What is Prenetix, how long does it take to take it?
Non-invasive prenatal test (NIPT) is an opportunity to early identify the most common genetic diseases in the fetus: Down, Edwards, Patau, Turner syndromes.
- Performed after ten complete obstetric weeks of pregnancy
- Results within 12 working days
- Safe for the health of women and children
- Available in all regions of Russia
- Recognized as the most objective and accurate in the world
| > 22 000 Number of patients who participated in testing the technology | 99,9% Test accuracy confirmed by research | >1 000 000 Number of women from different countries who trusted the Prenetics test |
Reviews for non-invasive prenatal DNA test
Diagnostics is a fundamentally new method, so many women, when deciding to undergo such a study, are guided by the reviews of those who have already undergone it.
Review #1
According to biochemistry, there was a high risk of Down syndrome (1:9), but an ultrasound showed that the thickness of the nuchal translucency was normal, the nasal bone was visible from the 11th week of pregnancy. They offered me amnecentesis, but I decided that it would be better to give the money. The research was carried out on Tula in Genomed, and she paid 35,000 rubles. My husband was also offered to take a DNA smear; it turned out that this way he could get the result faster, and there would be no need to re-donate blood. The result was ready within 10 days.
The verdict came to us by mail. Thank God the risk was low. Doctors said the test is 99% accurate. I don’t know whether to recommend doing the test, but it helped us get through that difficult period.
We recommend Can a pregnancy test be wrong?
Anna
Review #2
I did the test in, which is located on Starokuzmikhinskoe highway. I liked the laboratory, and the cost of the test is lower than in other clinics. The test result is good, we were additionally advised by a geneticist, Mikhail Ivanovich. He was the one who helped resolve many issues. The main thing is that the test is completely safe, and you can additionally find out the sex of the child.
Irina
Why take the Prenetix test?
Prenetix is a safe confirmation of diagnosis with 99.9% accuracy. Before the invention of non-invasive tests, there were two ways to confirm the diagnosis: examine fetal tissue by puncturing the abdominal wall or wait until delivery. Although the probability of pregnancy termination due to invasive diagnostics is low, not everyone wanted to risk the life of the child. Waiting for the birth and being left in the dark is stressful for the family.
Now there is an alternative to puncture - a non-invasive prenatal DNA test. Since the technology is new, testing is not yet considered mandatory in Russia. But the World Health Organization recommends it to every pregnant woman: even a low risk of 1:10,000 according to the first screening means that out of ten thousand children one is born sick.
What is the accuracy of the NIPT test?
NIPT is a highly accurate method. Its accuracy, according to the results of numerous studies, is up to 99.9%. At the same time, a low percentage of the need to re-sample blood due to a lack of fetal DNA in the sample was noted (less than 3% of cases), a low percentage of false positive results (that is, those cases when, with a positive test result, the child turns out to be healthy - no more than 0.72% or 1 case in 140). This means that only 1 case out of 140 positive test results will not confirm fetal pathology, and in 139 cases the test will reveal it.
The rate of false negative results (that is, cases when the test is negative for existing fetal pathology) is no more than 1 case per 10,000 tests.
However, when deciding to conduct a test, you need to be fully aware that this test is not a diagnosis, but only with a very high probability allows you to suspect a chromosomal pathology of the fetus. If a serious pathology of the fetus is suspected and the question of the possibility/impossibility of continuing the pregnancy is discussed, confirmation will be required using additional tests - chorionic villus biopsy, amniocentesis, etc., i.e. invasive diagnostics. However, due to the extremely low percentage of false-positive results, such studies will be required an order of magnitude less often than during standard screening.
What does Prenetix show?
Non-invasive prenatal diagnostics reveals the following pathologies:
- Down syndrome. Severe mental retardation and congenital defects. The most common chromosomal pathology.
- Edwards syndrome. Oligophrenia: pathologies of the skull, brain, chest, heart. Up to 5% of newborns with Edwards syndrome survive to one year.
- Patau syndrome. Severe developmental defects; out of 100 children, 5 survive to one year.
- Klinefelter's syndrome. Male disease: pathologies of the endocrine system, infertility, impotence.
- Turner syndrome. Female disease: infertility, physical retardation, tendency to obesity and heart disease.
- Extra X and Y chromosomes. Minor mental and/or physical abnormalities.
What Prenetics will not show
Prenetix studies only pathologies of chromosomes 21, 18, 13, X and Y. The analysis does not determine mutations of other chromosomes or hereditary diseases. The NIPT test will not give a reliable result in the following cases:
- Pregnancy with more than two fetuses;
- Chromosomal mutations in the mother;
- Malignant tumors;
- Donated bone marrow or organs from the mother;
- Recent blood transfusion;
- Death of one of the twins.
Why Prenetix is 99.9% accurate: diagnostics using new technology
It is impossible to study entire DNA molecules, so when testing they are divided into sections. In each section, the sequence of the structural blocks of the molecule - nucleotides - is studied. Disturbances in the order of nucleotides cause deviations in human development.
Sequencing is reading the sequence of nucleotides in DNA. There are two methods of sequencing: random and sample sites. Random research is ineffective: all DNA sections are studied, and the risk of not identifying pathology in the right ones increases. Selective sequencing examines only those regions whose mutations lead to common developmental defects.
Prenetix is based on selective examination of DNA fragments, with each section read more times than in other technologies. Then the computer program evaluates the research data, the height, weight, age of the pregnant woman, the concentration of cfDNA in the blood and displays the results.
What is the difference?
The main difference between a non-invasive test and an invasive one lies not only in the biomaterials used for testing, but also in the methods of collecting these materials themselves. Thus, with invasive techniques, specialists have to penetrate into the space of a woman’s uterus to take biopsies. Using a special syringe (probe), they pierce the abdominal wall and, depending on the type of testing, take for research:
- some amniotic fluid (during amniocentesis);
- fetal blood from the umbilical cord vessels (during cordocentesis);
- a fragment of one of the outer membranes (chorion) of the fetus (during chorinobiopsy).
In the case of a non-invasive genetic test in Perm, only blood from a vein is taken from the expectant mother for research. No penetrations into the internal cavity of the uterus are made, as a result of which we can conclude that the non-invasive technique is certainly safer than the invasive one.
Advantages of Prenetix prenatal diagnostics
| Accurate result | Eleven clinical studies, of which three were independent, showed that Prenetix is reliable in 99.9% of cases. For other non-invasive tests, the total number of studies is less than for Prenetix, so the result is not guaranteed. |
| Early deadline | Prenetics is performed at the full 10th week of pregnancy. A prenatal DNA test will give an accurate answer about the presence or absence of chromosomal pathologies at the earliest stage of pregnancy. |
| Any type of pregnancy | Only Prenetix will show true results in twin pregnancies, surrogacy, IVF, if donor sperm or eggs are used. Other tests will not work. |
| Testing throughout Russia | Representative offices of the Genetico Center operate in every region. It is enough to take a blood test in Moscow or any other city and get the result within 12 working days. |
| Rechecking the result | To make a correct diagnosis, the test results are checked by two doctors before being issued. |
| Determining the sex of a child at an early stage | A non-invasive blood test will show the exact sex of the baby from ten weeks, including in twin pregnancies. On ultrasound, sexual characteristics are noticeable no earlier than 23 weeks. |
| No risks | Blood for analysis is taken from a vein, so there is no risk of miscarriage or infection, as in the case of invasive diagnostics. |
| Reliability | More than 1,000,000 women around the world have taken the test. More than 22,000 people participated in the studies. |
Prenatal screening: clarifying tests
A “bad” result from prenatal screening is not uncommon. In accordance with the FIGO Recommendations (2015)1, if the calculated risk of having a child with a chromosomal pathology is 1:100 or higher, the patient must be offered clarifying tests. Every time we get “bad” results, we worry along with the patient, but we try to explain that it is too early to cry. Clarifying tests most often make it possible to reliably prove that the baby is healthy.
“All the girls there were crying, I was the only one who was sure that everything would be okay!” — the pregnant woman tells me, proudly showing a piece of paper with the result 46XY. We will give birth to an excellent healthy boy without chromosomal pathology.
Yes, the likelihood that the child is completely healthy is very high. But if the fetus does have genetic abnormalities, you need to know about it in advance. Consultation in such cases is carried out by specialists in medical genetics, who can talk in detail about the results of clarifying testing and help parents decide whether to continue or terminate the pregnancy.
In fact, there are only two clarifying tests - invasive and non-invasive
. An invasive test is an intervention into the world around the fetus to obtain cellular material. Non-invasive - a study that is carried out on the mother's blood. Of course, donating blood from a vein after the 10th week of pregnancy is not at all scary, but it is very expensive and is not covered by the compulsory medical insurance fund. Both methods have their limitations, so it is worth considering them in more detail.
Invasive tests
Invasive tests are performed by highly qualified specialists. The purpose of the tests is to obtain fetal cells to study its chromosome set. At 10–13 weeks, a chorionic villus biopsy
. A special instrument is inserted through the cervix to pinch off small fragments of the placenta.
amniocentesis is performed at 15–20 weeks.
- under ultrasound control, a puncture is made with a thin needle and a small amount of amniotic fluid is collected.
Both procedures have their own risks and a 1-2% chance of miscarriage. That is why invasive tests are recommended only in cases where the likelihood of having a child with a chromosomal disorder is higher than 1–2%.
Cells obtained through invasive procedures can be examined in different ways:
- karyotyping
- the study is carried out within 2 weeks, the fetal chromosomes are arranged in a special order and make sure that there are no extra or damaged ones in the set; - The FISH method
is a quick way to exclude the most common anomalies in the 13th, 18th, 21st pair and anomalies of the sex chromosomes X and Y. If abnormalities are found, karyotyping is required; - advanced molecular genetic analysis
, which can detect microdeletions - small chromosome breaks that lead to serious diseases; - specific DNA tests for specific diseases
. For example, if healthy parents are carriers of the cystic fibrosis gene, they can each pass on a “sick” gene to their child, and the child will suffer from a serious illness.
NIPT - non-invasive prenatal testing
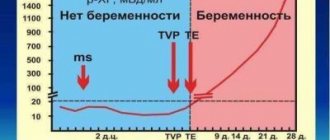
This is a completely new method that has been gradually entering clinical practice since 2011. Starting from the 9th–10th week of pregnancy, placental cells (trophoblasts) are isolated from the mother’s blood and their DNA is examined. This turned out to be enough to accurately diagnose the chromosomal pathology of the fetus in a very early stage of pregnancy (before the standard first screening).
The new method demonstrates excellent efficiency. According to researchers, out of 265 women with “poor” results of standard screening, only 9 patients will actually have a chromosomal pathology of the fetus identified2. If pathology is detected using NIPT, invasive methods will confirm the disease in 9 out of 10 fetuses3.
NIPT is a fairly expensive study. Highly accurate determination of the sex of a child is a very small free bonus of the method. Of course, the more parameters to be studied, the more expensive the analysis. A standard NIPT panel with an accuracy of 99% allows you to exclude Down syndrome, Edwards syndrome, Patau syndrome and sex chromosome abnormalities (this is a large group of diseases when instead of two sex chromosomes, one, three or even four are found).
The most expensive option is an extended study with microdeletions (small chromosome breaks), which makes it possible to exclude/confirm 22q11.2 deletion (DiGeorge syndrome), 1p36 deletion (Angelman syndrome, Prader-Willi syndrome, cat cry syndrome).
For example, 22q11.2 deletion of the fetus in young mothers is detected more often than Down syndrome4, and this pathology may not be immediately noticed even in newborns, and it is characterized by congenital heart defects, abnormalities in the structure of the palate, developmental delay, and schizophrenia at a young age.
Who should do NIPT?
You can find a huge number of indications for this test on the Internet. This includes the mother’s age 35+, habitual miscarriage, and cases of such children being born in the family. In fact, the only indication for NIPT is the woman’s desire
.
FIGO in 2020 proposed using the following diagnostic algorithm:
- at a risk of 1:100 or higher, carry out invasive diagnostics immediately, or first NIPT, then invasive diagnostics for those who have an abnormal result;
- at a risk from 1:101 to 1:2500, NIPT is recommended;
- if the risk is less than 1:2500, in-depth prenatal screening is not indicated.
It is much more important to understand in which cases the use of NIPT is impossible or inappropriate:
- history of blood transfusion;
- history of bone marrow transplant;
- maternal cancer;
- multiple pregnancy (three or more fetuses);
- twins in which one of the fetuses froze;
- donor egg/Surrogacy;
- the presence of ultrasound markers of chromosomal pathologies (in this case, NIPT is no longer needed).
In this case, it is very difficult to separate whose DNA is whose (the mother’s, one, or second, or third fetus, blood or tissue donor), so the results are uninformative.
Non-invasive tests have different brand names (Panorama, Prenetix, Harmony, Veracity) and differ slightly in the technique of execution. Each company carefully cherishes its “idea” and believes that its NIPT is much better than others.
What should you consider?
If your first screening reveals a high risk of chromosomal abnormalities, it is important to understand that risk is not a diagnosis. But if a woman is categorically against having a child with a chromosomal abnormality (it is important to understand that at the current stage of development of medicine such diseases are incurable), an invasive test is mandatory. It is possible to terminate a pregnancy after the 12th week only by decision of a medical commission with serious arguments in hand.
If a woman decides to carry the pregnancy to term in any case, she has the right to refuse further diagnostic procedures. At the same time, more specific information will help parents prepare for the birth of a “syndromic” child: find support groups on social networks, talk with parents raising such children, draw up a medical care plan in advance.
When it comes to choosing between invasive techniques and NIPT, it is important to understand that invasive test materials can be examined in different ways - and detect all sorts of diseases. And the NIPT technique answers only those questions formulated by the doctor. This is why invasive diagnostics still have the final word, although false-positive results occur with any type of testing.
Parents also have the right to completely refuse screening or any clarifying tests. In this case, it is sufficient to sign an informed voluntary refusal to intervene. However, if a woman changes her mind and still wants to undergo testing, some of them (those that are carried out strictly during certain periods of pregnancy) will no longer be possible.
Oksana Bogdashevskaya
Photo istockphoto.com
1. Best practice in maternal-fetal medicine. Figo Working Group On Best Practice in Maternal-Fetal Medicine // Int. J. Gynaecol. Obstet. 2020. Vol. 128. P. 80–82. [PMID: 25481030] 2. Norton ME, Wapner RJ Cell-free DNA analysis for noninvasive examination of trisomy // N Engl J Med. 2020. Dec 24; 373 (26): 2582. 3. Dar P., Curnow KJ, Gross SJ Clinical experience and follow-up with large scale single-nucleotide polymorphism-based noninvasive prenatal aneuploidy testing // Am J Obstet Gynecol. 2014 Nov; 211 (5): 527. 4. Combined prevalence using higher end of published ranges from Gross et al. // Prenatal Diagnosis. 2011; 39, 259-266.