Nerve fibers are an important element of the visual apparatus. It is thanks to them that impulses enter the brain, transmitting information about the world around us. And if the nervous tissue undergoes pathological changes, then this is immediately reflected in visual perception. When the optic nerve becomes inflamed outside the eyeball, retrobulbar neuritis is diagnosed. This disease is accompanied by serious visual impairment and can lead to complete blindness.
Pathogenesis of the disease
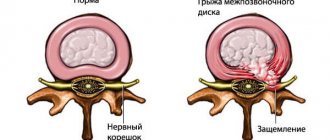
The optic nerve (ON) is a bundle of fibers whose main task is to transmit information from the retina to the brain. The head of the optic nerve, located inside the eyeball, gives rise to more than 1 million nerve endings that envelop the structures of the eye. When leaving the eyeball, the optic nerve is covered with several membranes that protect it from damage and ensure high-speed conduction of impulses. The chiasm, the visual crossroads, is formed in the cranial region.
The nerve sheaths have a close connection with the brain, so damage to the second can negatively affect the condition of the first. Depending on where the inflammatory process is localized, papillitis, neuroretinitis or retrobulbar neuritis are diagnosed. Retrobulbar optic neuritis is an inflammation of the optic nerve located between the optic chiasm and the orbit of the eye. With this disease, parts located outside the eye structures are damaged.
The first thing that occurs is a violation of the information transmission function, manifested by a deterioration in visual acuity and loss of optical fields. With subsequent progression of the pathology, more and more optical fibers are affected, and connective tissue formations form in the areas of destruction. As a result, this leads to loss of vision.
If completely damaged, functions are not restored.
Diagnostics at ON CLINIC
Currently, identifying the disease is not difficult. To diagnose this eye pathology, ophthalmologists at the ON CLINIC International Medical Center carry out:
- computer perimetry to assess visual acuity and fields (this is one of the main methods for identifying pathologies of the optic nerve, retina and glaucoma);
- color perception test;
- ophthalmoscopy, which allows you to see blanching of the nerve disc, narrowing of the vessels of the fundus;
- measurement of intraocular pressure.
Such diagnostics makes it possible to make an accurate diagnosis and prescribe the most appropriate treatment in each specific case.
Causes
The etiology of retrobulbar neuritis is not fully understood, but it is known that the pathology can be both primary and secondary. In the first case, inflammation develops independently, which is extremely rare. Secondary neuritis occurs against the background of other pathological processes. In most cases (65-80%) it appears in multiple sclerosis, in which demyelination of nerve fibers spreads to the optic nerves and causes inflammation.
Also, damage to the optic nerve can occur for the following reasons:
- traumatic brain injuries;
- brain tumors;
- neuroinfections;
- infectious diseases (sinusitis, otitis, cystitis);
- viral infections (herpes, mononucleosis);
- mycotic pathologies;
- autoimmune diseases;
- dental caries;
- allergic reactions;
- viral, fungal eye pathologies;
- blood diseases;
- kidney and liver diseases.
Some systemic diseases (diabetes mellitus, arthritis, gout, vitamin deficiency, and so on) can also provoke the development of pathology.
Due to such a large list of possible causes of optic neuritis, determining the exact etiology of inflammation is often difficult.
Partial optic atrophy in children
Partial atrophy of the optic nerve in children Source: Online-diagnos.ru The optic nerve (lat. Nervus opticus) is the second of twelve pairs of cranial nerves.
Through it, visual stimuli perceived by retinal cells are transmitted to the brain. Optic nerve atrophy is not an independent disease, but a condition resulting from various pathological processes. Pathomorphologically, atrophy is characterized by the disintegration of nerve fibers and their replacement with glial tissue.
Immediately after birth, the baby is examined by specialists, including an ophthalmologist, to identify congenital diseases. This must be done as early as possible to prevent possible complications. One such disease is optic nerve atrophy.
In simple terms, atrophy is the death of nerve fibers and their replacement by connective tissue, and this process is irreversible. Sometimes atrophy develops independently, but most often it is a consequence of other diseases:
- intoxications (including infectious),
- inflammatory processes in the brain,
- pathology of the eyeball,
- tumors,
- injuries
Partial atrophy of the optic nerve in a child is a serious disease, the main characteristic of which is the gradual death of nerve fibers. It can develop at any age and there are many reasons for its occurrence.
This diagnosis can only be made by an ophthalmologist with many years of experience, including practice in the treatment of similar diseases.
As a result of the progression of optic nerve atrophy in a child, the tissue of the nerve itself may gradually die and, as a result, be replaced by connective tissue. It can cause blockage of blood vessels and, as a result, limited access of blood to the eyeball.
When the optic nerve fibers die, the ophthalmologist diagnoses the patient with nerve atrophy. A sick child's vision deteriorates greatly. If the optic nerve has been subjected to inflammation, damage, dystrophy or compression, which negatively affects the condition of its tissues, this leads to optic nerve atrophy.
The disease occurs due to pathologies such as neuritis and stagnation. Congenital hereditary nerve atrophy, which is classified as primary, is often observed.
You need to be wary if the child’s pupil is enlarged and does not respond to bright light, there is no protective motor reflex of the eye when light rays hit it, the baby cannot follow anything with his eye. These are subtle symptoms of optic atrophy.
Optic nerve atrophy is a pathological-dystrophic process characterized by the death of all or part of the fibers of the optic nerve. The optic nerve performs a conductive function, transmitting information received from the retina in the form of impulses to the visual analyzer in the brain.
With atrophy of the optic nerve fibers, a disturbance in the conduction of impulses occurs: color and light perception changes, the dynamics of image perception are disrupted, the information received is transmitted in a distorted form, etc. Partial atrophy provides the possibility of treatment, complete atrophy leads to blindness.
Previously, even partial atrophy of the optic nerve was incurable and meant disability. Today, treatment in the initial stages, when only the first symptoms of the disease appear, has become possible.
Important
It makes no sense to treat the eye in the later stages, with complete atrophy, since restoration of all original functions is impossible due to the anatomical features of the eye, and the consequences of degenerative processes cannot be eliminated.
Optic nerve atrophy in children is considered a rare disease, typical for patients of certain age categories.
It was noted that there is no direct relationship between the patient’s age and the presence of the disease - today very young people, including children leading a healthy lifestyle, suffer from diseases characteristic of people of retirement and pre-retirement age.
And if previously the disease could only be diagnosed in adults, today nerve atrophy is detected in children (even newborns), so predicting the etiology and pathogenesis is often difficult.
Classification
Taking into account the nature of the inflammatory process, retrobulbar optic neuritis comes in two forms:
- Spicy. It occurs most often at a young age, with primary pathology. Visual functions decline very rapidly.
- Chronic. Visual functions deteriorate gradually against the background of cerebral damage. Most often it is a consequence of the progression of acute inflammation. Characterized by alternating periods of exacerbation and remission.
Depending on the location of the inflammatory process, the following types of neuritis are distinguished:
- Axial. The most common type of disease in which damage to the axial fasciculus is accompanied by deterioration of central vision and the formation of scotomas.
- Peripheral. The inflammatory process is localized on the periphery of the nerve and is accompanied by the formation of intrathecal contents, causing pain. Central vision is preserved, but the visual field is narrowed.
- Transversal. The most advanced form of the disease, accompanied by severe dysfunction of the visual apparatus. Inflammation begins in the axial structures and then spreads throughout the nerve trunk, leading to complete blindness.
Considering the extent of damage to the optic nerve, neuritis occurs:
- total – nerve sheaths and fibers are affected;
- axial – inflammation is localized in the papillomacular bundle;
- neuroretinitis – the retinal nerve fibers are additionally affected;
- perineuritis - fibers and membranes are affected.
Depending on the etiology, retrobulbar neuritis can be:
- infectious;
- toxic;
- autoimmune;
- parainfectious;
- ischemic.
Accurate determination of the form of the inflammatory process allows you to select the most appropriate treatment method.
Symptoms of optic neuritis
Clinical symptoms depend on the severity of the inflammatory reaction and the volume of the damaged nerve. Characterized by decreased visual acuity and reduced visual fields. Many people have impaired color vision, especially in the red spectrum. It is possible that scotomas may appear—some areas may fall out of sight.
Eye damage can be either unilateral or bilateral (for example, with diabetes).
If neuritis occurs due to methyl alcohol poisoning, then loss of visual functions can occur in 1-2 days or even at lightning speed.
Mydriasis (dilation of the pupil) and weakening or absence of its reaction to a light stimulus are also observed.
Symptoms of intrabulbar neuritis include:
- Rapid decrease in visual acuity, within 2 days by 0.5-2 diopters. If the nerve is completely damaged, complete blindness is possible. Depending on the infection and medical care provided, it may be reversible;
- Blind spots (scomas) appear in the center of the visual field;
- Twilight vision is impaired. Adaptation of the diseased eye to darkness lasts at least 3 minutes (normally this process takes minutes);
- The ability to distinguish some colors is lost.
In acute peripheral retrobulbar neuritis, the following symptoms are observed:
- Visual acuity is preserved, while the visual field decreases and the lateral visual field completely disappears;
- Pain sensations appear behind the eyeball, which intensify when it is pressed inward or when the head is turned. The pain decreases slightly after the use of non-steroidal anti-inflammatory drugs and completely disappears when treated with corticosteroids.
- There is hyperemia of the optic nerve head, its boundaries become unclear;
With axial neuritis, the following symptoms appear:
- Blind areas (comas) appear in the center of the visual field, which decrease over time;
- Within 2-3 days, there is a sharp decrease in visual acuity by 3-6 diopters. After a few days, vision begins to recover; in very rare cases, the eye may remain blind.
With transversal retrobulbar neuritis, peripheral and axial symptoms are combined.
In chronic retrobulbar neuritis, loss of visual acuity occurs gradually, and pain symptoms are less pronounced. Blind areas appear in the field of vision.
With retrobulbar neuritis of toxic origin, the symptoms differ:
- Within 1-2 days, visual acuity in both eyes is sharply lost, up to complete blindness;
- The pupils dilate, and their reaction to light becomes weakened or completely absent;
- There is hyperemia of the optic nerve head, while the fundus is normal;
- The disease is accompanied by symptoms of intoxication.
- During the first month, vision may improve, then deteriorates again and atrophy of the optic nerves occurs.
Symptoms
The clinical picture of retrobulbar neuritis of the optic nerve depends on the nature of its course.
Read in a separate article: Excavation of the optic nerve head: what is it, types and features
Acute form
Pathological manifestations occur immediately after the development of the inflammatory process. Accompanied by the following symptoms:
- decreased visibility;
- soreness in the area of the eyeballs;
- color vision impairment;
- edema;
- hyperemia.
First one eye is affected, and then the second.
Chronic form
Deterioration in visibility occurs gradually; after some time, the nerve atrophies and a scotoma is formed. In this case, the patient sees poorly in the dark, notes the appearance of hallucinations and complains of a headache. Sometimes there is eye hyperemia and nausea.
The following symptoms may indicate inflammation of the optic nerve:
- photophobia;
- flashes of light before the eyes;
- blurred image;
- increased sensitivity of the retina;
- weakness;
- pain in the eyes, eyebrows;
- myopia.
Symptomatic manifestations can intensify after severe physical exertion or mental stress. If the above symptoms are complemented by other unpleasant phenomena, greatly worsen the general condition or cause unusual sensations (numbness, weakness of the limbs, hyperthermia), then you should immediately consult a doctor.
Treatment price
The cost of treatment for optic nerve atrophy at MGK is calculated individually and will depend on the volume of therapeutic and diagnostic procedures performed. You can find out the cost of a particular procedure by calling 8 (495) 505-70-10 and 8 or online, using Skype consultation on the website, you can also familiarize yourself with the “Prices” section.
Go to the “Prices” section>>>
4.53/5 (144 ratings)
Yakovleva Yulia Valerievna
Possible complications
If treatment is incorrect or untimely, retrobulbar optic neuritis can cause the following complications:
- irreversible destruction of nerve trunk cells;
- nerve damage;
- optical neuropathy;
- partial or complete blindness;
- multiple sclerosis.
If steroids are taken for a long time to treat a disease, there is a negative effect on the immune system. This leads to the body becoming more susceptible to infections, sometimes resulting in osteoporosis.
Causes
Neuropathy is non-inflammatory damage to the nerves. The name combines various degenerative-dystrophic changes in peripheral nerves. The nervous system is formed by peripheral nerves and various nerve plexuses, the brain and spinal cord.
Peripheral nerves, having a thin and at the same time complex structure, are unstable to damaging processes. There are mononeuropathy, which means damage to one nerve, multiple mononeuropathy, in which several nerves are involved in the process, but in different parts of the body, and polyneuropathy, which involves several nerves and is localized in one area.
Causes of neuropathy
· diabetic neuropathy is damage to nerve fibers and small vessels due to high levels of sugar and lipids in the blood.
· toxic neuropathy – the cause is nerve damage due to infectious diseases, among which are diphtheria, HIV, herpes, etc. The normal state of the nerve trunks is disrupted by poisoning with chemicals and the over-dosed use of certain medications.
· post-traumatic – often a strong blow or other acute injury leads to disruption of the integrity of the myelin sheath of the nerve. This form is the result of compression of nerve fibers during bone fractures, improper formation of scars and tissue swelling. The most common lesions are the sciatic, ulnar and radial nerves.
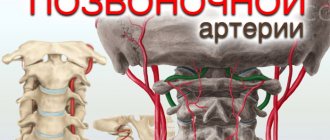
Anterior ischemic neuropathy is pathogenetically caused by impaired blood flow in the posterior short ciliary arteries and the resulting ischemia of the retinal, choroidal (prelaminar) and scleral (laminar) layers of the optic disc.
In the mechanism of development of posterior ischemic neuropathy, the leading role belongs to circulatory disorders in the posterior parts of the optic nerve, as well as stenosis of the carotid and vertebral arteries.
Local factors of acute circulatory disorders of the optic nerve can be represented by both functional disorders (spasms) of the arteries and their organic changes (sclerotic lesions, thromboembolism).
Diagnostics
To diagnose retrobulbar neuritis of the optic nerve, the following research methods are necessary:
- blood and urine tests;
- ophthalmoscopy;
- perimetry;
- visometry;
- biomicroscopy;
- fluorescein angiography;
- Ultrasound;
- CT, MRI.
Additionally, you may need to measure blood pressure and body temperature, blood tests for sugar and PB, as well as consultation with a neurologist and therapist.
Prognosis and prevention
There is no effective treatment. However, up to 40% of patients with nonarteritic infarction experience spontaneous partial recovery of function.
Even with the best predictions from doctors, it is almost impossible to completely restore vision. Full compliance with the entire treatment complex and compliance with all medical prescriptions will not save you from a decrease in visual acuity.
As a result, vision may still decline, and some defects associated with vision and atrophy of nerve fibers will remain. Every second patient manages to improve visual indicators by 0.2 units; this result is achieved only with intensive treatment in compliance with all necessary measures.
If the patient is faced with ischemia of both eyes, there is a risk of complete blindness without the possibility of restoring vision.
First aid
Before the cause of inflammation of the optic nerve is identified, the patient is prescribed antibacterial and anti-inflammatory therapy, as well as immunomodulators and agents to improve metabolic processes in the structures of the central nervous system. For 7 days, the patient must receive injections of broad-spectrum antibiotics and corticosteroids. The most commonly prescribed drugs are:
- Dexamethasone;
- Prednisolone;
- Solcoseryl;
- Piracetam;
- Diacarb;
- Glycerol;
- Urotropin;
- Dibazol.
Also, over the course of a week, a 40% glucose solution should be administered intravenously, a 0.1% adrenaline solution should be instilled into the nose, and 10 ml of a 25% magnesium sulfate solution should be injected intramuscularly.
It is prohibited to use ototoxic drugs, as they have a negative effect on the optic nerve.
Preventive measures
In order to prevent the development of the disease, it is recommended to carry out timely treatment of any systemic, metabolic and vascular diseases. After the appearance of symptoms of the disease, the patient is recommended to regularly visit an ophthalmologist; the patient must comply with all the doctor’s requirements.
At the slightest deviation in vision, it is important to promptly contact an ophthalmologist and undergo regular examination by a doctor. Any vascular diseases, metabolic disorders must be examined and treated so that complications do not develop, incl. and before our eyes. After the first symptoms appear, contact a medical institution and comply with all requirements.
Unfortunately, quite often, despite the therapy, the prognosis for ischemic neuropathy remains unfavorable: decreased vision and peripheral vision defects that have developed as a result of optic nerve atrophy persist. If both eyes are affected, low vision or complete blindness may occur.
To prevent the formation of the disease, adequate and timely treatment of vascular and systemic pathologies is necessary.
Patients with a history of ischemic optic neuropathy are subject to medical examination by an ophthalmologist.
The prognosis of ischemic optic neuropathy is unfavorable: despite treatment, a significant decrease in visual acuity and persistent peripheral vision defects (absolute scotomas) caused by optic nerve atrophy often persist. An increase in visual acuity of 0.1-0.2 can be achieved only in 50% of patients. If both eyes are affected, low vision or total blindness may develop.
For the prevention of ischemic optic neuropathy, treatment of common vascular and systemic diseases and timely seeking medical help are important. Patients who have suffered ischemic optic neuropathy of one eye require clinical observation by an ophthalmologist and appropriate preventive therapy.
Treatment
Treatment of retrobulbar neuritis depends on many factors and is selected on an individual basis. If the pathology was detected at an early stage of development, then drug therapy is prescribed, which may include the following drugs:
- antibiotics: Ceftriaxone, Tsiprolet;
- corticosteroids: Hydrocortisone, Methylprednisolone;
- diuretics: Furosemide, Acetazolamide;
- antihistamines: Chloropyramine, Desloratadine;
- interferons: Betaferon, Extavia;
- NSAIDs: Nimesulide, Interferon.
Vasodilators and antispasmodics, B vitamins, cholinesterase inhibitors and drugs to improve blood circulation are also prescribed. If the cause has been established, antiviral and anti-tuberculosis drugs may be prescribed. To achieve the best effect, it is recommended to undergo a course of physiotherapy (magnetic therapy, laser stimulation).
In severe cases, when conservative treatment fails, a surgical procedure called optic nerve sheath decompression is performed. The essence of this operation is to open the nerve sheath, thereby reducing intraocular pressure. Treatment tactics depend on the root cause and characteristics of the course of the pathology and can only be selected by a qualified specialist.
It is prohibited to take medications or folk remedies on your own.
How is optic nerve atrophy treated in children?
The outcome of the disease is favorable if timely and correct therapy is prescribed. The basis of treatment includes procedures to stop the atrophic process and preserve residual vision. Lack of treatment will lead to complete blindness.
If drug treatment is used, drugs are prescribed that improve blood circulation and metabolism. At the same time, taking vasodilators, multivitamins and biostimulants is indicated. With the help of these drugs, you can improve blood circulation, nutrition and activity of the optic nerve head.
Drugs from these groups help stimulate the vital activity of the remaining nerve fibers. If surgical intervention is indicated, then it is possible to eliminate the underlying disease that led to the pathology of the optic nerve.
Success in treatment depends on the timely initiation of therapy.
There may be an opinion that partial atrophy of the optic nerve is less dangerous, but this is not the case. Contributing factors during the transition from partial atrophy to the complete form may be:
- infectious diseases;
- increased load on the eyeball;
- pressure on the central nervous system.
If there is a hereditary pathology, therapy becomes more complicated.
The main goal of treating atrophy is to stop its development and convert complete atrophy to partial. Unfortunately, it is impossible to completely cure it, since dead tissue cannot be restored or regenerated.
An ophthalmologist can prescribe medication using special medications. They are determined based on how advanced the disease is and how early the patient sought help.
As with any ophthalmological disease, the most important role is played by the timeliness of seeking qualified help, since congenital partial atrophy of the optic nerve, the treatment of which is available here, in a progressive stage can lead to complete blindness.
A neurologist, micropediatrician and ophthalmologist increase the trophism of the child’s eyes. Glucose is used (up to 10 times a day), dibazole, vitamins in tablets and eye drops, amidopyrine, taufon, acetylcholine, ENKAD, cysteine, and other drugs that can at least slightly revive the vision analyzer.
Compliance with doctors' recommendations allows many patients to partially regain their vision after complex and neurovascular therapy using laser and reflex physiotherapeutic techniques.
Primary atrophy of the optic nerve in children is expressed by the limitation of the disc by a pale border. There are deviations in the level of deepening of the disc - excavation, it looks like a saucer, the arterial vessels of the retina are narrow.
Signs of secondary atrophy are unclear boundaries of the disc (it protrudes in the center), dilated retinal vessels.
Partial atrophy of the optic nerve is also possible, in which the functioning of the organ of vision is minimally affected. The nerve was not completely damaged and no destructive effect developed.
Signs of partial atrophy of the optic nerve: narrow field of vision (sometimes tunnel syndrome), blind spots called scotomas, insufficiently sharp vision.
Important
All actions in the treatment of optic nerve atrophy in a child are aimed at inhibiting the development of the disease and preventing complete death of the optic nerve if there is partial death. Before starting treatment, the causes of the disease are determined.
Medications are prescribed to enhance the nutrition of the nerve and non-dead cells during oxygen starvation. Drugs can be administered in different ways: drops, electrophoresis, injections. In some cases, ultrasound and oxygen therapy are useful.
Below we will tell you in more detail about the causes of optic nerve atrophy in children, the treatment of this disease using modern methods, and consider the characteristic symptoms of partial optic nerve atrophy.
Since optic nerve atrophy most often develops secondary, it is important to identify the cause and come to grips with the treatment of the underlying disease. If necessary, even surgical treatment is performed.
Unfortunately, today visual fibers that have died from atrophy are practically impossible to restore. The principle of treatment for this disease comes down to maintaining existing visual functions.
- The child is prescribed medications that improve blood circulation and trophism, including optic nerve tissue;
- vasodilators, biostimulants, vitamins, enzymes, etc.
- In the absence of contraindications, physical treatment may be recommended: ultrasound, acupuncture, laser stimulation, electrical stimulation, oxygen therapy, electrophoresis.
Treatment of optic nerve atrophy If optic nerve atrophy was diagnosed at an early stage and treatment was started in a timely manner, then it is possible to achieve preservation and sometimes a slight increase in visual acuity, but, alas, complete recovery does not occur.
If atrophy progresses rapidly, or treatment is started too late (or not started at all), then complete and irreversible blindness develops.
Remember!
At the first sign of visual impairment in your child, you should consult an ophthalmologist. Only a specialist will be able to make the correct diagnosis and prescribe the necessary therapy. Self-medication is often harmful and even dangerous to health. Take care of your children!
Treatment of optic nerve atrophy at any stage is very difficult for doctors. It is impossible to cure atrophied fibers, but it is necessary to cure the remaining fibers of the eye nerve so that the disease stops progressing.
If timely treatment is not applied, you can completely lose your vision and become disabled.