What types of rectal fistulas are there?
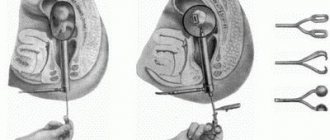
There are 3 varieties:
- Transsphincteric.
- Intrasphincteric.
- Extrasphincteric.
Additionally, a division is made into complete, incomplete, simple and complex fistulas. They differ in the number of passages, inlets and branches.
At CELT you can get a consultation with a proctologist.
- Initial consultation – 2,700
- Repeated consultation – 1,800
Make an appointment
Depending on the category of complexity - 106,000 - 140,000 rubles.
Included in the price:
surgery, anesthesia, dressings, medications, food and hospital stay
30-40 minutes
(duration of procedure)
2-3 days in hospital
Indications
The only indication for surgical intervention is the complete lack of results with conservative treatment. Often patients cannot get rid of the pathology for several years. The fistula closes and opens, which is accompanied by pain due to the inflammatory process.
Contraindications
A contraindication to surgery is a rehabilitation period of less than 8 months after treatment of acute paraproctitis. The development of a fistula and the growth of scar tissue must not be allowed, so you need to regularly see a proctologist (otherwise it will complicate surgical intervention). It is not recommended to perform surgery if you are intolerant to anti-inflammatory drugs, local and spinal anesthesia.
The structure of the fistula
External fistulas always have two mouths: external and internal, which are connected to each other by a channel. Sometimes the channel may be missing. In this case, the wall of the organ is adjacent to the skin, or even protrudes above it.
Granulating fistulas are covered with granulation tissue. They are pathological because they are formed against the background of inflammatory processes. The mechanism of their development is as follows:
- The inflammatory focus is delimited from the surrounding tissues, after which it breaks out.
- Due to the breakthrough that has occurred, a channel is formed through which the pathological contents exit.
- Over time, the canal becomes covered with granulation tissue, and connective scar tissue forms around it. The walls of the fistula become motionless and thicken.
What prevents such a fistula from healing is that some kind of discharge is constantly passing through it. If it has a chemically active formula, it will destroy granulations and promote the penetration of toxins and microbes into adjacent tissues. As a result, scars will form around the fistula. In addition, suppuration of fistulas is fraught with the fact that abscesses and new phlegmons can form other fistulas that open in nearby tissues. If the pathological contents stop passing through the fistula canal, then it can heal on its own.
Epithelized fistulas are those fistulas whose canal walls are covered with epithelium. When the epithelium of the mucous membrane of an internal organ passes to the skin, such fistulas are called labiform. Fistulas received this name because their wall protrudes above the skin and resembles a human lip in appearance. Most often, such fistulas are formed artificially. Epithelized fistulas cannot heal on their own.
As for the discharge that comes out of the fistula cavity, it depends on which organ the fistula is connected to. The more aggressive this exudate, the more damaged the skin around the fistula will be. For example, with intestinal fistulas, the skin very quickly corrodes and becomes covered with ulcers.
Fistulas are dangerous because they can lead to disruptions in the functioning of the body. In addition, they form against the background of an inflammatory process, which means their development is accompanied by intoxication and loss of fluid. All the same intestinal fistulas cause an outflow of digestive fluid. In the future, this leads to disruption of the water-salt balance and metabolic failures.
If pathological changes in the body are very pronounced, then there is a risk of death of the patient.
Diagnostics
The following methods are used to diagnose the disease:
- Examination by a proctologist. Digital examination of the rectum, probing of the fistulous tract, dye test.
- Anoscopy.
- Sigmoidoscopy (for diagnosing concomitant diseases of the rectum and sigmoid colon).
- Colonoscopy (to clarify the diagnosis and exclude inflammatory bowel diseases).
- Ultrasound transrectal examination (to clarify the location of the fistula tract, identify leaks and cavities).
- Computer and magnetic resonance imaging of the pelvic and perineal organs.
Modern diagnostic equipment at the CELT clinic allows for a full examination and determination of the position of the fistula.
What are the tactics in the presence of a rectal fistula?
During defecation, damaged soft tissues become infected with pathogenic bacteria contained in feces. This regularly causes exacerbations and makes the pathology chronic. Over time, a person cannot work normally and be in a team because the pads cannot completely contain pus and feces. This causes an unpleasant odor and discomfort. Additionally, immunity decreases, which in the fair sex can provoke the progression of colpitis.
As the pathology develops, scar tissue grows in the sphincter area, which causes incontinence of gases and feces. During an exacerbation, body temperature rises and symptoms of intoxication appear.
The disease does not go away over time, but only gets worse. In the last stages, the development of a malignant tumor is possible. Therefore, there is only one way to get rid of the pathology - to remove the affected tissue and prevent the growth of bacteria and the inflammatory process.
How do the forms of the disease differ?
Complete and incomplete fistula are two forms of the same pathology. Its first type is distinguished by the fact that the fistula has two holes. One is located on the surface of the skin next to the anus. The other is located in the anal crypt. An incomplete fistula has one hole, it is located inside, on the mucous surface. If the fistula is internal, in the full form of the pathology the fistula has two openings, but both of them will be located in the wall of the rectum. Medical specialists consider the incomplete form of the disease as one of the stages of the formation of a complete fistula, because the fistula is able to affect the surrounding tissues and “punch” a second hole.
The pathology can acquire a transsphincteric character. Such fistulas are considered one of the most common; they are located above the anus and have a branched shape. Transsphincteric fistulas are accompanied by tissue scarring and the formation of ulcers. Intrasphincteric fistula occurs much less frequently - in approximately 30% of patients diagnosed with fistulas. Most often they are called subcutaneous mucous membranes. Fistulas of this type are not characterized by a long-term inflammatory process. The fistula canal in this form of pathology is smooth. If the fistula is complete, its opening will be located close to the anus.
Types of operations
For transsphincteric and intrasphincteric fistulas, the purulent part is opened and completely cleaned. A gauze swab soaked in medicinal ointment is inserted into the wound. At the end of the procedure, the surgeon inserts a gas tube into the colon.
Removal of extrasphincteric fistulas takes longer because they have a lot of branches and are longer. Surgeons use the ligature method. Excision is performed and a thread is inserted into the internal zone, which passes out through the fistula. Next, the ligature is tightly tightened along the front, middle or back of the anus.
Minimally invasive methods show high effectiveness for simple fistulas. This is laser burning, the introduction of a therapeutic biotransplant or fibrin glue.
Preparing for fistula removal surgery
Before surgery the following is carried out:
- Computed tomography of the pelvic organs.
- X-ray examination of the fistula with a contrast agent.
- Sigmoidoscopy.
- ECG.
- Fluorography.
- Biochemical and general examination of blood and urine.
- Consultation with a therapist, proctologist and gynecologist.
- Culture of fistula secretions to test antibiotic sensitivity.
In the presence of chronic diseases, improvement must be achieved in order to normalize the functioning of the cardiovascular and respiratory systems. Additionally, the specialist prescribes rinsing with antiseptic agents and taking antibiotics after sowing purulent fistulous secretions.
For 3 days before the procedure, you should not consume foods that increase gas formation. In the evening and morning before the operation, an enema is performed to deep cleanse the intestines (in case of difficulties, laxatives are prescribed). Hair in the perineal area must be removed.
Information for patients. Perirectal fistula
If you find the symptoms and signs described above, you or your loved ones should contact a coloproctologist for help in diagnosing and properly treating the disease. In the absence of proper treatment and diagnosis, the consequences can be extremely serious for your health.
8-918-55-44-698
A telephone number for contacting specialists at the medical center, where they will try to provide you with the necessary assistance in selecting the right specialist and provide up-to-date contact information.
Surgical treatment of rectal fistulas
Treatment of rectal fistulas is carried out only by surgical methods. Healing cannot occur on its own or under the influence of medications.
Treatment is usually prescribed during an exacerbation, since the fistula is detected quite easily along its entire length. The surgeon opens the abscess and washes it with antiseptic solutions. The patient is prescribed antibiotics. After this, the fistula is removed. This is done in various ways, depending on the location and length of the fistula tract. Treatment is carried out in a hospital.
Symptoms
- A wound forms in the anal area
- blood is released, ichor from the hole, unpleasant odor
- painful redness and irritation of the skin
- seals form with the release of pus along the fistula
- unstable general condition of the patient: poor sleep, irritability
- urination and stool problems
Complete fistula tracts can be seen during a routine examination, and can be felt during hygiene procedures - this is a visible seal in the anus. A different clinical picture is expressed in the following manifestations:
- discomfort and itching in the anus due to skin irritation;
- discharge from the rectal canal (blood, mucus, purulent-bloody exudate);
- violation of defecation, urination;
- fever, general malaise, pain, aggravated by defecation.
Patients complain of abdominal pain of unknown etiology, there is weight loss while maintaining appetite, disturbances in stool consistency and functions of the gastrointestinal tract. In men, libido decreases and the quality of sexual life deteriorates.
It is easy to determine the presence of a fistula by observing the symptoms and signs of its appearance. The patient usually feels pain during bowel movements. Itching, maceration, burning, and irritation around the anus appear. If there is an external hole, due to lack of drainage, infiltrate and exudate are released, which causes additional pain to the patient.
However, you should not diagnose a fistula inside the rectum on your own. Differential diagnosis is carried out by a doctor using various methods:
- Examination and questioning of the patient.
- Palpation of internal tissues, revealing deformation in the rectal area.
- Probe research necessary to determine the direction of the passage and its depth.
- Ultrasonography – ultrasound of the digestive system.
- Taking a sample with a dye in order to determine the type of fistula - complete or incomplete.
- Sigmoidoscopy, which helps determine the presence of tumors, cracks, and nodes.
- Fistulography or irrigoscopy is an X-ray examination performed using a barium enema. Immediately after the enema is administered, an x-ray photo is taken.
- Sphincterometry is an instrumental examination that determines the quality of functioning of the sphincter organs.
- Gynecological examination in women if the fistula exit is in the cervix.
The symptoms of paraproctitis are not difficult to recognize; they are pronounced.
The main symptoms of fistulas:
- On the skin of the gluteal region, you can visually determine the opening of the fistula.
- From the external fistula opening and anus, minor discharge appears in the form of pus, blood, and feces.
- Near the external opening, the fistula tract can be easily palpated; it is defined as an elastic, dense cord.
- There are nagging pains in the area of the fistula and rectum, which greatly intensify during defecation, their intensity directly depends on the stage of the disease; When the disease worsens, the pain may become regular and be accompanied by a rise in temperature.
Perirectal fistula has pronounced symptoms. The clinical picture of this pathology is characterized by alternating stages of exacerbation/remission and wave-like symptoms.
Perirectal fistula, depending on the stage, can manifest itself with the following symptoms:
- the appearance of a wound in the perianal area, which is a fistulous tract;
- rectal discharge (purulent, serous-purulent, sanguineous), noticeable on panties;
- the appearance of unpleasant odor discharge;
- hyperemia of the skin surrounding the anus, itching, burning;
- dull pain in the rectal area;
- a significant increase in pain during exacerbation (formation of ulcers in the perirectal tissue) - in the pelvis, rectum, lower abdomen (when coughing, walking, defecation);
- disruption of the process of urination and bowel movements;
- increased body temperature;
- the appearance of signs of intoxication;
- headaches;
- weakness, decreased motor activity.
After opening the fistula, a period of remission begins, but the wound does not heal, since the inflammation is not relieved. Exudate continues to form and leak, which leads to disruption of the patient's sleep, loss of performance, sexual dysfunction and psychological problems.
Despite the severe symptoms, often patients, feeling shy, are in no hurry to seek medical help from a proctologist, self-medicating. However, you need to understand that for patients diagnosed with perirectal fistula, treatment without surgery will not bring absolutely any results, since only surgical intervention can provide complete relief from this problem.
Postoperative period
For 2 weeks, the patient spends time in the hospital with strict adherence to bed rest. Antibiotics are taken to prevent the spread of infection. You should avoid bowel movements for at least 5 days. Specialists slow down peristalsis with a special diet and medications. Dressing is carried out after 3 days. Tampons soaked in medicinal ointment and hydrogen peroxide are inserted. Anesthesia is performed first. If bowel movement does not occur after 5 days, an enema is performed.
It is important to strictly follow the diet throughout the entire period of rehabilitation. It is allowed to consume clean water, boiled vegetables, omelettes, semolina porridge without adding milk. You should not eat fruits and vegetables raw, or drink alcoholic beverages. After defecation, the colon is treated with chlorhexidine. The sutures are removed by the surgeon after a week. Tissue regeneration can take a maximum of 21 days. It is recommended to perform therapeutic exercises to avoid weakening of the anal muscles and incontinence.
Possible complications
- Injuries to the urethra.
- Reappearance of the fistula.
- Accumulation of pus in the surgical area.
- Heavy bleeding during and after surgery.
- Weakening of the anal muscles and incontinence.
The incidence of complications with correct excision of the fistula in the hospital is less than 10%.
Why do patients choose CELT for the treatment of rectal fistula?
- There are more than 100 different surgical interventions for the treatment of rectal fistulas. The CELT clinic employs proctologists with extensive experience who are proficient in all types of operations for rectal fistulas.
- The clinic guarantees not only high-quality treatment and anesthesia, but also a comfortable, pain-free stay in the postoperative period.
- After the operation, the patient remains in the hospital for an average of 2-3 days. The patient is observed in the clinic until complete recovery.
Reviews and conclusions
Patient B.: “About a year ago, pain appeared in the anus and the temperature rose. The pain was severe enough that I could not sit. But he didn’t go to the doctor, he treated himself - suppositories for hemorrhoids, chamomile baths, painkillers. A week later the abscess opened, a lot of pus came out, I felt better, I was happy.
About a month later I began to notice that my perineum was constantly wet, there was discharge on my underwear, and an unpleasant odor. I waited another two months, hoping that everything would go away on its own. In the end I decided to see a doctor. A rectal fistula was diagnosed.
For a long time he did not agree to the operation; he was treated with various folk remedies. However, there was no effect; pain began to appear periodically.
The operation took about an hour. A few days in the hospital, then I did the dressings myself at home, it’s not difficult. After 10 days, practically nothing bothered me.”
The bulk of rectal fistulas are a consequence of untreated acute paraproctitis.
Rectal fistula is not a fatal disease. You can live with it, but the quality of life is significantly reduced.