Calculator for assessing hCG dynamics after IVF
Determination of an elevated level of hCG in the blood is the earliest and most reliable sign of implantation of a developing embryo. And, despite the fact that hCG concentration alone is not able to unambiguously indicate a successful pregnancy, and its normal variability suggests a fairly wide range of values at each week of gestation, a natural increase in hCG in the first days of pregnancy, as a rule, indicates its viability and normal development.
A properly developing pregnancy in the vast majority of cases is characterized by a doubling of the concentration of hCG in the blood every 36-72 hours to a level of 1200 mIU/ml, then every 48-72 hours hCG increases by more than 50% to a level of 6000 mIU/ml. Subsequently, as pregnancy progresses, the doubling time of hCG concentration in the blood increases, losing its pattern, and therefore its practical significance. Already in the second trimester, the growth of hCG will slow down even more, and, ultimately, reaching a plateau, it will even decrease.
In general, after the 5th week, when it becomes possible to localize and visually monitor the process of pregnancy progression using transvaginal ultrasound scanning, determining the hCG level and assessing the dynamics of its increase loses practical meaning. At this time, the best evidence of a correctly developing pregnancy is confirmation of the location of the fertilized egg inside the uterine cavity, and subsequently recording the heartbeat of the developing embryo.
It has been noted that in fatal pathologies and ectopically located pregnancies, the concentration of hCG in the first days often increases more slowly than expected. In addition, early miscarriage (the so-called biochemical pregnancy) is accompanied by a drop in the control level of hCG. That is why dynamic assessment of hCG levels is often used in practice as the very first tool for monitoring early pregnancy, including after IVF.
What is the normal growth rate and hCG analysis?
All women carrying a child undergo certain tests, based on which the doctor makes a diagnosis and monitors how the pregnancy progresses. But not everyone understands the meaning of the numbers that will result from decoding the test. Only a specialist can do this correctly and give the optimal result of deciphering such values. A woman can also do this on her own if she finds an online calculator on the Internet, with which you can determine the norm and growth of hCG hormones in the early stages of pregnancy.
HCG means what level of growth and protein-producing hormone is in the blood. This hormone is capable of secreting certain substances that promote fetal development. This happens as soon as the latter attaches to the inner surface of the uterus. This process is usually carried out on the 3rd or 4th day after the woman’s cell is fertilized.
During the first period of gestation, hCG can control the production of the hormone in the ovaries. With the help of such a hormone, pregnancy proceeds in an acceptable state. These hormones are:
- Progesterone.
- Estriol.
- Estradiol.
The largest amount of such elements in the blood of the expectant mother is achieved at 7-8 weeks of pregnancy. When the gestation period of the fetus comes to an end, the amount of such hormones in the mother’s body gradually becomes smaller, as the fetus itself begins to produce them. The minimum amount of elements in the mother’s blood will be observed during the period of the end of gestation.
When a doctor diagnoses early pregnancy, the level of the hCG hormone in the woman’s blood will increase 9-10 days after the fertilization process. A specialist determines this rate and growth of the hCG hormone by the amount of protein in the urine during analysis. In order for the norm and growth of such hCG hormones to be determined as accurately as possible during the analysis, the test should be done no earlier than in the second week of pregnancy. When taking an analysis for normal or increased growth of the hCG hormone, it is worth providing the doctor to the laboratory with the urine that was collected on the morning of the appointed day, since this is where the largest amount of such protein is stored.
When pregnancy occurs, male hormones are also produced in a certain amount in the woman’s body, especially in the early stages of pregnancy. An increased level of male hormone contributes to the formation of sexual characteristics in the fetus. The amount of male hormone will determine whether a girl or a boy is born. Increased growth of such a hormone can be determined by taking an analysis in the early stages. The higher the level of this hormone in the body, the higher the likelihood that a boy will be born.
How to use a calculator for assessing hCG dynamics after IVF?
The hCG calculator allows you to compare the registered hCG level with the average statistical value for each day after embryo transfer, starting from the 10th to the 21st day, after which ultrasound acquires greater diagnostic significance in assessing the course of pregnancy. In addition, the HCG Calculator allows you to analyze the dynamics of hCG levels in the first days of pregnancy, helping to identify pregnancies that are at risk of a negative outcome.
To get the result you will need :
- Specify hCG levels
- Specify the interval in hours between studies
- Select the day after embryo transfer into the uterine cavity as part of the IVF program
- Click COUNT
For a new calculation, you must use the ZERO button.
How to use the calculator
To calculate the hCG increase, enter the first and second hCG values, the number of days after ovulation, and the number of hours between the two tests.
The calculator will calculate the difference between the two tests, the doubling time of hCG and the increase in hormone levels over two days.
On the graph you will see the possible (minimum, average and maximum) values for your period from ovulation and your hCG values. Normally, the hCG level should be between the top and bottom of the graph.
HCG by day
HCG is a hormone that helps determine pregnancy in the earliest stages, even when ultrasound is not yet informative. The most accurate method for determining the gestational age is to draw a chart.
Please note that the period determined by you will differ from what your doctor tells you. The fact is that there is an obstetric gestational age, calculated by the doctor relative to the last menstruation. And the result of the hCG analysis will show the real gestational age relative to the day of conception, and it reflects the real age of the child.
In addition, it should be remembered that each pregnancy is individual. And your indicators may differ from the average, but at the same time be the norm for you. Especially if such differences are insignificant and last up to 24 hours.
If you use the hCG calculator by day, it is most convenient to use the number of days relative to conception (53%), in second place is the number of days relative to the delay of menstruation.
How does hCG increase by day?
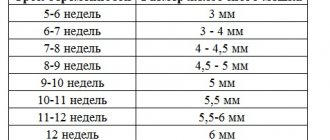
There is a special table of hCG by day, which presents indicators such as the age of the embryo depending on the level of hCG.
HCG value by day:
- at 1-2 weeks they are characterized by an indicator of 25-156 mU/ml;
- at 2-3 weeks the level is already 101-4870 mU/ml;
- 3-4 weeks – 1110-31500 mU/ml;
- 4-5 weeks – 2560-82300 mU/ml;
- 5-6 weeks – 23100-151000 mU/ml;
- 6-7 weeks – 27300-233000 mU/ml;
- 7-11 weeks – 20900-291000 mU/ml;
- 11-16 weeks – 6140-103000 mU/ml;
- 16-21 weeks – 4720-80100 mU/ml;
- 21-39 weeks 2700-78100 mU/ml.
Human chorionic gonadotropin is one of the most important indicators of the presence and development of pregnancy. The exponential increase in hCG by day of pregnancy begins after the embryo is implanted into the uterus. The chorion produces the hormone already 6-8 days after the fertilization of the egg.
In the first trimester, hCG guarantees support for the corpus luteum during pregnancy. stimulates the production of hormones such as estrogen and progesterone. And this support is necessary until the fetus-placenta system begins to function independently.
A must-have for an expectant mother is to register with the clinic and enter into an agreement for pregnancy management from the 8th week of pregnancy.
CIR offers:
current research methods - high standards - extensive monitoring capabilities for pregnant women - the work of experienced and renowned specialists who know everything about pregnancy and even more.
Online hCG calculator
The calculator will help you when deciphering blood tests for hCG. You will be able to monitor the growth dynamics of Beta-hCG and determine the duration of pregnancy.
The results indicated in the tables and the hCG calculator itself are approximate. To determine this hormone, various methods can be used and indicators may vary. Therefore, the analysis is deciphered where it was done. The units of measurement for the concentration of beta-hCG are also different. The concentration is indicated in honey/ml, mIU/ml, U/l and IU/l as well as U/l mIU/ml, IU/l. All indicators are the same and do not need to be recalculated. U stands for units, IU stands for international units, mIU/ml and U/l are the English display of units.
Free hCG
Free hCG is used in first and second trimester screening to diagnose and monitor fetal abnormalities. In addition to screening tests, the pregnant woman undergoes an ultrasound. In the first trimester, from weeks 10 to 12, a “double test” is performed, in which free hCG is tested together with PAPP-A (pregnancy-associated plasma protein A). First trimester screening is carried out to identify chromosomal abnormalities in the fetus: trisomy 21 (Down syndrome) and trisomy 18 (Edwards syndrome). Second trimester screening is a “triple test” that includes free estriol (E3), alpha-fetoprotein (AFP) and hCG. Second trimester screening also examines the manifestation of fetal developmental abnormalities. AFP analysis with hCG is carried out at 15-20 weeks, since earlier the level of AFP concentration in the blood is not reliable. The ratios of these indicators are used as an indicator of pathologies.
The risk of developing an anomaly is calculated using the deviation of indicators from the average values for a given period of pregnancy (for example, AFP and hCG) - MoM (multiple of the median). Pathology is determined by a combination of indicators (PAPP-A, AFP, E3, hCG) MoM. Such combinations are called MoM profiles. The norm, regardless of the indicators (PAPP-A, AFP, E3, hCG), MoM ranges from 0.5 to 2.5. For example, the analysis showed a beta-hCG value at week 7 of 60,000 mU/ml, the median of this period was 70,000 (the median can be viewed in the hCG table). HCG MoM = 60000/70000 = 0.85, which is not outside the normal range. An hCG calculator will help you calculate the result correctly.
Discharge before hCG test: menstruation or implantation bleeding
After fertilization, many women notice a characteristic pink discharge. As a rule, this terrifies many girls. In fact, such discharge can be associated not only with menstruation, but also be implantation bleeding.
According to statistics, 30% of pregnant women experience implantation bleeding. It is very different from menstruation. First of all, the difference lies in the nature of the discharge. During menstruation, the blood is thick, red and profuse.
Every day it becomes more and more. Implantation bleeding begins a few days before your main period and can last only a few hours. In rare cases, discharge lasts for several days.
Implantation bleeding is considered one of the first signs of pregnancy. As a rule, the girl does not yet know about her condition and thinks that fertilization has failed. In fact, after a few days, a woman may notice other characteristic signs of pregnancy.
Table of hCG norms by day.
It is extremely important for a woman to keep a special calendar in which to mark the beginning and end of her period every month. Later, with its help, you can understand that the girl is not menstruating, but is experiencing characteristic implantation bleeding.
Deviations from the norm
A pregnant woman after IVF is under constant supervision of a leading doctor; it is better if he interprets the results in order to prescribe a correction if necessary. But with the help of an online service, a woman can navigate the situation.
A low hCG level or its slow rise may indicate the following conditions:
- pregnancy fading;
- possible miscarriage;
- ectopic pregnancy;
- incorrect determination of gestational age.
An increase in hCG levels may indicate the following conditions:
- multiple pregnancy;
- anomalies of embryogenesis;
- late toxicosis;
- taking medications containing gonadotropin;
- gestational diabetes;
- incorrect source data.
If you are monitoring the hormone concentration at home using an online calculator that shows low or high values of human chorionic gonadotropin, contact your doctor immediately!
How is a human chorionic gonadotropin test taken?
For the analysis, blood from a vein is needed in the morning on an empty stomach. Measurement of beta-hCG concentration is performed no earlier than 3-5 days after a missed period. When taking hormones, you need to inform your doctor about this - they can affect the concentration of hCG.
To diagnose congenital pathologies (perinatal screening), an hCG test is performed at 14-18 weeks. Determination of hCG in men and non-pregnant women (analysis for tumor markers) can be carried out on any day.
Laboratory standards and user results
HCG standards may vary in different laboratories. This is due to the use of various research techniques, reagents and other factors. Therefore, to correctly assess the dynamics of hormone growth, it is necessary to conduct research in one laboratory and evaluate the results relative to the standards of this laboratory. The hCG calculator allows you to evaluate your results relative to the standards of different laboratories:
- HCG standards in the INVITRO laboratory
- HCG standards in the GEMOTEST laboratory
- HCG standards in the BIOTEC laboratory
- HCG standards in the CMD laboratory
The results of other users on the graph may also differ (depending on laboratory standards) and contain errors (for example, data was entered incorrectly).
- HCG norms in the INVITRO laboratory after IVF
- HCG norms in the GEMOTEST laboratory after IVF
- HCG norms in the BIOTEC laboratory after IVF
- HCG norms in the CMD laboratory after IVF
- HCG norms in the INVITRO laboratory for twins
- HCG norms in the GEMOTEST laboratory for twins
- HCG norms in the BIOTEC laboratory for twins
- HCG norms in the CMD laboratory for twins