Spermogram
- a laboratory method for studying reproductive function by studying the structure, motility, quantity and other characteristics of male germ cells. The diagnostic test is widely used to identify the causes of infertile marriage. A spermogram is a simple but informative way to study the fertility of the male body. Based on it, you can determine the presence or absence of infertility. The study helps to choose the best tactics for treating the pathology of the reproductive health of the sexual partner or make a choice in favor of artificial insemination.
Contact a specialist
A spermogram is a specific analysis that is not used for diagnostic purposes in the general population.
Typically, a study is prescribed to find out the causes of an infertile marriage and exclude or confirm the male factor. Infertile marriage - absence of pregnancy for six months while maintaining an active sexual life (active sexual life is considered intimate intimacy at least once every two days) and refusal of contraception. Much more often, this diagnosis is made when it is impossible to conceive during continuous attempts for 12 months. This is due to the fact that most couples do not have such frequent sexual intercourse.
Usually, when attempts to conceive are unsuccessful, the woman is the first to consult a doctor. After ruling out pathology in the wife, the man goes to a specialist for consultation. That is why most often a referral for a spermogram is issued by a fertility specialist.
This approach is irrational, since the share of female and male factors in infertility is equal. However, to confirm problems in a spouse, a much larger number of tests and studies are required.
Spermogram
- the most revealing study of male reproductive function. Based on its results, the doctor can judge the possibility of natural fertilization; the doctor does not require additional tests. That is why the most rational approach is when, in the presence of an infertile marriage, the man is the first to turn to a specialist. In this case, its diagnosis and treatment can be carried out by an andrologist, urologist or reproductive specialist.
Semen analysis is a simple and inexpensive method for studying male sexual function. That is why it is prescribed during the first conversation with the doctor. Already at the second consultation, based on the results of the spermogram, the doctor can exclude or confirm male infertility.
Types of spermogram analyzes
There are several types of spermogram, they differ from each other in the complex of proposed studies.
- Basic - includes standard studies recommended by WHO.
- MAR test - helps to identify the presence of antisperm bodies, which destroy sperm by their presence.
- Spermogram according to Kruger - involves determining the morphology of sperm.
You need to keep an eye on this: Inflammation of the testicles in men: symptoms and treatment of epididymitis.
Indications
A spermogram is prescribed in the following cases:
#1. Having an infertile marriage. The examination allows you to assess the quality of the sexual partner’s sperm and exclude the male factor.
#2. Pregnancy planning. This approach to conceiving a child is considered the most favorable. A man is recommended to examine the quality of seminal fluid before attempting fertilization. The analysis makes it possible to identify a spouse’s infertility at an early stage and provide competent treatment. Some diseases are practically untreatable once they enter the chronic stage. Also, poor spermogram results are a stimulus for a man to change his lifestyle. Smoking, alcohol, hot temperatures (baths, saunas) reduce the quality of germ cells.
#3. Concomitant disease. A spermogram can be prescribed outside the pregnancy planning period. This analysis allows you to evaluate male reproductive function in case of endocrine pathologies, injuries, varicocele or other pathologies.
#4. Preparing for IVF. Before the in vitro fertilization procedure, it is necessary to analyze the quality of a man's sperm. The analysis may show the need to use donor genetic material.
#5. Treatment control. Assessing the quantity and quality of ejaculate allows you to monitor the effectiveness of the therapy. Spermogram indicators change rapidly as male reproductive cells are renewed in response to lifestyle changes or medications.
Spermogram: indications, conduction, results
Why do the research?
However, it often happens that the main indicators of the spermogram are normal, but the desired pregnancy still does not occur. In this case, sperm morphology should be assessed. In other words, it is necessary to find out to what extent the structure of motile cells corresponds to the norm, since it is the structure of the cell that often determines successful conception. The length and shape of the tail are responsible for the trajectory of movement, the location of the acrosome is responsible for the dissolution of the egg shell, and the neck contains mitochondria that produce the energy necessary for movement, etc.
An advanced analysis, which also includes the morphology of the spermogram and the MAP test, establishes the feasibility of testing the structure of the ejaculate in order to clarify the nature of the pathologies.
Note that the ejaculate may contain a small percentage of cells with abnormalities that arise for a variety of reasons. A change in sperm morphology can occur, for example, as a result of stress, overheating, inflammation or an infectious disease. Social factors also have a significant impact on the quality of sperm: long-term stay within industrial zones with poor ecology, toxic effects, hazardous industries, etc.
A small number of defective cells does not affect the likelihood of conception in any way. The number of sperm with an ideal structure for natural conception should be at least 40–60%. If the number of quality cells is less than 20%, teratozoospermia is diagnosed. At a concentration of 4 to 40%, you should think about assisted reproductive technologies, in particular IVF. If the number of normal sperm is less than 4%, fertilization is only possible using ICSI.
Preparation
Preparing for a spermogram includes five rules:
#1. Abstinence. Before donating sperm, a man should not be sexually active or masturbate for 72-96 hours. When this time period is shortened, a sufficient amount of ejaculate does not accumulate, which may affect the reliability of the analysis results. Longer abstinence also skews the quality of the study. Lack of ejaculation for more than 5 days leads to the accumulation of abnormal sperm.
#2. Elimination of high temperatures. A week before the test, a man should not visit baths, saunas, or solariums. He is also prohibited from taking a hot bath; it should be replaced with a shower. Normal sperm maturation processes occur at a temperature of about 35 degrees Celsius. An increase in this indicator leads to a reduction in the number of normal male germ cells.
#3. Elimination of alcohol. Alcohol and its derivatives have an inhibitory effect on the maturation of sperm in the seminal ducts. A man is advised to refrain from drinking any alcoholic beverages at least a week before the expected test.
#4. Exclusion of medications. This rule does not apply only to vital medications. Some medications can distort the results of a spermogram, causing abnormal maturation of germ cells. It is recommended to discontinue the medications two weeks before the expected day of submitting the ejaculate for analysis.
#5. Elimination of physical and emotional stress. Various loads cause catabolic reactions in the human body, they lead to the breakdown of proteins. This is why stress can have a negative impact on the process of sperm maturation. A man should avoid going to the gym and other activities at least 3-5 days before the test.
Abnormalities in the spermogram
The normal spermogram assumes the presence of at least 50% of active germ cells. The reasons for the presence of a large number of immobilized sperm in the transcript may be as follows:
- Presence of diseases of the genital organs.
- Drinking alcoholic beverages.
- Smoking.
- Wearing tight underwear.
- Using intimate lubricants.
- Frequent stress.
- Hypovitaminosis.
Decoding the spermogram according to Kruger can reveal low sperm motility due to a disorder in the structure of the cells.
When deciphering a spermogram, it is important to know under what conditions the study was carried out. It has been noted that at elevated body temperature in the ejaculate, sperm motility increases, while at room temperature it decreases. Therefore, if the temperature in the room where the study is being carried out is within +10 degrees, then even healthy sperm will have little mobility. To ensure that the interpretation of the analysis is as reliable as possible, laboratories use special thermostats, which make it possible to study the material at temperatures as close as possible to those of the human body.
The reason for the decrease in the number of germ cells in the ejaculate may be one of the following conditions:
- Disturbances in the functioning of the endocrine system (dysfunction of the adrenal glands or thyroid gland, diabetes mellitus, disorders in the pituitary-hypothalamic system).
- Diseases of the genitourinary system (cryptorchidism, prostatitis, varicocele, etc.).
- Increased body temperature.
Immunologist Georgy Aleksandrovich Ermakov talks about the causes, symptoms, diagnosis and treatment of varicocele:
- Prolonged exposure to elevated temperatures (in the workshop, etc.).
- Genetic disorders (Klinefelter syndrome, etc.).
- The effect of toxic substances on the body (alcohol, some medications, such as sleeping pills, steroids, etc.).
When determining the fertility index, the doctor pays special attention to the number and motility of sperm. If, after deciphering the study, a man is diagnosed with asthenozoospermia, then his chance of becoming a father is significantly reduced. However, an increase in the motility of germ cells does not yet guarantee pregnancy.
Procedure
On the day of the spermogram, the man needs to come to the clinic.
Collecting ejaculate at home is undesirable, since it may lose its properties during transportation. Before donating sperm, a man needs to empty his bladder and perform hygiene procedures. Sperm collection should be done by masturbation. The use of a condom is prohibited because latex and lubricants may interfere with the examination results. It is also undesirable to obtain ejaculate through sexual contact of any kind. Women's vaginal mucus or saliva causes a change in pH and the death of sperm.
The entire portion of sperm is collected in a special sterile container and transferred to specialists. Various substances should not be allowed to enter the collected ejaculate. According to indications, a man may be prescribed a repeat spermogram no earlier than after 10-14 days.
Method of analysis
Preparation for a spermogram includes sexual abstinence before receiving ejaculate for 2-3 days, but not more than a week. Sperm is obtained through masturbation. This method is more physiological than interrupted sexual intercourse, which is also used in rare cases. You can use a special medical condom that does not contain lubricant or other chemicals. It is given out at the laboratory. Conditions for obtaining seminal fluid: it can be collected both in the laboratory and at home, in a more familiar environment.
Rules for submitting material: no later than an hour after collection, the ejaculate must be delivered to the laboratory for analysis. The temperature of the environment in which he is located at this time should be close to body temperature. It would be wise to use a special container - a thermostat. However, you can also take advantage of the body’s natural heat by placing the container with the resulting material in the armpit.
How to take a spermogram correctly?
During the four days before the spermogram, drinking alcohol, including beer, is prohibited, as well as taking thermal procedures - visiting a bathhouse, sauna, hot baths, working in unfavorable conditions. You should not take sleeping pills or sedatives. Otherwise, a man should lead a normal life. After antibiotics (taking the last pill or injection), at least two weeks should pass. It is believed that there is no influence of fluorography on spermogram parameters.
The analysis is relatively cheap, and the results are ready within a few days.
Normal indicators
Normal spermogram indicators reflect good fertility and fertility of a man.
They include several points of macroscopic and microscopic examination. During a macroscopic examination, the viscosity of sperm is assessed by sequentially liquefying and lowering a glass rod into it. Then it is slowly pulled out, the specialist observes the formed thread of ejaculate. Normally, sperm should not stretch less than 0.5 and more than 2 centimeters.
Next, specialists begin microscopic examination of the ejaculate. Laboratory assistants count the number of sperm in one milliliter of semen. It should exceed the 20 million mark. However, a sperm count of more than 120 million in one milliliter of ejaculate is considered pathological.
Attention! A sign of normal male fertility is the white-grayish color of the sperm. The volume of ejaculate is also assessed. In healthy men it exceeds 2 milliliters. A decrease in this indicator is a symptom of prostate or testicular disease. Decoding the spermogram analysis includes pH determinations. Normally, this indicator ranges from 7.2 to 8.0.
Experts also evaluate the motility of male germ cells. They are divided into four types. A-spermatozoa are actively motile, their number should be more than one quarter. The B-group is characterized by weak movement (sedentary), their share together with the A-group should exceed 50%.
Sperm may contain C-sperm cells with non-progressive motility and inert D-cells. Their total number should not exceed 50%.
Laboratory assistants count the number of live sperm, which should be at least half. The appearance of male reproductive cells is also assessed. Specialists examine the structure of the head, neck and flagellum of the sperm. In a healthy man, the rate of normal germ cells exceeds 50%.
Experts also evaluate various impurities in the ejaculate. Normally, it can contain up to two percent of the precursors of mature sperm. The presence of 3-5 leukocytes in the field of view is acceptable, there should be no erythrocytes and spermatophages.
Standard table:
Diagnostic value of spermogram with assessment of sperm morphology
A spermogram is the main analysis for assessing male health, with which any examination by an andrologist begins.
Based on its results, the doctor chooses treatment tactics and, if necessary, prescribes additional tests. The main reason for visits is suspicion of infertility. This should be discussed if pregnancy in a couple does not occur for more than a year with normal sexual activity. Let’s make a reservation right away that if infertility is suspected, both partners undergo examination. Modern research proves that almost half of cases of infertility are caused by the “male factor.” A spermogram is a simple analysis, but very informative. Macro- and microscopic indicators are examined: volume, viscosity, acidity, color, as well as the number and motility of sperm. As a result of the study, a conclusion is issued in the form of a spermiological diagnosis and quantitative indicators. Interpretation of the results is perhaps the most important stage in the survey; it is not so much the indicators in numbers that are important, but their combination. For example, a low sperm concentration can be compensated by a large ejaculate volume. It is advisable that the results of the study are assessed by the doctor who will subsequently provide treatment. It should be noted that ejaculate testing is one of the most subjective tests in laboratory diagnostics, the result of which directly depends on the experience and professionalism of the spermiologist. A qualified embryologist can evaluate not only the morphology, but also the potential fertilization prospects.
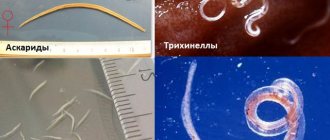
Based on this analysis, the cause of infertility cannot be clearly established, but some characteristic signs may indirectly indicate it. For example, viral infections often cause large numbers of sperm with double tails or heads. An abnormally large number of immature cells indicates a varicocele, but it may also indicate too much sexual activity, when the cells simply do not have time to mature.
If the specialist sees any deviations from the norm, he may order a repeat study in 2-4 weeks. If similar anomalies are detected in the next analysis, treatment will most likely be prescribed.
Abnormal Results
Deviations from the norm in the spermogram are a symptom of any pathology of the male reproductive function. The most common abnormal findings are:
Oligozoospermia
The pathology is accompanied by a decrease in the number of sperm in the ejaculate. A man's ability to physiologically fertilize depends on the degree of oligospermia. With a mild form, pregnancy is possible, although unlikely; with a severe type, it is practically excluded. Oligospermia is a symptom of many diseases. These include endocrine dysfunction, trauma, varicocele, vitamin deficiency, chronic infection, and radiological radiation. Also, a decrease in sperm count may be associated with bad habits, overheating and other environmental factors. The extreme degree of pathology, when male reproductive cells are absent in the ejaculate, is called azoospermia.
Asthenozoospermia
This anomaly is characterized by a decrease in the number of motile male germ cells. There are three degrees of the pathological condition, with the first the content of normal sperm (types A and B) above 40%, with the third below 30%. Male reproductive cells need to travel a long way from the vagina to the free abdominal cavity, so their low mobility is an obstacle to pregnancy. The causes of this pathology are hereditary diseases, intoxications, inflammatory processes and dysfunction of the prostate gland. The extreme degree of asthenozoospermia is akinozoospermia - a condition in which all sperm are immobile.
Teratozoospermia
The pathology is accompanied by an increase in the number of sperm with an abnormal structure. Due to incorrect morphology, male reproductive organs do not have the properties necessary to fertilize an egg. Also, abnormal sperm are the cause of congenital pathologies of the fetus, spontaneous abortions and fading of pregnancy in the early stages. The causes of teratozoospermia are varied, most often they are all associated with genetic defects, pathologies in the endocrine system and infectious processes in the male genital organs.
Leukocytospermia
This condition is observed when the number of leukocytes in the seminal fluid increases. The pathology itself is not the cause of male infertility. But leukocytes in sperm are markers of the inflammatory process in the male body. These cells are produced in response to the proliferation of pathogenic microorganisms: bacteria, fungi, protozoa, viruses. Leukocytospermia can be observed in sexually transmitted diseases, prostatitis, cystitis and other pathologies of the urogenital tract. Less often, such a spermogram conclusion indicates the systemic nature of the inflammation.
Hematospermia
The pathology is accompanied by the appearance of red blood cells called “erythrocytes” in the ejaculate. Normally, these elements should not be observed in sperm. Like white blood cells, red blood cells are not the direct cause of male infertility. Decreased fertility occurs due to an underlying disease. Typically, red blood cells appear in pathologies of the prostate gland - prostatitis, malignant neoplasms, cysts, stones. Also, hematospermia can be associated with violations of the integrity of the urethra - due to its injuries, cancer, inflammation.
Necrozoospermia
This condition is characterized by an increase in the number of dead male germ cells in the ejaculate. Necrozoospermia does not allow fertilization to occur, since this process requires a large number of viable sperm. The most common cause of pathology is the influence of the environment and a man’s lifestyle. A reduced number of viable sperm may be associated with congenital anomalies, systemic diseases (tuberculosis, diabetes mellitus), and injuries.
Aspermia
The pathology is characterized by the complete absence of ejaculate. Natural and artificial pregnancy with aspermia is completely excluded, since any type of fertilization requires seminal fluid with viable sperm. The pathology is rare; its cause is complete failure of the testicles and prostate gland, or obstruction of the vas deferens.
What to do if your sperm count is bad
Deviations from the norm can be critical or non-critical. That is, if the indicator does not significantly deviate from the normative range, this does not necessarily mean the presence of pathology. Non-critical parameters include the following:
- Acidity;
- Viscosity;
- Exceeding the norm of round cells;
- Long-term liquefaction.
Deviations of the above indicators from the norm do not have a significant impact on the possibility of fertilization.
Results critical for conception:
- Leukospermia, pyospermia - excess number of leukocytes.
- Oligozoospermia – few sperm. It is recommended to freeze some healthy individuals for subsequent fertilization.
- Teratozoospermia is a small number or complete absence of sperm with normal structure. Only individuals with an oval head and a long tail are able to penetrate the egg.
- Azoospermia – absence of sperm. Causes: blocked ducts (treated surgically) and production problems (corrected by hormonal stimulation of spermatogenesis).
- Asthenozoospermia – low sperm motility.
- Akinospermia is the absence of motile sperm.
- Necrospermia is the absence of living germ cells.
- Cryptospermia is a small number of living sperm.
A spermogram records the current state of the ejaculate; it is not yet a diagnosis. If inflammation is present, a course of antibiotics is prescribed; in case of non-critical deviations from the norm, you can get by with taking dietary supplements and lifestyle correction.
The simplest method for improving sperm count while maintaining a healthy lifestyle is regular sex . The absence of ejaculations leads to the accumulation of pathological forms of sperm and a decrease in their motility. Regular renewal reduces the effect of free radicals and prevents damage to DNA strands. Too active sexual life is undesirable (the number of mature forms of sperm decreases, sperm becomes too liquid). For example, for men aged 30 to 45 years, 3-4 times a week is quite enough.
Improving sperm count is facilitated by creating optimal conditions for the functioning of the gonads. You should not overheat the groin area, wear compressive underwear, it is important to prevent chronic inflammation of the genitourinary system.
Diet plays an important role. It needs to include more protein, vegetables, fruits and grains. Nuts, seafood, vegetable oils, honey are healthy.
Vitamins E and C, lycopene, and coenzyme contribute to improving morphology. Arginine and L-carnitine help prevent the formation of abnormal sperm. Smoking has an extremely negative effect on sperm. Alcohol and other intoxications can also cause reduced fertility.
Additional tests
Varicocele is one of the most common etiological factors of male infertility.
The disease is accompanied by varicose veins of the ovary, causing disturbances in temperature and circulatory pathology. To confirm the diagnosis, doctors use ultrasound scanning with a Doppler sensor. The study helps to visualize the vessels of the male pelvis. Ultrasound also allows you to identify tumors, strictures and other pathologies of internal organs. To exclude the endocrine factor of infertility, doctors prescribe a blood test of the patient. Experts count the number of different forms of testosterone, the main male hormone. It is also recommended to study the condition of the thyroid gland, adrenal glands, pituitary gland and hypothalamus. All organs of the endocrine system are closely connected with each other, so male fertility is affected not only by the testicles.
The MAP test is used to exclude or confirm the immune factor of an infertile marriage. This pathology is rare, occurring no more than in 5 percent of cases. Using the test, doctors determine the amount of antibodies to one's own sperm. Their increase indicates an abnormal immune response to germ cells and their spontaneous destruction. There are also female antibodies to sperm, produced in response to ejaculate entering the genital tract.
Karyotyping is used to determine a man's genome. Sometimes the cause of infertility is hereditary diseases. Such pathologies include Klinefelter's syndrome, Kallman's syndrome, as well as chromosomal mosaicism.
Also, to exclude an infectious process, a man can be referred for a smear from the urethra. This study is used to determine the microflora of the genital organs, identify pathogenic bacteria, fungi and protozoa. A more reliable and faster test is a serological blood test for antibodies or antigens of infectious agents in the patient’s blood.
This article will help you understand and decipher any spermogram. You will learn the history of sperm analysis, read in detail about the methods of donating sperm and the stages of its examination.
A standard spermogram takes into account physical parameters: sperm volume, its color, viscosity, pH; and microscopic parameters: the number and motility of sperm, the content of other cells, etc. Based on the data obtained, we can make assumptions about male infertility, diseases of the reproductive organs, and possible infections. A spermogram is usually recommended when preparing spouses for an IVF program. When treating male infertility, a spermogram is one of the first and most informative tests prescribed by an andrologist.
How to obtain sperm for analysis
Masturbation is considered the ideal method of obtaining sperm for spermogram analysis. This is the method recommended by the World Health Organization. Collecting sperm in a condom is not used due to the harmful effect of lubricants on sperm. Interrupted coitus is also not recommended: the semen sample may contain cells of vaginal origin or the microflora of the partner. It is possible to use stimulant drugs, such as Viagra, etc. If there are no sperm in the ejaculate (this condition is called “azoospermia”), it is possible to use surgical methods for obtaining sperm.
It is best to donate sperm in a clinic, this will allow specialists to begin analysis immediately after the ejaculate has liquefied. It is also possible to collect material at home if the patient can ensure delivery of the material to the laboratory within 1 hour. The MAMA clinic has a special room for obtaining sperm; its interior is far from “hospital” - this ensures psychological comfort for the patient. Those wishing to bring ejaculate from home are given a special transport container for sperm.
Before donating sperm for analysis, the patient is advised to abstain from sexual intercourse for 3–5 days. It is recognized that a shorter period of abstinence can lead to a decrease in semen volume and sperm count, while a longer period can lead to decreased motility and an increase in abnormal sperm. However, this dependence is not always clearly visible.
How to analyze ejaculate
The liquefaction time of the ejaculate is the first parameter studied. The ejaculated semen is usually a coagulum, meaning it is not completely liquid. After some time, the ejaculate becomes liquid under the influence of prostate enzymes contained in the seminal fluid. Liquefaction is determined by the change in sperm viscosity. To do this, the ejaculate collected in a pipette is released from a height of 2 to 15 cm. Viscosity is measured along the length of the “thread” trailing behind the released drop. Sperm is considered liquefied if the “thread” does not exceed 2 cm. Normal semen liquefies within 10–40 minutes (some laboratories consider liquefaction within one hour to be normal). If liquefaction is delayed or does not occur at all, this may indicate disturbances in the functioning of the prostate gland.
Liquefaction can affect the fertilizing ability of sperm. Increased viscosity indicates possible dysfunction of the prostate gland and, therefore, disturbances in the biochemical composition of seminal fluid, which in some cases can cause male infertility.
Analysis of unliquefied semen can lead to errors in determining sperm concentration and motility. Therefore, to determine other parameters of the ejaculate, specialists wait until it is completely liquefied, or add special substances to the sperm that accelerate this process.
Ejaculate volume is one of the most important characteristics of sperm. Together with the concentration of sperm, this indicator gives an idea of the total number of sperm ejected during sexual intercourse. A volume of less than 1.5 ml may be considered a cause of male infertility (oligospermia). The point is not only that a small ejaculate contains few sperm. Even if their concentration is high and the total number far exceeds the required 40 million, there is still a threat to normal conception.
When erupted into the vagina, sperm find themselves in aggressive conditions. The acidic environment of the vagina is detrimental to sperm and most of them die within 2–3 hours. During this time, the most mobile and “healthy” sperm should have time to penetrate the uterus, where the conditions for their life are favorable (sperm can remain mobile in the uterus and fallopian tubes for more than a day). Seminal fluid (or seminal plasma) temporarily alkalizes the vaginal environment, making it less acidic, and allows active sperm to enter the uterus. It is believed that a small volume of seminal fluid “cannot cope” with this task: the less seminal fluid, the less time it can restrain the acidity of the vagina.
In addition, a man’s seminal plasma locally suppresses a woman’s immunity (after all, for a woman’s immune system, sperm are like foreign objects). In the pathological course of this process, the so-called cervical factor of infertility occurs. And from this point of view, volume also plays a significant role.
However, too much sperm volume does not give a man any advantages. As a rule, no more than 5 ml of ejaculate is placed in the vagina, while the extra milliliters flow out and do not participate in conception.
Due to the importance of determining semen volume, the patient should collect as much of the ejaculate as possible into a container for a spermogram. If you lose part of the ejaculate intended for analysis, you must inform the clinic specialist about this. It should be borne in mind that the first part of the ejaculate is the richest in sperm.
Unfortunately, in some cases there is no ejaculation at all, despite the sensation of orgasm. This may indicate so-called “retrograde ejaculation” (ejaculation into the bladder). In such cases, it makes sense to examine the urine after orgasm to see if there are sperm in it. In the presence of urea, sperm quickly die and are destroyed, so special approaches are required in this case. Our clinic specialists will instruct you in detail about obtaining post-orgasmic urine and will analyze it quickly and efficiently.
Currently, the color, like the smell of ejaculate, does not have an important diagnostic value, and the World Health Organization does not recommend recording this parameter in a standard spermogram. However, most laboratories, maintaining tradition, record the color of the seminal fluid. Most men have sperm that is “white-greyish” in color. Numerous shades: milky white, yellowish, transparent cannot clearly indicate any violations. The only exception is the ejaculate that is “pinkish” in color, indicating hemospermia - an increased content of red blood cells in the sperm.
The pH value, or, more simply put, the acidity of the ejaculate, can often be an important clue in determining reproductive and sexual dysfunction. Normal ejaculate has a slightly alkaline reaction (pH 7.2–8.0). A change in this indicator in one direction or another from the norm, if there are no other deviations, cannot indicate any violations. But in combination with other signs it influences the diagnosis. For example, an increased pH with an increased content of round cells and non-liquefaction of sperm will strengthen the specialist’s opinion about a possible disorder of the prostate gland of an infectious nature; a lower pH with azoospermia will give hope for its obstructive nature (there are sperm, but the vas deferens are blocked), etc.
Still, the basic properties of sperm can only be determined by examining it under a microscope. The number of sperm is the first thing that specialists determine during microscopic examination. To count sperm, special devices are used - counting chambers. Usually the amount is expressed as a concentration (so many millions per milliliter). In a normal ejaculate there are at least 15 million sperm per milliliter. The sperm count depends on many factors. But at the MAMA clinic you can get a pregnancy with the most severe male factor - from single sperm.
Standards for spermogram
The motility of sperm is no less important than their number, because what good is a lot of sperm if they don’t move. In accordance with the new standards of the World Health Organization (2010), it is customary to divide sperm into 3 categories of motility: progressively motile (PR), non-progressively motile (NP) and immobile (IM).
The PR category (according to the old classification of category A + B) includes sperm with fast translational (at least half of its own length per second - 0.025 mm/s) or with slow, but still rectilinear movement. The NP category (category C) includes sperm that do not move in a straight line (both those that barely move in place and those that have a circular trajectory). Finally, category IM (category D) - completely immotile sperm.
All categories of motility are usually present in the ejaculate, although not always. There are often quite a lot of immobile sperm in the IM category (40 to 60 percent). As a rule, these are dead or dying “of old age” sperm. Therefore, the less abstinence before ejaculation, the fewer immobile sperm in the ejaculate. There are also usually a lot of fast, straight PR sperm - these are healthy, “young” sperm that have recently formed in the testicles. Non-progressively motile sperm of the NP category are usually 10–15 percent; these are, as a rule, sperm with abnormalities in the structure of the neck and flagellum or “aging”.
In normal fertile sperm, progressively motile sperm (PR or A+B) should be at least 32 percent. Sperm motility is influenced by many factors. In particular, temperature: at body temperature (about +37 °C) the speed of movement is maximum, at room temperature it decreases, and at temperatures less than +10 °C the sperm hardly moves. Therefore, in a number of laboratories, including the MAMA Clinic, the microscope for sperm analysis is equipped with a special heated “thermal table” adjusted to +37 °C.
There are methods that allow you to find out how many sperm among the immotile ones are alive. To do this, the sperm is tinted with eosin. This red substance cannot penetrate the membrane of the sperm, but the membrane of the dead sperm is quickly destroyed, and it turns red. This method makes sense to use in case of akinozoospermia (complete immobility of sperm) to find out whether this immobility is associated with disorders of the flagellar apparatus or with death. Accordingly, a fertility treatment plan can be developed.
A person who sees sperm for the first time under a microscope is usually stunned by the multitude of “ugly”, “crooked” sperm. There are headless ones, two-tailed ones, and ones with a crooked head. But there is no need to be afraid. Special studies have shown that men whose sperm contains up to 96 percent of pathological sperm can have healthy children when treated with IVF and sperm selection using the MAX method.
Of the ten sperm in the field of view, only two are normal. (Figure from WHO laboratory manual for the Examination and proceeding of human sperm, 5th edition, 2010).
The proportion of abnormal sperm is determined by two methods. The first is the study of the morphology of sperm in the native ejaculate, that is, the sperm as it is (native) is examined under a microscope. At the same time, they try to count how many sperm out of every 100 are abnormal. This method is very inaccurate, because, firstly, not all pathologies can be seen without special treatment of the sperm, and secondly, the sperm move and are difficult to examine in detail. Therefore, at the MAMA clinic, the “mandatory package” of ejaculate studies includes a Kruger analysis of a stained semen smear. To do this, a drop of sperm is smeared on a glass slide, dried in a stream of air, treated with alcohol, dried again, immersed in several different dyes, washed off excess paint and dried again. After this treatment, the sperm are glued to the glass, immobilized and colored. They can be easily examined and counted, and abnormalities that are invisible with the first method (for example, the absence of an acrosome) can be detected.
To assess sperm quality, not only the proportion of abnormal sperm is considered (it must be less than 96 percent in a stained smear), but also the average number of abnormalities per sperm (the so-called sperm abnormality index, SDI) and the average number of abnormalities per abnormal sperm (the so-called teratozoospermia index, TZI). If the TZI value exceeds 1.6, the sperm is considered abnormal, and if the SDI value exceeds 1.6, problems may arise even with artificial insemination and patients need IVF + ICSI.
Spermagglutination (gluing of sperm) is a signal of serious immune disorders, which, unfortunately, is not always given due attention. It is often incorrectly thought that agglutination prevents sperm from moving freely and reaching the egg. This is not true. Adhesion itself usually affects a small part of the sperm and does not interfere with the movement of the majority, but the presence of agglutination may indicate the presence of antisperm antibodies in the ejaculate, which can cause infertility.
Antisperm antibodies (ASA, or ASAT) are the body's antibodies against sperm. By connecting to the flagellum, ASA inhibits sperm movement. By sticking to the head, they prevent fertilization. ASA can form in both men and women, causing infertility. To diagnose ASA in sperm, various methods are used, the most common of which is the MAR test (Mixed Immunoglobulin Reaction).
In addition to sperm, the ejaculate contains so-called round cells. This collective name refers to leukocytes and immature cells of spermatogenesis, that is, the cells from which mature sperm are formed in the testicles. Normally, the concentration of leukocytes should not exceed 1 million/ml. It is generally accepted that a high concentration of these immune cells may indicate inflammatory processes in the accessory sex glands (prostate or seminal vesicles). Without special staining, it is difficult to distinguish leukocytes from immature spermatogenic cells, so WHO recommends staining if the total concentration of all round cells exceeds 5 million/ml.
What terms are used to describe sperm disorders?
There are various terms to describe sperm disorders. There is a rule here: definitions ending with “-spermia” refer to the characteristics of the ejaculate, and those ending with “-zoospermia” refer to spermatozoa. In accordance with the recommendations of the World Health Organization, the following nomenclature is used:
- azoospermia - absence of sperm in the ejaculate;
- akinozoospermia - complete immobility of sperm;
- asthenozoospermia - insufficient sperm motility (PR < 32 percent);
- hemospermia - the presence of red blood cells in the ejaculate;
- cryptozoospermia - single sperm can be detected only after centrifugation of the sperm and a detailed examination of the sediment;
- leukocytospermia - increased leukocyte content (more than 1 million/ml);
- necrozoospermia - live sperm less than 58 percent;
- normozoospermia - all characteristics associated with sperm fertility are normal, but deviations that do not affect infertility are acceptable (increased content of round cells, abnormal pH, abnormal viscosity or non-liquefaction of the ejaculate);
- normospermia - all characteristics of the ejaculate are normal, normal sperm;
- oligozoospermia - insufficient sperm count (concentration less than 15 million/ml or total number in ejaculate less than 39 million).
- oligospermia - insufficient ejaculate volume (less than 1.5 ml);
- teratozoospermia - increased content of abnormal sperm (more than 96% when examining a stained semen smear).
In cases where there are several disorders at once, complex definitions are used, for example, “oligoasthenoteratozoospermia” (OAT).
Everything changes
When a patient gets acquainted with the results of a spermogram, he should know the following. Every single characteristic of sperm changes greatly over time. If the sperm volume during analysis was 3 ml, then at the next ejaculation it may have completely different values, and it will also have different values after a month, especially after six months. The same principle applies to other parameters. The WHO guidelines provide the results of an interesting study. Sperm concentration graph of a man who had a spermogram twice a week for two years. Concentration values ranged from 120 million/ml (excellent sperm) to 15 million/ml (oligozoospermia). That is why in reproductive medicine it is generally accepted that for an objective analysis it is necessary to examine sperm at least twice with an interval of at least two weeks, and in case of significant differences in parameters - several times.
In addition, the patient must understand that even the most accurate data has its own area of error. For example, using a Goryaev counting chamber (a precision instrument for determining the number of cells) allows an error of 5 percent. If the results show a concentration value of 20.3 million/ml, this means that the concentration is in the range from 19 to 21 million/ml. If the concentration is indicated as 136.5 million/ml, then it should be perceived as the range of 129.7–143.3 million/ml.
All norms are relative and conditional. It cannot be said that sperm with a volume of 1.6 ml is “still normal”, and 1.4 ml is “already bad”. These values are approximately equal in terms of fertilizing capacity. Some samples with “deviations” may have a much better chance of conceiving than other formally “normal” sperm. For example, an ejaculate with a volume of 1.4 ml, with a sperm concentration of 180 million/ml, good motility (70 percent) and a low content of abnormal forms (22 percent) can formally be classified as a pathological condition of oligospermia. At the same time, formally “normal” sperm will be with a volume of 1.5 ml, a concentration of 16 million/ml, a motility of 35 percent, and three-quarters of abnormal sperm, although the chances of conception with such ejaculate are low. Therefore, only a specialist can correctly assess the condition of the ejaculate.
If you are planning to undergo examination and treatment by an andrologist, have a spermogram done at the MAMA clinic, make an appointment or test. You can do this about a week before your intended visit.
We recommend reading:
- Examination of a man: spermogram;
- Nutrition for “fertile” sperm;
- Bad sperm;
- Men's rules of conception;
- What is a spermogram;
- Spermogram decoding and analysis;
- What is a spermogram, spermogram analysis;
- Revolution for sperm;
- Spermogram - analysis on the verge of art
Take the first step - make an appointment!
or call from 9:00 to 18:00 Moscow time +7 495 921-34-26 8
free phone in Russia
Some features when decrypting
Viscosity and liquefaction rate are two different indicators, but they are never taken into account separately when deciphering a spermogram.
The color of the analysis is influenced by the number of sperm, the presence of red blood cells, white blood cells and mucus. Since all of the listed spermogram indicators are determined using microscopy, and color is a low-informative indicator, it is defined only as a tribute to the historical significance of the analysis.
There are 4 groups of sperm, depending on their motility:
- A – two seconds moving in a straight line at a speed of more than 25 µm/sec.
- B – two seconds are moving in a straight line, but their speed is less than 25 µm/sec.
- C – moving along a trajectory that cannot be described as a straight line, or making movements while remaining in one place.
- D – motionless.
The last two forms (C and D), even if present in the ejaculate, are not capable of fertilizing the egg. When more than 75% of category D sperm are detected, additional tests are performed to determine their viability.
What diseases does hemospermia indicate?
Red blood cells in semen are detected in the following pathologies:
- infectious and inflammatory diseases of the pelvic organs – prostatitis, vesiculitis;
- oncological diseases of the testicles, prostate;
- benign tumors of the pelvic organs;
- prostate adenoma.
A man may have sperm with blood after instrumental manipulation:
- biopsy of prostate tissue;
- injection into the genitals;
- sterilization;
- performing sclerotherapy in the treatment of hemorrhoids.
Elevated red blood cell levels are often found after pelvic trauma.
There is a hypothesis that hemospermia occurs in men due to irregular sperm turnover. Rare sexual intercourse is accompanied by stagnant processes in the pelvis, increased vascular permeability and deterioration of their condition. As a result, at the next contact, ejaculation occurs with blood. This reason has not been scientifically confirmed, but it cannot be completely excluded. In patients with vascular diseases, indeed, the frequency of sexual intercourse can affect the organoleptic properties of semen.
Symptoms
Men rarely pay attention to the color of semen on their own. During sexual intercourse without barrier contraception, it is difficult to notice the problem, since ejaculation occurs in the woman’s vagina. You can see semen coming out with blood during masturbation or when using a condom.
If the red blood cell count is high, a woman may discover the problem by washing herself after intercourse. However, in this case it is impossible to say for sure that there is blood in the sperm. There is a possibility that the coloration of the discharge occurred due to underlying diseases of the cervix.
The asymptomatic course of some pathologies does not allow this sign to be detected. When a clinical picture appears, a man may be concerned about:
- painful sensations in the groin and perineum;
- disturbance of the urination process;
- burning in the urethra;
- decrease or increase in seminal fluid volume;
- increase in body temperature.
Blood in urine and semen can be discovered completely by accident when going to the toilet after intimacy. If the cause is a disease of the urinary system, the color of the urine changes. This is especially noticeable after a long break between urinations or when going to the toilet after waking up in the morning.
If there is blood instead of sperm, this is an alarming signal for a man. The rich red color of the seminal fluid is considered a reason to immediately seek medical help, especially if accompanied by abdominal pain and hyperthermia.
Why does sperm count decrease?
The main reasons for a decrease in the number of sperm in the ejaculate:
- endocrine disorders (diabetes mellitus, adrenal and thyroid dysfunction, underdevelopment of the gonads, impaired hypothalamic-pituitary regulation);
- diseases of the genitourinary organs (varicocele, orchitis, prostatitis, genital injuries, cryptorchidism);
- genetic disorders (eg, Klinefelter syndrome);
- the effect of toxins (alcohol, steroids, sleeping pills);
- feverish condition;
- high external temperature.
How to improve spermogram
Improving the quality of spermogram is possible by following the following recommendations:
- do not overheat;
- eliminate the effects of toxins (nicotine, alcohol, medications and others);
- follow a daily routine, get enough sleep;
- Healthy food;
- ensure a normal rhythm of sexual life for every man;
- engage in physical therapy, including exercises for the abdominal muscles and pelvic floor;
- effectively treat urological and endocrine diseases;
- as prescribed by a doctor, take medications to improve sperm count (biostimulants, vitamins, etc.).
It will be useful to include nuts, bananas, avocados, tomatoes, apples, pomegranates, pumpkin seeds, and asparagus in your diet.
Quite often, to improve sperm quality, doctors recommend dietary supplements to men, for example, Spermactin or Speman. They contain amino acids and vitamins, including carnitine. Such supplements are used in preparation for in vitro fertilization and for the treatment of severe oligoasthenozoospermia. They improve the performance of sperm used for donation or cryopreservation (freezing).
Do not underestimate such a factor as the frequency of sexual intercourse. It should be sufficient for each specific couple; there is no need to “save” sperm. In this case, the likelihood of conception increases even if the spermogram is not very good.