The health of the reproductive system is very important for a woman.
Only if there are no diseases of the genital organs and congenital anomalies can you easily conceive and bear a child.
Some diseases may be asymptomatic, and the woman wonders why she cannot get pregnant for a long time.
And sometimes the cause of infertility lies in pathologies, the symptoms of which do not bring noticeable discomfort and therefore remain unattended.
Adenomyosis of the uterus - what is it?
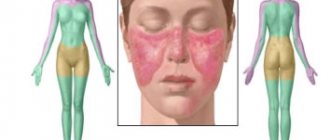
One of the common diseases of the female reproductive organs is uterine adenomyosis. In order to understand the essence of the disease, you need to remember the structure of this reproductive organ.
The uterus is a hollow organ, the inside is covered with endometrium, the outer layer consists of smooth muscle cells. Between them there is an intermediate submucosal layer of tissue.
During the menstrual cycle, the thickness of the endometrium changes due to the growth of its functional part facing the uterine cavity. In this way, the woman’s reproductive system prepares for the possible occurrence of pregnancy.
After the death of the egg, if conception does not occur, the endometrial mucosa is torn off and comes out along with bloody discharge during menstruation.
After menstruation, restoration and re-growth of the functional layer occurs due to endometrial growth cells.
But disorders occur in which endometrial cells can be thrown into a woman’s abdominal cavity, and even carried by blood to other organs, such as the lungs.
This disease is called endometriosis. Uterine adenomyosis is internal endometriosis, in which endometrial elements grow into the body of the uterus, its muscular layer. It is most often diagnosed in women over 30 years of age.
This disease is quite common, and a woman may not be aware of its presence. Adenomyosis is often asymptomatic, or manifests itself as painful periods or menstrual irregularities.
Meanwhile, a woman may unsuccessfully try to get pregnant, not understanding the reasons for her infertility.
And, although the direct connection of this disease and problems with pregnancy has not yet been proven, approximately half of women with infertility who turn to a gynecologist learn about the diagnosis of “adenomyosis of the uterine body.”
What is adenomyosis?
Adenomyosis is a disease of the uterus that can cause prolonged uterine bleeding, spotting in the middle of the cycle and severe pain in the lower abdomen.
Adenomyosis is said to occur when the endometrium, which normally should only be found in the uterine cavity, penetrates deep into the muscular layer of the uterus. Due to the fact that the endometrium begins to grow where it is not supposed to grow, an inflammatory reaction develops and the uterus increases in size.
Adenomyosis and endometriosis
Adenomyosis is sometimes called uterine endometriosis or internal endometriosis. Indeed, both adenomyosis and endometriosis develop for the same reason: if the endometrium begins to grow where it is not supposed to grow.
With endometriosis, endometrial foci can be found outside the uterus (on the ovaries, in the fallopian tubes, in the cervix, etc.) There is a separate article on our website dedicated to endometriosis.
It is not uncommon for the same woman to have both endometriosis and adenomyosis at the same time.
Why does adenomyosis appear?
The causes of adenomyosis are not known. There are several theories explaining the possible causes of this disease, but none of them is generally accepted yet.
It is known that sex hormones (estrogen, progesterone, prolactin, FSH) play an important role in the development of adenomyosis. When the level of sex hormones in the blood decreases (this happens in women during menopause), the symptoms of adenomyosis usually go away.
Who is at increased risk of adenomyosis?
Adenomyosis is a fairly common disease among middle-aged women who have given birth (over 35-40 years old). An increased risk of adenomyosis occurs:
- in women who have given birth (either independently or by caesarean section)
- in women who have had uterine surgery (for example, removal of uterine fibroids)
- in women over 35-40 years old
Forms of adenomyosis
Depending on how large the endometrial areas are in the muscular layer of the uterus, several forms of adenomyosis are distinguished:
- Focal adenomyosis: the endometrium forms separate islands, or foci of adenomyosis, in the muscular layer of the uterus. Focal adenomyosis is often asymptomatic or with mild symptoms.
- Nodular adenomyosis: The endometrium forms separate nodes in the muscular layer of the uterus. Endometrial nodes in the nodular form of adenomyosis are also called adenomyomas, since they are very similar to uterine fibroids.
- Diffuse adenomyosis: large areas of the endometrium almost uniformly grow throughout the entire muscular layer of the uterus.
Some women may have several forms of adenomyosis at once: for example, a combination of diffuse and nodular forms (diffuse nodular adenomyosis).
Degrees of adenomyosis
Depending on how deep the endometrium penetrates into the muscular layer of the uterus, there are 4 degrees of adenomyosis:
- 1st degree of adenomyosis: shallow penetration of the endometrium deep into the uterus. The endometrium is found only in the submucosal layer of the uterus.
- 2nd degree of adenomyosis: deeper penetration of the endometrium deep into the uterus: foci of adenomyosis are found in the muscular layer of the uterus, but affect no more than half of the muscular layer.
- Stage 3 adenomyosis: foci of endometriosis are found in the muscular layer of the uterus and affect more than 50% of its thickness
- 4th degree of adenomyosis: deep lesion. The endometrium grows into all layers of the uterus.
Symptoms and signs of adenomyosis
Sometimes adenomyosis can be asymptomatic and discovered only incidentally during an examination for another reason. But often with adenomyosis the following symptoms are observed:
- Long and heavy periods that last more than 7 days in a row. Often with adenomyosis, uterine bleeding may occur.
- Spotting brown (bloody) discharge in the middle of the cycle.
- During menstruation, blood is released in clots (lumps).
- Severe abdominal pain during menstruation or in the middle of the cycle. Pain with adenomyosis can be cramping or cutting.
- Pain in the lower abdomen during sex
With adenomyosis, the uterus can increase in size by 2-3 times. Because of this, some women manage to feel a round, dense formation in the lower abdomen (behind the pubic bone). This is an enlarged uterus.
Consequences of adenomyosis
Adenomyosis is not life-threatening and usually does not cause any serious complications. However, heavy bleeding from adenomyosis can provoke anemia, and severe abdominal pain worsens the quality of life and can lead to depressed mood, anxiety and depression.
Adenomyosis and pregnancy
Despite the fact that adenomyosis is often found in women suffering from infertility, a direct connection between this disease and the inability to conceive a child has not yet been established.
Some experts believe that the cause of infertility with adenomyosis is not adenomyosis itself, but the endometriosis that accompanies this disease. For information on how to get pregnant with endometriosis, read the article at the link.
If you have adenomyosis and are unable to get pregnant, you may need careful evaluation and then treatment. Read below about how to get pregnant with adenomyosis.
Diagnosis of adenomyosis
Contact your gynecologist if you have at least one of the symptoms of adenomyosis listed above. The gynecologist will perform a gynecological examination and determine whether there is a need for a more thorough examination.
The difficulty of diagnosing adenomyosis lies in the fact that there are no examination methods that would allow one to confidently make such a diagnosis. The only reliable method for diagnosing adenomyosis is removal of the uterus and subsequent examination of uterine tissue under a microscope (histological examination).
Of course, removal of the uterus is an unacceptable diagnostic method for many women, so alternative examination methods have been used to clarify the diagnosis: ultrasound, MRI, hysterosalpingography, sonohysterography, uterine biopsy.
These examinations allow you to find signs of adenomyosis and exclude other diseases with similar symptoms: uterine fibroids, uterine polyps, endometriosis, endometrial hyperplasia. Only if other possible diseases are excluded is a diagnosis of adenomyosis made.
Gynecological examination in a chair
Despite the fact that during a routine examination the gynecologist cannot notice foci of adenomyosis in the uterus, a gynecological examination is very important. First of all, the gynecologist will be able to determine the size of the uterus: with adenomyosis, the uterus increases in size by 2-3 times and takes on a spherical shape. Secondly, during the examination, the gynecologist will rule out other possible causes of bleeding or abdominal pain.
Ultrasound of the pelvic organs
Ultrasound is also not a definitive method for diagnosing adenomyosis, but this examination is very important, as it will exclude other possible diseases of the uterus or uterine appendages. The main signs (echo signs, echo picture) of adenomyosis on ultrasound are:
- an increase in the size of the uterus and a change in its shape
- the presence of hypoechoic inclusions in the muscular layer of the uterus (myometrium)
- heterogeneous structure of the myometrium
- the presence of small cysts (up to 5 mm in diameter) in the muscle layer of the uterus
- thickening of the walls of the uterus (thickening of the posterior wall of the uterus is especially common)
It is important to understand that no doctor can diagnose adenomyosis solely on the basis of pelvic ultrasound and general examination. Ultrasound only allows one to suspect the presence of adenomyosis.
MRI (magnetic resonance imaging)
MRI is a more expensive examination method that allows you to clarify the structure of the muscular layer of the uterus. The main signs of adenomyosis on MRI are thickening of the muscular layer of the uterus, heterogeneity of the myometrium and the presence of foci in it, which may be foci of the endometrium. MRI can also help rule out other possible uterine diseases.
Hysteroscopy
Hysteroscopy can be used to exclude other possible causes of uterine bleeding (uterine polyps, uterine fibroids, endometrial hyperplasia, malignant diseases of the uterus, etc.). During hysteroscopy, the doctor may take a piece of tissue for further examination under a microscope. The procedure for collecting material for research is called a biopsy, and studying the obtained material under a microscope is a histological study.
Hysterosalpingography (HSG) and sonohysterography
Hysterosalpingography and sonohysterography are also used to exclude other possible diseases of the uterus. In addition, if a woman has adenomyosis, then hysterosalpingography or sonohysterography can detect indirect signs of this disease. There is a separate article on our website dedicated to hysterosalpingography.
How is adenomyosis diagnosed?
Despite the fact that adenomyosis cannot be called a rare disease, doctors very often “miss” it or confuse it with other diseases that cause similar symptoms.
For example, uterine bleeding can occur both with adenomyosis and with submucosal uterine fibroids, uterine polyps, hormonal disorders, endometrial hyperplasia, malignant diseases of the uterus, etc. Abdominal pain during menstruation can occur not only with adenomyosis, but also with primary dysmenorrhea and endometriosis.
In this regard, many experts are of the opinion that to make a diagnosis of adenomyosis, it is necessary to exclude all other possible diseases with similar symptoms. If all examinations performed did not reveal other disorders, but did reveal indirect signs of adenomyosis, then the diagnosis of adenomyosis is considered confirmed. The final diagnosis can only be made by histological examination of the uterus after its removal.
Does adenomyosis need to be treated?
As mentioned above, adenomyosis does not threaten a woman’s life and, as a rule, does not cause any serious complications. In this regard, not all women require treatment for adenomyosis. You do not need treatment if:
- signs of adenomyosis were discovered by chance during an examination for another reason
- you have no symptoms of adenomyosis, or the symptoms are not pronounced and are tolerable
- the symptoms of adenomyosis do not cause significant inconvenience, you are over 45-50 years old and you are about to experience menopause
Is it possible to completely cure adenomyosis?
Unfortunately, there are no medications that can help get rid of adenomyosis. All medications used in treatment only help cope with the symptoms of adenomyosis, but do not eliminate the disease itself. The only guaranteed way to get rid of adenomyosis is to remove the uterus.
Treatment of adenomyosis
Treatment of adenomyosis depends on the symptoms that bother the woman.
- Painkillers in the treatment of adenomyosis
If, with adenomyosis, a woman often experiences severe pain in the lower abdomen, then non-steroidal anti-inflammatory drugs (NSAIDs) are prescribed: Ibuprofen, Ketoprofen, etc.
In order for them to really work, you need to start taking the pills even before your period appears (1-2 days before the expected date of menstruation and take one pill every 6 hours).
- Birth control pills in the treatment of adenomyosis
With adenomyosis, women often experience severe uterine bleeding, spotting in the middle of the cycle, and menstrual irregularities.
In order to regulate the menstrual cycle, the doctor may prescribe birth control pills (Zhanin, Yarina, etc.). Birth control pills do not cure adenomyosis, but sometimes help eliminate or reduce symptoms of adenomyosis such as severe uterine bleeding and abdominal pain during menstruation.
- Mirena intrauterine device for adenomyosis
The Mirena intrauterine device has proven effectiveness for adenomyosis, endometriosis and uterine fibroids. Mirena helps relieve abdominal pain during menstruation and reduce the amount of blood loss during menstruation. In some women, prolonged wearing of the Mirena coil leads to a complete cessation of menstruation, which has a beneficial effect on the course of adenomyosis.
However, Mirena will not be able to get rid of adenomyosis. After removal of the IUD, menstruation returns, as well as all the symptoms of adenomyosis.
- Utrozhestan and Duphaston in the treatment of adenomyosis
The drugs Utrozhestan and Duphaston are often used in the treatment of adenomyosis and endometriosis. During treatment with these drugs, periods become less abundant, and foci of adenomyosis may decrease in size. The course of treatment can last from 6 to 9 months.
- Analogs of gonadotropin-releasing hormones (Buserelin, Goserelin, Sinarel) in the treatment of adenomyosis
Buserelin, Goserelin (Zoladex), Sinarel and other drugs analogues of gonadotropin-releasing hormones are often prescribed for severe symptoms of adenomyosis and endometriosis.
While taking these medications, a woman stops menstruating, the ovaries temporarily stop working, and the level of sex hormones in the blood decreases. All these effects lead to the fact that endometrial lesions begin to decrease in size, and the symptoms of adenomyosis disappear or become less noticeable.
The duration of treatment of adenomyosis with these drugs is no more than 6 months, but after completion of the course of treatment, all symptoms of adenomyosis may return. In order to prolong the positive effect, after the end of treatment, the doctor may prescribe further use of birth control pills or the drug Visanne.
- Visanne in the treatment of adenomyosis
The drug Visanne contains the substance dienogest, which prevents the growth of endometrial lesions in the muscular layer of the uterus. This drug is prescribed not only for adenomyosis, but also for endometriosis.
It has been noted that in some women with adenomyosis, Visanne can cause severe uterine bleeding, so taking this medication is possible only after consultation with a gynecologist and under his close supervision.
Adenomyosis and menopause (menopause)
Often, adenomyosis can be detected in women at premenopausal age (several years before the expected onset of menopause or menopause): at 45-50 years.
If there are no symptoms of adenomyosis, or if they do not cause great inconvenience, no treatment is prescribed. For minor symptoms (irregular periods, abdominal pain), birth control pills or pain medications may be prescribed. If symptoms of adenomyosis impair quality of life, your doctor may recommend removal of the uterus.
Surgery (removal of the uterus) for adenomyosis
Removal of the uterus for adenomyosis is not always required. Surgery may be recommended in the following cases:
- if adenomyosis causes severe uterine bleeding that cannot be treated and leads to large blood loss
- if a woman already has children and does not plan to become pregnant in the future
- if a woman is premenopausal (over 45-50 years old) and is not against hysterectomy
- if adenomyosis is combined with large uterine fibroids
- if adenomyosis is combined with undesirable changes in the endometrium or cervix
You can read about how the operation goes, how to prepare for it and how to behave after the operation in separate articles on our website: Removal of the uterus (hysterectomy): before surgery and Removal of the uterus: after surgery, consequences.
How to get pregnant with adenomyosis?
It is believed that adenomyosis cannot cause infertility, so you have every chance of becoming pregnant with adenomyosis on your own, without treatment.
If you are unable to become pregnant for 12 months or more, you and your husband need to be tested. What examinations should a woman undergo:
- Ultrasound of the pelvic organs
- blood test for hormones
- hysterosalpingography (HSG) to assess tubal patency
- measuring your basal temperature for at least 3 consecutive months to determine if you are ovulating
What examinations should a man undergo:
- semen analysis (spermogram)
Depending on the examination results, the doctor prescribes treatment. For example, if obstruction of the fallopian tubes is detected, then laparoscopic surgery is prescribed to restore their patency. If a woman does not ovulate, treatment is prescribed to restore normal ovarian function, or courses to stimulate ovulation. If during the examinations concomitant diseases were discovered (uterine polyps, fibroids, etc.), then appropriate treatment is prescribed.
Types of uterine adenomyosis
Adenomyosis can develop in several forms, which differ in the nature of endometrial growth:
1 Diffuse adenomyosis of the uterus - proliferation of the inner layer is observed over large areas of the organ; individual foci and nodules are not detected during examination of the woman.
2 The nodular form of uterine adenomyosis is characterized by the appearance of nodules at the site where the endometrium grows into the muscle layer. For this reason, adenomyosis and uterine fibroids are often confused.
3 Focal adenomyosis of the uterus is characterized by penetration of the inner layer into the muscular layer in limited areas of the organ, which are called foci.
Interesting! Uterus: structure, changes during pregnancy and childbirth
Different forms of adenomyosis require different treatment methods, and the consequences of such a disease for a woman will also differ.
Methods for diagnosing adenomyosis
Adenomyosis on ultrasound is diagnosed by conducting a transabdominal and transvaginal examination. In the first case, an ultrasonic sensor is placed in the lower abdomen.
During a transvaginal examination, a woman is inserted into the vagina with a special elongated ultrasound probe. A condom is first placed on the equipment and lubricated with ultrasound gel. This method is more informative. After the procedure, unpleasant symptoms may appear in the vagina, which disappear after 1–2 hours.
Degrees of uterine adenomyosis
Gynecologists have developed several schemes that can be used to determine the degree of uterine adenomyosis.
The most commonly used system is:
1 With grade 1 adenomyosis of the uterus , the endometrium grows deep into the body of the uterus, but only into its submucosal layer or into the most superficial part of the muscle tissue.
2 With grade 2 adenomyosis, the germination of endometriotic tissue extends deep into the wall of the organ, the lesion covers up to half the thickness of the muscular layer of the uterus.
3 Adenomyosis grade 3 is characterized by damage to the uterine wall of more than half the thickness of the muscle layer, but it does not reach the outside of the organ.
4 Grade 4 adenomyosis affects all layers of the uterus, that is, endometrial cells penetrate between the smooth muscle fibers, causing deep damage to the organ.
The higher the degree of the disease, the more effort needs to be made to improve the situation.
Decoding the results
At the initial stage, adenomyosis is shown on ultrasound as a slightly enlarged uterus. An ultrasound sensor detects the porosity of small cystic formations in the walls of the uterine cavity up to 3 millimeters in diameter.
In this case, the structure of the inner layer of tissue, the myometrium, becomes rough and heterogeneous. Echogenicity, the ability of internal organs to reflect ultrasonic waves, is increased in this place.
A sonologist uses an ultrasound to detect adenomyosis of the uterus if the organ visually resembles a circle or ball in shape on the device screen. This is due to the enlargement of the uterus in front and behind due to cystic tumors. The ratio of the length and thickness of the uterine cavity changes to 1–1.1.
With the development of the 2nd and 3rd stages of the disease, the muscular walls of the reproductive organ atrophy towards the serous layer. In this case, diffuse damage to the uterus is diagnosed, which is characterized by changes on ultrasound:
- the thickness of the uterine walls becomes asymmetrical;
- the overall size increases;
- the echogenicity of the myometrium resembles a honeycomb;
- hyperechogenicity of the layers of the uterine cavity adjacent to the sensor, so it will be difficult for the doctor to view the lower wall of the organ;
- the uterine connective region thickens (more than 12 millimeters);
- the median M-echo appears linearly striated with an indistinct outline;
- a large number of linear stripes with medium and reduced echogenicity appear, which are located perpendicular to the scanning plane; the image appears on the screen in the form of a fan.
With nodular adenomyosis, round formations without a clear contour with increased hyperechogenicity (light areas) are visible in the uterus. This indicates the absence of a connecting capsule.
Video of an ultrasound of the uterus with nodular adenomyosis:
On ultrasound, the heterogeneous structure of the uterus appears as cystic anechoic or hypoechoic circular areas. Their diameter reaches 6 millimeters. The adenomatous wall of the uterine cavity may include several endometriotic nodes, inside of which a cyst grows.
Signs of uterine adenomyosis
Many women find out about the presence of this disease by chance, during routine examinations or visiting a gynecologist for other reasons. In other cases, with uterine adenomyosis, symptoms may be as follows:
1 Disorders of the menstrual cycle: shortening its duration with increased frequency of menstruation, increasing their duration and intensity, the appearance of spotting in the middle of the cycle.
2 Pain due to uterine adenomyosis can be quite severe, paroxysmal, cutting, and taking analgesics does not always bring relief. Painful sensations intensify during sexual intercourse.
3 In response to endometrial growth, smooth muscle cells begin to increase. Severe cases of adenomyosis lead to an enlargement of the uterus up to the size characteristic of 5-6 weeks of pregnancy.
The doctor may suspect this diagnosis during a routine gynecological examination of a woman, or notice echo signs of uterine adenomyosis during an ultrasound examination.
But ultrasound does not convey the full picture of the disease; hysteroscopy and MRI are more informative research methods.
Reviews
Thus, upon closer examination of the essence of the disease, we can say that cervical adenomyosis is not as harmless as it might seem at first glance. There is no doubt that the anomaly must be treated.
If you have personally encountered the problem described in this article, you can share your opinion below, in the “comments” section, and perhaps your story will be useful to someone.
If you find an error, please select a piece of text and press Ctrl+Enter.
Causes of uterine adenomyosis
Medicine has not yet found the answer to the question of why women develop adenomyosis.
But gynecologists are inclined to believe that the appearance of this disease is most often associated with various surgical interventions (abortion, caesarean section, various operations on the uterus), natural childbirth experienced or inflammatory processes in the walls of the organ.
Sometimes adenomyosis is diagnosed in young girls who have just started menstruating.
It is believed that this development of events may be associated with a narrow lumen of the cervix.
Menstrual discharge is retained in the cavity of the organ and negatively affects its inner lining.
Adenomyosis can also be congenital, when in girls, while still in the womb, endometrial cells occupy an atypical position and penetrate into the muscle layer.
Why is uterine adenomyosis dangerous?
This disease itself does not threaten a woman’s life, but can cause her discomfort due to menstrual irregularities or recurring pain.
If the disease is accompanied by heavy menstrual and even uterine bleeding, anemia may develop.
The main problem is a decrease in the chances of pregnancy with uterine adenomyosis.
Interesting! Delayed menstruation - causes and treatment
Symptoms
The specificity of the manifestations of the disease is that its main symptoms may be inherent in a number of other diagnoses of the female genital area, while the presence of two or more symptoms most likely indicates cervical adenomyosis:
- pain syndrome in the pelvic area and lower abdomen – the degree of intensity of sensations is different – pain is most severe in the nodular form of adenomyosis, especially at stages when the internal muscle layers are already quite deeply damaged.
If the area of the anomaly is closer to the anus, then the pain may shift to the rectum and coccygeal area;
- bleeding from the genital tract, not directly related to the menstrual cycle and discharge - this is a manifestation of the diffuse type of the disease. Almost always, after a short time it provokes anemia;
- the appearance of nonspecific discharge that occurs several days before the onset of menstruation – a very characteristic sign for this disease. The discharge is not too abundant, has a spotting structure, is dark, closer to brown, in color, with a sharp, unpleasant odor.
After the end of menstruation, the phenomenon repeats again. Such fragments of discharge are a product of the breakdown of pathological cells and are thus spontaneously excreted from the woman’s body;
- poor tolerance of menstrual symptoms - accompanied by depression, nervous breakdowns, excessive agitation, often bordering on aggression. This is explained by vegetative-vascular dystonia, which is a frequent companion to the pathology;
- chronic infertility is a hormonal imbalance caused by adenomyosis, which negatively affects the process of fertilization, inhibits it and provokes miscarriage.
Adenomyosis of the uterus - treatment
Women diagnosed with uterine adenomyosis should be aware of two main points. Firstly, this disease cannot be completely cured unless extreme measures are taken - removal of the uterus. But there is good news: when menopause occurs, adenomyosis disappears on its own.
Despite the impossibility of completely eliminating the disease during the childbearing period, its manifestations can be reduced. The answer to the question of how to treat uterine adenomyosis depends on the type and severity of the disease and the woman’s desire to have a child.
The medical treatment of adenomyosis involves the use of hormonal drugs, for example, oral contraceptives. A woman should be prepared to take medications for a long time, because the course of treatment can last for several months.
If the last stages of the disease are diagnosed, or the area of damage to the muscle layer is large, only surgical intervention will be effective.
When a woman no longer plans a pregnancy, the uterus can be removed for adenomyosis.
This is a radical solution, but it can eliminate unpleasant symptoms if they greatly affect the woman’s health.
In the case when a woman wants to give birth to a child in the future, the doctor turns to other methods of surgical intervention. At the moment, laparoscopy is a very effective technique.
It involves a minimal degree of intervention in the woman’s body, and only 3 small, unnoticeable seams remain on the body.
The patient's rehabilitation is faster and easier than with other types of surgery.
There are other, more complex methods of treating adenomyosis, for example, by changing the blood circulation of the uterus.
Only the attending physician, who takes into account all the individual characteristics of the woman’s body and the nuances of the course of the disease, can speak about the appropriateness of such treatment methods.
Adenomyosis of the uterus: treatment with folk remedies
Adenomyosis of the uterus cannot be cured with folk remedies, as well as with medications. However, some women use various medicinal herbs (nettle, knotweed, shepherd's purse, cinquefoil).
Another popular way to treat adenomyosis is blue clay compresses. The recipe calls for heating a mixture of clay and water, but the woman must remember that exposure to high temperatures can cause complications of genital diseases.
Therefore, the compress should never be hot.
A woman should treat adenomyosis with folk remedies with great caution. Before using any of the decoctions, compresses or other methods of alternative medicine, you should consult a doctor.
Diagnostics
To identify the disease and obtain the most complete clinical picture of the process, the following diagnostic methods are used:
- inspection – standard examination of the patient’s genitals using mirrors.
Additionally, a colposcope is used, a special device whose strong optics allows you to obtain a large-scale three-dimensional image of the desired part of the organ, determine its condition, and if pathological processes are suspected, refer the patient for a more in-depth examination;
- Ultrasound is the most accessible and common way to detect diseases of the pelvic organs and genitourinary system. Ultrasound clearly shows the size of the uterus, the presence of compactions and formations, their location and size;
- hysteroscopy is the most progressive diagnostic method. Provides an opportunity to study the cervical canal in detail. The hysteroscope is inserted into the organ - first into the cervix and then into the uterus. Shows the qualitative condition of the mucous surface, the structural content of the internal walls and takes a fragment of material for in-depth analysis to determine the nature of the anomaly.
Find out what causes of stomach cancer have been proven by scientists. This article describes treatments for bowel cancer.
Causes https://stoprak.info/vidy/mochevydelitelnaya-sistema/polovoj-chlen/golovki-pochemu-obrazuetsya-kak-obnaruzhit-chem-lechit.html of the formation of cancer of the glans penis.