Acute intestinal infection is a disease caused by microorganisms that have entered the human intestines. The causative agents of the disease are bacteria, viruses, protozoa or fungi. The source of infection is a sick person, an animal, everyday items and the environment, food, water.
Acute intestinal infections (AI) are characterized by indigestion, causing abdominal pain, diarrhea, vomiting and intoxication of the body. The disease is severe in children: the body quickly becomes dehydrated and has weak immunity.
Intestinal infections are dangerous during pregnancy: dehydration and intoxication of a woman’s body lead to miscarriage or provoke oxygen starvation of the fetus.
According to ICD 10, intestinal infections are in first place in the list, their codes are A00-A09. The most dangerous disease is cholera (ICD code 10 A00). The list of intestinal infections begins with this.
What are acute intestinal infections?
Intestinal infections are characterized by rapid spread. Transmission is by oral-fecal, nutritional and airborne routes. The infection is transmitted from person to person through unwashed hands, household items, poorly washed fruits and vegetables, and by water.
Human intestinal infections
Pathogenic microorganisms are carried by insects (flies, cockroaches), sick farm animals, birds or rodents.
Pathogenic microorganisms choose the human intestine as their habitat.
Intestinal infectious diseases have similar clinical manifestations; etiology and epidemiology are different.
Intestinal infections, a list of which can be found in the medical literature, vary depending on the type of pathogen and the effect on the body. Medical reference books, books, magazines and online publications provide a list of OKIs describing the etiology, pathogenesis, clinical manifestations, methods of diagnosis and treatment.
ethnoscience
For AEI, the following traditional medicine recipes are used:
20 gr. peppermint leaves, 15 gr. fennel fruits and calamus root, 30 gr. daisies. Grind the ingredients, 1 tbsp. Brew a spoonful of the prepared mixture with a mug of hot water. Take 1/3 cup three times a day;- 40 gr. oak bark, pour a liter of boiling water, simmer for 10 minutes over low heat. Cool, take ½ cup 6 times a day;
- For a liter of boiled water, 8 teaspoons of granulated sugar and ½ teaspoon of soda, 1 cup of orange juice, a teaspoon of salt, drink throughout the day.
Etiology of acute intestinal infections
Types of OKI:
- Bacterial – pathogens – pathogenic bacteria (Salmonella dysentery bacillus, Pseudomonas aeruginosa and others) and their toxins. Bacterial infections include: dysentery, salmonellosis, escherichiosis, infection caused by Pseudomonas aeruginosa, typhoid fever, cholera, botulism and others.
- Viral – pathogens: reovirus, rotavirus, enterovirus, adenovirus, coronovirus and others.
- Fungal – pathogens – fungi of the Candida species.
- Protozoan – caused by parasitic protozoa (amoeba, giardia, parasitic ciliates Balantidium coli).
Regardless of what types of microorganisms caused the disease, its symptoms are unpleasant, the treatment period is long, and the outcome is not always favorable.
Prevention
Preventive measures include:
- Drinking boiled water;
- Washing vegetables and fruits;
- Compliance with personal hygiene rules;
- Short-term storage of perishable products;
- Heat treatment of food before consumption;
- Home cleaning;
- Do not swim in polluted waters.
• Inflammatory processes of the abdominal organs • Intestinal obstruction • Calculous cholecystitis.
Treatment
• Diet. Limiting and changing the diet using lactic acid products in the diet, observing the principle of mechanical sparing. It is recommended to consume foods that slow down peristalsis - those with a high tannin content (blueberries, bird cherry, strong tea); substances with a viscous consistency (mucoid soups, pureed porridges, cottage cheese and kefir, jelly); crackers; indifferent substances - steamed dishes from lean meat and fish. Avoid fried and fatty foods, raw vegetables and fruits. • Etiotropic therapy for bacterial infections (carried out to all children, the elderly, patients with severe and complicated forms): antibiotics, sulfonamide drugs, nitrofuran or hydroxyquinoline derivatives for 7-10 days. Preference is given to drugs prescribed orally and poorly absorbed in the intestine. Parenteral administration of drugs is used for severe and complicated forms. • For all acute intestinal infections - rehydration therapy • Oral rehydration therapy: citroglucosolan, glucosolan, rehydron up to 120-150 ml/kg/day • Infusion rehydration therapy (usually solutions containing sodium chloride, potassium chloride, sodium bicarbonate) is used for severe forms of dehydration. • Symptomatic therapy - if necessary. • For vomiting - dimenhydrinate 50 mg every 4 hours or aminazine 25-100 mg/day/m, or prochlorperazine (meterazine) 25 mg 2 times/day in suppositories. • For severe intestinal cramps - meperidine 50 mg IM every 4-6 hours. • For diarrhea for 12-24 hours - diphenoxylate 2.5-5 mg orally 3-4 times a day or preparations containing bismuth extract belladonna, atropine sulfate or kaolin.
Complications
• Bacterial infections of the respiratory system and middle ear • Intestinal dysbiosis • Intestinal bleeding • Perforation of the intestinal wall • Intussusception. Prevention. Carrying out sanitary and hygienic measures and strict adherence to technological rules for the preparation, storage and sale of food products. Early diagnosis and isolation of patients with acute intestinal infections. In areas of infection, disinfection is carried out (treatment with disinfectant solutions, boiling of dishes). Convalescent drugs are prescribed only after a negative result of a stool test. All convalescents are actively observed in a clinic (dispensary observation) for 1 month after the illness. In closed and children's groups, laboratory examinations of contact persons and service personnel are carried out. Reduction. ACI - acute intestinal infection
AOO-A09 Intestinal infections
Handbook of Diseases. 2012.
See what “ACUTE INTESTINAL INFECTIONS” is in other dictionaries:
Intestinal gases - Flatulence (from the Greek μετεωρισμός rising upward, bloating) excessive accumulation of gases in the intestines. Manifested by bloating, swelling, bursting pain in the abdomen; possible abundant (explosive) release of large amounts of digestive gases ... Wikipedia
IN-HOSPITAL INFECTIONS - (syn: nosocomial infections) - infectious diseases and wound infections that were added to the main disease in the hospital, as well as diseases of health workers that arose in connection with the treatment and care of infectious patients. Source... ... Encyclopedic Dictionary of Psychology and Pedagogy
Proteus infections - infectious. processes caused by bacteria of the genus Proteus (see). All representatives of this genus are conditionally pathogenic for humans and are capable of causing diseases characterized by a variety of localization and a polymorphic wedge pattern. In the 70s and 80s ... Dictionary of Microbiology
CHILDREN'S INFECTIONS - a group of infectious diseases. diseases that occur predominantly. in children. A common sign of all infections. Diseases have the ability to be transmitted from an infected organism to a healthy one and, under certain conditions, to become widespread (epidemic). Source... ...Russian Pedagogical Encyclopedia
Epidemiology of AEI
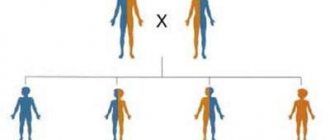
The reasons for the occurrence and spread of acute intestinal infections are that pathogenic microorganisms are quickly transmitted from a sick person or a carrier of infection.
Pathogenic microorganisms are resistant to environmental conditions, retain harmful qualities for a long time in the cold, and remain on objects with which an infected person has been in contact.
Pathogens leave the body infected with an intestinal infection along with feces and vomit and are transferred to surrounding household items, water, food with the help of hands, insects, and end up with sewage in water bodies. Transmission of the pathogen is “along the chain”, which leads to the emergence of an epidemic.
Classification of epidemics depending on the source of infection:
- Water epidemics. Characterized by mass infection of people using a water source. When the use of water from the source or its disinfection is stopped, the epidemic subsides.
- Food epidemics. As a result of eating foods that have not undergone heat treatment, or the ingestion of pathogenic microorganisms.
- Household. A large number of sick children. Infections are transmitted through toys and household items.
Epidemics vary in intensity and seasonality.
Children who are unable to follow the rules of hygiene are susceptible to intestinal diseases.
If one child gets sick, the entire group of children is at risk.
Children under 2 years old
A child under 2 years of age needs to drink at least a liter of saline solutions or other liquid per day. Give in small quantities, but often. Offer your child the food he usually eats. Better more often and little by little. Products that are healthy for a child: cereal, bread, potatoes, lean meat, unsweetened yogurt, bananas, applesauce, vegetables. It is not advisable to limit the diet to liquid food, since it is not enough to replace the loss of vitamins and other nutrients through vomiting and loose stools.
Clinical picture of OKI
Intestinal infections are common diseases.
The clinic of all acute intestinal diseases is characterized by common manifestations:
- Infectious toxic syndrome. A sharp increase in body temperature to low-grade or high or fever. Manifestations of intoxication of the body are aches, muscle pain, nausea.
- Intestinal syndrome. Abdominal pain, severe diarrhea and vomiting. Depending on the type of pathogen that has entered the body, manifestations of intestinal syndrome differ in the localization of pain, consistency, stool color and frequency, the presence of mucus or blood in the stool, and the nature of vomiting.
- Dehydration of the body. Rapid dehydration and rapid weight loss. Acute lack of moisture in the tissues of the body (dry skin and mucous membranes, severe thirst).
The first symptoms of the disease appear 6-48 hours after infection.
Drug treatment
Medicines intended to treat intestinal infections are prescribed by a doctor on the basis of laboratory tests, through which the type of causative agent of the disease is identified. So, if the infection is viral in nature, then antiviral drugs are prescribed. If the source of the disease is bacteria, the patient is prescribed antibacterial tablets.
Since intestinal poisoning the most pronounced symptoms are intoxication and stool disturbances, first of all, they need to be eliminated. This is achieved by eliminating from the body of the diseased pathogenic agent that caused the disease. It is also necessary to normalize the water-electrolyte balance in the intestines and remove toxic substances from the body. To achieve the latter, it is necessary to treat the patient with sorbents.
Treatment of intestinal infection includes taking the following groups of drugs:
- antibiotics;
- antiviral agents;
- sorbents;
- medicines for diarrhea;
- enzymes;
- painkillers.
For intestinal infections of bacterial origin, antimicrobial agents from the group of fluoroquinolones, tetracyclines, amphenicolones or metronidazoles are prescribed. These may be Ofloxacin, Norfloxacin, Ciprofloxacin, Levomethicin, Doxycycline. All types of intestinal infections are accompanied by the formation of toxic substances as a result of the activity of pathogenic microorganisms.
Therefore, it is necessary to take medications to remove them from the gastrointestinal tract. For this purpose, sorbents are prescribed; they absorb harmful substances and remove them from the intestines unchanged. The most popular drug in this group is activated carbon. The recommended dose of the drug is 1 tablet per 10 kg of body weight. Also, in case of severe intoxication, Polysorb, Smecta or Enterosgel are prescribed.
To normalize stool and eliminate diarrhea, special medications are prescribed. Their names are as follows: Trimebutin, Loperamide, Stopdiar, Fthalazol, Nifuroxazide. Taking these drugs will have a positive effect on the functioning of the gastrointestinal tract. They help reduce intestinal tone and motility.
If, along with other symptoms, an intestinal infection is accompanied by severe pain, you can take painkillers. But this should be done only after the doctor’s approval, since taking them independently before being examined by a doctor can change the clinical picture, which will significantly complicate diagnosis. Usually, Spazmaton, No-shpa or Benalgin are prescribed to alleviate the condition.
After eliminating the acute symptoms of an intestinal infection, it is recommended to take enzymatic preparations to normalize and accelerate digestive processes. As such, Mezim forte, Pancreatin or Micrazim are most often prescribed. It is also necessary to restore the intestinal microflora; for this purpose, taking probiotics is provided. They are included in the complex treatment of intestinal infections in both adults and children.
In some cases of intestinal infection, emergency treatment may be required. The need for this arises when the patient experiences uncontrollable diarrhea more than 8 times a day. The nature of the stool is also important; it is watery and resembles rice water that is alarming. For such symptoms, it is recommended:
- put in a dropper with glucose and isotonic sodium chloride solution;
- Inject the lytic mixture intramuscularly;
- take steps to rehydrate;
- ensure the intake of adsorbents.
In case of food poisoning, gastric lavage and a cleansing enema are also performed. These procedures must be prescribed by the attending physician.
Intestinal infection requires complex treatment
Intestinal flu is the most common intestinal infection
Intestinal flu affects children from six months to two years. The nature of the disease is viral, the causative agent is rotavirus - a pathogenic microorganism that has a three-layer dense shell and a “wheel” shape.
Pathways and mechanism of infection with rotavirus
Rotavirus intestinal infection is transmitted by the fecal-oral route. Trillions of bacteria leave in the stool of an infected person, while a hundred units are enough to infect others. Rotaviruses are tenacious, resistant to low temperatures and remain on household items with which the patient or carrier of the virus has come into contact.
From these objects they are transferred through poorly washed hands into the oral cavity of a healthy person and settle on the mucous membranes of the stomach and intestines. In close contact, rotavirus is transmitted through the saliva of an infected person.
Rotavirus enters through unboiled water and food that is poorly washed or has not undergone sufficient heat treatment.
In the event of mass infection, a rotavirus epidemic occurs. An outbreak of the disease occurs in late autumn and winter. Foci of infection are in crowded places - kindergartens, schools, nursing homes, dormitories.
In order to prevent the mass spread of intestinal infections in schools, preschool institutions, groups, and enterprises, an “Operational Action Plan for the Prevention of Acute Intestinal Infections” is being drawn up.
Sources of infection
Sources of infection are sick adults and children who have already shown symptoms of the disease, or virus carriers - persons in whose body there is a virus, but there are no signs of the disease.
Rotavirus gets into the water supply system and water bodies with wastewater, where swimming leads to infection.
Incubation period and duration of the disease
The incubation period lasts up to six days.
The duration of illness for intestinal rotavirus infection is 2 weeks. The disease goes through two phases: acute and convalescent phase. The first phase lasts 7 days: the body fights the infection, the symptoms are severe. During the second phase, the body develops immunity, and gradual recovery begins.
Symptoms
Clinical manifestations of intestinal flu are similar to acute respiratory viral infections in the first days of the disease:
- temperature rise to 39 degrees;
- headache;
- sore throat and redness,
- runny nose, cough, headache;
- pain in the abdominal area;
- diarrhea;
- bouts of vomiting;
- lack of appetite;
- lethargy and weakness.
OKI in an adult
The absence of high temperature distinguishes food poisoning from intestinal infections caused by pathogenic bacteria or viruses.
A dangerous manifestation in the acute phase of the disease is dehydration. The patient must be given water.
Features of the course of the disease in adults and children
The three-layer shell makes rotaviruses invulnerable to the environment of the gastrointestinal tract and intestinal enzymes. During the course of the disease, the virus infects enterocytes - intestinal epithelial cells - and leads to their death, modifying the epithelium. Severe diarrhea and severe dehydration of the body occur; This is the pathogenesis of the disease.
Rotavirus in children
Intestinal infections are dangerous for children, which is due to the characteristics of the child’s body and immunity. OCI is a common disease among children from six months to two years.
Enterovirus and rotavirus infections often occur in childhood and are similar to each other. At first, parents confuse them with acute respiratory infections, as there is a jump in temperature, cough, watery eyes, and runny nose. Then vomiting and diarrhea follow.
For both enterovirus and rotavirus infections, the symptoms are high fever, diarrhea and vomiting, abdominal pain, lack of appetite, and weakness.
Unlike rotavirus, enterovirus affects, in addition to the gastrointestinal tract, the liver, heart and nervous system of the child and affects vision.
Dehydration and intoxication are manifestations of the disease. Dehydration of the body occurs so quickly that the child does not produce urine or tears. The pain disrupts the baby's sleep patterns.
Treatment boils down to drinking salted water or administering fluids intravenously.
Breastfed children are less susceptible to gastrointestinal infections due to the quality of mother's milk.
Due to the high infant mortality rate due to intestinal infections, pediatrics pays special attention to the prevention, diagnosis and treatment of acute intestinal infections in children.
Today, there are manuals and scientific articles devoted to the problems of child nutrition, methods of feeding them safely, methods of treating and preventing intestinal infections, and the development of the immune system.
Rotavirus in adults
Features of the manifestation of intestinal flu in adults are that the course of the disease occurs with less pronounced symptoms. This is due to the protection of the adult organism - the acidic environment of the stomach and the content of immunoglobulin A in the secretion produced by intestinal enterocytes.
The manifestation of the disease in an adult is intestinal disorder. A person is a carrier of infection, not suspecting that an intestinal disease is hidden behind the mild symptoms.
Rotavirus in pregnant women
Rotavirus infection during pregnancy does not pose a danger to the fetus. Dehydration of a woman’s body provokes oxygen starvation of the fetus. Therefore, it is important to prevent dehydration and maintain bed rest at the first signs of intestinal flu. Preventive measures and hygiene will help reduce the risk of intestinal infection.
Diagnosis of rotavirus infection
Identification of signs of disease - through examination of the patient and conversation. Data on body temperature is recorded, blood pressure is measured, and the abdominal area is palpated. They conduct examinations of the patient’s urine, feces and blood, and examine the mucous membranes of the rectum.
Differential diagnostics – for salmonellosis, cholera, dysentery, food toxic infections.
Determining the virus based on the analysis of RSC or RTHA in the first days is impossible: antibodies are produced in an adult after a few days, in a newborn - after a few months. The diagnosis is confirmed based on the epidemiological situation and seasonality.
Diagnostics
In each case, the disease is diagnosed preliminary, as a result of examination and questioning of the patient. But an accurate determination of the causative agent of intestinal infection will be given by bacteriological examination of feces, blood, and vomit.
Laboratory diagnostics include culture and microbiological examination of stool for intestinal group, blood test for RNGA with shigella diagnosticums.
For the purpose of preliminary diagnosis, a relationship is established between the quality of food consumed and the appearance of stool. Then a test for rotavirus infection is performed.
If the result is negative, the following type of diagnosis is necessary:
- stool culture;
- examination of wash water for a nutrient medium for bacteria that provoked the disease;
- Vomit is examined using a similar method.
Test results may take up to five days. The serological method allows you to detect specific antibodies to viruses of various types using ELISA, RNGA.
The patient is tested for carriage of intestinal pathogens from a vein, which is carried out not on the first day of the disease, but in the process of fighting the progressive virus.
It is mandatory to study the signs of a particular type of bacteria in biological material (PCR study). Changes in the intestinal microflora inherent in one or another type of gastrointestinal lesion can be detected by studies using sigmoidoscopy, colonoscopy and other methods.
If the culture result is negative, immunological diagnostic methods are used. Enzyme immunoassay methods can detect antibodies to Campylobacter and Salmonella; enterotoxins of pathogenic strains can be detected using PCR and latex agglutination.