periodically exposed to allergens unknown to them.
Experts classify such episodes as follows:
- " Harbingers ". The patient may feel dizzy and weak throughout the body. Very quickly he develops nausea and headache. A large number of patients exhibit various types of allergic manifestations on their mucous membranes and skin. There is discomfort and a feeling of anxiety. The patient may complain that he cannot breathe, hearing loss, loss of vision, and numbness in the limbs.
- " Height " An allergic person's blood pressure rapidly drops, which can cause him to lose consciousness. The skin becomes painfully pale, tachycardia develops, and sticky cold sweat appears. The person begins to breathe noisily, develops cyanosis of the limbs and lips, and develops severe itching. Problems with urine output begin; this process may be stopped, or, on the contrary, incontinence may occur.
- " Coming out of shock ." This stage of anaphylaxis can last for several days. All this time, the allergy sufferer will retain characteristic symptoms: weakness, lack of appetite (partial or complete), severe dizziness.
Modern medicine has identified 5 clinical forms of this pathological condition:
| Allergy sufferers experience respiratory failure and bronchospasm may occur. Such conditions are accompanied by characteristic symptoms: the voice becomes hoarse, breathing becomes difficult, and shortness of breath appears. At this stage, quite often allergy sufferers develop Quincke's edema, the danger of which is that the patient's breathing may be completely blocked. | Asphyxial |
| An allergy sufferer experiences pain in the abdomen. Sometimes they are so intense that they are confused with symptoms of acute appendicitis or perforated ulcerative pathology. A gag reflex may begin and the process of defecation may be disrupted. | Abdominal |
| This form of pathological condition is dangerous because the patient may experience swelling of the brain and its membranes. This process is accompanied by convulsions. The victim may experience severe nausea, which will be replaced by a gag reflex (usually it does not bring even short-term relief). The patient may fall into stupor or coma | Cerebral |
| Pain sensations appear in the heart area (they resemble pain during myocardial infarction). Blood pressure drops rapidly | Hemodynamic |
| This form occurs in most victims. Victims exhibit general symptoms | Generalized |