Causes and mechanism of development
The cause of a throat abscess is a pyogenic infection. These can be streptococci and staphylococci, E. coli, Klebsiella and other conditionally pathogenic bacteria.
Most often, the infection enters the throat through contact, due to improper treatment of diseases such as purulent tonsillitis, mastoiditis, inflammation of the middle ear, osteomyelitis of the lower jaw, pharyngitis, pulpitis of the seventh-eighth tooth, inflammation of the salivary glands against the background of a decrease in the protective functions of the body.
The main cause of throat abscesses of any location is chronic tonsillitis.
Much less common is the lymphogenous or hematogenous route of penetration of pathogenic flora into the throat - bacteria through the blood or lymph flow enter the fatty tissue and settle there, forming an abscess. In this case, any purulent process in the human body can become a source of infection. Abscesses in the throat can develop due to trauma, for example, when swallowing sharp objects and damaging the mucous membrane of the oropharynx.
general description
Peritonsillar abscess (J36) is an inflammatory process in the paratonsillar tissue (tissues surrounding the tonsil).
The disease occurs mainly at the age of 15-30 years equally in men and women, more often in late autumn, early spring, but also develops in the summer as a result of local cooling, for example, drinks, ice cream.
Types: anterosuperior, anterioinferior, posterosuperior, posteroinferior, lateral paratonsillar abscess. The process is one-sided, develops a few days after the end of a sore throat, exacerbation of chronic tonsillitis.
Symptoms
One of the symptoms is an increase in temperature to 40 degrees.
Throat abscess is an acute disease characterized by a sudden onset. Main features:
- increase in body temperature up to 40 degrees;
- chills;
- aches in muscles and joints;
- general weakness and malaise;
- severe headache;
- sore throat that gets worse when swallowing;
- spasms of the masticatory muscles, which are manifested by a sharp spastic clenching of the teeth;
- sharp pain when opening the mouth;
- swelling of the neck;
- irradiation of pain when swallowing into the ear;
- increased salivation;
- bad breath;
- enlargement and tenderness of the cervical lymph nodes (cervical lymphadenitis).
How do doctors classify the disease?
Phlegmonous tonsillitis is always located in the tonsil area. But to be more precise, all paratonsillar abscesses can be divided into the following types:
- Located between the tonsil and the anterosuperior region of the palate. This is the so-called anterosuperior peritonsillar abscess.
- Peritonsillar abscesses located behind the palatine arch are called posterior.
- If phlegmonous tonsillitis is localized between two tonsils - lingual and palatine, it is customary to speak of a lower paratonsillar abscess.
- The diagnosis of external paratonsillar abscesses is made when paratonsillitis is localized on the outside of the tonsil.
- In pediatric practice, phlegmonous tonsillitis occurs, located in the muscles of the pharynx, then a retropharyngeal abscess is diagnosed.
Diagnostics
To make a diagnosis of “purulent throat abscess,” the otolaryngologist performs a general examination of the patient, examines the throat using a laryngoscope, and prescribes laboratory tests and puncture.
During a general examination, swelling of the soft tissues of the neck, pain and enlargement of the lymph nodes, pain when palpating the neck below the chin and along the jugular vein are observed.
A general blood test will show the presence of the disease.
Pharyngoscopy will show a fluctuating protrusion at the site of the oropharyngeal abscess and redness, infiltration and swelling of the mucous membrane. Of the laboratory tests, the most informative is a general blood test - against the background of a pronounced increase in the number of leukocytes, a shift in the leukocyte formula to the left is observed. The erythrocyte sedimentation rate is increased.
When the protrusion is punctured, purulent contents with an unpleasant odor are obtained. The pus should be sent for culture, followed by determination of sensitivity to antibiotics. The puncture can be performed with or without local anesthesia.
Characteristic symptoms of an abscess
Any peritonsillar abscess, regardless of location, has typical symptoms. The throat hurts, and the pain gradually intensifies as the disease progresses. It is difficult for the patient not only to swallow, but also to simply open his mouth. The voice becomes hoarse and nasal. Body temperature is high, sometimes hyperthermia reaches critically high levels. The lymph nodes in the neck and under the lower jaw become enlarged.
Erased symptoms are characteristic of only one type of pathology - posterior paratonsillar abscess. With such localization, instrumental diagnosis of the disease is used - laryngoscopy. A detailed examination of the posterior pharyngeal wall helps to clarify the diagnosis and prevent spontaneous opening of a peritonsillar abscess.
A tonsil abscess is rarely bilateral, so patients often complain of pain on the affected side. Patients try not to turn their heads, and if necessary, turn their whole body towards the interlocutor. Sometimes it is easier for a person to keep his head constantly tilted to the painful side - pain in this position bothers him less.
Symptoms of general intoxication are always present - the patient refuses to drink and eat, becomes lethargic and weak, and looks exhausted and apathetic from constant pain.
If after a sore throat you have a headache, feel a lump in the throat, have a fever, feel weak and short of breath, then this may mean a complication in the form of meningitis.
Treatment
Treatment for oropharyngeal abscess is only surgical. Hospitalization to a hospital is required, where specific symptomatic therapy is prescribed and an autopsy of the formation is performed.
For symptomatic treatment, the following is prescribed:
- antipyretic drugs (non-steroidal anti-inflammatory drugs);
- novocaine injections into the masticatory muscles to relieve spasms;
- antihistamines - to reduce swelling and prevent autoimmune complications;
- in severe cases of the disease with severe intoxication syndrome, detoxification therapy is mandatory.
Specific treatment involves the use of broad-spectrum antibiotics. These can be second-third generation fluoroquinolones (Norfloxacin, Levofloxacin, Ofloxacin), sulfonamides (Biseptol, Sulfargin) and first-third generation ceftriaxones (Cefazolin, Ceftriaxone, Cefotaxime). Protected penicillins and their combination with clavulanic acid, such as Amoxil, Amoxiclav, Lincomycin, have proven themselves well. The type of antibiotic, its dose and method of administration are prescribed only by a doctor, after a thorough assessment of the patient’s condition.
Surgical treatment includes opening and cleaning the abscess cavity along with drug therapy. Using traditional methods, an abscess of the oropharynx should be treated only after consultation with your doctor.
How to treat with medications?
It is important to identify the disease in its initial stage. To diagnose it, you will need to consult an otolaryngologist and possibly an infectious disease specialist. Using special smears, the nature of paratonsillitis is determined. Only after this is appropriate treatment prescribed. Self-treatment of the disease is strictly prohibited. This can lead to a more severe form of it, with possible serious complications.
Different forms and stages of paratonsillitis require different treatment tactics.
Infiltrative paratonsillitis is treated with conservative therapy prescribed by a doctor. An important condition for this is to identify the localization of inflammation at an early stage and hit the source of infection. It is necessary to use all the necessary medications for 4-5 days until a purulent paratonsillar abscess forms and prevent complications. Antibiotics are an effective treatment.
Do you need anesthesia?
Patients with throat abscess undergo surgery under local anesthesia. General anesthesia is not recommended due to the fact that the volume of the operation is small and local anesthesia is quite sufficient. Local anesthesia does not require lengthy preparation, the patient is available for contact during the operation, and can be performed on persons with cardiovascular diseases and elderly patients. Anesthesia in the treatment of oropharyngeal abscess is used for people with mental illness and people who are intolerant to drugs for local anesthesia.
How is the operation performed?
After lubricating or applying lidocaine to the incision site, the mucous membrane is infiltrated with a solution of procaine for anesthesia. When sensitivity disappears, an incision up to two centimeters long and to the same depth is made in the area of greatest bulging. Next, the hole is expanded with forceps and drainage is installed. To prevent the walls of the cavity from sticking together and sticking together, a small gauze turunda is placed into the incision. The puncture is checked for three days, noting whether the purulent contents drain sufficiently; if necessary, the hole is widened. To prevent pus and blood from flowing into the throat, aspirators are used. The cavity is washed with a solution of an antibiotic or antiseptic; sulfonamides, for example, Streptocide, are often used for such purposes.
Depending on the location of the abscess, it is recommended to remove the tonsils. When the formation is localized peritonsillar, this procedure is necessary not only to eliminate the disease, but also to prevent relapses. Depending on the severity of the disease, one or both tonsils are removed.
Indications for tonsillectomy:
- frequent recurrences of abscess in the past;
- chronic tonsillitis;
- lateral localization of paratonsillar abscess;
- complicated paratonsillitis;
- severe abscess;
- diabetes;
- After surgical treatment, the patient's condition worsens.
Contraindications for tonsil removal:
- diseases of the hematopoietic system;
- vitamin deficiency, in particular scurvy;
- hypertonic disease;
- decreased blood clotting;
- tuberculosis;
- decompensated diseases of the cardiovascular system;
- sepsis;
- thrombosis of cerebral vessels;
- inflammation of the meninges.
After surgery, it is necessary to gargle with an antiseptic to drain the pus.
Typically, the tonsils are removed during drainage of the abscess. Very rarely, access to the pathological formation is carried out through the anterior surface of the neck. To improve the discharge of pus after surgery, gargling with antiseptic solutions (Orasept, furatsilin) or a hypertonic solution of salt and iodine is prescribed.
The positive effect of treating a throat abscess in uncomplicated cases is observed in the very first minutes after opening the abscess cavity. The temperature drops, the pain decreases, and the symptoms of intoxication go away. In this case, the doctor may discharge the patient on the fifth day of hospitalization. On average, a patient stays in hospital for about ten days.
Question: What is the opening of a peritonsillar abscess?
The site provides reference information for informational purposes only.
Diagnosis and treatment of diseases must be carried out under the supervision of a specialist. All drugs have contraindications. Consultation with a specialist is required! What is the opening of a peritonsillar abscess?
Opening an abscess is the main method of treating purulent diseases in the pharynx (
peritonsillar abscess, retropharyngeal abscess
). It is performed on almost all patients, regardless of their age or gender. It is believed that an abscess can be opened 4–5 days after its formation. If you perform the operation earlier, it may turn out that the cavity with pus has not yet formed. At this stage, pyogenic microbes have already saturated the fiber around the tonsil, but the melting of the tissue has not yet occurred. To check the “readiness” of the abscess for opening, a diagnostic puncture is sometimes performed.
A diagnostic puncture is an injection with a special thick needle into the most protruding area near the tonsil. If possible, the needle stroke is monitored using fluoroscopy or ultrasound. After the puncture, the doctor carefully pulls back the syringe plunger and draws a small amount of content into the barrel. Detection of pus is a signal that an abscess has formed and is ready to be opened. If the syringe does not collect liquid, or a mixture of blood, lymph and a small amount of pus is collected, then an abscess is still forming. At this stage, it is better to start intensive antibiotic therapy, since there is still a chance to avoid surgery.
Indications for diagnostic puncture are:
- a sore throat lasting more than 5 days ( this time is enough for an abscess to form
); - severe pain in the throat ( worsens when swallowing, talking, moving the head
); - temperature more than 39 degrees;
- severe enlargement of one of the tonsils ( bilateral paratonsillar abscess is very rare
); - enlargement of regional lymph nodes ( at least one
); - signs of general intoxication - headaches, apathy, drowsiness, muscle pain;
- moderate increase in breathing and heart rate.
In principle, during a puncture under ultrasound or fluoroscopy control, most of the pus can be removed from the cavity. However, it is still recommended to open the abscess.
Opening an abscess is considered a necessary procedure for the following reasons:
- It helps prevent the spread of pus. The contents of the cavity are released or sucked out with a special syringe.
- During an autopsy ( as opposed to a puncture
), the doctor has the opportunity to treat the abscess cavity. To do this, he washes it with special antiseptic solutions. - For small abscesses ( up to 1 centimeter in diameter
), a decision may be made not to open the cavity, but to remove it entirely, including the walls. - After releasing the pus, a sharp improvement in the patient's condition is observed. The pain subsides, body temperature decreases, and the general condition returns to normal within a few days.
- Opening an abscess involves the destruction of pyogenic microbes ( as opposed to puncture
), so the risk of re-formation of a purulent cavity is very small. - When opening an abscess, a parallel tonsillectomy ( removal of tonsils
) is often performed.
This facilitates access to deep abscesses and eliminates the chronic inflammatory focus. By removing the tonsils, the risk of relapse ( re-formation of an abscess
) is greatly reduced.
From a medical point of view, the operation itself is quite simple and rarely leads to any complications. Most patients are not even admitted to hospital treatment. The opening of the abscess is performed on an outpatient basis, after which the patient is prescribed a detailed course of treatment at home and warned of the need for a follow-up examination in a few days.
The following categories of people with peritonsillar abscess are subject to hospitalization:
- children ( preschool children may be hospitalized with one of their parents
); - persons with reduced immunity;
- persons with severe concomitant diseases;
- pregnant women;
- patients with a high risk of complications ( sepsis, phlegmon, mediastinitis
); - patients whose puncture showed the absence of a formed cavity with pus are hospitalized for careful medical monitoring.
Direct opening of the abscess is carried out under local anesthesia ( dicaine solution 2%, cocaine solution 5%
).
In emergency cases, dissection of the abscess wall is allowed without additional local anesthesia. An incision is made at the point of greatest protrusion of the pharyngeal wall ( here the wall is thinnest and the abscess lies more superficially
). The depth of the incision should not exceed 1 - 1.5 cm, so as not to damage nearby bundles of blood vessels and nerves. After releasing the bulk of the pus, the doctor penetrates the cavity with a blunt instrument and destroys the partitions inside it, if any. This improves the outflow of pus and prevents its point accumulations, which can subsequently lead to relapse. After this, a disinfectant solution is pumped into the cavity. After suturing the cavity, additional measures to stop bleeding are usually not required.
Antibiotic therapy is a mandatory element of surgical treatment of peritonsillar abscess. For planned surgery, antimicrobial drugs are started several days before the intervention. This weakens pyogenic microbes and prevents them from spreading to neighboring areas during the operation. After opening the peritonsillar abscess, antibiotics are taken for several more days. This is necessary to prevent relapse of the disease.
If an abscess is opened, but it is discovered that the pus is not localized, but has begun to spread between the fascia of the neck, the doctor acts according to the situation. Such cases pose a danger to the patient’s life, so there are no uniform rules for such operations. If the abscess has formed under the influence of anaerobic microbes, the scope of the operation can be expanded. These microorganisms develop best in conditions without access to air. To create unfavorable conditions for them, drainage can be left ( a special tube or tubes
). They are brought out through additional incisions in the skin of the neck. This creates additional air flow and outflow of forming pus and blood. After a few days, if there are no signs of relapse, the drainage is removed and the incisions are sutured.
Complications
If oropharyngeal abscesses are left untreated or treated independently, the following complications may occur:
- As a result of purulent melting of the soft tissues of the neck, vessels of different calibers can be damaged, which leads to bleeding. Hemorrhage from arteries and arterioles can be fatal.
- The breakthrough of an abscess into the retropharyngeal space leads to the penetration of pus into the fatty tissue behind the pharynx, from where it can go down, provoking mediastinitis.
- Sepsis. Generalization of the process due to hematogenous or lymphogenous spread of infection.
- Dissemination of pyogenic flora into the cranial cavity can lead to brain abscesses, bacterial meningitis, and thrombosis of the cavernous sinus.
- Retropharyngeal abscesses can be complicated by phlegmonous laryngitis, perichondritis or phlegmon of the neck.
- Pneumonia when the infection spreads to the lungs.
- Asphyxia due to swelling of fatty tissue and bulging of a purulent cavity into the windpipe.
Bleeding can also occur during an incision, but in a hospital setting the chances of preventing or stopping hemorrhage in time are much higher. Also, throat abscesses can lead to exacerbation of chronic diseases such as rheumatism, pyelonephritis, tuberculosis or cardiovascular diseases.
Types of abscesses of the pharynx and throat
Despite popular belief, an abscess in the throat area consists of several different diseases, the form, complexity of treatment and symptoms of which depend on a group of factors and localization - the place of origin. It is customary to distinguish abscesses:
- peripharyngeal or peritonsillar - a purulent process on the tissues of the tissue in the pharynx, caused by the spread of infection through the lymphatic tract;
- retropharyngeal or retropharyngeal is localized in the posterior part of the pharyngeal region, affects the tissue, starting with damage to the lymph nodes;
- a paratonsillar purulent process can develop as a consequence and complication of tonsillitis in an elderly person.
It is important to know: What causes a sore throat - causes and dangers
In this case, an abscess of the pharynx associated with the tonsils can affect them from above, on the outside of the side, below and in the back. The most dangerous scenario may be a complicated course of a lateral abscess on the tonsils. In its advanced form and when the immune system is weakened, it can spread to other organs and cause mediastinitis.
Prevention
There is no specific prevention of throat abscesses. To prevent or reduce your chances of getting sick to a minimum:
- treat sore throats or other throat infections in a timely manner;
- to refuse from bad habits;
- be examined by a dentist once every six months;
- for chronic tosillitis – remove the tonsils;
- adhere to the rules of personal hygiene;
- strengthen the body's defenses.
To avoid complications, you must strictly follow your doctor’s recommendations and do not interrupt the course of antibiotics prematurely.
Causes of paratonsillitis
The spread of infection in the oral cavity is due to the anatomical features of the tonsils and surrounding tissues. The tonsils have small depressions called crypts. During the course of the disease, pus accumulates in them and an abscess is formed. The deepest crypts are located on the top of the tonsils, so this is where the development of tonsillitis is observed.
Gradually, scars form in place of the ulcers, which impair the drainage function of the tonsils. Pus and fluid remain in the recesses, and an intratonsilal abscess begins. If the source of inflammation is not eliminated, new sources of infection appear, and the cleansing of the crypts slows down. The infection has the opportunity to penetrate deep into the glands and into the adjacent space. This phenomenon is called a paratonsillar abscess. Loose periamond tissues are “fertile ground” for infection. Therefore, abscesses occur here very often.
The cause of a paratonsillar abscess is often any purulent inflammation in the mouth: caries, periotitis, trauma. Less commonly, the infection enters through the blood or inner ear. Doctors observe a predisposition to abscesses in the following categories of patients:
- patients with diabetes mellitus,
- with anemia,
- with reduced immunity,
- during oncological processes in the body.
If a small portion of lymphoid tissue remains after tonsil removal, it can also become a source of inflammation. All of the above health problems lead to deterioration of immunity. Thanks to this, it is easier for the infection to overcome the defense and enter the body. The inflammation first takes on a catarrhal form, suppuration gradually appears, the inflammation intensifies and develops into a peritonsillar abscess.
Classification
For peritonsillar abscess, treatment should be prescribed taking into account the identified form of the disease. This determines what medications to take and how to prevent complications. There are three main forms of paratonsillitis, the description of which will help to accurately establish the diagnosis:
- Edema. It is the most difficult to diagnose because the symptoms are difficult to distinguish from the common cold. Characteristic signs are sore throat, redness, and swelling of the mucous membrane.
- Infiltrative. It is accompanied by obvious signs of intoxication: headache, fever, weakness. Local symptoms also appear: the throat becomes red, every sip causes severe pain. Up to 15% of patients see a doctor with this form of paratonsillitis.
- Abscessing. If the disease was not diagnosed at previous stages, then ulcers of various locations appear. Most often, patients (about 85%) see a doctor at this stage of the disease.
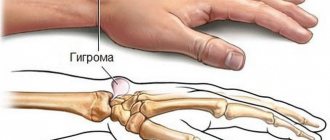
The location of the abscess affects symptoms and treatment. Taking this factor into account, several types of the disease are distinguished. The most common are the anterior and supratonsillar. It is localized above the tonsil, covering the mucosa between the tonsil and the anterior arch. Occurs in 70% of patients. The second most common type of abscess is the posterior abscess. It develops in 16% of cases, located on the mucosa between the posterior arch and the tonsil. In only 7% of cases, a lower abscess occurs. Its location is between the lateral part of the pharynx and the lower part of the tonsil.
The rarest (up to 4%), but the most severe form is a lateral or lateral abscess. It covers the mucous membrane between the pharynx and the middle of the tonsil. Considering that the limited space does not allow the abscess to break through and clean the cavity, pus accumulates and neighboring tissues become inflamed.
Inflammation is equally likely to begin on either side of the tonsils. Left-sided paratonsillar abscess occurs no less often than right-sided one. There are no special anatomical prerequisites for which side the abscess will appear on. The severity of symptoms and the nature of their manifestation help to identify the disease.