Cervical dysplasia is a disease associated with changes in the epithelial tissue of the mucous lining the cervix. Unlike cervical erosion, this pathology is rare, mainly in women of childbearing age (from 25 to 40 years).
Experts consider dysplasia as a precancerous condition and recommend not delaying treatment of the disease until a later date. The diagnosis is made depending on how extensive the epithelial changes are. Timely treatment of dysplasia is the surest prevention of cervical cancer, which is very common today.
Classification of the disease
A classification system for cervical dysplasia was developed to facilitate diagnosis. In its development, the disease goes through three main stages, each of which requires special treatment. The more advanced the dysplasia, the higher the risk of developing cancer.
Cervical dysplasia of the 1st degree (CIN1) affects individual cells of the mucosal epithelium, located, as a rule, in its uppermost layers, has no characteristic signs and is quite difficult to diagnose. The disease can be identified at an early stage of its development by resorting to screening.
Cervical dysplasia grade 2 (CIN2) involves the spread of the process of cell change to the deeper layers of the mucosa. There are also no external signs of the disease.
Cervical dysplasia of the 3rd degree (CIN3) is characterized by strong and extensive changes in the structure of the epithelium of the uterine mucosa, affecting the deepest layer of the mucosa - the basal one, an actual precancerous condition. Sometimes, at this stage of the development of the disease, carcinoma in the city is already diagnosed (a local tumor that has not yet spread in the body).
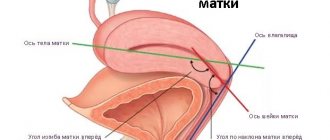
Dysplasia can affect various parts of the mucous membrane of the cervix, in particular it can be found on its outer part, in the canal connecting the vagina and uterus, and in the area adjacent to the uterus itself.
YOU WOULD BE INTERESTED
Ureaplasma in women
Severity of dysplasia
In medical practice, the classification of dysplasia, which is carried out according to degrees, is considered widespread.
- Weak degree.
- Moderate.
- Pronounced or severe.
- Atypical hyperplasia.
The criterion for determining the degree is the intensity of the atypical process in epithelial cells.
As the severity increases, changes develop:
- Increase in the size of the cell nucleus of epithelial cells.
- Polymorphism of nuclei and the entire epithelial cell.
- Hyperchromatism when staining preparations.
- Changes in the structure of chromatin, which forms rough clumps.
- Increase in the number of cell nucleoli and their size
- Activation of mitosis.
The course of epithelial dysplasia can be progressive, stable or regressive. Dynamic transformations in the structure of cells directly depend on the duration of the pathological process and the degree of intensity.
The mildest degree of epithelial dysplasia often has a favorable prognosis and is subject to reverse regression in 100% of cases. The higher the degree of activity of the pathological process, the greater the percentage of likelihood of cancerous degeneration of cells. The appearance of cancer in situ can be considered as an extreme degree of development of dysplasia.
Symptoms of dysplasia
In itself, the presence of pathological processes in the uterine mucosa does not manifest itself in any way, but it is often associated with various infectious diseases of the genital area (STIs), which have pronounced symptoms. Many women with a similar diagnosis also have cervicitis (inflammatory process of the cervical canal), HPV, and trichomoniasis.
Suspicion of cervical dysplasia should arise if the following symptoms are present:
- rare nagging pain in the lower abdomen;
- bloody vaginal discharge not associated with menstruation;
- itching in the vaginal area;
- discomfort, pain during sexual intercourse;
- copious discharge with an unpleasant odor.
These symptoms are characteristic of many diseases of the female reproductive system, including those associated with cervical dysplasia. In the absence of concomitant diseases, dysplasia does not manifest itself in any way and can only be detected during a medical examination of the patient.
A specialist may notice changes in the mucosa characteristic of dysplasia even during examination. The mucous membrane affected by the disease becomes red, loose, spots of various diameters and colors (most often light pink), minor ulcerations, and erosions may be observed on it.
Prevention
The main preventive measure is to avoid infection with the human papillomavirus; to do this, it is enough to use condoms every time you have sexual intercourse and avoid casual relationships. It is also important to remove provoking factors:
- stop smoking;
- maintain immunity at the proper level;
- monitor your partner’s health;
- treat diseases in a timely manner, especially gynecological diseases;
- avoid stress;
- monitor the correct diet.
Treatment of dysplasia
To determine the disease, it is necessary to conduct a number of studies, in particular:
- colposcopy, which allows not only to see structural changes in the mucous membrane, but also to take tissue for further study in the laboratory;
- a biopsy, during which a small fragment of the changed mucosa is taken. Next, this fragment is subject to cytological examination to detect the presence of cancer cells;
- examination of the cervix by a gynecologist.
Most women with suspected dysplasia are recommended to be tested for STIs, since the main cause of the development of this disease is considered to be a fairly common infection - HPV. PCR gives the most accurate result.
The question of how to treat cervical dysplasia is answered by gynecologists and gynecological oncologists. Therapy is prescribed taking into account the degree of development of the disease and the cause of its occurrence. There are many causes of the disease. Atypical processes in the mucous membrane can be triggered by pregnancy, difficult childbirth, any surgical interventions in the woman’s genital area, as well as smoking and low immunity.
YOU WOULD BE INTERESTED
Conization of the cervix
Treatment of the initial stage of the disease is carried out using conservative methods. The patient is prescribed immunostimulating drugs and vitamins. A woman with a similar diagnosis, regardless of age, should be under the supervision of a specialist and undergo regular examinations (every 3 months). There are cases of spontaneous cure of cervical dysplasia.
In cases where the likelihood of developing cancer is high, more radical treatment methods are used, in particular cauterization of dysplasia. If there is a high risk of cervical cancer, the altered area of the mucosa is simply removed. The procedure is carried out using a laser, liquid nitrogen, and a radio knife. If the initial stage of cancer is detected, amputation of the cervix is recommended, while the uterus itself remains intact and fully performs its functions.
Causes
The main reason leading to the development of cervical dysplasia is a special papillomavirus that attacks humans.
There are more than 80 types of infection, but only 30 of them lead to diseases of the cervix or other genital organs. 13 types of HPV have a high risk of cancer, and when infected with virus 16 or 18, cancer develops in more than 80% of cases.
Not in all cases, infection with papillomavirus leads to cancer. For epithelial dysplasia to occur, which then develops into cancer, provoking factors are needed:
- the woman has parity, that is, a history of multiple births;
- long-term use of hormonal drugs as protection against unwanted pregnancy. When taking tablet forms of contraceptives for five years, the risk of atypical changes in the cervix doubles;
- the presence of cancerous changes in the partner’s penis;
- sharp hormonal surges - pregnancy, use of postcoital contraception, menopause;
- tobacco use – even passive smoking increases the risk of developing neoplasia;
- hypovitaminosis – the most dangerous is a lack of vitamins A and C;
- decrease in the body's defenses - AIDS, taking immunosuppressants, stress conditions, depletion of the immune system due to diffuse infections;
- the presence of infections in the genital tract, chronic inflammation.
Predisposing factors also include early pregnancies (before age 18), injuries during abortion or childbirth, and sexual activity that began at a young age. In addition, heredity plays a big role.
The cause of the development of epithelial cell dysplasia may be one or more provoking factors. As a rule, a combination of several negative phenomena leads to its occurrence.
Possible causes include the following:
- Hormonal imbalance in the body.
- Genetic predisposition.
- Inflammatory processes.
- Infectious diseases.
- Damage to the epithelium of organs.
- Failure of metabolic processes in the body.
- Living in an area with poor environmental conditions.
One cannot discount a person’s lifestyle. A lot depends on him too. The likelihood of developing the disease increases if you drink alcohol, smoke, exercise little, or eat unhealthy foods.
Dysplasia develops in several stages. The following forms are distinguished:
- Weak.
- Moderate.
- Heavy.
They differ from each other in the extent of the lesion, manifested by symptoms. Mild dysplasia of squamous epithelium can rarely be detected, because it does not bother patients with unpleasant symptoms. At the middle stage, symptoms begin to appear, but they are not too pronounced, so many do not pay attention to them. In severe cases, it is almost impossible not to notice the disease.
Based on the type of affected cells, doctors distinguish dysplasia of glandular epithelium and dysplasia of squamous epithelial cells. The first type is observed most often in women, because such tissues line the genitals. But they are also present in the digestive tract. The second type can often be found in the lungs.
A natural question arises: why, after infection with the papilloma virus - and according to various sources, up to 95% of the world's population are its carriers - only a few of them will encounter the disease? What factors enable the virus to emerge from its “dormant” state and begin active division?
1. Stress. Emotional experiences reduce immunity, and even strong positive emotions are stressful for the body.
2. Pseudo-erosion (ectopia) of the cervix is a physiological feature of the body, which nevertheless creates favorable conditions for infection with a large amount of virus. Young women with unestablished stable relationships with the opposite sex are most susceptible to this risk.
3. Inflammatory diseases (colpitis, cervicitis). The endometrium of the vagina and cervix performs the function of the skin - it protects against infections. Inflammatory diseases not only reduce its barrier ability, but they are a favorable condition for the progression of the virus. Therefore, women with frequent inflammation are at risk for developing dysplasia.
4. Smoking. Nicotine itself is one of the most powerful carcinogens, and its concentration in the mucus of the cervical canal is often much higher than in the blood. The second factor in the carcinogenic effect of cigarettes is tar. They radically change the properties of vaginal mucus and cervical plug, weaken local immunity and make the epithelium extremely vulnerable to HPV and other infections.
5. Heredity. Genetic predisposition to the development of atypical processes, which can often occur even without the participation of HPV. You need to be especially attentive to yourself if your direct relatives are diagnosed with cervical dysplasia or cervical cancer.
6. HPV of high oncogenic risk. These serotypes increase the risk of developing dysplasia because they are better adapted than other viruses to protect against suppression by the immune system.
Conization of the cervix with dysplasia
The procedure of conization of the cervix is a radical treatment method. Among its main indications are grade 2 and 3 dysplasia. During conization, the altered area of the mucous membrane is completely removed, while the adjacent tissues remain intact and unharmed.
This method of treatment is not used if a malignant tumor of the cervix is detected. Conization is also contraindicated in the presence of an STI. In such a case, the infection is first treated with antibiotics, then the dysplasia is removed.
Conization of the cervix with a scalpel is considered an outdated method of treatment. Today, the procedure is carried out using more gentle methods (laser and radio wave conization). In the first case, the area of tissue being removed is exposed to a laser beam that completely burns out the atypical tissue; in the second case, a high-frequency current is applied, under the influence of which the cells of the mucous membrane literally evaporate.
The operation is performed in a hospital setting. After its completion, the patient remains in a medical facility for 3-4 days and is subject to medical supervision. In the first few hours after the procedure, she may be bothered by nagging pain and slight bleeding from the vagina. The result of treatment is assessed 2-3 weeks after the operation.
YOU WOULD BE INTERESTED
Endometriosis of the uterus
Conization of the cervix is performed under local anesthesia; complications are rare. If the procedure is carried out correctly, a slight scar remains on the mucous membrane, which is not a subsequent obstacle to the birth of a child.
Severe dysplasia
Severe dysplasia is commonly called intraepithelial neoplasia. The condition in clinical practice is regarded as obligately precancerous. Severe dysplasia can be considered the initial stage of pathomorphological changes, which gradually transform into a malignant neoplasm.
The histological picture of severe dysplasia shows many similarities with the morphology of cancer cells. A distinctive feature is the absence of invasion into adjacent tissues. This explains the need for emergency treatment and a number of preventive measures when signs of severe dysplasia are detected in a patient. Treatment of this stage is necessarily surgical and is radical in nature. The patient must be seen by an oncologist.
Cervical dysplasia and pregnancy
Dysplasia often occurs in pregnant women due to changes in the hormonal levels of their body. If the disease progresses slowly and is at an early stage of development, there is no particular need for treatment. In such cases, experts recommend waiting until the baby is born. Often after childbirth the disease progresses, so in such cases, medical supervision is simply necessary.
If a woman expecting a future pregnancy has been diagnosed with grade 2 or 3 dysplasia, treatment is carried out using the most gentle method (laser conization of the cervix).
You can also watch the video for more detailed information about cervical dysplasia.
How is dysplasia treated?
Many doctors agree that there is no need to treat mild dysplasia, you just need to carefully monitor the condition of the patient’s reproductive system to prevent the disease from worsening.
More advanced cases necessarily require therapy; surgery is usually required only for non-invasive cancer; moderate neoplasia is treated conservatively.
In gynecology, dysplasia can only be treated with medications when the pathology was detected at the very beginning of its development. Several groups of drugs are used for this:
- immunomodulators – increase the body’s resistance, resistance to infections, help fight HPV (Isoprinosine, Prodigiosan);
- antiviral – drugs aimed at destroying the papillomavirus;
- hormones - restore the normal structure of epithelial cells; oral contraceptives are usually used, which contain varying concentrations of estrogen and progesterone;
- anti-inflammatory drugs – neoplasia is always accompanied by inflammation, which is important to remove for a successful recovery.
Vitamin complexes are also prescribed, which necessarily contain increased concentrations of ascorbic acid and carotene.
When neoplasia is accompanied by a bacterial infection, antibiotics and probiotics are used. The former fight the infection itself, while the latter restore the intestinal microflora after taking antibacterial agents.
The use of medications does not always give a positive result, so in certain cases it is necessary to resort to surgical removal of cervical dysplasia.
Indications for switching to more effective methods are non-invasive cancer and lack of response to medications taken for more than six months.
Pathological tissues are destroyed under the influence of high frequency electric current, and healthy cells are formed in their place.
The laser is aimed at the diseased area and it dries out the abnormal cells, evaporating the fluid from them. As a result, they are destroyed, giving way to healthy counterparts.
The method is similar to diathermocoagulation, but tissue necrosis occurs under the influence of cold rather than current.
Radio waves, like a laser, cause the cellular fluid to evaporate and the epithelium to necrotize.
If the above methods are ineffective, the woman is offered surgery. It can be of two types - excision of altered tissues or complete removal of the neck.
We invite you to familiarize yourself with Diazolin: what it helps with, instructions for use
The second option is recommended for patients who have given birth and who do not plan to have children in the future. Young girls are trying to preserve their reproductive function.
After surgery, certain prohibitions are imposed - for several months you cannot have sex, lift heavy things, and in addition, it is advisable to avoid physical activity.
Folk remedies
Treatment of cervical dysplasia with folk remedies is possible only in combination with traditional therapy. You can take tinctures or decoctions from plants that increase immunity, stabilize hormonal levels, and fight inflammation. The use of tampons is also popular.
Celandine is often used in the fight against neoplasia. Tampons or douching are used with a decoction or oil from its flowers; taking the flower internally is contraindicated.
Products based on boron uterus can help restore women's health. The plant has antitumor, analgesic and antiseptic effects. In addition, it is able to normalize the patient’s hormonal levels, causing the sex glands to work more actively.
Diagnostic procedures
Cervical dysplasia has symptoms, which in most cases are erased, and requires considerable physical and material costs to confirm the diagnosis.
Examination of the cervix in speculums
A routine examination that is performed on all women who contact a gynecologist with complaints or for a routine examination. In this case, the eye evaluates the appearance of the cervix, the condition of the mucous membrane, color, relief, presence and consistency of discharge. During the examination, all necessary tests are taken.
An examination is not enough to make a diagnosis! The histological conclusion obtained after studying a scraping of the mucous membrane of the cervical canal and biopsy material from the cervix is of decisive importance.
Cytological examination of a smear (Papanicolaou smear (PAP test))
The most accessible type of research available, which allows you to examine a large number of women in a relatively short time. Using a cytobrush or an Eyre spatula, epithelial cells are scraped from the surface of the cervix and from the cervical canal (after careful removal of mucus and secretions). Next, the collected material is distributed onto a glass slide, which is sent to the cytology laboratory, where, after a series of mandatory procedures (drying, fixation, special staining), cytologists examine the scraping under a microscope. Cytological examination of the PAP test in solution is becoming increasingly popular. The material is collected with a cytobrush, which is immediately immersed in a special solution and in this form is transported to the laboratory, where a smear is prepared using a special technology. The method is considered more informative, but is more expensive and is not yet performed in all medical institutions.
A woman should prepare to go to an antenatal clinic. In order for the tests to be as informative as possible, you should abstain from sexual contact, douching, the use of suppositories, vaginal creams, and tampons two days before going to see a specialist. A smear is not taken during menstruation or during inflammatory processes.
Extended colposcopy
Colposcopy is the study of the structure of the cervix using optical instruments (microscope). Extended colposcopy, unlike conventional colposcopy, is performed using chemical solutions that specifically stain areas of altered epithelium. The most commonly used test is acetic acid and Schiller's test (2% Lugol's solution).
Targeted cervical biopsy
Biopsy is a highly informative research method that involves taking a piece of tissue for further layer-by-layer examination. To obtain a reliable result, an area must be sampled at the border of healthy and diseased tissue. There are several methods for obtaining material, but the most preferred is the use of a scalpel or conchotome. Despite the relative pain and “bloody”, this is how it is possible to obtain the most informative areas. Some clinics offer painless, bloodless procedures for taking a biopsy using an electric loop, for example. But! Tissues exposed to heat are destroyed, simply boiled and charred, and it is simply impossible to obtain reliably informative material from such a sample, the exception being if a large piece is taken, inside of which “living” tissue remains. Therefore, before agreeing to such a procedure, a woman should weigh everything carefully and decide what is more important - a painless procedure or obtaining accurate results. Moreover, recently specialists have been performing vaginal manipulations at the woman’s request under local anesthesia.
A targeted biopsy is performed after an extended colposcopy, when the specialist knows exactly from which area the tissue needs to be obtained to obtain the most informative sections.
Curettage of the mucous membrane of the cervical canal
The procedure is performed in a hospital or antenatal clinic under local anesthesia. Necessary to clarify the prevalence of the pathological process. The resulting scraping is immersed in a special fixing solution and sent to the laboratory, where smears are prepared from it, which are further studied under a microscope.
Additional Research
The methods described above are quite sufficient to establish and confirm the diagnosis. However, the specialist who will treat the affected cervix will prescribe a number of examinations that will help choose the most effective and safe method of treatment. To clarify what triggered the development of the process, the following will be assigned:
- blood hormonogram (exclude hyperestrogenism and other hormonal disorders);
- immunogram (immunodeficiency states);
- blood test from a vein for HIV, syphilis, chlamydia, hepatitis;
- blood test to detect tumor markers;
- smears for diagnosing STIs, which will necessarily include a detailed analysis to detect HPV infection.
An OMT ultrasound is performed to exclude damage to the internal genital organs.
Treatment
When diagnosing cervical neoplasia, treatment methods are prescribed based on the identified degree of the disease. In the initial stages, drug therapy is used. But for grades 2 and 3, the doctor performs surgery.
Drug therapy
The drugs are prescribed as additional therapy, since neoplasia is most often treated with surgery. This is due to the fact that in the initial stages the disease does not show symptoms and is quite difficult to identify.
The objectives of drug therapy are:
- Increasing local and general immunity.
- Restoration of microflora - normalization of vaginal biocenosis.
- Treatment of hormonal imbalance.
- Antiviral therapy.
- STI therapy.
For the treatment of cervical neoplasia, interferon preparations and interferon inducers are prescribed. Prodigiozan, Interferon-alpha 2, Cycloferon, Groprinosin, Kagocel, Genferon and others are used. Considering the fact that HPV largely suppresses the production of its own interferon produced by leukocytes, the prescription of drugs is justified.
Among antiviral agents, Panavir is highly effective.
To normalize the vaginal flora, probiotic medications containing bifidobacteria and lactobacilli are prescribed.
STIs are treated with antibiotics depending on the microorganism isolated.
The intake of vitamin complexes (B vitamins, antioxidants) and omega acids is also indicated.
With the help of drugs, it is not possible to completely get rid of the disease in all cases. That is why most often specialists still prescribe surgical intervention. Before and after surgery, drug maintenance therapy is indicated.
Treatment of cervical neoplasia should be combined and long-term, affecting all aspects of the pathogenesis of the disease.
Surgery
The operation is prescribed in cases of 2 or 3 degrees of cervical dysplasia. Based on the individual characteristics of the body, the presence of contraindications, and the area of damage, the following methods of surgical intervention can be prescribed:
- Laser excision. The method is performed using a laser scalpel, through which the affected area is removed.
- Radio wave therapy. It is one of the new treatment methods. Removal of affected cells occurs when exposed to high-frequency radio waves. The procedure is performed with the Surgitron apparatus.
- Electroconization. Using a metal loop to which a current discharge is applied, a cone-shaped section of the cervix is excised, capturing healthy tissue. This technique is considered the most common in the surgical treatment of cervical neoplasia - it involves the complete removal of altered tissue. Conization can be performed using a laser method. This reduces the risk of bleeding. All procedures are performed after the end of menstruation.
- Photodynamic therapy. A modern method of treating pathological conditions of the cervix. The principle of operation is based on the selective accumulation of a photosensitizer by the neoplasm after administration. In tissue cells, singlet oxygen is released, which leads to the death of the altered cells.
- Diathermocoagulation and cryodestruction are used extremely rarely in the treatment of cervical neoplasia. The doctor cannot control the depth and volume of the impact, so the likelihood of relapse after the procedures is high. When excision of tissue, a mandatory histological examination is carried out, but when cauterized or frozen, this method is impossible. Traditionally, liquid nitrogen and cauterization are used to treat underlying pathologies, not precancerous ones.
After receiving the response from the histological analysis, the doctor decides on subsequent actions. If cancer cells are detected, additional surgical treatment, radiation therapy, and chemotherapy are possible.
Risk factors and groups
The main factor is HPV. Why is it activated?
The HPV virus itself can exist for a long time in the human body without causing any changes, and in 40% of cases, epithelial cells are able to independently eliminate it. In order for the pathogen to be activated, it needs certain conditions:
- hormonal imbalance (hyperestrogenism);
- general chronic diseases that deplete the body;
- infectious diseases of the genital tract;
- trauma to the cervical epithelium during diagnostic curettage, abortion, childbirth;
- promiscuity in sexual relations;
- smoking;
- early sexual debut;
- congenital and acquired immunodeficiency conditions.
Some sources contain information about an increased risk of developing cervical cancer in women using oral contraceptives. The question is debatable and there is no clear opinion.
At-risk groups
Based on the above, several risk groups can be identified. These are women:
- with menstrual irregularities;
- with a violation of fat metabolism;
- have undergone repeated medical intervention on the cervix;
- multiparous;
- leading a promiscuous sex life.
Methods for diagnosing cervical neoplasia
- Gynecological examination. The doctor sees changes in the color of the mucous membrane, on which light spots appear that can bleed on contact.
- Colposcopy is an examination of the mucous membrane using a colposcope equipped with optics and a light source. The device allows you to see the ectocervix under magnification so that the doctor can see even small precancerous lesions. Often, during the examination, other pathologies are revealed in a woman - erosions, polyps, condylomas.
- Extended colposcopy, during which the ectocervix is treated with special solutions. This allows you to better identify existing changes and determine the boundaries of pathological foci. The patient undergoes:
- Schiller's test, in which the surface of the ectocervix is lubricated with solutions containing iodine. Normal healthy tissue in this area contains glycogen, a substance that turns brown when reacted with iodine. Cells affected by neoplasia do not have glycogen, so they remain light.
- Vinegar test - under the influence of vinegar, the affected areas become white. This tissue is called acetowhite epithelium.
Colposcopy
Pathological changes are detected in the cervix:
- Punctuation - when performing an iodine test, red dots - small vessels - are revealed in the light area of neoplasia. Depending on the severity of dysplasia, punctuation can be weak (gentle) or pronounced (rough).
- Mosaic - under the influence of iodine and vinegar, a network of small vessels - capillaries - appears on the surface of the ectocervix, which merge, forming a kind of mosaic. In mild cases it can be gentle, and in severe cases it can be rough. With severe dysplasia, the mucosal surface becomes uneven, similar to cobblestones.
- Keratosis is the appearance of dense keratinized areas on the mucous membrane, which are an accumulation of dead cells.
- Internal boundaries - in this case, inside one pathological area another, also changed, is found. This is a sign of severe disease.
- The ridge is an opaque, ridge-like growth found at the exit of the cervical canal from the uterus. The growths most often appear in young women with severe precancer.
Improperly developed vessels, ulcerations, compactions, and ulcers may also be found on the surface of the cervix. Such lesions usually indicate severe dysplasia, which could have already turned into cancer.
- Taking a smear for Papanicolaou cytology. To do this, a smear is taken from the surface of the ectocervix and cervical canal. Samples are stained in the laboratory and examined under a microscope. Four criteria are studied by which one can suspect the onset of precancerous degeneration:
- Cellular - in the laboratory they study the shape of cells, their size, structure, and the structure of the chromatin protein that is part of them. With dysplasia, the shape and size of cells are changed, and the structure is disrupted.
- Functional - for this purpose, the cytoplasm is studied - the liquid part of the cell. With dysplasia, various unusual compounds and impurities are found in it.
- Structural - during the examination, the structure of the tissue itself, which changes during precancer, is assessed.
- Background – background inclusions are detected in the material, which should not be present in healthy tissue.
Cervical brush
If the material is taken correctly and modern laboratory methods and technologies are used, the effectiveness of the study reaches 96%.
There are several classifications of cervical neoplasia –
Papanicolaou, Bethesda, Dysplasia, CIN System, WHO (World Health Organization) classification. Based on their results, you can find out what exactly was found in a woman.