An ovarian cyst is a benign tumor, which is a cavity in which secretions accumulate. As the amount of content increases, so does the education. It is often diagnosed in women of childbearing age. In menopause, the detection rate is lower - only 6% out of 100
It differs from cystic-solid formations in that the latter contain not only fluid, but also parts of tissue. A solid formation has a dense shell and contains tissue inside. At the same time, it is important to know what you can and cannot do.
What are ovarian cysts?
An ovarian cyst is a round-shaped formation filled with liquid contents and characterized by a benign course in most cases.
It tends to increase in size and accumulate more secretions. Cystic formations are capable of spontaneous disappearance. It can occur at absolutely any age, even in newborns, but mainly affects girls of childbearing age (up to 90% of cases); in women over 50 years of age it occurs in 5 - 7% of cases. It occurs twice as often in women with irregular menstrual cycles. In order not to miss this pathology, it is necessary to examine the ovaries at least 2 times a year.
Treatment of paraovarian cyst
It forms in the area of the ligaments connecting the ovaries and the uterus. The formation in question is not prone to malignancy. Paraovarian ovarian cyst is organic - its treatment is carried out only surgically. If the size of the formation does not exceed 3 cm, surgical treatment is not required.
Indications for the operation are:
- Increase in size of the formation.
- Inflammation, rupture, torsion of the cyst.
- Feeling of discomfort.
- Preparing for pregnancy (any ovarian cyst is a potential threat of premature termination).
Sometimes this cyst is discovered directly during pregnancy, then surgical intervention has to be postponed. Small formations do not have a negative effect on gestation. Read more about ovarian cysts during pregnancy →
Types of ovarian cysts
The following types are distinguished:
- follicular (70 - 73% of cases);
- endometrioid (10%);
- corpus luteum cysts (5%);
- theca lutein (2%);
- paraovarian (periovarian) (8 - 10%), etc.
Follicular and corpus luteum cysts can go away without medical intervention.
They can also be single or multiple, unilateral or bilateral, complicated and uncomplicated.
Follicular cyst
First of all, it is necessary to say what ovulation is. This is the process of release of the egg (female reproductive cells) from the ovary into the abdominal cavity, due to the rupture of the dominant (main) mature follicle - the place of maturation of the egg. Due to a number of factors (early onset of menstruation before age 11, various menstrual cycle disorders, etc.), the preovulatory follicle does not rupture, its growth continues and a cyst is formed. They are observed more often in reproductive age, rarely in postmenopause (the period after the complete end of “menstruation”).
The cyst is a thin-walled formation consisting of 2 - 3 layers of follicular epithelium (specific tissue) containing a transparent light yellow liquid. On top it is covered with dense connective tissue. A sign of the transition of a normal follicle into a pathological cyst is an increase in fluid formation to 30 mm or more. Growth continues up to a maximum of 10 cm in diameter.
More often, they do not manifest themselves clinically; occasionally pain in the lower abdomen and menstrual irregularities may occur.
Endometrioid cysts
Endometriosis is a disease in which cells from the lining of the uterus spread beyond the uterus. Such heterotopias (altered ovarian sites) reach the ovaries and undergo changes during the menstrual cycle with the formation of cysts of various sizes. But endometriotic tissue can spread to other organs:
- intestines;
- bladder;
- ureters;
- other pelvic organs.
For a long time, cysts are asymptomatic. From time to time, you may experience discomfort during sexual intercourse and nagging pain in the abdomen.
Corpus luteum cyst
This type occurs at the site of an already burst follicle due to the accumulation of fluid. Sometimes they may contain blood and such cysts are called hemorrhagic. The volume of such a cyst is usually small and can reach four to six centimeters. It is believed that these cysts are formed when blood or lymph circulation in the corpus luteum is impaired. Available from 16 to 45 years old.
There are no specific manifestations; occasionally, when a cystic formation forms, minor abdominal pain is noted. The most common complication is hemorrhage into the cyst cavity. It can be strong and lead to the picture of an “acute” abdomen (pathologically tense and overly painful).
Paraovarian cyst
This is a tumor-like formation located between the leaves of the broad ligament of the uterus, formed from the ovarian appendages (periovarian, vesicular appendages). Most often occur between the ages of 20 and 40 years. Sizes vary from a couple of cm to gigantic ones, capable of occupying the entire abdominal cavity. They are located on the side or just above the uterus. Their wall is thin up to 2 mm, transparent, with a pronounced vascular network (similar to the blood supply in malignant tumors). The contents of the cyst are watery fluid. They do not manifest themselves clinically, but as they grow, pain and an increase in the abdomen in size and menstrual irregularities are possible. Paraovarian cysts do not resolve on their own.
Dermoid cyst
This is a benign formation measuring up to 15 cm in diameter. It is most often localized on the right side (you can palpate it yourself). The contents of the cyst can be:
- adipose tissue;
- teeth;
- hair;
- nerve tissue;
- bone.
Occurs at any age. Puberty and abdominal trauma are provoking factors. A dermoid cyst is formed due to the entry of residual embryonic tissue into the ovarian structures. As the formation grows, nagging pain in the lower abdomen is characteristic.
Thecal lutein cyst
Such cysts are formed as a result of a very rare disease in pregnant girls - hydatidiform mole. Formed due to excessive stimulation by hormonal drugs. Cysts are usually multiple, located symmetrically on both sides. The best prevention of the disease is childbirth, but medical manipulations, on the contrary, worsen the course of the pathology.
Other causes of cysts
Ramollic benign formations develop against the background of organ necrosis. The site of damage is overgrown with connective tissue, which in the future will become the wall of the tumor. Enzymes soften dead tissue and gradually turn it into liquid. Most often, cysts of this type appear in the brain (for example, after a stroke) or with osteoblastoma.
It is not uncommon for one cyst to grow inside another. This usually occurs inside the glandular tissue, due to its structure. Adenoma and other cysts of secretory organs provoke the onset of growth of a second tumor. Trauma can also cause the formation of a tumor. The epithelial layer is damaged, and a cyst forms at the site of damage.
Seven reasons for the formation of ovarian cysts
The following reasons are distinguished:
- Previous abortions, “pill” abortions. The formation of cysts after these interventions accounts for 30 - 35% of cases due to the formation of hormonal disorders and inflammatory phenomena.
- Poor functioning of the ovaries. When it occurs, follicle maturation is disrupted.
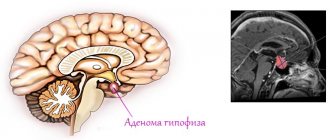
- Diseases of the pituitary gland (adenoma or other tumors, injuries), thyroid gland. Hormonal imbalance occurs.
- Diabetes mellitus, obesity. In these diseases, the synthesis of hormones is disrupted.
- Smoking. It causes vasospasm and, as a result, disruption of the blood supply to the ovaries.
- Chronic inflammatory diseases of the female genital organs (adnexitis, sexually transmitted infections, etc.).
- Endometriosis. Cells from the inner layer of the uterus are thrown into the ovaries and undergo changes during the menstrual cycle to form cysts.
Previously cured ovarian cysts can recur, so it is necessary to see a gynecologist at least 2 times a year.
Treatment of dermoid cyst
The second name of the pathology is ovarian teratoma. A dermoid formation is a cavity filled with various tissues of the body. Most often the contents are hair, fat, bone and cartilage tissue. There are no medications to treat this type of ovarian cyst. Progesterone therapy is ineffective. The only way to get rid of the formation is through surgery.
Clinical picture
If you have this pathology, symptoms such as:
- feeling of fullness in the lower abdomen;
- aching pain in the same area, especially with the growth of a cystic formation;
- discomfort and pain during sexual intercourse;
- menstruation occurs later or earlier than expected (irregular);
- pain during menstruation;
- frequent urination;
- nausea or, less commonly, vomiting.
Symptoms that require immediate medical attention
The occurrence of these symptoms is a reason for an immediate visit to a specialist:
- sharp pain in the lower abdomen;
- abdomen that is pathologically tense when palpated (“wooden”);
- an unconditional rise in temperature;
- menstrual irregularities;
- the appearance of facial hair or deepening of the voice in the fairer sex;
- the presence of asymmetry of the abdomen, an increase in its volume, especially one-sided;
- palpation of a tumor-like formation on the anterior abdominal wall;
- pain when urinating.
Corpus luteum cyst
Functional cyst of the right ovary - what is it? This formation is often also called a corpus luteum cyst. All due to the fact that it consists of exactly that. Such a cyst forms in the second phase of the menstrual cycle. It often appears during pregnancy. After ovulation, a woman’s ovary forms the so-called corpus luteum. It maintains sufficient levels of progesterone and promotes the development of pregnancy if it occurs. Normally, the size of the corpus luteum does not exceed two centimeters. If the diameter of the formation is slightly larger, then experts are already talking about a cyst.
This tumor does not require treatment. Only in some cases the patient is prescribed oral contraceptives for a course of 3-6 months. These drugs include “Janine”, “Logest”, “Novinet”, “Tri Regol” and many others. These compounds correct the cycle and promote ovarian rest. It is worth noting that such correction products are not suitable for patients planning pregnancy.
Consequences of ovarian cysts
Ovarian cysts are complicated quite rarely. The reason may be untimely examination by a gynecologist and late treatment. The following complications are possible:
- twisting of the pedicle of an ovarian cyst. The more pronounced the torsion, the more severe the pain in the lower abdomen. With a torsion of 90 degrees (incomplete), a gradual increase in the clinical picture is noted. When complete, there is a sharp disruption of the blood supply to the ovarian cyst with its necrosis (necrosis) and the development of a picture of peritonitis (inflammation of the peritoneal layers) - vomiting occurs, body temperature rises, severe abdominal pain, positive Shchetkin-Blumberg symptoms (irritation of the peritoneum). Urgent hospitalization is required;
- rupture of the cyst capsule. The pain is acute, symptoms of internal bleeding appear - weakness, dizziness, decreased blood pressure, sticky cold sweat, pain radiating to the right shoulder, fainting, and with severe blood loss - shock. There is pain during vaginal examination in the pouch of Douglas - the posterior vault of the vagina due to the accumulation of blood in it. A rupture can be provoked by sudden lifting of weights, jumping, bending, aggressive sexual intercourse, etc.;
- suppuration of the cyst. Accompanied by a clinical picture of intoxication syndrome - increased temperature to high values, pain in the lower abdomen, general weakness, malaise, tachycardia (rapid heartbeat);
- malignancy is the transition of a benign cyst to a malignant form (cancerous degeneration). The endometrioid cyst is most prone to this.
In addition, I would like to note that cystic ovarian formations adversely affect attempts to get pregnant or the course of pregnancy itself. It affects the physiological development of the fetus and can rarely cause miscarriage. It is extremely rare that if a woman has not undergone a preliminary examination before pregnancy, the presence of a cyst and its constant growth can disrupt the blood supply to the walls of the uterus, which may become an indication for termination of pregnancy.
Symptoms of the disease
The clinical picture of the presence of cysts in the ovary appears at a late stage of their growth and formation. Before this, the woman does not experience any unpleasant sensations.
If the patient has the following symptoms , then you should immediately consult a doctor :
- Pain in the lower abdomen. This may be caused by torsion of the cyst stalk or its rupture. Most often this happens after sexual intercourse.
- The belly is getting bigger and this has nothing to do with food consumption or pregnancy.
- Pain in different parts of the pelvis is a sign that a large tumor is pressing on the organs adjacent to it.
- Violation of the cyclicity of menstruation. In severe cases, it may stop completely.
- A woman cannot get pregnant. Blood appears from the vagina, and this has nothing to do with menstruation, since it is secreted in small quantities for 10-15 days
- The woman feels sick, even to the point of vomiting.
Diagnostics
The following diagnostic measures are carried out:
- gynecological examination. Allows you to identify pain in the lower abdomen and an increase in the size of the appendages. This is the initial procedure for suspected ovarian cysts;
- ultrasound examination of the ovaries, especially the transvaginal method. A very informative method that allows you to visualize a round formation of varying echogenicity with the presence of fluid inside;
- CT scan. Allows you to differentiate a cyst from other tumor neoplasms;
- puncture of the pouch of Douglas or, in other words, the posterior vaginal vault. This procedure is used if there is a suspected accumulation of blood or other fluids in the abdominal cavity. Puncture is especially valuable in the presence of complications - capsule rupture, bleeding;
- diagnostic laparoscopy. It is performed under general anesthesia and allows not only to diagnose a cystic formation, but also to remove it if necessary;
- general blood analysis. Allows you to identify the inflammatory process or the presence of infection (increased leukocytes, erythrocyte sedimentation rate, shift of the leukocyte formula to the left), allows you to assess the degree of blood loss (hematocrit - the number of red blood cells, decreased hemoglobin);
- A general urine test also allows you to determine the presence of infection (increase in leukocytes);
- pregnancy test. Important for differential diagnosis of ectopic pregnancy. It shows absolutely any presence of pregnancy in a woman.
The symptoms of ovarian cysts are also similar to diseases such as:
- acute appendicitis;
- intestinal diseases (Crohn's disease, ulcerative colitis, enteritis and others);
- ectopic pregnancy;
- malignant neoplasms;
- inflammatory diseases of the pelvic organs (adnexitis, etc.).
Postoperative period
Treatment after removal of an ovarian cyst in uncomplicated cases is not required. However, during the postoperative period, the patient still remains under the supervision of the attending physician. If there is a suspicion of a possible relapse, hormonal pills are prescribed. In addition, immunomodulators and vitamin complexes are used.
After surgery, heavy physical activity and bad habits should be avoided. If the intervention is performed laparoscopically, the sutures are removed after a week.
Treatment of ovarian cysts
The choice of treatment method will depend on:
- severity of symptoms;
- the age of the patient (preservation of the reproductive system depends);
- the likelihood of transition to a malignant form;
- size and structure of the diagnosed formation.
Conservative treatment
If a cyst of the corpus luteum or follicular type is detected, a wait-and-see approach is followed. These cysts are capable of self-resorption. It is possible to prescribe vitamin complexes (B1, B6, C, A), mono- or biphasic oral contraceptives (Jess, Lindinet, Rigevidon, etc.). A herbal preparation such as Civilin helps in resolving cysts. It is possible to use traditional methods of treatment, acupuncture.
Surgical treatment of cysts
If there is no positive dynamics, then surgical treatment is resorted to. It is carried out in the following ways:
- laparoscopic cyst removal. It is done through small punctures in the anterior abdominal wall. It is characterized by minor trauma and fairly rapid rehabilitation after the intervention;
- laparotomy removal - through a wide incision along the anterior wall of the abdomen. It is carried out if the malignant nature of the neoplasm is proven, with a very large size of the tumor, in women with severe obesity.
Scope of operation
- cystectomy - removal of a cyst within healthy ovarian tissue;
- oophorectomy - the essence of the operation is the complete removal of the ovary, often along with the fallopian tube;
- wedge resection is the removal of a cystic formation and adjacent tissue.
After treatment, the cyst tissue should be sent for histological examination (to exclude the malignancy of the process).
ethnoscience
Traditional methods of treatment do not lead to the complete disappearance of cysts. The following remedies are more effective:
- dandelion root decoction. Grind the root, pour boiling water, leave for about 15 minutes. Take a third of a glass 2 times a day for 5 days before each menstruation;
- decoction from boron uterus. Pour a teaspoon of chopped herbs into a glass of boiling water, leave for one day, strain. Drink a third of a glass three times a day an hour before meals for one week. The course can be repeated at the onset of the next menstruation. This medicinal herb contains natural phytoestrogens, bioflavonoids, arbutin, saponins and other beneficial substances.
Propolis, infusions of red brush, wintergreen, burdock juice and others are also widely used.
Treatment of a functional cyst
The principles of combating functional cysts are built on several successive stages.
Among them:
- Waiting tactics. The attending physician monitors the patient without prescribing medications. This is explained by the fact that functional formations are prone to self-resorption.
- Drug treatment. In cases where a functional ovarian cyst does not disappear on its own, oral contraceptives are prescribed (for example, Zhanin, Yarina). They are necessary for regulating the menstrual cycle. Treatment of functional ovarian cysts with hormones is considered the main method of combating this pathology.
- Surgical intervention. If the functional ovarian cyst is large and does not disappear, treatment is carried out surgically. This does not happen often and is a necessary measure to prevent or eliminate dangerous complications.
Mucinous and serous tumor
Less common than those described above are serous and mucinous ovarian cysts. What it is? Photos of some new growths are presented to your attention. Mucinous and serous cysts contain liquid mucous contents. Sometimes the tumor may appear as uneven contours. This often causes difficulties in diagnosis.
Treatment of such cysts is most often surgical. If they do not cause the woman discomfort and do not pose any danger, then doctors may recommend a wait-and-see approach.