Adnexitis is one of the most common diseases of the female reproductive system. It is an inflammation of the appendages and fallopian tubes, and, according to statistics, almost every woman has encountered this pathology in practice at least once.
Adnexitis is called a seasonal disease, since the number of exacerbations occurs in the cold season, when the risk of hypothermia is highest. In fact, the mechanism of inflammation is much more complex than simple exposure to low temperatures, but nevertheless, a sharp increase in the number of gynecologist patients with this disease is associated with cold weather.
The question naturally arises: is it possible to treat a diagnosis of adnexitis at home and what methods exist for this?
Causes of adnexitis
Inflammation of any organ occurs under the influence of two factors: a bacterial or viral pathogen and a decrease in general or local immunity.
The causative agents of adnexitis are:
- streptococci;
- gonococci;
- staphylococci;
- tuberculosis bacillus;
- coli;
- fungi.
They enter the body sexually, during surgical interventions, after infectious diseases (flu, pneumonia, etc.). The infection may remain in the body for a long time, but the immune system will prevent the development of inflammation, so bacteria and viruses will be in “sleep mode”.
Under the influence of a provoking factor, the clinical picture of the disease can manifest itself in full. Such a factor may be stress, somatic pathology, sudden climate change, pregnancy or hypothermia. When immunity decreases, the disease becomes active or the person becomes susceptible to the penetration of pathogenic viruses and bacteria into the body.
Thus, it becomes obvious that the key to successful treatment is to destroy pathogenic microorganisms, eliminate inflammation caused by their presence, and strengthen the immune system.
Conditions for the development of infection
Acute right-sided salpingoophoritis is caused by a variety of specific and nonspecific microflora. The causative agents of specific inflammation of the uterine appendages are most often tuberculosis bacillus, gonococcus and diphtheria corynebacterium. Nonspecific acute adnexitis is caused by all kinds of pathogenic and opportunistic microflora:
- Staphylococci.
- Streptococci.
- Trichomonas.
- Candida fungi.
- Chlamydia.
Infection can affect the appendages in two ways: descending and ascending.
Descending infection and inflammation of the appendages occurs when pathogenic microflora is introduced through the circulatory and lymphatic systems during various infectious pathologies within the body. Ascendingly, microorganisms enter the uterine appendages through the lower part of the reproductive system when:
- Intrauterine surgical interventions: abortion, therapeutic and diagnostic curettage.
- Placement of an intrauterine contraceptive device.
- Difficult childbirth, accompanied by injuries and ruptures.
- Sexual contacts without a condom.
- Neglect of intimate hygiene rules.
For the development of an inflammatory process in the fallopian tube and ovary, infection alone is not enough. In order for adnexitis to develop, a decrease in immunity is necessary, provoked by hypothermia, stress, and bad habits.
Why is adnexitis dangerous?
The main danger of any somatic disease is the increased load on the human immune system. If the disease becomes chronic, it becomes a source of chronic infection, which in turn causes autoimmune diseases, which are currently incurable.
Inflammation of the ovaries and fallopian tubes often causes disruption of reproductive functions in the body. If the inflammation is localized in the ovary, then its capsule thickens due to the proliferation of connective tissue and cannot rupture during ovulation so that the egg can be fertilized. When the fallopian tubes become inflamed, a problem arises in their patency. In addition, chronic adnexitis can cause ectopic pregnancy.
In addition to reproductive dysfunction, the digestive tract also suffers: adhesions that occur in the peritoneum lead to frequent diarrhea, constipation, flatulence, and pain.
Prevention
Having learned what it is - right-sided adnexitis, you need to find out how to prevent it. The main measures to prevent inflammation of the uterine appendages are:
- Regular hygiene of female genital organs.
- Protected sex.
- Prophylactic administration of antibiotics during intrauterine procedures.
- Strengthening the immune system - a healthy lifestyle, avoiding hypothermia, vitamin therapy.
At the first symptoms of adnexitis, you should not delay contacting a doctor, so as not to provoke the occurrence of serious and dangerous complications.
Diagnostics
The symptoms of any disease vary depending on what form we are talking about: chronic or acute. Acute adnexitis is characterized by such symptoms as:
- heat;
- abdominal pain;
- discharge from the genital tract with pus;
- signs of intoxication (nausea, headache, weakness, sweating).
The chronic form of adnexitis is a consequence of incorrect or incomplete treatment of the acute form. The clinical picture in the chronic form is less pronounced and weak. But when exposed to any provoking factor, acute adnexitis is highly likely to develop. Symptoms and treatment at home - knowledge that will allow you to quickly recognize the disease and take the necessary actions before visiting a doctor.
Chronic adnexitis is characterized by regular aching pain in the lower abdomen, disruption of the menstrual cycle, and discharge. The pain can appear before menstruation or during sexual intercourse and can be quite severe.
Of course, a doctor must make a final diagnosis before prescribing treatment. But knowing the symptoms of the disease allows you to make a correct guess about what kind of disease you are talking about, which means that thanks to this you can quickly get to the right specialist.
Inflammation of the appendages: causes, symptoms, treatment
In the general structure of diseases in the gynecological field, inflammation of the uterine appendages is in the leading place. This pathological process in most cases forces women of reproductive age (from 18 to 45 years) to visit a specialist. Quite often, inflammation of the uterine appendages occurs together with endometritis, as a result of which serious negative health consequences such as infertility and miscarriage may occur.
Inflammation of the appendages in women - what kind of disease is it?
The fallopian tubes and ovaries are also called the uterine appendages. The fallopian tubes are long, narrow cords (about 10 centimeters in length) extending from the corners of the uterus, in the curved area of which the ovaries are located. They are localized on each side one at a time and are attached to the walls of the peritoneum through the mesentery. Nutrition of the pelvic organs is carried out with the help of vessels and nerves passing through the mesentery.
Inflammation of the appendages is characterized by an inflammatory process that occurs in the pelvis and is localized in the fallopian tubes and ovaries. The reason for this is the vital activity of bacteria and viruses as a result of their penetration into the appendages, and the main contributing factor is the weakening of local and general immunity due to hypothermia of the body. The signs of this pathology are varied, they can manifest as scanty vaginal discharge, nagging pain in the lower abdomen, menstrual irregularities, and symptoms of acute inflammatory diseases.
An inflammatory process may occur in the ovaries, this disease is called oophoritis, as well as in the fallopian tubes - salpingitis. If the uterine appendages are affected simultaneously, and this happens in the vast majority of cases, salpingoophoritis occurs, which is also called adnexitis. It mainly affects patients aged 18 to 45 years; inflammation of the appendages in women occurs extremely rarely during adolescence and menopause.
According to statistical information from the National Guide to Gynecology, up to 60% of women at least once discovered symptoms of inflammation of the appendages and consulted a specialist; approximately 20% of patients who have had this disease are subsequently diagnosed with infertility; 5% developed complications of a purulent nature that required surgical intervention; to cure salpingoophoritis, every second patient is forced to stay in the hospital; inflammation of the appendages increases the risk of developing an ectopic pregnancy up to five times.
Salpingo-oophoritis belongs to a broad group of inflammatory diseases of the pelvic organs, which also includes endometritis (an inflammatory process in the inner mucous layer of the uterus), myometritis (inflammation of the muscular ball of the vagina), pelvioperitonitis (a local infectious-inflammatory process of the pelvic serous layer).
A correct diagnosis can only be made after a comprehensive diagnosis. The examination should include instrumental, laboratory, and differential techniques.
Causes of inflammation of the appendages
Salpingoophoritis is an infectious disease. Most often, during the examination, microorganisms representing opportunistic flora are detected. In the presence of immunodeficiency states, the causative agents of the disease are often fungi (including fungi of the genus Candida).
Possible culprits for inflammation of the appendages include:
- Trichomonas;
- yeast-like fungi;
- Staphylococcus aureus and Staphylococcus epidermidis;
- gonococci;
- streptococci;
- chlamydia;
- enterobacteria (which includes E. coli);
- mycoplasma, ureaplasma;
- bacteroides.
Determining what caused the occurrence of salpingoophoritis is only possible by carrying out a comprehensive examination. As a rule, a mixed type infection is detected.
Factors that provoke the appearance of adnexitis are:
- neglect of personal hygiene standards;
- overly active sex life, constant change of partners and, as a result, the occurrence of sexually transmitted infections;
- artificial termination of pregnancy;
- complicated labor;
- use of intrauterine contraceptives;
- surgical manipulations in the uterine cavity performed for diagnostic and therapeutic purposes.
Often there is a “transfer” of the inflammatory process from the cervix and vagina to the appendages and its spread to all pelvic organs. The infection is actively developing due to the delayed start of treatment, as well as if the therapy was chosen incorrectly by the specialist. It should be noted that the risk of salpingoophoritis increases significantly in patients with immunodeficiency.
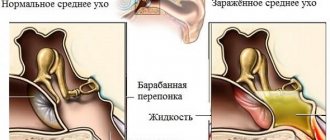
Signs of inflammation of the appendages
During the development of the inflammatory process, the uterine appendages thicken and increase in size. Quite quickly, the patency of the fallopian tubes is disrupted due to the formation of adhesions; there is also an accumulation of inflammatory secretions and the formation of hydrosalpinx and pyosalpinx (the appearance of purulent fluid in the tubes). It is possible for the affected fallopian tubes to connect with the layers of the pelvic peritoneum and nearby loops of the large intestine. Free fluid may appear in the pelvis.
Acute inflammation of the uterine appendages is characterized by such signs as the occurrence of severe pain in the lower abdomen, fever, and the manifestation of dysfunction in the process of emptying the bladder. If treatment is started on time, the patient can count on a favorable outcome and full recovery. In the absence of proper therapy, the disease will become chronic.
Chronic inflammation of the appendages is manifested by the following symptoms:
- the presence of moderate nagging pain in the lower abdomen;
- pain in the groin and lower back;
- painful sensations during intimacy;
- disruption of the process of emptying the bladder;
- disruptions in the menstrual cycle - irregular periods, the presence of bleeding between them;
- malaise, general weakness of the body.
The chronic form of salpingoophoritis is not characterized by an increase in temperature. The course of the disease can last for several years, exacerbations will be replaced by remissions. With acute inflammation of the uterine appendages, the patient feels increased pain in the lower abdomen and fever appears. At the time of exacerbation of the disease, treatment is carried out in a hospital.
For a long period of time, chronic salpingoophoritis may not manifest clinical symptoms. The only thing a woman can pay attention to is the inability to get pregnant for a long time. Often, chronic inflammation of the appendages is discovered randomly during diagnostic studies when other diseases are suspected.
Possible complications
If salpingoophoritis is not treated, there is a high risk of a number of complications.
Tuboovarian formation
This is an inflammation of the appendages in the second stage of development, resulting in the formation of a tumor, adhesions between the ovaries, fallopian tube and nearby organs. Also often diagnosed are acute purulent salpingitis (suppuration of the fallopian tube), purulent tubo-ovarian abscess (purulent melting of the tissues of the fallopian tube and ovary with the formation of a single cavity surrounded by a pyogenic capsule).
The development of purulent complications causes a sharp deterioration in the patient’s well-being and body condition. The body temperature rises, sharp, severe pain occurs in the lower abdomen or on the side where the lesion occurred. Pus begins to discharge profusely from the vagina. Severe intoxication can cause diarrhea. If there is a purulent formation in the pelvic cavity, delay in starting treatment can lead to the most negative consequences; self-medication is impossible. Emergency hospitalization to a gynecological hospital is indicated. Therapy is carried out through surgery.
Pelvioperitonitis
This is an inflammatory process, the development of which occurs in the pelvic peritoneum against the background of ongoing infectious processes. In most cases, pelvioperitonitis occurs as a consequence of the inflammatory process of the uterus or its appendages; sometimes it can be the result of labor, which occurs with complications. Inflammation is provoked by the action of pathogens such as staphylococci, chlamydia, E. coli, gonococci, and viruses. This pathology can also appear as a side effect after surgery or installation of an intrauterine device.
Signs of pelvioperitonitis:
- sharp, severe pain in the lower abdomen;
- increase in body temperature to 39-40 degrees;
- feeling of chills;
- rapid heartbeat;
- feeling of dry mouth;
- nausea, vomiting (may happen once);
- bloating;
- redness of the skin;
- pain during defecation and urination.
If timely medical care is not provided, the inflammatory process may spread beyond the boundaries of the pelvis and the development of peritonitis (inflammation of the parietal and visceral layers of the peritoneum) and sepsis (a systemic inflammatory reaction in response to a local infectious process, also called blood poisoning).
Ectopic pregnancy
A complication of pregnancy in which the attachment of a fertilized egg occurs outside the uterine cavity due to the presence of adhesions in the fallopian tubes as a result of the localization of the inflammatory process there. With rare exceptions, ectopic pregnancies are not viable and are often life-threatening to the woman due to the excessive internal bleeding that begins after a fallopian tube rupture or miscarriage (usually occurring between 6 and 9 weeks of pregnancy). An ectopic pregnancy is a condition that requires urgent medical attention, otherwise it can be fatal.
Infertility
As a result of a pronounced adhesive process in the fallopian tubes, this organ becomes impassable, as a result of which the sperm and egg do not meet, and pregnancy does not occur. If complete obstruction of the fallopian tubes is diagnosed, conception is possible only through in vitro fertilization (IVF method).
Diagnostic procedures
If inflammation of the appendages is suspected in women, a gynecological examination is performed. The doctor conducts a survey of the patient, taking into account the presence of an intrauterine device, the number of abortions, complicated labor, the number of sexual partners, general health and complaints. During the examination on the chair, enlarged, painful uterine appendages are revealed on one or both sides.
For laboratory tests, general blood and urine tests are prescribed - to assess the general condition of the body and the functioning of internal organs, bacteriological culture of flora and microscopic examination of a smear taken from the vagina, cervical canal and urethra in order to determine the causative agents of the disease and their concentration. Such information can help assess the degree of inflammation in the pelvis. If sexually transmitted infections are detected, both partners must be treated. If this is not done, there is a high risk of relapse of the disease.
An ultrasound examination of the pelvic organs can detect signs of an inflammatory process - an increase in the size of the fallopian tubes and ovaries, the presence of adhesions, and the presence of free fluid in the pelvic cavity. An ultrasound performed through the vagina (transvaginal) allows the doctor to timely see purulent complications, pelvioperitonitis and not mistake salpingoophoritis for an ovarian tumor.
It is also possible to use instrumental diagnostic methods - diagnostic laparoscopy to identify purulent formations and adhesions in the fallopian tubes, hysterosalpingography (x-ray examination of the uterus using contrast) to detect pathological changes in the fallopian tubes and assess their patency.
Treatment of salpingoophoritis
Treatment of inflammation of the appendages in women is carried out in accordance with the severity and form of the disease, the presence of complications. The choice of therapy is made only after a comprehensive examination of the patient. If it is decided to treat salpingoophoritis with medication, broad-spectrum antibiotics are prescribed - macrolides, cephalosporins and others. Which drug will be used is decided depending on the pathogen detected and its sensitivity. Usually the course of treatment lasts up to ten days. First, antibiotics are administered intravenously or intramuscularly, then it is possible to use drugs in tablets. Also, for severe pain, analgesics are prescribed, and for fever, antipyretic and detoxifying agents are prescribed. Probiotics help restore the vaginal microflora, local antiseptics and anti-inflammatory drugs help eliminate the inflammatory process in the genital tract. When the course of treatment comes to an end, a control culture is taken from the patient’s cervical canal.
After the acute inflammatory process subsides, it is possible to begin non-drug therapy, for example, physio - electrophoresis, magnetic therapy, UHF. Referring a patient to spa treatment can also be effective.
Treatment through surgery is also an option. Indications for it are the futility of conservative methods, the presence of purulent complications, the desire to conceive a child against the background of obstruction of the fallopian tubes and adhesions. Most often, a laparoscopic operation is performed through punctures in the abdominal wall, during which a specialist removes purulent formations, dissects adhesions and treats the pelvic cavity with antiseptic agents. In serious cases, it is possible to remove the affected uterine appendages followed by hormone replacement therapy.
Prevention
To prevent inflammation of the appendages, it is recommended:
- give up promiscuous sex life and do not forget that frequent changes of partners can lead to the presence of sexually transmitted infections;
- use reliable means of contraception with non-regular partners - in particular, a condom;
- do not neglect regular preventive examinations with a gynecologist;
- promptly treat inflammatory processes of the cervix and vagina;
- If you experience scanty vaginal discharge, nagging pain in the lower abdomen, or menstrual irregularities, consult a doctor immediately;
- strengthen the immune system, adhere to the principles of a healthy lifestyle, eat a balanced diet, observe a work and rest schedule, devote time to walks in the fresh air, do not abuse alcoholic beverages and nicotine, avoid hypothermia and stress.
Treatment
By considering information about symptoms and complications, you can understand the seriousness of the disease called adnexitis. Treatment at home is indicated in most cases; hospitalization in a hospital is extremely rare. It is usually due to the fact that either the woman cannot bring down the high temperature, or the signs of intoxication from inflammation are too pronounced.
In its normal course, the disease can be treated on an outpatient basis. That is, at home, on your own, according to the doctor’s recommendations.
There are several well-known methods of treating a disease called “adnexitis”. Treatment at home - tablets, injections, traditional recipes - should be considered in detail in order to understand the effectiveness and safety of the methods.
Antibiotics
There is a treatment plan that is prescribed based on diagnostic data, the patient’s condition, medical history and concomitant diseases. That is, different methods can be effective, but by default the one that has proven its maximum effectiveness with minimal danger is used. For adnexitis, this treatment method is to take antibiotics.
Treatment of adnexitis at home with antibiotics is highly effective due to the fact that the drug destroys the very cause of the disease - pathogenic bacteria. However, when treating at home, it is strictly forbidden to “prescribe” the drug yourself. To prescribe, it is necessary to do a culture, which will determine sensitivity to different types of antibiotics.
In addition, for a productive result, which treatment of adnexitis should have at home, the drugs must be used in a certain dosage. If the dose is selected incorrectly, you can either provoke the transition of the disease into a chronic form, or cause the body to become resistant to the drug. The latter is a very serious problem, because the lack of effect of the medicine can further pose a threat to human life.
It is also important to stop taking the medication in a timely manner - often when self-medicating, people stop taking the drug immediately after the symptoms of the disease pass. This approach is fundamentally wrong, because if undefeated bacteria that provoked the disease remain in the body, they will again lead to the development of pathology, while pathogenic microorganisms will become resistant to the previously taken antibiotic. Taking antibiotics for too long destroys beneficial microflora and suppresses the immune system.
Regardless of whether there is an acute form of the disease or chronic adnexitis, treatment at home with antibiotics is equally effective. The most commonly prescribed are Zomax, Cedex, Erythromycin, Metronizadol, Ceftriaxone, etc.
Antimicrobial drugs as the main treatment for the disease
Since the causative agent of the pathology is often an infection, antibacterial therapy plays a leading role. If the result of bacterial culture from the vagina is negative, it is difficult to identify the causative agent of chronic adnexitis. For this reason, gynecologists prescribe drugs with a broad spectrum of action, the duration of treatment is at least two weeks. Antibiotics for chronic adnexitis, most often used, are described in the table.
| Name of the drug | Action provided | Directions for use and dosage |
| Amoxiclav. | The main active component of the drug, indomethacin, has a pronounced bactericidal effect against most gram-positive and gram-negative microorganisms. Noone is destroyed by β-lactamase secreted by bacteria. To inactivate it, clavulanic acid was added to the antibiotic composition. | The required amount of the drug is calculated individually. It can range from 625 mg to 1 g every 12 hours. |
| Augmentin. | ||
| Ceftriaxone. | This drug belongs to third generation cephalosporin antibiotics. The medication is available in the form of injections, can cause an allergic reaction and is used only in hospital settings at the late stage of chronic adnexitis. | The contents of the bottle with powder are dissolved in saline or water for injection and administered intravenously or intramuscularly, 1 g 1-2 times a day. |
| Doxycycline. | Belongs to the group of tetracyclines and is effective against gonorrhea and other sexually transmitted diseases. | 100 mg twice a day. |
| Digital | They contain ciprofloxacin, an antimicrobial agent from the fluoroquinolone group. It has a very wide spectrum of action and is prescribed not only for chronic adnexitis, but also for bacterial infections of any localization. However, due to its high toxicity, it is prescribed when other drugs are ineffective. | 0.5 g twice a day. |
| Tsiprinol. | ||
| Nolitsin. | Contains norfloxacin. Bacteria rarely develop resistance to this drug. | 400 mg morning and evening. |
In parallel with taking antibiotics, medications are indicated to normalize the intestinal microflora. For example, Linex, Bio-gaia, Bifiform, Enterozermina. This will avoid dysbiosis and associated digestive disorders. Women with impaired liver and kidney function need constant medical supervision.
Other drugs
In addition to antibiotics, the doctor may prescribe medications for symptomatic treatment. First of all, we are talking about painkillers, since adnexitis in the acute stage causes quite sharp pain in the lower abdomen.
If chronic adnexitis is present, treatment at home may include taking anti-inflammatory drugs, most often corticosteroids (Celeston, Triamcinolone, Kenacort, Cortineff). It is extremely important that the treatment plan in this case also includes antibiotics, because corticosteroids act by suppressing the immune response. If a pathological pathogen is present in the body, the picture of symptoms can develop quickly and quite strongly.
Signs
Manifestations of inflammation of the appendages depend on the form of the disease and the general health of the patient. The acute stage begins rapidly. Characteristic symptoms:
- severe nagging or cramping pain on the affected side or throughout the lower abdomen is the main sign of the disease. They intensify with sexual contact and physical activity. Irradiation to the lower back and anus is noted;
- fever (temperature above 38 degrees);
- intoxication: muscles, joints, head hurt. Weakness, sweating, tachycardia, loss of appetite are observed. There may be dyspeptic disorders;
- intense vaginal itching, aggravated by urination;
- purulent or serous discharge, unpleasant odor with advanced inflammation of the appendages;
- the menstrual cycle is disrupted, the periods become more abundant or scanty, irregular;
- non-cyclic discharge, bleeding.
Symptoms of the chronic phase of inflammation of the appendages are less pronounced, and there is often an asymptomatic course. During an exacerbation, the patient complains of mild aching pain that occurs periodically. The cycle and nature of bleeding are disrupted. Due to discomfort during sex, a woman may refuse sex. Since certain manifestations are constantly present, the quality of sexual life deteriorates significantly and libido decreases. As a result, emotional tension and irritability appear. If there are no manifestations, then it is extremely dangerous. The woman does not undergo medical examinations or see a gynecologist. In this case, inflammation of the appendages leads to the development of serious consequences for the reproductive system, including infertility.
In many cases, people come to the doctor when they cannot conceive children. If traditional treatment does not help, then you can become a mother only through in vitro fertilization.
ethnoscience
When it comes to a disease such as adnexitis, treatment at home with folk remedies cannot be an independent method of therapy. Before using any prescription, you should consult your doctor. Despite the fact that herbal infusions and infusions are considered harmless, they may well affect the drugs prescribed by a specialist, enhancing their effect or nullifying it.
In the event that traditional medicine is used as the only method of treatment, there is a serious risk of “earning” a diagnosis of “chronic adnexitis”. Treatment at home using traditional methods should be auxiliary in nature: reduce inflammation, eliminate symptoms of the disease and increase immunity. They must be used with extreme caution, because the natural ingredients that form the basis of traditional medicine often cause an allergic reaction, which is sometimes difficult to recognize when a person’s well-being is already impaired due to existing adnexitis.
Tampons
Speaking about traditional medicine, first of all you should pay attention to topical remedies. They have practically no contraindications, they are easy to use, and the effect, although not quick, is always noticeable as a result of the cycle.
The only caveat is the risk of an allergic reaction. To prevent it, you should carefully consider the composition of the recipe - if you have previously had an allergic reaction to any of the ingredients, you should not use such a remedy. And if after inserting a tampon you feel pain or discomfort, the tampon should be removed immediately and take an antihistamine.
Therefore, a disease such as adnexitis can be easily treated at home. It is important to make tampons yourself, since ready-made tampons have high absorption, so the effect of the product will not be pronounced. To make a tampon, you need to take a piece of cotton wool and wrap it in a gauze bandage. After this, the product is generously moistened with a medicinal composition and inserted deep into the vagina at night. The course of such manipulations is about 2 weeks, and the therapeutic effect will be noticeable after at least one week of treatment.
The following can be used as a composition for impregnating a tampon:
- propolis in equal proportions;
- Vishnevsky ointment;
- garlic juice (2-3 drops), warm water (20 ml) and celandine infusion (a couple of drops);
- mumiyo diluted in warm water.
It is recommended to choose one recipe and follow it through the course. If it is ineffective, you can try another prescription under the supervision of your doctor.
Infusions
Recipes intended for internal use have a complex effect on the entire body. They improve immunity, allow it to quickly eliminate inflammation, increase vitality, reducing the severity of symptoms.
However, do not assume that herbal recipes are completely safe. Many medicinal plants that are highly effective contain a high concentration of active substances. Therefore, if taken uncontrolled, there is a serious risk of causing an overdose.
Herbs with anti-inflammatory effects help with a large list of diseases, which include adnexitis. Treatment at home with a red brush is one of the most popular methods.
Red brush, or Rhodiola colda, is a unique plant that can only be found in the Altai Mountains. It can help treat diseases of almost all body systems. But most often it is recommended to use it for gynecological diseases.
The red brush has an excellent anti-inflammatory effect, but the most pronounced effect can be obtained by using it as a preventive measure rather than as a method of treatment. However, the reviews available for such treatment of adnexitis at home indicate the high effectiveness of the drug with minimal side effects.
The easiest way to use red brush is to prepare a decoction. Take one tablespoon of red brush root per glass of boiling water, and then infuse for an hour. It is recommended to eat a spoonful of natural honey while directly consuming the decoction. Do not leave the prepared broth for a long time. A glass of the product should be drunk within one day, diluting the portion with boiling water.
It is important to know that the product is incompatible with taking hormones, as well as some herbs: licorice, hops, clover, cocklebur.
Baths
Herbal baths are a proven remedy in the fight against gynecological inflammation. Everyone can take such baths, except pregnant women, people with cancer and skin diseases in the acute stage.
Thyme is the best choice for preparing a medicinal bath for a diagnosis such as adnexitis. Treatment at home involves preparing a decoction: add 200 grams of herb to three liters of boiling water, infuse for an hour and pour into a moderately hot bath one-third filled with water.
The bath should be taken in a sitting position for 20 minutes. After this, you need to wrap your body in a previously prepared sheet, without wiping yourself with a towel, and go to bed. To achieve a therapeutic effect, it is recommended to take a course of baths at least 10 times.
Given the moderate water temperature, it is important to remember that this procedure carries the risk of hypothermia from the indoor air. Therefore, the room must be preheated, for example, by turning on a hot shower for a few minutes.
Steam bath
Milk baths are recommended for women provided that they do not have menstruation or pregnancy that accompany adnexitis. Treatment at home using a bath is carried out as follows: you need to boil 3 liters of milk, pour it into a basin and sit over it for a while until the milk cools down.
The principle of operation of the method is based on heating the tissues: a rush of blood will speed up metabolism and allow the body to quickly cope with the inflammatory process. This simple treatment of adnexitis at home, reviews of the positive experience of the use of which are given by women on various forums, allows you to get rid of the chronic form of the disease.
Immediately after the steam bath, it is recommended to lie down in a warm bed. You can take baths until the symptoms of the disease completely disappear, but at least 14 times in a row.
Types of inflammatory process in the uterus and their manifestations
Experts distinguish three types of inflammation of the uterus in women, which differ from each other in the location of the pathological process. This:
- Endometritis occurring in the uterine mucosa.
- Metroendometritis, located in the membranes of the mucous membrane and muscles of the uterine body.
- Perimetritis developing in the outer membrane of the reproductive organ.
With endometritis, inflammation of the uterine mucosa is caused by the penetration of pathogens into muscle tissue. Usually it develops for a short time, later flowing into inflammation of the appendages of the genital organ. With this type of pathology, a woman experiences white discharge, which can then acquire a yellowish tint.
Over time, such discharge may become green in color, and an unpleasant odor will be felt. In addition, patients often experience increased body temperature, weakness, and pain in the lower abdomen.
If the acute form of uterine disease is not treated in a timely manner, there is a high risk that it will become chronic. Also, the chronic form can occur due to the fact that a woman’s body is negatively affected by an infection such as gonorrhea. Other causes of inflammation of the uterine mucosa can be hypothermia, abortion, and gynecological manipulation using unsterile instruments.
Metroendometritis of the uterus develops when long-term stagnation occurs in a woman’s pelvis. This may be due to incorrect location of the reproductive organ, the presence of tumors in the pelvic organs, masturbation, problems with blood circulation, or incomplete sexual acts.
In the acute form of uterine metroendometritis, patients experience increased body temperature, rapid pulse, deterioration in general condition, pain in the lower abdomen, which can radiate to the sacral part, and discharge mixed with pus or blood.
Upon examination, the gynecologist feels the increased size of the uterus, its swelling, and the woman feels pain upon palpation. The severity of symptoms depends on the extent to which the stagnation process develops, the nature of the inflammation, and where it is located.
With perimeter, an inflammatory process occurs in the outer layer of the uterus. It occurs because the pathology moves from the organ itself to the ligaments that hold it, muscle tissue, and the abdominal cavity. Thus, inflammation covers the entire surface of the uterus.
Clinical manifestations include a feeling of tension in the abdominal area, severe pain, vomiting, and high fever. There may also be problems with bowel movements and urination. If left untreated, the acute form will become chronic, which can lead to serious complications.