Epilepsy is considered one of the common neurological diseases that are considered chronic. The reason often lies in damage to parts of the brain. The most important symptom is an epileptic seizure, which is difficult for a person to control. The article also discusses the treatment and prognosis of this disease, a common type of which is temporal lobe epilepsy.
Treatment approaches
The main treatment method for partial epilepsy is medication with additional psychotherapeutic support. If a secondary nature of the disease is identified, therapy for the underlying disease is carried out. If the patient has a tumor, vascular malformations, cysts and other space-occupying formations in the brain, neurosurgical removal is necessary.
Medicines prescribed for partial epilepsy
The focal form of epilepsy is most often treated on an outpatient basis, since the patient does not require hospitalization after diagnosis. The patient is prescribed various anticonvulsants to avoid the development of repeated epileptic seizures. Therapy always begins with one drug, since the partial type of pathology responds well to the use of medications of this group. Taking two or more anticonvulsants is not recommended due to their negative impact on the cognitive and mental sphere of a person. Preference is given to the following drugs:
- Depakine, Konvulex and other valproates. In addition to the anticonvulsant effect, they reduce the patient’s anxiety and normalize his mood. Recommended for use in case of changes in the emotional-volitional sphere.
- Finlepsin and Carbamazepine eliminate epileptic seizures, and also improve mood and increase mental activity. Used in most patient groups. Carbamazepine should not be used in patients with absence seizures.
- Lamotrigine is a classic drug that affects serotonin reuptake. Additionally, it has antidepressant activity. With long-term use, it improves the cognitive functions of patients and the prognosis for the patient.
- Trileptal is the drug of choice when medications are used to treat concomitant pathologies. Unlike the above agents, it does not interact with other drugs.
- Levetiracetam is one of the modern drugs for the treatment of partial epilepsy. It has pronounced anticonvulsant and neuroprotective activity. Recommended as first-line therapy in patients with primary or re-diagnosed epilepsy, including the elderly and women of childbearing age.
In the presence of pronounced mental and cognitive abnormalities, it is possible to prescribe nootropics (Piracetam, Glycine), antidepressants (Fluoxetine, Amitriptyline), mood stabilizers (lithium salts) and other drugs. When using several types of psychotropic drugs, the doctor takes into account their drug interactions.
On the subject: Drug treatment of epilepsy
In addition to drug treatment, psychotherapy is indicated for all patients. An experienced specialist helps sufferers improve their quality of life and improve their adaptation to society.
The duration of therapy depends on the number of identified attacks. For a single seizure, therapy should continue for 2 years until it is completely discontinued. With 2 attacks, the duration increases to 5 years. With three or more – for life.
Treatment of temporal lobe epilepsy
It can take up to a year to diagnose temporal lobe epilepsy. Treatment is mainly aimed at controlling the occurrence of seizures, reducing their occurrence. This helps to lengthen the time of remission and improve the patient’s well-being. With timely treatment, complete relief from the disease is possible in 60% of cases.
In the treatment of temporal lobe epilepsy, anticonvulsant therapy is used, which in 60% of cases reduces the number of seizures, and in 11-25% of cases a prolonged absence of seizures is recorded.
Antiepileptic drugs are the main ones and are used as monotherapy and polytherapy. Here are used:
- Valproate.
- Hydantoins.
- Barbiturates.
- Phenytoin.
- Carbamazepine.
If one drug is ineffective, several are prescribed (Finlepsin and Lamictala or Finlepsin and Depakine). Lamotrigine and Benzodiazepines are also prescribed. However, the patient becomes accustomed to them. They provide only a temporary effect in stopping the occurrence of attacks. This forces doctors to use other methods of treating temporal lobe epilepsy - neurosurgical intervention:
- Amygdalotomy.
- Selective hippocampotomy.
- Focal resection.
- Temporal resection.
These procedures allow you to get rid of epileptic seizures forever (in 75-80% of cases), since the source of their occurrence is eliminated. In other (more complex) cases, these measures are ineffective. Complications may occur:
- Hemiparesis.
- Mnestic disorders.
- Speech disorder.
That is why when choosing a method, many factors are taken into account, which are diagnosed by the doctor.
Forecast
Focal epilepsy is a disease that has a much more positive prognosis than the generalized form.
If you take medications correctly and follow the therapy prescribed by your doctor, it can be cured. As a last resort, there is a surgical method, that is, removal of the affected area of the brain.
Epilepsy is the most common neurological disease.
This means that no one is immune from developing this pathology.
It can easily appear after an injury - even if several years have passed.
Therefore, it is necessary to carefully monitor your condition and be sure to consult a doctor without waiting for the pathology to develop into a disease that cannot be controlled with medications.
Classification
In clinical practice, there are three variants of PE:
- symptomatic;
- cryptogenic;
- idiopathic.
The symptomatic form is associated with organic changes in the brain that developed as a result of previous diseases - infections, traumatic brain injuries, the growth of malignant tumors, etc. Similar conditions are detected in the patient during MRI and other research methods.
The cryptogenic variant of the disease is associated with previous damage to the central nervous system, however, organic changes in the brain are not detected during examination. As a rule, patients themselves note a history of traumatic brain injuries, stroke and other lesions of the nervous system.
In the case of idiopathic focal epilepsy, there is no disease or injury to the brain. The cause is genetic disorders of the nervous tissue or functional immaturity of the cerebral cortex. The prognosis is positive, since symptoms in adolescents and young children are mild and do not lead to the development of neurological deficits. The following types of idiopathic epilepsy are distinguished: Gastaut childhood occipital epilepsy, benign rolandic epilepsy, etc.
Symptoms of partial seizures
The leading symptom of epilepsy is considered to be focal seizures, which are divided into simple and complex. In the first case, the following disorders are noted without loss of consciousness:
- motor (motor);
- sensitive;
- somatosensory, supplemented by auditory, olfactory, visual and gustatory hallucinations;
- vegetative.
Prolonged development of localized focal (partial) symptomatic epilepsy leads to complex seizures (with loss of consciousness) and mental disorders. These seizures are often accompanied by automatic actions that the patient has no control over and temporary confusion.
Over time, the course of cryptogenic focal epilepsy can become generalized. With such a development of events, an epileptic attack begins with convulsions affecting mainly the upper parts of the body (face, arms), after which it spreads lower.
The nature of the seizures varies depending on the patient. In the symptomatic form of focal epilepsy, a person’s cognitive abilities may decrease, and in children there is a delay in intellectual development. The idiopathic type of the disease does not cause such complications.
Foci of gliosis in pathology also have a certain influence on the nature of the clinical picture. Based on this feature, types of temporal, frontal, occipital and parietal epilepsy are distinguished.
Frontal lobe lesion
When the frontal lobe is damaged, motor paroxysms of Jacksonian epilepsy occur. This form of the disease is characterized by epileptic seizures during which the patient remains conscious. Damage to the frontal lobe usually causes stereotypical short-term paroxysms, which later become serial. Initially, during an attack, convulsive twitching of the muscles of the face and upper limbs is noted. They then spread to the leg on the same side.
Turning of the eyes and head is often observed. During seizures, patients often make complex movements with their arms and legs and become aggressive, shouting words or making strange noises. In addition, this form of the disease usually manifests itself during sleep.
Temporal lobe lesion
This localization of the epileptic focus of the affected area of the brain is the most common. Each attack of a neurological disorder is preceded by an aura characterized by the following phenomena:
- abdominal pain that cannot be described;
- hallucinations and other signs of visual impairment;
- olfactory disorders;
- distortion of the perception of surrounding reality.
Depending on the location of the focus of gliosis, attacks may be accompanied by a short-term loss of consciousness, which lasts 30-60 seconds. In children, the temporal form of focal epilepsy causes involuntary screams, in adults – automatic movements of the limbs. At the same time, the rest of the body freezes completely. Attacks of fear, depersonalization, and a feeling that the current situation is unreal are also possible.
As the pathology progresses, mental disorders and cognitive impairments develop: memory impairment, decreased intelligence. Patients with the temporal form become conflicted and morally unstable.
Parietal lobe lesion
Foci of gliosis are rarely detected in the parietal lobe. Lesions in this part of the brain are usually observed with tumors or cortical dysplasia. Seizures cause tingling sensations, pain and electrical discharges that shoot through the hands and face. In some cases, these symptoms extend to the groin area, thighs and buttocks.
Possible symptoms include disturbances in speech functions and spatial orientation. In this case, attacks of parietal focal epilepsy are not accompanied by loss of consciousness.
Occipital lobe lesion
Localization of foci of gliosis in the occipital lobe causes epileptic seizures, characterized by decreased quality of vision and oculomotor disorders. The following symptoms of an epileptic seizure are also possible:
- visual hallucinations;
- illusions;
- amaurosis (temporary blindness);
- narrowing of the field of view.
With oculomotor disorders the following are noted:
- nystagmus;
- fluttering eyelids;
- miosis affecting both eyes;
- involuntary rotation of the eyeball towards the focus of gliosis.
Along with these symptoms, patients are bothered by pain in the epigastric region, pale skin, migraine, and attacks of nausea with vomiting.
Symptoms
Cryptogenic epilepsy is manifested by the following features:
- Sudden epileptic seizures.
- Developing mental disorders.
- Decreased intellectual abilities, personality degradation.
Distinctive signs of a cryptogenic seizure:
- Increased physical activity (sharp running, shouting, chaotic movements).
- Vegetative manifestations: fever, dizziness, blood pressure surges.
- Mental manifestations: confusion, hallucinations, delusions.
- Frequent insomnia, attacks of tachycardia, after which a prolonged seizure develops.
An epileptic attack during FE develops as follows:
- Clonic convulsions occur: tension of the torso, throwing back of the head, bending of the limbs.
- Tachycardia occurs and blood pressure rises.
- The skin turns pale.
- Breathing becomes hoarse and apnea may develop.
- The tongue sinks in, foam comes out of the mouth.
After the seizure ends, the body relaxes and the patient falls asleep. Then he feels headache, fatigue, and drowsiness for a long time.
Patients with CE develop mental disorders:
- Decreased ability to think. The patient cannot solve basic logical problems.
- In speech, there is a focus on unimportant details.
- Uncontrollable outbursts of rage and aggression occur.
- A manic tendency towards order develops.
Find out more about epilepsy and its types:
- symptomatic and absence, Jacksonian and Kozhevnikovsky forms;
- rolandic and pharmacoresistant, partial and myoclonic;
- congenital and acquired, including alcoholic, nocturnal.
Symptoms of focal epilepsy
The leading symptom complex of FE is repeated partial (focal) epileptic paroxysms. They can be simple (without loss of consciousness) or complex (accompanied by loss of consciousness). Simple partial epileptic seizures are: motor (motor), sensitive (sensory), vegetative, somatosensory, with a hallucinatory (auditory, visual, olfactory or gustatory) component, with mental disorders. Complex partial epileptic seizures sometimes begin as simple ones, and then a disturbance of consciousness occurs. May be accompanied by automatisms. In the period after the attack, some confusion is noted.
Secondary generalization of partial seizures is possible. In such cases, an epileptic attack begins as a simple or complex focal one; as it develops, the excitation diffusely spreads to other parts of the cerebral cortex and the paroxysm takes on a generalized (clonic-tonic) character. One patient with FE may experience partial paroxysms of various types.
Symptomatic focal epilepsy, along with epileptic seizures, is accompanied by other symptoms corresponding to the underlying brain lesion. Symptomatic epilepsy leads to cognitive impairment and decreased intelligence, and delayed mental development in children. Idiapathic focal epilepsy is characterized by its benign quality and is not accompanied by neurological deficits or disorders of the mental and intellectual spheres.
Clinical features depending on the location of the epileptogenic focus
Focal temporal lobe epilepsy
. The most common form with localization of the epileptogenic focus in the temporal lobe. Temporal lobe epilepsy is most characterized by sensorimotor seizures with loss of consciousness, the presence of an aura and automatisms. The average duration of an attack is 30-60 s. In children, oral automatisms predominate; in adults, automatisms similar to gestures predominate. In half of the cases, paroxysms of temporal FE have secondary generalization. With damage to the temporal lobe of the dominant hemisphere, post-ictal aphasia is observed.
Frontal focal epilepsy
. An epi-focus located in the frontal lobe usually causes stereotypical short-term paroxysms with a tendency to be serial. The aura is not typical. Turning of the eyes and head, unusual motor phenomena (complex automatic gestures, pedaling with legs, etc.), and emotional symptoms (aggression, screaming, agitation) are often noted. With a focus in the precentral gyrus, motor paroxysms of Jacksonian epilepsy occur. In many patients, epileptic seizures occur during sleep.
Occipital focal epilepsy
. When the focus is localized in the occipital lobe, epileptic attacks often occur with visual impairment: transient amaurosis, narrowing of visual fields, visual illusions, ictal blinking, etc. The most common type of paroxysms is visual hallucinations lasting up to 13 minutes.
Parietal focal epilepsy
. The parietal lobe is the rarest location of the epi-focus. It is mainly affected by tumors and cortical dysplasias. As a rule, simple somatosensory paroxysms are observed. After the attack, short-term aphasia or Todd's palsy is possible. When the epiactive zone is located in the postcentral gyrus, sensory Jacksonian seizures are observed.
What is temporal lobe epilepsy?
Epilepsy has been known to mankind since ancient times. What is temporal lobe epilepsy? This is one of the forms of epilepsy, the lesion of which is located in the temporal lobe of the brain. It is characterized by the same seizures as other types of epilepsy.
This form manifests itself in simple seizures, when a person retains consciousness, and in severe ones, when consciousness is lost. Epileptic seizures are periodic, that is, repeated. However, temporal lobe epilepsy is not a death sentence. There are many surgical techniques that can help control the disease.
Mental disorders develop from the frequency of seizures. Doctors often note that the disease may be localized not in the temporal lobe, but in another part, but radiate to the temporal lobe.
This disease has been studied. The doctor identifies it through special diagnostic examinations, and he also prescribes treatment. To diagnose temporal lobe epilepsy the following is prescribed:
- MRI.
- PET scan of the brain.
- EEG.
- Neurological status data.
- Polysomnography.
Treatment is often carried out not only with medication, but also with psychotherapy.
Diagnostics
The diagnosis is made on the basis of some complaints from the patient himself, information received from loved ones who have observed epileptic seizures, data from a general examination, and in the absence of evidence of an etiological factor.
Laboratory methods are not very informative, since general and biochemical blood parameters and urine composition do not change.
Instrumental diagnostics are used to a greater extent. A study such as electroencephalography is the gold standard; it shows the bioelectrical activity of the brain and tells with high accuracy about the localization of the lesion, its size and the spread of pathological impulses. The only drawback is the fact that reliable information can only be obtained at the moment of an attack; the rest of the time, changes may not be recorded.
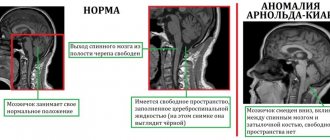
In order to have an idea of the structure of the brain and its changes, computed tomography and magnetic resonance imaging are additionally prescribed. It allows you to study the anatomical structures of the organ layer by layer.
Treatment is based on the use of antiepileptic drugs, these include Carbamazepine, Lamotrigine, Gabapentin, Topiramate, and valproic acid salts. Initially, the patient is prescribed one specific drug, preferably valproic acid and Carbamazepine. For some time, the patient is under the supervision of an epileptologist; if there is no effect, a combination of two medications is possible; this is no longer advisable, since the risk of complications increases. The dose of the active substance and the duration of therapy are selected individually. The drug is discontinued only after a few years and gradually with a positive trend and the absence of pathological changes on the electroencephalogram.
Treatment with folk remedies is possible, but it should not cancel taking medications prescribed by a specialist. Decoctions and infusions of oregano, adonis, meadowsweet, and valerian roots calm the nervous system, relieve convulsions and reduce the frequency of seizures. Such drugs can be used only in the absence of hypersensitivity and a tendency to allergic reactions.
Cryptogenic epilepsy, treatment of the disease
To cure the cryptogenic form of epilepsy, you should regularly use medications or go to a special clinic for a while. What dosage of the drug should be prescribed, what type it should be and how long it should be taken is decided by the attending physician. It will be based on the patient’s test results and research data on his condition.
Cryptogenic epilepsy requires competent treatment, which includes proper organization of the daily routine (be sure to alternate exercise and rest). In addition, it is advisable to protect the patient from various shocks. A healthy lifestyle is the basis for treating this disease.
Some patients are completely cured of all symptoms of cryptogenic epilepsy, while others reduce its manifestations to a minimum. In any case, the chance of successful treatment is high.
Classification by type of seizures
Let us consider in detail the manifestation of each.
A type of attack that is distinguished by a generalized nature and a state of short-term loss of consciousness with gaze stopping. Absence seizures were first studied and described in 1705, although the term “absence seizure” itself was used in 1824.
According to statistics, focal or other epilepsy manifests itself in absence seizures in 2-8 people per 100,000. They are more common in children, and in girls 2 times more often than in boys.
Almost all patients, at least 9 out of 10, suffer from variable motor disorders during absence seizures, and about two thirds experience automatisms - uncontrolled repetitive actions. When there is a combination of several symptoms of absence seizure in children or adults, it is called complex.
If you trace the behavior of absence seizure on the EEG, you will see bilaterally synchronous peak-wave complexes recorded at a frequency of 3 Hz. In this case, the maximum value of the peak wave occurs in the frontal regions, the minimum - in the back of the head and temporal lobes. But this does not mean that the source of activity is in the frontal lobe. Over one of the hemispheres, the complexes may be more pronounced, but this predominance can change its direction, as generalized epilepsy suggests. Also, only 40% or more of patients have discharges recorded on the EEG and between attacks.
The duration of one absence seizure ranges from 5 seconds to 2-3 minutes. Thus, children often exhibit atypical absence seizures, which can be interrupted by external factors.
Idiopathic epilepsy often manifests itself in the form of involuntary muscle contractions, which may be accompanied by joint movements. Epilepsy with myoclonus can be either generalized (general convulsive seizure) or focal for individual muscle groups.
Each convulsion in myoclonus corresponds to an electrical discharge on the EEG.
There is another option when myoclonus is in a negative form - the tone “turns off”, but the movement continues under the influence of gravity.
Generalized tonic-clonic seizure
Another option for how epilepsy can manifest itself is successive phases of continuous convulsions-contractions, followed by intermittent contractions. Loss of consciousness often occurs, with one phase of prolonged tone lasting 30-40 seconds, after which sharp rhythmic twitching begins. At the end of the attack - complete relaxation, up to weakness and falling into sleep. Salivation, involuntary urination and stool leakage are often observed.
Treatment
Relatives of patients with TBE should know how to properly provide first aid during an epileptic attack.
The algorithm is as follows:
- Place the patient on a horizontal surface, away from sharp corners.
- Place something soft under your head to prevent injury.
- Turn your head to the side so that the person does not choke on vomit and the tongue does not sink.
- Loosen the collar, remove the scarf, unbutton your outerwear.
- You cannot unclench your teeth, hold an epileptic, or straighten your arms.
- If the attack lasts too long, you should call an ambulance.
- After the seizure ends, the patient should be put to sleep.
There is no exclusive treatment regimen suitable only for this type.
The patient is prescribed anticonvulsants (Carbamazepine, Ethosuxemide).
They reduce the duration and frequency of seizures. GABA receptor antagonists (Picamilon, Aminalon) are also used. Additionally, diuretics are used to reduce swelling of the brain.
It is important to eat a high-fat diet. In this case, carbohydrates should be kept to a minimum. The patient must stop smoking and drinking alcohol.
As a last resort, they resort to surgical intervention, which involves influencing the excitation center.
Therapy for cryptogenic focal epilepsy in children is no different, only in the dosages of drugs; some drugs are prohibited for use in childhood.
Surgery is also not used. The duration of treatment depends on the severity of the disease. In some cases, you will have to take the drugs for life.
Frontal epilepsy
Among all symptomatic and probably symptomatic (cryptogenic) epilepsies, symptomatic frontal lobe epilepsy accounts for 20%. It can begin at any age depending on the cause. Depending on the location of the epileptogenic focus, 7 forms of frontal lobe epilepsy are distinguished, and each manifests itself with its own types of seizures. In general, it is characterized by local simple or complex seizures that arise in the frontal cortex - contralateral clonic convulsions, unilateral, bilateral tonic convulsions that end in Todd's palsy, complex automatisms that look like threshing movements of the limbs, swaying of the body, pedaling movements of the legs. Epileptic discharges in the supplementary frontal motor area are manifested by complex focal seizures in the form of tonic convulsions of the arms, the classic “fencer's pose,” adversion of the head, bilateral extension of the trunk, neck, and vocalization. Activity in the area of turning the head and eyes is manifested by adversion of the eyes to the opposite side, blinking. Consciousness is preserved or not completely lost. Seizures with a focus in the central zone (the area of the cortex at the Rolandian fissure) are characterized by a Jacksonian march or strictly localized clonic or tonic convulsions, facial convulsions, and loss of muscle tone. With skin irritation, a motor attack without loss of consciousness, facial spasms with swallowing, chewing movements, salivation with a sense of a different taste, and laryngeal symptoms may occur. The attacks are nocturnal, very often, short-term.
The neurological status reveals paresis, ataxia, intellectual and speech disorders.
EEG characteristics:
- underlying background activity is slowed down;
- regional epiactivity (sharp waves, acute-slow wave complexes, peak waves) bifrontal or diffuse activity;
- secondary bilateral synchronization (a sign of worsening of the disease, the appearance of cognitive impairment).
The treatment is complex. Very often attacks are resistant to adequate therapy. It is necessary to start with monotherapy with first-line drugs in an adequate dose, and then switch to a combination of drugs with different mechanisms of action, according to the Uniform Protocol for the Treatment of Epilepsy in Children 2014 First-line drugs - carbamazepine (contraindicated in secondary bilateral synchronization), oxcarbazepine, topiramate, second - drugs valproic acid, lamotrigine, the third - a combination of drugs.
Definition of the disease and its etiopathogenesis
In recent decades, there has been a growing interest in the study of the human brain in general and this disease in particular. This was largely facilitated by advances in the field of basic sciences, which provided new opportunities in the creation and use of fundamentally different medical technologies. They have made it possible to significantly expand both experimental and clinical research in the field of studying various problems of epilepsy, clarify the definition of the disease and its classification, and also improve treatment methods.
In 1989, the International League Against Epilepsy proposed a definition of epilepsy as a disease. It was based on repeated epileptic seizures. According to this definition, epilepsy was considered a condition characterized by repeated seizures (two or more) that were not provoked by an immediate cause.
This definition did not take into account, mainly, mental disorders of the patient and manifestations of pathology identified through electroencephalography. Despite significant shortcomings, for a long time it was of great importance in practical medical practice.
A more precise formulation was proposed by a group of Moscow researchers: epilepsy is a disease that is characterized by repeated (two or more) seizures or progressive neurological disorders that are not directly provoked by any specific cause and are combined with persistent activity of focal origin of the epileptic type, determined on the electroencephalogram .
Temporal lobe epilepsy is a localization-related and, most often, symptomatic form of the disease with the localization of the epileptogenic focus in the temporal lobe of the brain. The causes of the pathological condition are numerous and varied. Conventionally, they are combined into two main groups:
Perinatal damage to the central nervous system
The period covering from 22 weeks of pregnancy to the 28th day after birth. According to the anamnesis, it is detected in 36% of patients with this type of pathology. The group of causes includes mainly intrauterine infection (mainly cytomegalovirus, toxoplasmosis, herpetic, rubella measles), hypoxia and asphyxia of the fetus, focal cortical dysplasia (abnormal development of the structure of the cerebral cortex in a limited area) and some others.
The most common cause cited by many authors is birth trauma, which causes neuronal death. It is pathogenetically caused by ischemia (local vascular disruption of blood supply to tissues), hypoxia (decreased oxygen content in tissues) and the damaging effect of certain neurotransmitters, in particular the excitatory neurotransmitter glutamate, that develop during birth trauma.
Postnatal lesion
This group mainly includes:
- mesial temporal (temporal) sclerosis and hippocampal sclerosis, which account for more than 50%;
- tumor of the temporal lobe of the brain;
- neuroinfection, meningitis, encephalitis, encephalomyelitis after vaccination;
- traumatic brain injury and/or brain surgery;
- cerebral infarction, strokes, hyperglycemic and uremic conditions;
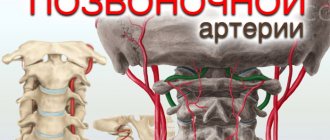
- vascular malformations (vascular development disorders) of various types;
- tuberous sclerosis (genetically determined disease) and some others - about 7%.
A topical and not completely resolved by modern science is the question of the relationship between the development of temporal lobe epilepsy and prolonged febrile convulsions. They are tonic-clonic or tonic convulsions in the extremities, which can occur in the form of seizures at febrile temperature (37.8-38.5°) in children of infancy, early and preschool age. Febrile seizures are considered to be a high risk factor for subsequent transformation to temporal lobe epilepsy.
It is assumed that the mechanism of development of the latter in this case, especially in the presence of atypical and very prolonged attacks of febrile seizures, consists of hypoxic, ischemic and metabolic changes in the temporal lobe of the brain, leading to the development of temporal mediobasal sclerosis and, accordingly, the disease in question.
The widespread use of surgical treatment methods stimulated the emergence of the so-called concept of the presence of functional zones in the cerebral cortex, which takes into account the possible origin of the disease. When considering the causes and mechanisms of development of pathology and in accordance with this concept, 5 zones are identified:
- Epileptogenic lesion.
- Epileptogenic focus, which refers to a zone of the cerebral cortex that has the ability to independently generate neural discharges of excessive severity.
- Irritations.
- Symptomatogenic, which is precisely the area of the cerebral cortex, upon irritation of which clinical manifestations of an attack occur.
- The attack began.
The classification of pathology is based on criteria such as the origin of the disease and the nature of the seizures, that is, etiopathogenetic principles. In accordance with these criteria, the following forms were previously distinguished:
- by etiology - idiopathic and symptomatic;
- according to the semiotics of seizures - primary and secondary generalized epilepsy, that is, neuronal discharges arising in different areas or in one area of the brain, quickly covering networks of neurons located in both hemispheres of the brain, and focal temporal lobe epilepsy (limited to a network of neurons in one hemisphere, that is, one hemisphere ) in both adults and children.
This division, including the term “focal,” has lost its relevance. However, these terms are acceptable for use in relation to the nature of the attacks, but not in relation to the forms of the disease.
Currently, it is relevant to divide the disease in accordance with etiopathogenetic principles into:
- symptomatic;
- idiopathic;
- cryptogenic.
How does symptomatic temporal lobe epilepsy differ from structural, or structural-metabolic?
The first is a form of pathology in which the examination reveals an epileptogenic focus localized directly in the temporal lobe of the brain. The most common cause of the symptomatic form is medial, or mesial, temporal sclerosis, that is, sclerotic damage to the medial structures represented by the hippocampus and ammon's horn.
Structural temporal lobe epilepsy cannot differ from symptomatic epilepsy, since this concept does not denote the form of the pathological condition, but a structural, morphological characteristic. In other words, these two concepts do not contradict each other, but only complement each other. In addition, structural changes in brain tissue can be located in other areas of the cerebral cortex (most often in the occipital region), from where a pulse discharge can irradiate to the temporal region and determine the corresponding clinical picture of this zone.
The reasons leading to structural disorders can be genetically determined or acquired. That is, traumatic brain injury, vascular disorders, inflammatory processes and brain tumors, hippocampal sclerosis, etc., causing disruption of certain brain structures, are the acquired cause of the disease.
Idiopathic, or primary, epilepsy usually has a genetic cause and is characterized by the absence of structural changes in brain tissue.
In cases where, after all examination methods, it is not possible to find out the cause of the disease, a diagnosis of “cryptogenic temporal lobe epilepsy” is established.
It should be noted that these forms are very rarely found in “pure” form. Most forms of this pathology are caused by a combination of genetic causes and external damaging factors.
Symptoms and signs of idiopathic epilepsy
The idiopathic form of epilepsy is characterized by the absence of any pathological changes in the brain with a clear external manifestation. The following typical syndromes are distinguished:
- absence seizures;
- myoclonic phenomena;
- classic seizures.
The above syndromes can be combined with each other, or they can manifest themselves separately.
The main manifestations of the disease are:
- Seizures of various kinds;
- Loss of consciousness;
- Convulsions of general and local significance;
- Lack of response to the environment;
- Visual impairment;
- Urge to vomit.
Diagnosis
1. Primary diagnosis of the disease is carried out using an EEG - this will help to identify the focus of the disease, the characteristics of the waves and changes in state between attacks.
2. To confirm the diagnosis, CT or magnetic resonance imaging is performed.
3. To exclude neoplasms of any form, positron emission tomography is performed.
4. They try to identify the root cause in order to start therapy based on it.
5. Decipher the blood test for karyotype.
6. The newborn is prescribed observation by a neurologist and epileptologist.
Below we will discuss in more detail the symptoms of the disease depending on the forms of manifestation.
Features of development and causes of occurrence
Focal epilepsy unites all forms of epileptic paroxysm, which occurs against the background of increased epi-activity in limited structures of the brain. The development of idiopathic focal epilepsy can occur with the involvement of surrounding brain tissue in the pathological process, which causes the appearance of secondary generalization of the attack. Epilepsy often accompanies cerebral palsy (CP).
Such paroxysm of focal epilepsy is distinguished from generalized epilepsy, which has a primary diffuse nature. There is also a multifocal type of epilepsy, which is characterized by the appearance of several local zones in separate areas of the brain.
Looking at the statistics, we can conclude that a similar disruption of brain cells, that is, focal type epilepsy, is diagnosed in 80% of cases among all forms of the disease. Most of them occur in childhood. As for the possibility of entering the army with such a diagnosis, young men are removed from service, excluded from military service and given a military ID.
The main causes of structural changes are organ injury, infectious or ischemic brain damage. Among the etiological factors:
- congenital malformation of the brain, which is localized in a clearly limited area and occurs as focal cortical dysplasia in a newborn, congenital cerebral cyst in an infant, arteriovenous malformation of an organ, manifested in a child in infancy;
- history of traumatic brain injury (in childhood or throughout life in an adult);
- infectious damage to the brain with the formation of an abscess, the development of encephalitis, cysticercosis, neurosyphilis;
- disruption of the functioning of blood vessels in an organ, for example, after a hemorrhagic stroke, with metabolic encephalopathy, or a tumor-like neoplasm.
There are symptomatic focal epilepsy, idiopathic and cryptogenic. With the symptomatic type, in all cases it is possible to determine the cause and characteristics of morphological changes. The latter are easy to see during a tomographic examination of the organ. Cryptogenic epilepsy has a secondary etiology; in this case, it is impossible to identify morphological changes by neuroimaging.
The development of idiopathic focal epilepsy occurs in the absence of any changes in the central nervous system that contribute to the development of pathology. The etiology of the disease is associated with genetic channel- and membranopathy, a disorder of maturation of the cerebral cortex. In all cases, idiopathic pathology is benign in nature.
After the death of neurons, gliosis develops in the brain - a process caused by the replacement of dead neurons with other cells with the formation of a kind of scar, which is based on glial elements. The latter protect tissues that remain healthy.
Clinical picture
Partial epileptic paroxysms are the main symptom of focal epilepsy. Neurologists divide them into two types: simple, not leading to loss of consciousness, and complex, associated with it. Depending on the clinical manifestations, simple paroxysms can be motor, sensory, hallucinatory, somatosensory, vegetative, and have a mental component. A complex variant of an attack can begin with single simple paroxysms with the gradual addition of disturbances of consciousness. After the end of an epileptic seizure, the patient is poorly oriented in the environment, time and his own personality, and there is inhibition of reactions.
An important feature of FE is the possibility of various types of paroxysms occurring in the patient, i.e., epileptogenic foci can form in any zone of the cerebral cortex. Focal seizures may become generalized when moving to neighboring areas of the brain. In this case, the primary simple or complex paroxysm leads to the appearance of tonic-clonic seizures, characteristic of a classic epileptic seizure.
Due to the fact that in the symptomatic form of the pathology there is organic damage to the central nervous system, the patient is noted for its clinical manifestations. For example, with a stroke in the area of the precentral gyrus, paresis and paralysis of the limbs of varying degrees of severity develop. In addition, cognitive impairment is characteristic: memory impairment, decreased ability to concentrate, changes in intelligence, etc. If partial focal epilepsy occurs in childhood, the child lags behind his peers in psychomotor development. In the case of an idiopathic disorder, intellectual and mental disorders do not occur, which characterizes a favorable prognosis for the patient.
Damage to individual areas of the cerebral cortex is characterized by various symptoms:
- In focal temporal lobe epilepsy, sensorimotor paroxysms are observed. In this case, there is an aura of a seizure in the form of a temporary disruption of the sensory organs, a feeling of anxiety and motor automatisms. In children, speech automatisms predominantly occur, and in adults, they are associated with gestures. The attack lasts up to one minute. This type of focal disorder is the most common.
- When the epileptic focus is localized in the occipital lobe of the brain, visual impairments come to the fore: its temporary absence, the appearance of illusions, loss of individual fields of vision, etc. Visual hallucinations of varying duration may occur.
- When an epi-focus occurs in the frontal lobe, the aura of the attack does not develop. The patient develops complex motor movements in the form of motor automatisms, as well as emotional disorders, manifested by shouting out individual words and remarks. General psychomotor agitation is noted.
- A pathological focus in the parietal zones is rarely detected. Most often, focal parietal epilepsy is associated with impaired development of the cerebral cortex, or with the growth of tumors of the nervous tissue. The main manifestation is simple independent paroxysms, characterized by unpleasant sensations in various organs and parts of the body.
The patient needs a comprehensive diagnosis aimed at identifying the original cause of changes in the brain.
Development of pathology
Secondary, or symptomatic focal epilepsy occurs against the background of diseases of the central nervous system. Most often it is caused by traumatic brain injuries, encephalitis of viral and bacterial causes, congenital disorders of the structure of brain tissue, post-stroke changes, metabolic damage to the central nervous system and neoplasms. There are studies proving the role of congenital or acquired disorders of neuronal metabolism, leading to the appearance of epileptogenic foci.
The structure of the causes of the development of FE attacks in children has a number of differences. The main factors are intrauterine damage to the central nervous system as a result of hypoxia, intracranial birth trauma and intrauterine infections. Epi-seizures in childhood may reflect immaturity of the cerebral cortex. In these cases, the symptoms of the disease go away on their own as the child grows up.
The development of symptoms is based on an epileptogenic focus, consisting of neurons with a low threshold of excitability. This causes their active excitation under the influence of minimal irritating factors. In addition to the area of hyperexcitability, an area of functional deficit is identified in the cerebral cortex, which is associated with concomitant neurological disorders during an attack.
Features of treatment
The success of treatment of the focal form of the disease depends on the timeliness of therapy. The specialist prescribes antiepileptic drugs. To reduce the intensity of attacks, the patient is recommended to take anticonvulsants. The choice of medication and dosage depend on the patient’s age, location of brain damage and the causes of the pathology.
In the absence of positive dynamics, surgical treatment is performed. During therapy, the patient is prescribed a special diet and daily routine. With early diagnosis and proper treatment, the prognosis for children is positive. The final disappearance of attacks is observed in a third of patients.
In the idiopathic form, there is sometimes a spontaneous cessation of attacks upon reaching adolescence. The prognosis for symptomatic focal epilepsy depends on the location of the lesion.
Disease with established etiology
Symptomatic focal epilepsy includes frontal, temporal, occipital and parietal. The severity and manifestations of symptoms will depend on the disruption of various structural parts of the brain. When the frontal lobe is damaged, problems with speech and coordination of cognitive, emotional and volitional processes are recorded; there is a violation of the patient's individuality. The temporal lobe is responsible for speech understanding and auditory processing, complex memory, and emotional balance; if it is damaged, these functions will be impaired. The parietal lobe regulates the sense of body position in space and movement, therefore the occurrence of seizures and paresis is associated with the localization of the lesion in this zone. And if there is an epileptoid focus in the occipital lobe, there will be problems with processing visual information (hallucinations, pareidolia) and coordination of movements.
However, it cannot be said that any type of focal epilepsy will have certain symptoms and no others. This is due to the spread of pathological impulses beyond the affected area.
Pediatric generalized epilepsy
Generalized epilepsy in children is predominantly idiopathic in nature. At the same time, in this category of patients, various factors can provoke epileptic seizures, including:
- allergic reactions;
- helminthic infestations;
- elevated body temperature and other childhood diseases.
Idiopathic epilepsy with generalized convulsive seizures in childhood occurs mainly in the form of absence seizures, which are characterized by temporary shutdown (but not loss) of consciousness. The presence of symptomatic epilepsy in children may be indicated by:
- regular visits to everything;
- sudden attacks of fear;
- unexpected mood changes;
- causeless pain in various parts of the body.
In medical practice, it is customary to distinguish two syndromes characteristic of epilepsy in children:
- West syndrome;
- Lennox-Gastaut syndrome.
The first syndrome is more often detected in infants. It is characterized by muscle spasms that cause uncontrollable nodding. West syndrome mainly develops with organic brain damage. In this regard, the prognosis for the development of the disease is unfavorable.
Lennox-Gastaut syndrome first manifests itself after two years and is a complication of the previous one. The pathological deviation causes atypical absence seizures, which over time can cause a generalized attack of epilepsy. With Lennox-Gastaut syndrome, dementia develops very quickly and there is a lack of coordination of movements. The disease in this form is not amenable to drug treatment due to complications that arise, which lead to changes in the patient’s personality.
Causes
The causes of attacks of symptomatic epilepsy include various diseases and pathological conditions:
- infectious and inflammatory diseases of the brain (abscess, encephalitis, meningitis):
- congenital brain anomalies, dysgenesis, atriovenous malformations;
- consequences of intrauterine hypoxia or birth trauma;
- traumatic brain injuries;
- rheumatism of the nervous system;
- hereditary metabolic diseases;
- intoxication, including severe childhood infections (scarlet fever, chickenpox, mumps, measles, rubella, infectious mononucleosis);
- neoplasms (benign or malignant) of the brain;
- pathology of the liver, kidneys;
- diabetes;
- acute cerebral circulatory disorders, consequences of stroke;
- multiple sclerosis.
The pathology develops as a result of circulatory disorders, injury and oxygen starvation of the brain. The following reasons lead to the development of pathology in childhood:
- heredity;
- intrauterine hypoxia;
- infectious damage to the fetus;
- brain tumors;
- prematurity;
- cyst or intracranial hematoma;
- congenital pathology (for example, Down's disease);
- head injury;
- brain damage by bilirubin in severe neonatal jaundice;
- infectious diseases of the meninges;
- disturbance in brain development.
Classification and forms
Idiopathic epilepsy is divided into two large groups:
- Localized . Seizures occur in one clearly defined area of the brain. Divided by:
- benign childhood epilepsy;
- primary reading epilepsy;
- epilepsy localized in the occipital region.
- Idiopathic generalized epilepsy . With this type of pathology, all cells of the cerebral cortex suffer. Includes:
- absence syndrome;
- generalized seizures upon awakening;
- photosensitivity;
- common benign seizures.