Liver failure is a condition that is described by the keyword “failure”. That is, it is assumed that the patient will not perform one or more liver functions completely (to an insufficient extent).
It is important to note that in the early stages, with timely treatment, these disorders can be reversible. And in the future, taking into account complex therapy and eliminating the causes of liver failure (LI), it will be fully compensated.
The main reasons for the development of severe liver pathologies are viral hepatitis and alcohol-induced damage to hepatocyte cells.
Attention. Every year, more than one hundred thousand patients with viral hepatitis develop acute liver failure. The probability of death in such patients ranges from seventy to ninety percent.
Liver failure - what is it?
For reference. Liver failure is a combination of various disorders of hepatocyte functions, manifested by the inability of the liver to adequately maintain metabolic processes and ensure the constancy of the internal environment of the body.
At the initial stages of the disease, it is possible to maintain the normal functioning of the liver due to the maximum activation of its compensatory capabilities. However, the progression of the disease is accompanied by rapid depletion of the liver's potential.
Acute liver failure is a severe impairment of liver function that develops in less than eight weeks and is accompanied by the development of severe coagulopathy (blood clotting disorder), jaundice and hepatic encephalopathy.
Chronic liver failure is a pathological condition accompanied by progressive damage to liver tissue, destruction of hepatocyte cells and impairment of liver function for more than six months.
Liver failure that develops over eight to twenty-four weeks is called subacute.
For reference. If symptoms of liver failure develop within seven days from the onset of jaundice of the skin, a diagnosis of fulminant (fulminant or hyperacute) PN is made.
The ICD10 liver failure code depends on the type of disease:
- alcoholic acute and chronic liver failure is classified as K70.4;
- unclassifiable PN is numbered as K72;
- acute and subacute PN as K72.0;
- PN with hepatic necrosis, which developed as a result of toxic damage to the liver, is classified as K71.1;
- chronic liver failure - like K72.1;
- unspecified liver failure - like K72.9;
- damage to liver tissue in pregnant women, as well as in women in the postpartum period - like O26.6.
Attention. It should be noted that the very definition of “acute or chronic liver failure” has a fairly broad interpretation. This diagnosis does not have clear, standard diagnostic criteria, such as cardiovascular, respiratory or renal failure.
In this regard, the diagnosis of acute liver failure can be made both on the basis of only deviations in biochemical tests and coagulogram parameters (in this case, the clinical symptoms of the disease may be mild), and on the basis of a clear clinical picture of the disease.
However, in both cases, the basis of the pathogenesis of the disease will be a decrease in the mass of normally functioning hepatocytes.
The severity of clinical symptoms, the rate of disease progression and prognosis depend on the severity of hepatocyte necrosis. The development of PN is accompanied by a violation of:
- protein metabolism;
- protein synthetic function of the liver;
- blood clotting;
- the process of detoxification, neutralization of exogenous toxins and products of protein metabolism;
- synthesis of substances such as choline, glutathione, taurine, etc.;
- bilirubin metabolism;
- carrying out reactions such as deamination, transamination, decarboxylation of proteins and amino acids;
- regulation of metabolic processes by the liver, etc.
As a result, acute and chronic liver failure is manifested by the occurrence of severe hypoproteinemia, hypoalbuminemia, hypoglobulinemia, hypofibrinogenemia, hypothrombinemia, hypocoagulation and hyperfermentemia.
These disorders in liver failure are clinically manifested by the development of jaundice, severe weakness and drowsiness, aversion to food, nausea and vomiting, hemorrhagic rash and bleeding, edema and ascites, tremors of the limbs or convulsive attacks, neurological disorders, etc.
Etiology
Hepatocellular failure syndrome can develop both against the background of diseases directly related to gastroenterology, and against the background of other pathological processes that affect other organs or systems, or even have a negative impact on the entire body.
Thus, hepatic cell failure has the following etiology:
- infectious diseases affecting the entire body, with a long, relapsing course;
- hepatitis of all types;
- poisoning with toxic substances, poisons, heavy metals and similar chemicals;
- drug abuse, long-term pharmacological treatment;
- vascular diseases of the liver;
- diseases of the genitourinary system;
- obstruction of the bile ducts;
- liver damage by pathogenic organisms, including parasites;
- infection with Epstein-Barr virus, herpes simplex, cytomegalovirus, adenovirus;
- poisoning with poisonous mushrooms;
- chronic heart failure;
- transfusion of blood incompatible with the group;
- massive infiltration of the liver with malignant cells;
- sepsis;
- fatty liver;
- surgical intervention on this organ;
- massive blood loss;
- alcohol abuse, drug use;
- systematically unhealthy diet.
At risk are people who have a personal history of the following diseases:
- alcoholism;
- addiction;
- obesity;
- cirrhosis of the liver;
- systemic diseases;
- incurable chronic diseases.
It should be noted that if hepatocellular failure develops with cirrhosis of the liver, then the likelihood of death increases significantly.
Causes of hepatocellular failure
Liver failure - classification
A unified classification of liver failure has not been developed.
Based on the time of development, liver failure is divided into acute, subacute and chronic. Some classifications indicate fulminant, subfulminant and delayed forms of failure.
Attention! The severity of liver failure is always extremely high. This condition is life-threatening and is accompanied by a high risk of fatal consequences.
Even in cases where the diagnosis is made at the compensated stage (often without pronounced clinical symptoms, only based on test results), it must be taken into account that decompensation of liver function can develop almost at lightning speed. Therefore, the prognosis for the disease is always serious.
By stage, these pathologies are divided into initially compensated, severely decompensated, and terminal-dystrophic stages of hepatic coma.
Based on clinical symptoms, the following stages are distinguished:
- massive necrotic damage to hepatocyte tissues;
- development of hepatic encephalopathies.
According to the forms of damage to hepatocyte cells, the following are distinguished:
- hepatocellular types, developing against the background of inflammatory-necrotic damage to the liver cells and accompanied by a sharp decrease in skin turgor, skin pigmentation, the development of gynecomastia, intense jaundice of the skin and mucous membranes, as well as the development of hepatic encephalopathy and coma;
- excretory (cholestatic), developing as a result of prolonged intrahepatic stagnation of bile and manifested by intense jaundice, skin itching, bradycardia, steatorrhea, stool disorder and severe intestinal dysbiosis;
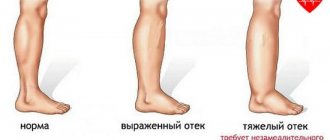
- vascular (vascular) form, which develops as a result of impaired hepatic microcirculation and is manifested by the development of symptoms of portal hypertension, “head of the jellyfish”, varicose dilations of the esophageal veins and bleeding from them, ascites, edema in the legs, splenomegaly (enlarged spleen).
Prevention
In order to reduce the risk of developing hepatic-renal failure, the following recommendations must be followed:
- Treat chronic and acute diseases of internal organs in a timely manner.
- Visit your doctor regularly to monitor the development of cardiovascular disease.
- Moderately, or better yet, avoid drinking alcohol.
- Before taking any medications, especially antibiotics, be sure to consult your doctor.
- Follow the principles of proper nutrition and regularly replenish the deficiency of beneficial enzymes in the body.
- Maintain good hygiene.
- Get vaccinated against hepatitis regularly.
- Carefully monitor your body's symptoms.
If the disease is detected at the first stage of development, there is a high chance of successful treatment.
Do not self-medicate. Only a doctor can give you competent recommendations, based on the characteristics of your body and the course of the disease. The prognosis for self-medication is not the most reassuring.
Liver failure - symptoms in men and women
It should also be noted that the liver has a large reserve of compensatory and regenerative capabilities. In this regard, pronounced and specific manifestations of liver dysfunction develop after more than seventy to eighty percent of the liver cells have died.
Attention. In acute liver failure, as a rule, seventy to ninety percent of liver cells are rapidly destroyed.
In chronic liver failure, the inflammatory process and necrotic damage to hepatocytes can gradually progress and last for years.
In most cases, symptoms of chronic renal dysfunction develop against the background of decompensated hepatic cirrhosis.
At the stage of massive inflammatory-necrotic lesions of the liver tissue, the disease can manifest itself:
- progressive weakness
- aversion to food and complete lack of appetite,
- constant drowsiness,
- lethargy,
- slight lethargy,
- nausea and vomiting,
- persistent febrile symptoms that are not relieved by antipyretics.
Also, at this stage of liver failure, the appearance and gradual progression of icteric staining of the skin, specific liver odors (sweet, cloying breath), a decrease in liver size (due to dystrophic damage to hepatocyte cells), blood clotting disorders, high ESR levels and the appearance of leukocytosis.
Therapy
Treatment for different forms of liver failure is very different.
Acute form:
- If the patient has an acute form of the disease, he requires emergency care: the person is hospitalized and preferably solutions (rather than tablets) are used for treatment: solutions are better absorbed, act faster and do not put a strain on the already affected liver.
- If the patient is found to have internal bleeding, the first step is to suppress it. In this situation, blood-restoring drugs are actively used, and blood transfusions are performed.
- To minimize the degree of intoxication, the patient is recommended to regularly cleanse the intestines, use cleansing enemas, and drugs that improve intestinal motility.
- When treating acute liver failure, doctors prescribe infusion therapy: solutions are injected into the patient's body to maintain blood pressure levels. Indicated for the treatment of diuresis with the prescription of diuretics and lactulose to suppress ammonia production.
- Antibacterial therapy is used to avoid side infections. With severe excitability, patients are prescribed psychotropic drugs that reduce agitation. Medicines are used to normalize blood circulation in the brain.
- Patients are given oxygen inhalations.
Chronic form:
- If a patient is diagnosed with chronic liver failure, they immediately begin to search for and eliminate the factor that caused the liver problems. In the case where tumors and fibrous lesions are detected in a patient, surgical intervention is recommended.
- To reduce intoxication and eliminate toxic brain poisoning, doctors prescribe lactulose preparations, as well as agents that remove ammonia from the body. Antibiotics are prescribed to suppress pathogenic microflora. Medicines are also used to reduce pressure in the portal vein.
- If patients have narrowing of the bile ducts, they are prescribed cholespasmolytics.
- In a number of severe and advanced cases, when the effect of the drugs is weak and the patient is in critical condition, the patient undergoes a liver transplant.
In case of liver failure, doctors recommend patients a diet without proteins, based on light foods that are well digestible and contain fiber and vitamins. The calorie content of food per day should be about 1400–1600 kcal.
Patients should consume more fruits and vegetables, dairy products, cereals, lean meats and fish, and they can also eat honey. Sweets, strong tea, smoked foods, alcohol are contraindicated, as are all foods high in fat. Spicy foods are also prohibited.
Diagnostics
For reference. Diagnosis of this disease often presents significant difficulties. Upon admission of patients with acute PN, clear specific symptoms of the disease and pronounced abnormalities in tests are often noted.
However, with gradual progression of liver dysfunction (chronic PN), often
there are no clinical manifestations of the disease (or nonspecific symptoms are detected: weakness, lethargy, drowsiness, decreased appetite, bloating, nausea, etc.). In this case, the diagnosis is often made based only on laboratory data.
Laboratory diagnostic criteria include the following indicators:
- total protein,
- albumins,
- cholesterol,
- blood clotting indicators,
- results of assessing hepatic clearance and bromosulfalene tests (radionuclide methods for assessing the volume of mass of active hepatocytes),
- performing ultrasound examination of the liver and CT (computed tomography).
A complete blood count, bilirubin levels, liver transaminases, ammonia, metonine, tyrosine, phenol, phenylalanine, protein profile, cholesterol, bilirubin, and alkaline phosphatase levels are also assessed.
For reference. Additionally, computed gammagraphy is performed, and, if indicated, a biopsy of liver tissue is performed.
An important role is also played by collecting anamnesis and identifying concomitant pathologies that could provoke the development of PN or may aggravate its course.
Treatment of pathology
Elimination of hepatic-renal failure consists of drug therapy, diet and daily routine.
First of all, treatment consists of eliminating the primary pathology that led to liver and kidney failure. An important point is the selection of medications, since the liver may not withstand the heavy load that medications provide. The patient is strictly recommended to adhere to a diet that limits protein and fats. Hepatoprotective agents and oxygen therapy are prescribed. When the liver is partially affected, the patient is prescribed Prednisolone.
Glucose, calcium, and diuretics must be administered intravenously.
If necessary, peritoneal dialysis or hemodialysis using an artificial kidney is performed. In medicine, to treat pathology, they resort to the hetero-liver method, but in modern medicine this method is questionable and is used extremely rarely. The hemodialysis method is used to combat coma and resulting intoxication, when the patient’s blood is purified using an “artificial kidney” apparatus. If there is inflammation, then weak antibiotics are prescribed. When the patient loses blood, a drip infusion of donor blood is used.
Danger of disease
The main danger of hepatic-renal failure lies in the failure of the kidneys and liver due to damage to the tissues of these organs.
The main danger of hepatic-renal failure lies in the following:
- Failure of the kidneys and liver due to damage to the tissues of these organs.
- Due to exposure to toxins, other organs are involved in the destructive process. The respiratory system, gastrointestinal tract and central nervous system may be affected.
- The affected organs begin to accelerate each other’s destructive pathogenic processes. As a result, the disease progresses rapidly and can very quickly lead to the death of the patient if the brain is involved in the process. The mortality rate is approximately 80-90%.
- Those who survive the disease develop postnecrotic cirrhosis of the liver.