Systemic autoimmune diseases
Autoimmune diseases often present diagnostic difficulties, require special attention from doctors and patients, are very different in their manifestations and prognosis, and, nevertheless, most of them are successfully treated.
This group includes diseases of autoimmune origin that affect two or more organ systems and tissues, for example, muscles and joints, skin, kidneys, lungs, etc. Some forms of the disease become systemic only as the disease progresses, for example, rheumatoid arthritis, while others immediately affect many organs and tissues.
Major systemic autoimmune diseases:
- Systemic lupus erythematosus;
- systemic sclerosis (scleroderma);
- polymyositis and dermapolymyositis;
- antiphospholipid syndrome;
- rheumatoid arthritis (does not always have systemic manifestations);
- Sjögren's syndrome;
- Behçet's disease;
- systemic vasculitis (this is a group of different individual diseases, united on the basis of a symptom such as vascular inflammation).
What else can you do to improve your condition?
If you're living with an autoimmune disease, there are things you can do every day to feel better:
- Eat healthy, well-balanced foods. Make sure your diet includes fresh fruits and vegetables, whole grains, low-fat or low-fat dairy products, and a lean source of protein. Limit your intake of saturated fat, trans fat, cholesterol, salt and refined sugar. If you follow a healthy eating plan, you will get all the nutrients you need from food.
- Be physically active. But be careful not to overdo it. Talk to your doctor about what types of physical activity you can do. A gradual increase in loads and a gentle exercise program often has a positive effect on the well-being of people with muscle damage and joint pain. Some types of yoga or Tai Chi exercises can be very beneficial for you.
- Get plenty of rest. Rest gives your body's tissues and joints the time they need to recover. Healthy sleep is a great way to help your body and mind. If you don't get enough sleep and are stressed, your symptoms may get worse. When you don't sleep well, you also can't fight illness effectively. When you are well rested, you can better solve your problems and reduce your risk of developing disease. Most people need at least 7 to 9 hours of sleep every day to feel well-rested.
- Reduce stress levels. Stress and anxiety can cause symptoms of some autoimmune diseases to flare up. Therefore, using ways that can help you simplify your life and cope with daily stress will help you feel better. Meditation, self-hypnosis, visualization and simple relaxation techniques can help you reduce stress, control pain, and improve other aspects of life related to your illness. You can learn how to do this through books, audio and video materials or with the help of an instructor, and you can also use the stress relief methods described on this page - How to Get Rid of Stress - Top 10 Ways.
Causes of autoimmune diseases
Reasons are conventionally divided into two types. The first type includes internal reasons, and the second type includes external reasons. Internal causes include type I gene mutations. In this case, the cells of the immune system (lymphocytes) cease to be identified.
The second internal reason: this includes gene mutations, directly type II. In this case, the uncontrolled proliferation of nurse lymphocytes begins. Against this background, autoimmune diseases may occur. For example, such as:
- chronic disease - multiple sclerosis;
- Systemic lupus erythematosus often develops.
As a rule, such diseases are most often hereditary.
External causes of autoimmune diseases:
- protracted infectious diseases;
- severe infectious diseases;
- negative impact on the body from the environment, for example: solar or radiation exposure of the body.
It is necessary to note another important reason that can lead to autoimmune diseases. Cells that cause a particular disease, they may be similar to one’s own cells. Therefore, the hospital lymphocytes cannot recognize them.
Long-term immunodeficiency arising from a harmful environment, poor nutrition, bad habits and chronic infections Imbalance in the interaction of the immune, nervous and endocrine systems Congenital and acquired abnormalities of stem cells, genes, the organs of the immune system themselves, as well as other organs and groups of cells Cross-reactions of the immune system to background of immunodeficiency.
It is known that in “backward” countries, where people eat poorly and mostly plant foods, autoimmune diseases are poorly developed. It is now known for sure that an excess of chemically processed foods, fatty and protein foods, together with chronic stress, gives rise to monstrous disruptions of the immune system.
Therefore, the “Sokolinsky System” always begins with cleansing the body and supporting the nervous system, and against the background of this, you can try to calm the immune system.
You can read about our special view on the causes of autoimmune diseases here
Autoimmune diseases still remain one of the most important and still unresolved problems of modern immunology, microbiology and medicine, so their treatment is still only symptomatic. It’s one thing if the cause of a serious illness is an error of nature, and quite another thing when the prerequisites for its development are created by the person himself, who does not care about his health in any way. Take care of yourself: your immune system is as vindictive as it is patient.
The human immune system matures most intensively from birth to the age of fifteen. During the process of maturation, cells subsequently acquire the ability to recognize certain proteins of foreign origin, which becomes the basis for fighting various infections.
There is also a part of lymphocytes that perceive proteins of their own body as foreign. However, in the normal state of the body, the immune system exerts strict control over such cells, so they perform the function of destroying sick or defective cells.
But under certain conditions in the human body, control over such cells may be lost, and as a result they begin to act more actively, destroying normal, full-fledged cells. Thus, the development of an autoimmune disease occurs.
To date, there is no exact information about the causes of autoimmune diseases. However, research by specialists allows us to divide all causes into internal and external.
The external causes of the development of diseases of this type are determined by the impact on the body of pathogens of infectious diseases, as well as a number of physical influences (radiation, ultraviolet radiation, etc.). If, due to these reasons, a certain tissue in the body is damaged, the altered molecules are sometimes perceived by the immune system as foreign elements. As a result, it attacks the affected organ, a chronic inflammatory process develops, and tissues are damaged even more.
Another external reason for the development of autoimmune diseases is the development of cross immunity. This phenomenon occurs if the infectious agent is similar to one’s own cells. As a result, human immunity affects both pathogenic microorganisms and its own cells, damaging them.
Gene mutations that are hereditary are defined as internal causes. Some mutations can change the antigenic structure of any tissue or organ. As a result, lymphocytes can no longer recognize them as their own. Autoimmune diseases of this type are usually called organ-specific.
Due to other mutations, the balance of the immune system is disrupted, which does not ensure proper control over autoaggressive lymphocytes. If, under such circumstances, the human body is affected by certain stimulating factors, then as a result, the manifestation of an organ-nonspecific autoimmune disease is possible, which will affect a number of systems and organs.
To date, there is no accurate information about the mechanism of development of diseases of this type. According to the general definition, the occurrence of autoimmune diseases provokes a violation of the general functions of the immune system or some of its components. There is an opinion that directly unfavorable factors cannot provoke the onset of an autoimmune disease. Such factors only increase the risk of developing diseases in those who have a hereditary tendency to such pathology.
Classic autoimmune diseases are diagnosed quite rarely in medical practice. Autoimmune complications of other ailments are much more common. As some diseases progress, the tissue structure partially changes, causing them to acquire the properties of foreign elements.
Sometimes the immune system attacks healthy tissues because a foreign antigen attaches to them. This is possible, for example, with viral hepatitis B. There is another mechanism for the development of autoimmune reactions in healthy organs and tissues: the development of allergic reactions in them.
Most autoimmune diseases are chronic illnesses that develop with alternating exacerbations and periods of remission. In most cases, chronic autoimmune diseases provoke serious negative changes in the functions of organs, which ultimately leads to disability.
Experts identify two groups of reasons that can lead to disruptions in the functioning of the immune system.
Internal are gene mutations that are inherited. They are divided into two categories. The first is mutations that disrupt the balance of the immune system. When certain factors appear, a person is faced with an autoimmune disease affecting several organs. The second group involves diseases that are inherited and affect the same organs in each generation.
External - this includes: • radiation or solar radiation; • severe infectious infections, after which the immune system begins to work incorrectly; • pathogen cells, which are very similar to the cells of the body itself, and therefore cause the activity of lymphocytes in relation to healthy and diseased cells.
By studying the main reasons, you can understand who is at high risk and should pay special attention to their health.
Skin precancer
This is a special group of dermatological pathologies, against the background of which malignant processes can develop that threaten the patient’s life. If we consider oncological diseases, we cannot help but remember Bowen’s disease. This pathology was first described in 1912. Unpleasant symptoms can develop in both men and women aged 20-80 years. The pathological process usually causes prolonged exposure to harmful chemicals, radiation or ultraviolet radiation.
Single or multiple formations begin to appear on the skin. Rare symptoms begin to develop rapidly. Initially, malignant cells are present in the epidermis and do not grow further. But in the absence of complete therapy, the disease can transform into squamous cell carcinoma. This will increase the risk of metastases.
When considering the more common skin cancers, it is worth paying attention to melanoma. The pathological process develops as a result of malignant degeneration of moles (nevi). Melanoma is a very dangerous condition. Cancer cells spread very quickly, leaving a person with only a slim chance of survival.
A pre-cancerous condition is not something to joke about. If a mole begins to change color or gets larger, you should make an appointment with an oncologist as soon as possible. The skin disease can be managed if therapy is started at an early stage.
Autoimmune diseases, infections, allergies - all these pathological processes can affect the condition of the skin. Only a doctor can prescribe the correct treatment. Any changes are a reason to seek a consultation.
List of autoimmune diseases
There is a certain classification of all autoimmune diseases.
| By type of lesion | Diseases |
| System | · lupus erythematosus; · Behçet's disease; · vasculitis; · acquired chronic disease scleroderma. |
| Organ-specific | · joint and nervous diseases; · diseases of the gastrointestinal tract; · liver diseases; · diseases of the circulatory system. |
Organ-specific diseases also include pulmonary and skin diseases. The most common: psoriasis, allopathy, myocarditis, rheumatic fever.
This treatment method helps eliminate the cause of the disease. As a rule, the dietary method is prescribed to those patients whose cell membrane permeability is impaired. For example: for diseases such as: Hashimoto’s, type I diabetes mellitus, as well as Alzheimer’s disease or encephalitis.
What is the point of the dietary method? The main goal of this treatment is to restore “damaged” cell membranes as quickly as possible.
It should be noted that membranes can be damaged due to radiation, so the human immune system begins to recognize such cells as pathogenic, despite the fact that they are healthy.
Therefore, if the membranes are restored in a timely manner, the autoimmune process automatically stops.
To restore the membrane, you can use Ginkgo Biloba dietary supplement, and also include healthy fats in your diet.
Ginkgo biloba - traditional medicine recipes
Dietary supplements should be taken on an empty stomach, then consume healthy fats. For example:
- lecithin;
- fish fat;
- oils (linseed oil, hemp oil or olive oil);
- fish roe.
Important! If you take the Ginkgo Biloba dietary supplement correctly, the process will speed up faster than just sticking to proper nutrition.
The dosage of pure Ginkgo Biloba is 100 mg per day. If you purchased an impure dietary supplement at a pharmacy, then you need to consult a doctor to choose the optimal dose for your problem. The course of treatment for autoimmune diseases ranges from 3 weeks to 8 months, it all depends on the severity of the disease.
There are several types of autoimmune diseases. Some of them attack cells in a specific organ, such as type 1 diabetes, which damages cells in the pancreas, or autoimmune thyroid diseases, which affect only the thyroid gland. Other types can affect the entire body, as is the case with lupus.
1. Rheumatoid arthritis.
Rheumatoid arthritis is a disease in which the immune system attacks the joints, causing inflammation, redness, stiffness and pain in the joints.
2. Diabetes.
Type 1 diabetes is an autoimmune disease in which cells in the pancreas are damaged by the immune system, causing the organ to be unable to produce insulin or to produce too little insulin. Insulin is an essential hormone for regulating blood sugar levels, and a lack of it can cause the glycemic index to be persistently high.
3. Psoriasis.
Psoriasis, also known as psoriatic arthritis, is a skin disease in which epithelial cells grow in size and then separate. This causes skin cells to multiply much faster than normal, resulting in excess skin cells that can form red spots and scales on the skin (see photo).
4. Lupus.
Also called systemic lupus erythematosus, lupus is an autoimmune disease that causes a rash. However, it is not just a skin disease as it affects several organs including the kidneys, brain, heart and joints.
5. Multiple sclerosis.
Multiple sclerosis occurs when the immune system attacks myelin, which is the lining of nerve cells in our body. Such damage can damage the nervous system and affect the transmission of nerve signals between the brain and the rest of the body.
This results in unpleasant symptoms that vary from patient to patient and can include numbness, balance problems, difficulty moving, weakness and various other health problems.
6. Inflammatory bowel disease.
Inflammatory bowel disease is an inflammation of the lining of the intestines that occurs in two forms: Crohn's disease, in which inflammation can occur anywhere in the gastrointestinal tract, or ulcerative colitis, which affects only the lining of the colon and rectum.
7. Chronic inflammatory demyelinating polyneuropathy (CIDP).
CIDP is a disease in which the immune system attacks the body's nerves, impairing their motor function. In some cases, when diagnosis and treatment take too long, the disease can result in patients having to use wheelchairs.
8. Graves' disease.
In Graves' disease, the immune system attacks the thyroid gland and prevents the production of hormones. This change in hormone production can cause symptoms such as increased heart rate, weight loss, nervousness, and heat intolerance.
9. Addison's disease.
Addison's disease is an autoimmune disease that affects the adrenal glands, which are responsible for producing the hormones aldosterone and cortisol. Low amounts of these hormones in the body can impair the consumption and storage of carbohydrates, leading to symptoms such as fatigue, low glycemic index and weakness.
10. Guillain-Barre syndrome.
Guillain-Barré syndrome is a disease in which the immune system attacks the nerves that control the muscles in the legs and upper body. This can cause muscle weakness in these regions and other symptoms that affect mobility.
11. Hashimoto's thyroiditis.
In this autoimmune disease, the production of thyroid hormones decreases, causing symptoms such as hair loss, fatigue, swelling of the thyroid gland, sensitivity to cold, and weight gain.
12. Celiac disease.
Celiac disease occurs when the immune system comes into contact with gluten from food. Therefore, people with this disease cannot eat foods containing gluten.
13. Sjögren's syndrome.
Sjögren's syndrome is another autoimmune disorder that affects the joints and glands that lubricate the eyes and mouth. Thus, the main symptoms of this syndrome are dry mouth and dry eyes, and joint pain.
14. Myasthenia Gravis.
This autoimmune disease affects the nerves that help the brain control muscles. Thus, symptoms such as muscle weakness during physical activity and problems with swallowing and facial movements may occur.
15. Pernicious anemia.
Pernicious anemia is an autoimmune disease that affects a protein called intrinsic factor, which helps the intestines absorb vitamin B12 found in diet foods.
A lack of vitamin B12 reduces the synthesis of red blood cells, which in turn can impair the absorption of other nutrients and oxygen to various organs of the body.
16. Vasculitis.
Vasculitis is an autoimmune condition in which the immune system attacks the blood vessels. This leads to inflammation, which reduces the size of veins and arteries, which impairs blood circulation.
It is impossible to determine a list of symptoms that could accurately diagnose an autoimmune disease. We said above that different organs and their entire systems can be affected. Depending on this, the signs accompanying health problems will differ.
Let's consider the main diseases that are most often encountered in medical practice: 1. Rheumatoid arthritis. Characterized by joint damage. Small joints in the hands are especially susceptible to problems. Rheumatoid arthritis manifests itself in fairly severe pain and impaired mobility. Additional signs include swelling and numbness of the hands, and increased body temperature.
General muscle weakness may also occur. Rheumatoid arthritis tops the list of diseases because it is diagnosed more often than others.2. Multiple sclerosis. Develops against the background of damage to nerve cells. A person observes previously unusual tactile sensations. He loses sensitivity and notes that visual acuity decreases.
Multiple sclerosis is also differentiated by other signs, such as muscle spasms, numbness of certain parts of the body, and memory impairment. 3. Type 1 diabetes mellitus. In most cases, it cannot be completely cured. A person must use insulin injections throughout his life to maintain normal blood glucose levels.
The main symptoms are increased urination, intense thirst and a significantly increased appetite. 4. Vasculitis. It is considered a very dangerous autoimmune disease. Characterized by damage to the circulatory system. The vessels become highly fragile. As a result, organs seem to be destroyed from the inside.
Various levels of hemorrhage intensity are observed. The signs are very pronounced, so there are no problems in diagnosis. 5. Lupus. It belongs to the group of systemic diseases, because it affects almost all organs. The person notices pain in the heart, difficulty breathing, and increased fatigue.
Red raised bumps form on the skin. They are characterized by an irregular shape. They itch and become crusty. 6. Pemphigus. The main symptom is the appearance of large blisters on the surface of the skin. Inside they are filled with lymph.7. Hashimoto's thyroiditis. Autoimmune thyroid disease.
The symptoms are quite vague. They manifest themselves as drowsiness and roughening of the skin. There is also a significant increase in body weight. 8. Hemolytic anemia. Quite a serious health problem. Here the white blood cells begin to work against the red blood cells. A lack of red blood cells contributes to increased fatigue, constant lethargy and fainting. 9.
Graves' disease. Like Hashimoto's thyroiditis, it affects the thyroid gland. The latter produces excessive amounts of the hormone thyroxine. As a result, a sufficiently clear clinical picture appears. The person notes weight loss, poor heat tolerance, and increased nervous excitability. 10. Myasthenia gravis.
Accompanied by damage to muscle tissue. The main symptom is increased weakness. Fatigue is especially acute in the eye muscles. Symptoms are usually eliminated with the use of special medications that increase muscle tone. 11. Scleroderma. Concerns connective tissue.
Baldness due to alopecia areata
If a person begins to lose a large amount of hair, large bald spots form on the scalp, this may be due to the manifestation of alopecia areata (alopecia areata). In this disease, the immune system attacks hair follicles in healthy people.
This pathology is characterized by hair loss, and baldness occurs in areas that have a rounded shape. As a result, the patient may lose all hair on the scalp and body.
Alopecia areata is an unpredictable disease, and there is no effective definitive treatment for this disease.
Hair growth sometimes “restarts” on its own; some procedures can stimulate its renewal. A dermatologist may prescribe corticosteroids and some topical medications that can help restore hair thickness or slow down hair loss, and may also suggest a hair transplant to the patient.
Cleansing the body of toxins is the basis for self-regulation of the immune system
This group of diseases includes autoimmune thyroiditis (Hashimoto's thyroiditis), Graves' disease (diffuse toxic goiter), type 1 diabetes mellitus, etc.
Unlike many autoimmune diseases, this particular group of diseases does not require immunosuppressive therapy. Most patients are observed by endocrinologists or family doctors (therapists).
A very broad group. Treatment of these diseases is the prerogative of neurologists. The most well-known autoimmune diseases of the nervous system are:
- Multiple (multiple) sclerosis;
- Guillain-Bart syndrome;
- myasthenia gravis.
Common diseases and their symptoms
Many autoimmune diseases usually have very similar initial symptoms. Thus, people with this type of disorder usually feel:
- muscle pain;
- fever;
- hair loss;
- fatigue;
- swelling and redness of the skin;
- difficulty concentrating;
- skin rash;
- numbness and tingling in the arms and legs.
In some cases, such as people with type 1 diabetes, other symptoms such as extreme thirst, weight loss and fatigue are also observed. Irritable bowel syndrome, on the other hand, can cause abdominal swelling, abdominal pain, and diarrhea.
In most cases, symptoms are temporary and may change over time. The period in which most symptoms occur is called crisis, and the period in which symptoms cease is called remission.
There are a lot of autoimmune diseases, each disease has its own characteristics in the clinical picture, so it is difficult to determine common symptoms.
The diseases listed above develop gradually and, as a rule, haunt a person throughout his life.
The most common autoimmune diseases:
- With rheumatoid arthritis, the patient's small joints are affected. As the disease progresses, severe pain, swelling, fever, and general muscle weakness occur.
- The second equally common autoimmune disease is multiple sclerosis. The second name is nerve ending disease. With multiple sclerosis, the patient begins to feel strange tactile sensations and sharply loses body weight. In addition to these symptoms, this disease also causes muscle spasms and memory impairment.
- With diabetes, there is frequent urination and the person is constantly thirsty. In type 1 diabetes, a person depends on insulin throughout his life.
- One of the most dangerous autoimmune diseases is vasculitis. With this disease, damage to the circulatory system occurs. The affected vessel becomes fragile as the disease progresses, so they bleed from the inside. As a rule, the prognosis for vasculitis is unfavorable.
- Systemic diseases also include lupus erythematosus. This disease harms the entire body. Clinical picture: pain in the heart area, red spots of irregular shape on the skin, itching occurs.
- When a patient develops huge blisters on the surface of the skin, the disease is called pemphigus. The blisters themselves are filled with lymph, and the disease is accompanied by a pronounced clinical picture.
- The autoimmune disease Hashimoto's Thyroiditis, which affects the thyroid gland. The patient experiences drowsiness, the skin becomes rough, and there is an increase in body weight.
- Graves' disease also affects the thyroid gland. The main mechanism for the development of an autoimmune disease is that the thyroid gland begins to actively produce hormones, in particular thyroxine. Therefore, this disease can be distinguished from Hashimoto’s thyroiditis by its symptoms. With Graves' disease, weight loss occurs and nervous irritability occurs.
A common autoimmune disease is scleroderma, a chronic connective tissue disease. Clinical picture: degenerative changes are observed not only in the joints and skin, changes also affect internal organs.
Diagnostics
At the initial stage, a physical examination of the patient is prescribed, and a family history is also collected.
Laboratory diagnostics: blood test (general), blood test for autoantibodies.
General diagnosis: biopsy, a tissue sample is taken from the affected area.
Instrumental diagnostics include x-rays and tomography.
Classification of immunodeficiencies in children: primary and secondary
One type of immune system disorder is congenital primary immunodeficiency, which is caused by genetic damage in the immune system, is rare and usually manifests itself at an early age.
Most primary immunodeficiencies are inherited autosomal recessively or linked to the X chromosome.
When collecting a family history, the doctor needs to find out whether there were any consanguineous marriages in the family and conduct genealogical research. If necessary, the patient should be sent to a geneticist and have a chromosome analysis done.
Often this type of immunodeficiency is accompanied by malformations of organs and systems, manifested by continuous acute diseases and rapidly developing chronic diseases.
The frequency of primary immunodeficiencies varies from 1:500 (selective deficiency of IgA production) to 1:5,000,000 (severe combined immunodeficiency).
According to the classification, primary immunodeficiencies are of various types:
- insufficiency of humoral immunity;
- insufficiency of cellular immunity;
- combined deficiency of humoral and cellular immunity;
- phagocyte deficiency;
- complement deficiency.
Secondary immunodeficiency is not a manifestation of genetic defects. It happens:
- induced, that is, caused by stress and other factors that suppress the immune system, which include infections, antibiotics and hormones, trauma, radiation, etc.;
- spontaneous secondary immunodeficiency in children and adults (without a clearly identified cause) is the most common form of immunodeficiency;
- acquired - AIDS.
Diseases that should alert doctors to immunodeficiency!
1. Mother's illnesses during pregnancy. The most dangerous are the HIV virus and the rubella virus. HIV causes a deficiency of humoral and cellular immunity, and the rubella virus causes a deficiency of humoral immunity. But other maternal diseases also play an important role (chlamydia, toxoplasmosis, candidiasis, herpes, cytomegalovirus, etc.).
2. Mother's age and baby's birth weight. In premature infants (less than 30-32 weeks), due to a lack of maternal IgG received through the placenta, hypogammaglobulinemia is noted. Low birth weight infants are more susceptible to infections.
3. Complications after transfusion of blood components.
4. Inflammatory diseases of the digestive tract: stomatitis, gingivitis, periodontitis, esophagitis, gastritis, gastroduodenitis, colitis, enterocolitis, cholecystitis, gastric ulcer, duodenal ulcer, infectious gastroenteritis; subcompensated and decompensated dysbacteriosis.
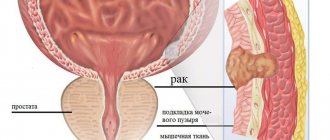
5. Inflammatory diseases of the genitourinary system.
6. Congenital viral diseases in children (congenital herpes, Epstein-Barr virus, cytomegalovirus, enterovirus, etc.); malnutrition and related conditions of the child.
7. Frequent ARVI, acute and chronic viral infections, including herpes, Epstein-Barr virus, cytomegalovirus, enterovirus, mononucleosis, warts, genital warts, human papillomavirus, hepatitis B and C, molluscum contagiosum (dermotropic virus), etc. ; chlamydia, toxoplasmosis, including congenital toxoplasmosis.
8. Various fungal infections (fungal infection, fungus, mycosis), including candidiasis, trichophytosis, ringworm.
9. Chronic respiratory diseases: chronic bronchitis, obstructive bronchitis, recurrent bronchitis, bronchiectasis, chronic pneumonia, etc.
10. Diseases of the skin and its appendages: various dermatitis, psoriasis; furunculosis, streptoderma, staphyloderma, pityriasis rosea, pyoderma, candidiasis.
11. Various neuroinfections.
12. Various oncological diseases and many other diseases of children and adults.
Treatment
Let us immediately note that diagnosis is not always as simple and accurate as we would like. To identify the disease, it is necessary to conduct a special blood test. But often the patient has to suffer for a long time, suffering from existing symptoms, before the doctor refers him to the necessary research.
In medical practice, a number of markers are used that can confirm or refute the presence of health problems. This requires a comprehensive analysis: • general blood test. The main indicator here is the ESR level, or rather its significant excess of the norm; • blood chemistry.
Rheumatoid factor is determined, and in inflammatory processes - C-reactive protein; • immunological tests. They are performed to confirm the diagnosis and isolate the titer of autoantibodies. Their severity and stability are assessed. Autoimmune diseases are characterized by persistent and clearly visible hyperproduction.
If we talk about dysfunction of the thyroid gland, the components in relation to which painful reactions are noted are thyroglobulin (TG), the enzyme thyroid peroxidase (TPO) and the TSH receptor. Therefore, markers in the blood are examined in a complex manner - anti-TG anti-TPO. According to diagnostic results, sometimes only one marker is elevated. It happens that both markers are deviated from the norm.
It should be understood that the accuracy and quality of diagnosis is strongly influenced by proper preparation for testing. Therefore, before donating blood, it is necessary to avoid drinking alcohol, reduce physical activity and try to avoid stress and emotional outbursts. It is also important to stop using all medications.
In order for the treatment of autoimmune diseases to be as effective as possible, you need to understand which doctor to contact. Considering that various organs can be affected, depending on the situation, the help of the following doctors will be relevant: • urologist. She deals with kidney problems, so she can help, for example, with lupus erythematosus;
• rheumatologist. Treats joint diseases, prescribes treatment for rheumatoid arthritis, scleroderma, or systemic lupus erythematosus; • endocrinologist. Specializes in hormonal disorders and dysfunction of hormonal glands, such as the thyroid gland. He will be able to draw up a treatment regimen for diabetes or problems with the thyroid gland;
• neurologist. Specializes in nervous disorders such as multiple sclerosis or myasthenia gravis; • hematologist. It should be contacted for blood diseases and any forms of anemia; • gastroenterologist. Helps solve problems with the digestive tract; • dermatologist. Specializes in diseases of the skin, hair and nail plates.
If we talk directly about the tactics of treating autoimmune diseases, we immediately note that there is no single scheme here. Considering that there are many variants of diseases, doctors select complex therapy on an individual basis. It all depends on the diagnosis, stage of the disease and characteristics of the clinical picture.
Based on these factors, specialists can prescribe the following treatment for autoimmune diseases: 1. Relief of symptoms. If the pain is minor, over-the-counter medications will be prescribed, for example, Aspirin or Ibuprofen. If a person complains of severe pain, the doctor will prescribe medications that are sold only by prescription.
They will help relieve symptoms, cope with swelling, depression, sleep disorders, increased fatigue and other symptoms.2. Replacement therapy. It is based on the introduction into the body of substances that it is not able to produce on its own. A striking example is type 1 diabetes.
Here, the body cannot produce insulin in the required amount, so the hormone is administered artificially through injections to maintain normal glucose levels. Also very often, replacement therapy is practiced for diseases of the thyroid gland. Patients are prescribed medications to help restore hormonal balance. 3.
Suppression of the immune system. Here we are talking about drugs that suppress the activity of the immune system. They allow you to control the processes occurring in the body and preserve the functions of its organs. Similar drugs are used in the treatment of patients suffering from lupus. They help control the inflammatory process in the affected areas.
Quite often, doctors prescribe chemotherapy to relieve inflammatory processes. It differs from therapy for cancer in the minimal doses of the active substance. Drugs called anti-TNF are also used. They block inflammatory processes and are useful for arthritis or psoriasis.
It should be noted that any treatment for autoimmune diseases is accompanied by side effects, so experts do not stop there and continue to search for drugs that could be more effective and safe.
The occurrence of 1 or 2 of the above symptoms is not sufficient to make a diagnosis. But this is already a reason to look for a doctor.
There is no single test to diagnose most autoimmune diseases. Therefore, different tests may be required.
Typically, an antinuclear antibody test is the first test requested when autoimmune diseases are suspected. A positive result indicates that there is an ongoing autoimmune disease, but the test is not able to identify the specific disease.
The doctor may also order blood tests to see how inflammation levels in the body are progressing or other tests to look for specific antibodies, which are usually done by a specialist once there is an idea of what disease is affecting the patient.
Some specialists who treat autoimmune diseases:
- Rheumatologists in cases of arthritis or Sjögren's syndrome;
- Endocrinologists for the treatment of autoimmune thyroid diseases such as Graves' or Addison's diseases;
- Dermatologists, for psoriasis;
- Gastroenterologists, when the immune system attacks the gastrointestinal tract, as in celiac disease and Crohn's disease.
Other doctors who can treat autoimmune diseases or help manage symptoms include physical therapists, nephrologists, neurologists, hematologists and internists.
The most widely used drugs to treat autoimmune diseases in general are nonsteroidal anti-inflammatory drugs, such as naproxen sodium or ibuprofen, and immunosuppressive drugs to regulate the activity of the immune system. Immunosuppressants help control the disease and maintain the integrity of the affected organ.
Your doctor may also prescribe additional remedies to relieve pain, fatigue, swelling, and rashes.
Having a balanced and healthy diet and regular exercise also help maintain the symptoms of autoimmune diseases.
Certain diseases, such as type 1 diabetes, require insulin injections to regulate blood sugar levels. In cases of autoimmune thyroid disease, hormone replacement therapy may be required.
That is, each case is a separate case. It is extremely important to consult a doctor to determine the best treatment for your specific illness.
The list of doctors is quite extensive, since all autoimmune diseases are divided into several categories.
If a patient has a systemic or mixed form of an autoimmune disease during a diagnostic examination, then it is necessary to undergo an additional examination by specialized specialists.
For example: cardiologist, hematologist, neurologist, dermatologist, endocrinologist, as well as gastroenterologist and pulmonologist.
Before prescribing the drug, the doctor assesses the general condition of the patient and the type of disease.
Treatment regimen:
- Prescribed drugs to cleanse the intestines, blood, blood vessels and liver.
- Oxidant therapy, which includes: iodine therapy or ozone therapy.
- Antioxidant therapy (include freshly squeezed juices in the diet, take vitamins from group E, C and A).
- Metabolic restoration of the liver.
- Unsaturated fatty acids (Omega 3-6-9) are prescribed. The drugs help quickly restore cell membranes.
- Taking microelements.
- Antiparasitic therapy is prescribed.
- Detoxification is carried out. Most often, the drug Reosorbilate or Heptral is used in treatment.
- Restores blood pH.
- Yoga detox combined with oxygen enrichment.
Vitamin C in food
For autoimmune diseases, Prednisolone or Cyclophosphamide may be prescribed. The first drug belongs to the group of corticosteroids. The hormonal drug is intended for local and systemic use.
Cyclophosphamide is a cytostatic antitumor drug. The active components of the drug have a fairly strong alkylating spectrum of action.
Important! Prednisolone and Cyclophosphamide have contraindications for use. In order to avoid serious adverse reactions, you need to choose the right dosage; your doctor will help you with this.
If the drugs do not bring a positive result, then Azathioprine or Methotrexate can be used as a treatment for autoimmune diseases. The first drug has an immunosuppressive spectrum of action; do not take it if you are hypersensitive to azathioprine.
Methotrexate, the main component of methotrexate, contains 2.5 mg per tablet. The drug belongs to the group of antimetabolites - folic acid antagonists.
As a treatment, the patient may be prescribed immunomodulatory drugs of natural origin. The preparations must contain thymalin, a component obtained from the thymus gland of animals, as well as cordyceps, which is obtained from the mycelium of the cardiceps fungus. With the help of such means, you can quickly restore the balance between T-helper and T-suppressor lymphocytes, which in turn stimulate humoral and cellular immunity.
Red, scaly patches due to psoriasis
Psoriasis is an autoimmune disease that is associated with inflammation and is the result of increased activity of skin cells. New skin cells are formed too quickly, and the body cannot get rid of old ones quickly enough. As a result, skin cells accumulate and a silvery, scaly, red, itchy rash appears, most often on the knees, elbows, lower back and scalp.
Psoriasis can be treated with:
- various creams;
- oral medications;
- phototherapy;
- injectable biological drugs;
- lifestyle changes.
"Treatment that targets the inflammation associated with psoriasis may help relieve symptoms of the disease," says J. Mark Jackson, MD, clinical professor of dermatology at the University of Louisville in Kentucky.