The value of hCG during pregnancy
In the first weeks of gestation, human chorionic gonadotropin begins to be produced in a woman’s body.
Its secretion by chorionic villi begins from the moment of implantation of the blastocyst into the endometrium of the uterus and continues throughout the entire period of gestation. In its structure, hCG is similar to other gonadotropic hormones produced by the pituitary gland - follicle-stimulating and luteinizing. Functions of human chorionic gonadotropin during pregnancy:
- prolongs the functioning of the corpus luteum - a temporary gland, which, in the absence of conception, regresses 2 weeks after ovulation (in pregnant women it exists until 10–12 weeks of gestation);
- stimulates the secretion of progesterone and estrogen, due to which the level of these hormones becomes higher than before pregnancy;
- increases the secretion of glucocorticoids by the adrenal cortex, which helps the female body adapt to pregnancy;
- participates in immune suppression;
- helps the formation of the placenta.
How does it grow during pregnancy?
HCG has its own dynamics of growth. After the embryo attaches to the wall of the uterus, it begins to be actively produced, and its growth obeys the law: “every 2 days, 2 times.”
The period of doubling of concentration can be reduced to one and a half days, which is also the norm.
So it grows until 10-11 weeks and by this time reaches its maximum concentration. After 10-11 weeks, the fetal membrane gradually degenerates into the placenta and continues to produce this hormone, but in reduced quantities.
This is due to the fact that in addition to hCG, the placenta completely takes over the synthesis of progesterone, which was previously carried out by the corpus luteum.
HCG was primarily needed to activate this process, therefore, when the placenta itself became able to produce progesterone, the need for excessively active growth of gonadotropin disappeared.
Normal hCG levels in the early stages
In early pregnancy, hCG levels rise rapidly. Before conception, its content in the blood should not exceed 5 mIU/ml. Starting from the first week of pregnancy until the end of the first trimester, the concentration of human chorionic gonadotropin increases by one and a half to two times every day. HCG reaches its maximum by 11 weeks, and then gradually begins to decrease and remains at the same level from 21 weeks until birth.
The table shows the norms for hCG levels in the first trimester:
| Weeks of gestation | Lower limit of normal, mIU/ml | Upper limit of normal, honey/ml |
| 1 | 16 | 56 |
| 2 | 101 | 4870 |
| 3 | 1110 | 31500 |
| 4 | 2560 | 82300 |
| 5 | 23100 | 151000 |
| 6 | 27300 | 233000 |
| 7–10 | 20900 | 291000 |
Why do hormone levels drop?
Normally, in the early stages of pregnancy, the content of human chorionic gonadotropin in the body should only increase. Why does the concentration of hCG decrease, which means a decrease in the level of the hormone in the blood? Possible reasons for this phenomenon:
- ectopic pregnancy - the attachment of the fertilized egg did not occur in the uterine cavity, but in the fallopian tube, cervical canal or peritoneum;
- threat of miscarriage (if hCG has decreased by 50%, most often the cause is progesterone deficiency);
- delayed development of the embryo;
- death of the embryo and frozen pregnancy.
If human chorionic gonadotropin falls after the transfer of embryos obtained through IVF, this indicates that the pregnancy did not survive and the embryos did not engraft.
An unsuccessful transplant can be confirmed or refuted using ultrasound. A sharp decrease in the amount of the hormone in the blood is a reason to immediately undergo a medical examination. If the reason is ectopic implantation of the embryo and it is not possible to save the child, the woman is advised to have surgery to remove the fertilized egg. If there is a threat of miscarriage, a course of hormonal therapy will be prescribed.
HCG level too high
Any deviation from the normal concentration of the hormone in the blood is fraught with various diseases and complications. Elevated levels of the substance in the blood of non-pregnant women and men may be a sign of abnormalities that a person may have, such as:
- Tumors in the testicles;
- Tumors in the gastrointestinal tract;
- Abnormal growths in the lungs, uterus, and kidneys;
- Hydatidiform mole, in which conception occurs, but the chorionic tissue begins to form bubbles rather than a full-fledged embryo;
- Chorionic carcinoma is a malignant tumor, most often formed from fetal cells (sometimes found in non-pregnant women).
Can hCG levels decrease and then increase as pregnancy progresses?
For what reason does the hCG level first fall and then rise? The gap between the lower limit of normal and the upper limit is quite large. If the hormone fluctuations are insignificant, then its slight decrease may still be within the normative limits. In this situation, doctors monitor the woman’s condition, suggest she do tests again in a week and prescribe an ultrasound. In addition, a discrepancy between the test results and the norm during a developing pregnancy may indicate that the gestation period is determined incorrectly.
A situation where human chorionic gonadotropin fell at the beginning of pregnancy and then increased again occurs after the IVF procedure. In the first days of gestation, the level of the hormone in the blood is increased due to the hormone therapy protocol, which includes taking hCG.
The production of human chorionic gonadotropin is influenced by other hormones, such as progesterone. If your hCG drops but then rises again, this may be due to fluctuations in progesterone. If the hormone decreases by more than 50% of the norm, therapy with hormonal drugs such as Utrozhestan or Duphaston, which contain synthetic analogues of gestagens, is prescribed. Under the influence of drugs, the concentration of gonadotropic hormone gradually increases.
Pregnancy with low hCG is possible
The hCG hormone - human chorionic gonadotropin - begins to be produced soon after conception, or more precisely, after implantation of the fertilized egg into the uterine wall. It is by its presence that the fact of pregnancy is determined. Test strips react to the appearance of hCG in a woman’s urine, but are not able to show the exact level of the hormone. Meanwhile, this is necessary to understand how the fetus develops and whether everything is okay with it. But how will pregnancy proceed with low hCG and is it possible to raise its level?
Normally, hormone production occurs only during gestation. In a non-pregnant woman, hCG levels range from 0 to 5 mIU/L. Tests detect pregnancy already at hormone levels of 10 to 25 mIU/l, while with ultrasound the fetus will be noticeable only when the hCG level reaches 1000 mIU/l.
The greatest increase in the level of hCG in the blood occurs in the first two months after conception. At this time, the chorion actively secretes gonadotropin, and every 48 hours its level doubles. Low hCG levels during pregnancy, therefore, may indicate the following pathologies:
The hCG level is required to be determined during screenings in the first and second trimesters. It must be said that an increase in level relative to the norm is not a very good sign, except in cases of multiple pregnancies. High hCG may be an indirect sign of some fetal pathologies, including Down syndrome.
What to do if the indicators do not meet the norm? Is it possible to continue pregnancy with low hCG? First of all, don't panic: the result may be wrong, and here's why. It is almost impossible to find out the exact day of conception and implantation of the egg, unless the woman has undergone IVF. Meanwhile, hCG levels, as we have already said, are growing very quickly
Source
At what value is the heartbeat heard?
The heart begins to develop as early as 2-3 weeks of pregnancy.
At first it is a hollow tube located in the very center of the embryo, then gradually separate chambers begin to form from it: first two, then three, then four. The human heart has four chambers and this explains the work of two circles of blood circulation.
To hear the heartbeat of the embryo and evaluate the effectiveness of its work, the following methods are used:
- Auscultation - listening to heart sounds with a phonendoscope (the method is unreliable and can only be used from the 20th week of pregnancy, when the noises are already clearly distinguishable.
- Echocardiogram.
- Cardiotocography.
- Ultrasound.
ATTENTION! Ultrasound can be transvaginal (from inside the vagina) and transabdominal (the sensor is “moved” along the surface of the abdomen), where intravaginal is prescribed only in case of serious complications.
Ultrasound is the most commonly used and accurate method of listening to the fetal heart, and the ability to distinguish its beats will depend on the method chosen. For example, transvaginal ultrasound allows hearing even at a hCG concentration of 7200 IU/l . But intravaginal diagnostic methods are prescribed to pregnant women extremely rarely, because any invasion of the vagina in the early stages can provoke the threat of miscarriage.
As for other research methods, you can hear the sound of the baby’s heart at 10–12 weeks .
At what week does your baby start to have heart palpitations?
The formation of the heart in the embryo occurs in the 4th obstetric week.
It looks like a hollow tube, and already in the 5th week the first contractions of the organ, which has not yet fully formed, are noted. The vital organ begins to beat not sharply, but gradually, as if adjusting the rhythm. The period from 4 to 10 weeks, during which the heart develops, is very important for the health of the child. Deviations in the development of a muscular organ are possible due to genetic abnormalities, early maternal diseases, and exposure to toxic substances. In order not to miss pathology, the obstetrician listens to the embryo's heart during each appointment. Without an ultrasound sensor, this can be done from 18-20 weeks.
Normal heart rate at different times
The fetal heart rate will provide the obstetrician with important information about the development of pregnancy. If no knocking is heard at week 8, a frozen pregnancy is diagnosed. Erratic rhythms in the early stages suggest a heart defect. Arrhythmia in the last trimester often indicates oxygen starvation of the fetus.
Normal indicators of the baby’s heartbeat in the womb (beats per minute):
- 6-8 weeks – 110-130;
- from 9 to 11 weeks – 170-190;
- from 12 weeks until the onset of contractions – 140-160.
Increase pattern
From the 5th-6th day of pregnancy, active growth begins. It obeys the following pattern: it doubles every one and a half to two days .
This norm is the same for all women, and any deviation from it can be regarded as a pathological course of pregnancy.
Here are the likely reasons why hCG production may be reduced:
- Frozen pregnancy.
- Ectopic pregnancy.
- Intrauterine fetal death.
- Congenital developmental anomalies.
- Risk of miscarriage.
In the first weeks after applying for registration at the antenatal clinic, doctors prescribe a hCG test several times in order to objectively assess the course of pregnancy and promptly notice the development of abnormalities or threats to fetal loss.
INTERESTING! Increased growth will continue until the 10-11th week of pregnancy, and then, after the fetal membrane has degenerated into the placenta, its level will begin to gradually decrease and will remain in a concentration corresponding to the 7th week of gestation until the end of pregnancy.
HCG increased for 3 days
HCG has more than doubled in two days, is this normal? I'm scared.
where did you get the idea that it was clearly 2 times? Don't do bullshit. Pregnancy is not a mathematical science; what is in theory is not always in practice.
Why are you taking hCG? And then you screw yourself over. cool, anything to do? Wear and enjoy your pregnancy
You're just like me. At first I also calculated hCG: sometimes it’s too much for me (everyone! Save yourself! Hydatidiform mole! Stay tuned, internet!), sometimes it’s not enough for me. And when I gave birth, I realized that there was nothing to invent for myself and spoil my nerves, pregnancy is the most wonderful time and you should enjoy it, not worry! My increase also more than doubled, a wonderful healthy boy was born! And your hCG level Everything is fine!
my hCG increased 3.4 times in two days, I was also scared, but I found a lot of information on the Internet that doubling every day, especially at the beginning, is also a variant of the norm, don’t worry)))
Oh, how familiar everything is;))) I was also VERY worried that hCG grew faster than 2 times - just like yours at 2.5. I started to have all sorts of fears:) well, it’s worth saying that everything was wonderful. Don’t even think about worrying for a second, this is absolutely normal. and they say that hCG grows faster during pregnancy with a girl. I don’t know if it’s true or not, but it coincided with me :) good luck
Oh, how familiar everything is;))) I was also VERY worried that hCG grew faster than 2 times - just like yours at 2.5. I started to have all sorts of fears:) well, it’s worth saying that everything was wonderful. Don’t even think about worrying for a second, this is absolutely normal. and they say that hCG grows faster during pregnancy with a girl. I don’t know if it’s true or not, but it coincided with me :) good luck
Healthy pregnancy - healthy offspring
dgas is normal during pregnancy Hello!
Pregnancy is approximately 3 weeks. They ordered tests. Everything is excellent, except for two indicators: Dihydroepiandrosterone sulfate DEA-SO4 263 when the norm is up to 230., Progesterone 42.3 when the norm is 32.6-139.9., HCG 18896 I didn’t understand which I.e. for almost 2 weeks it goes down very slowly. A week before the decline, hCG began to smear, and after the decline in hCG - blood
Source
Methods for diagnosing fetal heartbeat
An obstetrician can monitor the heart rhythm of the embryo and then the fetus using the following methods: auscultation, ultrasound, cardiotocography, cardiointervalography. Any of them allows you to evaluate the frequency of contractions, rhythm, and heart sounds. It is especially important to monitor this indicator during childbirth, when the baby’s body experiences the first serious stress.
Using an obstetric stethoscope
Listening to the fetal heart with a stethoscope is a classic method that shows reliable results from 18-20 weeks. Manipulations are carried out during each visit to the doctor. The location of the area where heart sounds are best heard depends on how the fetus is positioned in the uterus. After 24 weeks, multiple pregnancy is confirmed by several points of best listening, as they are noted in different parts of the abdomen.
Cardiotocography method
Cardiotocography allows you to record the heartbeat and physical activity of the fetus, as well as the number of uterine contractions from 28-32 weeks of gestation.
The study is shown to all expectant mothers. In case of pregnancy pathology, it is carried out regularly. Indications:
- operations on the uterus (caesarean section, removal of fibroids), as a result of which a scar formed;
- gestosis in the third trimester;
- oligohydramnios;
- stimulation of labor;
- post-term pregnancy;
- premature aging of the placenta;
- polyhydramnios;
- umbilical cord entanglement according to ultrasound;
- change in the nature of the heart rhythm detected by auscultation.
Listening to your heartbeat using a heart monitor lasts about 45 minutes. The expectant mother is usually in a lying position. Sensors are applied to the place where the heartbeat can be heard best. They record cardiac parameters and display the results on paper. The information obtained allows the doctor to issue an opinion on the condition of the fetus. The specialist takes into account the following parameters: frequency and rhythm of heart parameters, the presence of a reaction from the heart to uterine contractions (increased frequency, arrhythmia).
Ultrasonography
A transvaginal sensor records the fetal heartbeat in the 6th week after conception, a transabdominal sensor a couple of weeks later. The absence of a rhythm during these periods is a reason to undergo additional examination, which includes donating blood for hCG. If the hormone level is low, a control ultrasound is performed after 7 days. The embryo probably froze.
In the last stages of pregnancy, ultrasound diagnostics makes it possible to determine the number and frequency of heart contractions and clarify the location of the muscular organ in the baby’s chest. A study called the “four-chamber slice” makes it possible to evaluate the development of the ventricles and atria. The method detects heart defects in 80% of cases.
Cardiointervalography technique
The technique is used when fetal developmental pathologies are suspected. It consists of a long (about an hour) ultrasound recording of the heart. The information is immediately displayed on a computer, which analyzes the rhythm frequency, heart rate fluctuations, and identifies moments of acceleration of the heart muscle. A connection is established between the heartbeat and the baby’s movements in the abdomen, and periods of decreased rhythm frequency are identified. Cardiointervalography is an informative method that can be used to identify serious heart defects during fetal development.
HCG indicator during frozen pregnancy
A frozen pregnancy is one of the worst nightmares of an expectant mother. The complexity of the situation also lies in the fact that the fact that the fetus is no longer developing is not always detected immediately and quite quickly. And there can be quite a few reasons for this - from the fact that you can’t hear the heart beating yet, to the fact that studies such as ultrasound are carried out regularly only at a later date. This is where heartbreaking stories appear online about how a woman carried a frozen pregnancy under her heart for 3-4 or more weeks.
One of the simplest and most reliable ways to make sure that pregnancy is progressing or that it has suddenly stopped is to take a blood test. This is usually determined based on hCG, a special hormone. HCG during a frozen pregnancy necessarily decreases.
What is this hormone and why is it so important?
HCG is the abbreviation of the medical name human chorionic gonadotropin. It is a hormone that appears in a woman exclusively during pregnancy. By the way, the standard home test for determining an interesting position is also based on this hormone.
In this case, hCG is present only during progressive pregnancy. If everything goes according to plan, its level increases. Moreover, this happens at a fairly noticeable pace every week. There are even special tables with the norms for the level of this hormone in a woman’s blood. So, for example, there are situations when the embryo is small, and then the indicators may slow down somewhat. However, if everything is already over, then the hCG during a frozen pregnancy will definitely go down and nothing else.
Checking the hCG level to determine a frozen pregnancy
If for some reason doctors suspect that the pregnancy has stopped developing, they will conduct additional research. For example, indications for blood testing may include:
- the fetal heart is not visible and inaudible on ultrasound (during those time periods when it should already appear);
- unchanged size of the uterus (determined by manual examination);
- sudden disappearance of all traditional signs of pregnancy, especially if before this they made themselves felt very noticeably.
Also among the signs indicating the development of a frozen pregnancy are usually called:
- the appearance of spotting bloody discharge (may not always occur);
- nagging pain in the lower abdomen - it is known to many ladies, because it is similar to premenstrual pain;
- lower back pain.
Naturally, expectant mothers should not immediately stress themselves out. After all, all this happens not only because the pregnancy has frozen. It is quite possible that the fetus is simply small or the development is slightly behind the deadlines, because these deadlines were set incorrectly. It is simply advisable to conduct a control study, which will already give final forecasts. (And for an ectopic pregnancy, what kind of hCG).
How to measure hormonal levels
If suddenly there is a suspicion of premature termination of pregnancy in the early stages, a blood test is prescribed. Moreover, you should understand that you will have to submit the material more than once. This is due to the fact that it decreases in the same way as it increases – in waves. Naturally, based on the first indicator, it will be quite difficult to assess the scale of the disaster, unless, of course, we are talking about a global drop in hormone levels.
It is worth understanding that for different ladies the indicators will be purely individual. So, for example, in some people during a frozen pregnancy, hCG will drop almost instantly. For others, it will decrease quite smoothly. There are also exceptions in which it continues to grow. But here you will have to take into account that the increase in level will be extremely slow and will not fit into the normal limits at all.
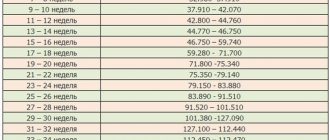
What are the standards - what to look for
So that the expectant mother can understand her chances of a successful pregnancy, she should study the hormone levels depending on the duration of pregnancy. Doctors say that the following figures can be taken as a basis:
- 25-156 in the second week;
- 1110-31500 – fourth week;
- 23100-151000 – fifth week;
- 20900-291000 – 11th week.
This difference in results is due to the fact that each laboratory has its own methods for testing blood, as well as drugs and other means that are used for this. If something worries you, you should visit your observing obstetrician more often in order to notice in time if something is going wrong.
How quickly does it fall after a miscarriage?
HCG begins to fall not after a miscarriage, but some time before it.
With normal hormone levels, a miscarriage simply cannot occur unless it is due to an injury or extreme stress. 5-7 days before a miscarriage, production begins to sharply decrease. If you do the appropriate tests in time and take measures, then this consequence can be avoided and the fetus can be saved.
When the hormonal concentration is no longer able to support pregnancy, the embryo is rejected and it comes out through the bloodstream.
By the time a miscarriage occurs, the hCG level has already reached its minimum concentrations, and after it has already occurred, the body restores the hormone to its original level within a few days.
Early
If a miscarriage occurs early, then in this case it is very easy to diagnose it in advance. The concentration of hCG increases so quickly that any deviation is extremely easy to notice. Otherwise, everything will depend on an adequate diagnosis of the gestation period and the doctor’s attention to the patient’s complaints.
After a miscarriage, the hormone will decrease gradually, because it is not easy to stop such active synthesis (every 2 days it increases by 2 times) in one day. Within a week, as a rule, hCG returns to its original level. Nevertheless, this is a fairly short period of time compared to miscarriages in the third trimester.
At later times
In the later stages after a miscarriage, it is much more difficult for the body to recover. Despite the moderate increase in hormone production, its concentration reaches large levels.
Late miscarriage can occur for various reasons, and the subsequent period of restoration of the initial hCG number will depend on their nature.
Main reasons:
- injuries, falls;
- severe stress;
- Rhesus – conflict between mother and fetus;
- incompatibility by blood groups, etc.
IMPORTANT! During the second or third trimester, any cramping pain and especially bloody discharge should be a reason to immediately consult a doctor, otherwise you may lose the baby.
After a miscarriage, some time must pass for the body to fully recover and hormonal concentrations to return to normal. This usually takes up to one month.