What is IUGR?
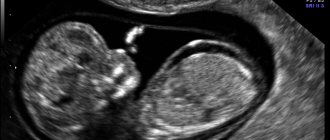
Intrauterine growth restriction is usually diagnosed based on ultrasound examination. Pathology is determined if the baby’s weight is less than the normative indicators characteristic of this period of development. In medical practice, specially designed tables are used that indicate the weight of the fetus in accordance with its gestational age, that is, the time since fertilization. This indicator is usually defined in weeks. In other words, there are certain norms for each stage of pregnancy. The basic unit of measurement in such tables is the percentile. If the fetus is less than the 10th percentile on this table, the doctor confirms the presence of pathology.
Prerequisites for the development of ventriculomegaly
Normally, each person has four cerebral ventricles. Two of them - ventriculi laterales (telencephalon) - are located in the thickness of the white matter: below the corpus callosum, symmetrically on both sides of the midline. Communication with the third of the ventricles - ventriculus tertius (diencephalon) - is carried out through the Monroe (or interventricular) foramina.
The third of the ventricles is located between the visual thalamus, it has the shape of a ring, and in its walls, formed by the gray matter of the brain, there are subcortical autonomic centers. Through the cerebral aqueduct of the midbrain, it communicates with the fourth ventricle - ventriculus quartus (mesencephalon), which is connected to the central canal of the spinal cord.
The main function of the ventricles of the brain is the synthesis of cerebrospinal fluid (CSF), which then, if there are no malformations, enters the subarachnoid (or subarachnoid) space. Impaired cerebrospinal fluid outflow provokes the development of ventriculomegaly.
Intrauterine growth restriction: causes
Sometimes, when diagnosed with IUGR, parents do not need to worry. It happens that a baby is born small in size, since his father and mother are not very tall. This physiological feature does not affect the child’s activity, mental and physical development. During pregnancy and after birth, such a baby does not need highly targeted therapy.
In all other situations, special attention should be paid to the diagnosis. This condition can lead to deviations in the development of the child or even the death of the fetus. IUGR may indicate that the baby in the womb is not eating well. This means that it does not receive sufficient nutrients and oxygen. Nutritional deficiency is usually due to the following reasons:
- Incorrect chromosome set.
- Bad habits of the mother (smoking, drinking alcohol and drugs).
- Pathogenic diseases (hypertension, anemia, diseases of the cardiovascular system).
- Incorrect location and subsequent formation of the placenta.
In addition, doctors name a number of other reasons that can also provoke intrauterine growth retardation syndrome:
- Multiple pregnancy.
- Use of medications without prior doctor's prescription.
- Childbirth after 42 weeks.
- Poor nutrition. Many women do not want to gain weight during pregnancy, so they exhaust themselves with diets. By doing this, they provoke exhaustion of the body, which leads to the development of pathology.
- Diseases of an infectious nature (toxoplasmosis, rubella, syphilis).
Why is SZVRP dangerous?
The danger of the diagnosis lies in the severity of its manifestation. So, with early diagnosis of developmental delay, there is a great chance to identify the cause and carry out benign treatment.
The risk of fetal death increases regardless of gestational age. In the first weeks of pregnancy, FGR leads to spontaneous miscarriage in 89% of cases.
The risk of complications during labor and perinatal morbidity increases. Possible death increases 7 times.
After birth, children require resuscitation measures.
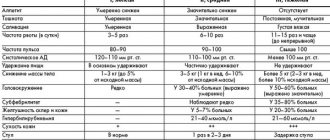
Clinical picture
What symptoms accompany intrauterine growth retardation? Signs of pathology most often appear in the early stages (approximately 24-26 weeks). A woman is not able to determine them on her own; this can only be done by a doctor. IUGR syndrome is diagnosed when the following indicators do not meet the standards:
- The size of the baby's head and femur.
- Abdominal circumference at a certain level, height of the uterine fundus.
- Volume of amniotic fluid.
- Impaired functioning of the placenta (its structure and size change).
- Fetal heart rate.
- The speed of blood flow in the placenta and umbilical cord.
In some cases, the pathology develops quite quickly and progresses without any special disturbances, that is, it is asymptomatic.
Clarifying examination
The simplest method of monitoring fetal development is to regularly measure the size of the uterus. At about 4 months it becomes possible to easily palpate it above the womb, and now at each visit the doctor will take readings. This allows the doctor to judge the size of the fetus. But the data are not very objective, because they do not take into account the thickness of the anterior abdominal wall and the amount of amniotic fluid. The only thing that can be visually determined is the woman’s build and physique. Therefore, ultrasound is now used to confirm the diagnosis. This is the most accurate study that allows you to evaluate many parameters at once, the condition of the uterus and placenta, the size of all parts of the fetal body.
Severity
- I degree. Stage 1 intrauterine growth retardation is considered relatively mild, since the developmental lag from anthropometric data corresponding to a certain stage of pregnancy is only two weeks. Timely prescribed therapy can be effective and minimize the likelihood of negative consequences for the baby.
- II degree. The developmental delay is approximately 3-4 weeks and requires serious treatment.
- III degree. It is considered the most severe form due to a delay in fetal parameters of one month or more. This condition is usually accompanied by so-called organic changes. Stage 3 intrauterine growth retardation often results in death.
Types of ventriculomegaly in the fetus
Ventriculomegaly is usually divided into three different types:
- Mild ventriculomegaly - which is characterized by a single lesion and does not require serious treatment;
- Average ventriculomegaly – characterized by an increase in the size of the ventricles up to 15 mm and causing certain disturbances in the outflow of cerebrospinal fluid;
- Severe ventriculomegaly is characterized by a pronounced enlargement of the cerebral ventricles, which is observed in the fetus against the background of other brain pathologies.
In general, one of the characteristics of the human brain is that its ventricles are somewhat asymmetrical. This asymmetry is determined during gestation. As a rule, in male children the differences are slightly more pronounced than in female children.
The term "borderline ventriculomegaly" is used when the width of the atrium of the lateral ventricle is between 10 and 15 mm. This condition greatly increases the risk of developing all kinds of anomalies in the central nervous system, as well as other systems and organs.
Isolated borderline ventriculomegaly in most cases is not accompanied by any clinically significant consequences, however, in some situations it is considered as one of the manifestations of initial brain damage caused by the negative impact of various reasons: brain malformations, its destructive lesions, infections, fetal hypoxia during the period intrauterine development, etc.
Asymmetrical form of pathology
In this case, there is a significant decrease in fetal weight with normal growth. The child is diagnosed with a lag in the formation of the soft tissues of the chest and abdomen, and abnormal development of the torso. Uneven growth of internal organ systems is possible. In the absence of adequate therapy, a gradual decrease in head size and a lag in brain development begin, which almost always entails the death of the fetus. The asymmetric variant of IUGR syndrome occurs mainly in the third trimester against the background of general placental insufficiency.
What are the ventricles of the brain, their role
The ventricles of the brain are strips of tissue necessary for the deposition of cerebrospinal fluid.
External and internal factors can lead to their increase in volume. The lateral ventricles are the largest. These formations are involved in the formation of cerebrospinal fluid. Asymmetry is a condition in which one or both cavities are enlarged to varying degrees.
Types of ventricles:
- Lateral. The ventricles are the most voluminous, and they contain cerebrospinal fluid. They connect to the third ventricle via the interventricular foramina.
- Third. Located between the visual tuberosities. Its walls are filled with gray matter.
- Fourth. Located between the cerebellum and medulla oblongata.
Diagnostic measures
If this pathology is suspected, a woman is recommended to undergo a full diagnostic examination. First of all, the doctor collects the patient’s medical history, clarifies previous gynecological diseases, and the characteristics of the previous pregnancy. Then a physical examination is carried out with mandatory measurement of the abdominal circumference, uterine fundus, height and weight of the woman.
Additionally, ultrasound examination, Doppler measurements (assessment of blood flow in the arteries and veins) and cardiotocography (continuous recording of the fetal heart rate, its activity and direct uterine contractions) may be required. Based on the results of the tests, the specialist can confirm or refute the diagnosis.
Establishing diagnosis
In order to confirm his suspicions, the doctor may additionally refer the pregnant woman for a Doppler examination of blood vessels. In this case, the specialist must evaluate the speed and nature of blood flow in them. Cardiotocography complements the examination and records the heartbeat. If the data is normal, then even with a low weight of the baby, its development is considered successful. Doppler examinations are performed free of charge upon referral from a doctor.
What treatment is required?
To determine subsequent pregnancy management tactics after confirming the diagnosis of intrauterine growth retardation, the causes of the pathology, the form and degree of the disease should be taken into account. The basic principles of therapy should be focused on improving blood flow in the uterus-placenta-fetus system. All therapeutic measures are carried out in a hospital setting. First of all, a woman needs to ensure peace, balanced nutrition and good, long sleep. Monitoring the current condition of the fetus is considered an important element of therapy. For these purposes, ultrasound examination every 7-14 days, cardiotocography and Doppler blood flow are used.
Drug treatment includes taking angioprotectors to protect blood vessels, tocolytics against muscle tension of the uterus (Papaverine, No-shpa), and general restoratives. In addition, all women, without exception, are prescribed drugs that reduce neuropsychic agitation (tincture of motherwort, valerian) and improve blood flow in the placenta (“Actovegin”, “Curantil”).
Depending on the severity of the pathology, treatment results may vary. Stage 1 intrauterine growth retardation usually responds well to treatment, and the likelihood of further negative consequences is minimized. For more serious pathologies, a different approach to treatment is required, and its results are quite difficult to predict.
Prevention of the occurrence of IUGR syndrome
To avoid the development of a pathological condition during pregnancy, all women planning to give birth to a child are recommended to undergo a comprehensive diagnostic examination. Even at the stage of preparation for conception, it is necessary to sanitize all foci of chronic infection (diseases of the genitourinary tract, carious teeth, infectious pathologies of the upper respiratory tract, etc.), as well as give up bad habits.
Very much attention should be paid to the nature of nutrition (the daily diet of the expectant mother should be complete and balanced), and also, on the recommendation of a doctor, take vitamin and mineral complexes. In particular, it is recommended to take the drug “Alvogenium” - it serves as a source of DHA (dosehexaenoic acid) and Oega-3 fatty acids, which are directly involved in the development of the child’s brain.
Drug prevention of intrauterine growth retardation involves the use of drugs that improve placental-uterine circulation (they are prescribed in the prenatal period to women at risk of developing IUGR).
Abortion
Early delivery, regardless of the stage of pregnancy, is recommended in the following cases:
- Lack of fetal growth for 14 days.
- A noticeable deterioration in the baby’s condition inside the womb (for example, a slowdown in blood flow in the vessels).
Pregnancy is maintained until a maximum of 37 weeks if, thanks to drug therapy, there is an improvement in indicators, when there is no need to talk about the diagnosis of “intrauterine growth retardation.”
Consequences and possible complications
Babies with such a pathology after birth may have deviations of varying severity; their subsequent compatibility with ordinary life will largely depend on their parents.
The first consequences appear already during delivery (hypoxia, neurological disorders). Intrauterine growth retardation inhibits the maturation of the central nervous system and its functions, which affects all systems. In such children, the body’s defenses are usually weakened; in later life, there is an increased likelihood of developing cardiovascular diseases.
Children under five years of age are often diagnosed with slow weight gain, psychomotor retardation, improper formation of internal organ systems, and hyperexcitability. During adolescence, there is a high risk of diabetes. Such children usually tend to be overweight and have problems with blood pressure. This does not mean that their daily existence will be reduced to taking medications and living in hospitals. They will simply need to pay a little more attention to their own nutrition and daily physical activity.
Some children who have been diagnosed with stage 2 intrauterine growth retardation and given appropriate treatment do not differ from their peers. They lead a normal lifestyle, play sports, communicate with friends and get an education.
How can IUGR be prevented?
The best prevention of this pathology is planning for the upcoming pregnancy. About six months in advance, future parents must undergo a comprehensive examination and treat all existing chronic diseases. Giving up bad habits, a healthy lifestyle, a balanced diet and daily dosed physical activity are the best options for preventing IUGR.
Visiting the antenatal clinic on a regular basis after registration plays an important role in the diagnosis of intrauterine growth retardation. Treatment of timely detected pathology allows minimizing the risk of negative consequences.
A pregnant woman should have a well-structured work and sleep schedule. Proper and complete rest implies 10 hours of sleep at night and 2 hours during the day. This regimen improves blood circulation and transport of nutrients between mother and child.
Daily walks in the fresh air and dosed physical activity not only improve the general well-being of the pregnant woman, but also normalize the condition of the fetus inside the womb.
Preventing the occurrence of the syndrome during pregnancy
No pregnant woman is insured against FGR.
Preventive measures will reduce possible risks. The main condition for prevention is pregnancy planning, where future parents undergo a full laboratory and instrumental examination.
It is also necessary to adhere to a healthy lifestyle. Hiking, staying outdoors, and a balanced diet are the simplest measures to prevent the development of IGR.
Visit the gynecologist's office and treat gynecological problems on time.
Author: Elena Yuryevna, obstetrician-gynecologist of the highest category Specially for the site kakrodit.ru