Infections that pose a particular threat to the human embryo have, in all likelihood, been present for many centuries, but no one knew about them and the appearance of abnormalities in intrauterine development was considered “God’s punishment for human sins.”
The term “TORCH”, like many others in the medical lexicon, appeared only at the end of the 20th century. Nowadays, testing for TORCH infections is considered mandatory during pregnancy. And it’s even better to do it when planning a new addition to the family, because treating a pregnant woman is much more difficult than preparing for this important event. The TORCH complex includes the most significant diseases from the group of intrauterine infections (intrauterine infections), including a number of STIs (sexually transmitted infections).
What does TORCH mean?
TORCH is not just one disease, it is several diseases that occur in a latent form in a woman during pregnancy and pose a serious threat not only to the patient, but also to the fetus in the process of antenatal (intrauterine) development . Of particular danger are infections that are present before the 12-week period, that is, in the first trimester, when the main organs and systems of the new organism are formed. TORCH infections in children born from infected mothers can manifest as various deformities immediately after birth or have long-term consequences in the form of delayed mental and physical development.
A number of infectious agents, combined into one group, are classified by gynecologists as pathogens that pose a serious danger to a woman’s health and the normal development of her child. To get rid of the need to repeatedly list all these pathogenic microorganisms, doctors came up with an easy-to-remember abbreviation, the decoding of which explains the meaning of each specific letter:
Before and during pregnancy, it is advisable to avoid contact with pets due to the risk of toxoplasmosis.
T – Toxoplasma gondii. Toxoplasma opens the list of TORCH infections; it itself belongs to the causative agents of parasitic diseases, since it is an intracellular parasite. The danger to humans is posed by infected pets (cats, dogs, guinea pigs, rabbits), as well as predators, rodents, herbivores that live outside a person’s home, but run in and leave traces of their presence (feces);
O – group of infections, including pathogens:
- sexually transmitted diseases – syphilis, gonorrhea;
- viral infections - HIV, varicella zoster viruses, hepatitis B and C, Epstein-Barr, associated with a wide range of diseases, as well as parvovirus B19, which can be transmitted vertically;
- other infectious processes caused by representatives of various classes of microorganisms - chlamydia, myco- and ureaplasma, etc.;
R – Rubella, which means rubella. It is caused by a highly contagious airborne virus. Rubella contracted in childhood is considered harmless and provides lasting immunity. It is more difficult for women who were not vaccinated as children or were not “lucky enough” to get sick. The encounter of such a pregnant woman with rubella is fatal and is grounds for termination of pregnancy for medical reasons;
C – CMV (CMV). Cytomegalovirus infection (CMVI) can be silently present in the body and not manifest itself with any symptoms. In the case of primary infection during pregnancy, the issue of terminating it is decided;
H – HSV (Herpes simplex virus) – two types of herpes simplex virus. For the genital herpes virus, the placenta is not a particular obstacle, so there is a fairly high risk of infection of the fetus, both during embryonic development and during childbirth.
A list of microorganisms encrypted in this way that cause intrauterine damage to the fetus and pose a threat to the health of the expectant mother is called the TORCH complex, which is considered mandatory when registering for pregnancy and recommended if a woman is just planning a pregnancy.
Read more about 6 dangerous infections
Rubella. When infected in the first trimester, almost 90% damage to the fetus. Rubella is a problem specific to Russia. Many women were sick in childhood - they are no longer afraid of infection. But it often occurs in a mild form and the disease goes unnoticed. The infection can be prevented by getting vaccinated - you just need to get tested! If there are no IgG and IgM antibodies, go for vaccination.
Toxoplasmosis is a less common infection; approximately 15% of women of reproductive age have had the disease, that is, 75% of women can become infected with toxoplasma during pregnancy! Prevention and treatment measures during pregnancy are very effective. It is important to know the exact status of the infection before pregnancy or at a very early stage. If there are no IgG and IgM antibodies, ask your doctor how to avoid getting toxoplasmosis during pregnancy and how to monitor antibody levels (once a month).
Herpes types 1 and 2 are especially dangerous during childbirth and after childbirth. In the absence of antibodies to herpes, in addition to preventing infection during pregnancy, close attention to the baby after birth is necessary.
Cytomegalovirus is transmitted by airborne droplets; most women of reproductive age have already encountered the virus (up to 90%). 10% of women do not have antibodies, which means there is a risk of contracting CMV, and the probability of infection of the fetus is 30%! If there are no antibodies, be sure to ask your doctor how to avoid getting infected and how to monitor antibody levels. It is especially dangerous in the autumn-winter period!
Parvovirus B19 – increased risk of infection in the autumn-winter period. There may be an asymptomatic or minimally symptomatic course, so before pregnancy it is important to test for antibodies to parvovirus B19. If there are no antibodies, monitor antibodies monthly during pregnancy.
Basic methods for detecting TORCH infections
The priority right when conducting research on the presence of specific antibodies in human serum to pathogens of TORCH infections belongs to the enzyme-linked immunosorbent assay (ELISA), which is considered the cheapest and most accessible.
Polymerase chain reaction (PCR), also used for similar purposes, detects not antibodies, but the DNA or RNA of the virus itself in biological fluids (blood, urine, discharge from the genital tract), and in the most insignificant concentration, therefore it is especially good for identifying carriage ( asymptomatic). However, the cost of PCR diagnostics is higher, and not every laboratory has the equipment. Meanwhile, it should be noted that the combined use of ELISA and PCR significantly increases efficiency , making it possible to determine not only the presence of the virus, but also its type. Often, in addition to or as an independent study, which is also better done with PCR, the direct immunofluorescence (DIF) technique is used, which is also considered a highly informative study.
Direct methods for identifying TORCH pathogens include bacteriological culture on a nutrient medium (for example, gonococcus requires exactly this approach) and cytological diagnosis, however, the latter still cannot be considered reliable, since it only finds indirect signs of infection (gonorrhea, chlamydia, herpetic infection) , which require confirmation by other methods (ELISA, PCR, bacterial culture).
How is the TORCH complex deciphered?
The TORCH complex received its name based on the names of infections.
- To – toxoplasmosis;
- R – rubella;
- C – cytomegalovirus;
- H – herpes.
The herpes virus includes several types. In preparation for pregnancy, a woman is tested for herpes simplex types I and II.
This is important to know. Chlamydia is not considered a TORCH infection, despite the generally accepted opinion. The doctor must prescribe a test for them, as well as for other infections that can cause intrauterine infection of a child, separately. Often these infections are referred to as the letter O in the abbreviation TORCH, since “other” is translated from English as others. This letter includes hepatitis, listeriosis, syphilis, HIV, enterovirus and chickenpox.
All these viruses and bacteria attack the bodies of many people, but the term TORCH is applied only to pregnant women and their babies. A group of these infections causes congenital anomalies of the fetus, and can cause fetal death and the birth of a stillborn baby. TORCH infections provoke minor pain in expectant mothers and can even go unnoticed. However, in this case, the fetus becomes infected, which leads to serious complications, especially if the infection began in the first trimester of pregnancy. During this period, all systems and organs of the child are formed, and the impact of pathogenic factors on them is very noticeable.
If there is a need for examination
Nowadays it is absolutely easy to get tested for the TORCH complex. When planning a pregnancy, you can contact your antenatal clinic, where the gynecologist will certainly guide the patient in the right direction. By the way, there is no need to disturb the husband or the alleged biological father, since he is not subject to such an examination. When planning a pregnancy, you should keep in mind that the analysis may be paid and its cost, depending on many factors, including the region, the status of the clinic, the characteristics of test systems and methods, can range from 1.5 to 6.5 thousand (average price 2000 – 4000) . Of course, residents of Moscow and St. Petersburg will pay the highest price, but the periphery will benefit in this situation.
Pregnant women have their own special rules. In most cases , women registered at the antenatal clinic are subject to a free examination or on preferential terms, when the price of the analysis is 3 times cheaper.
You can get tested for TORCH, except for the antenatal clinic, where the test is mandatory, in any clinic or medical center that has an ELISA laboratory equipped with special equipment and test kits. It should be noted that the analysis is quite labor-intensive, carried out in two stages and often on a semi-automatic analyzer, which only involves automatic reading of the results, while the rest of the process is performed manually. Of course, it is clear that the “automatic machine” available in the laboratory will take over almost all the functions.
In addition, patients are often outraged by the fact that they are told to come back in two weeks, or even a month, for an answer. This means that to use the test system, a certain number of serum samples is required, since spending a whole kit on 1-2 people will be very impractical and expensive. In this regard, it is better for pregnant women to get tested in specialized institutions that conduct a lot of research and do not delay receiving results.
To carry out the analysis using the enzyme immunoassay method, blood is taken from the patient’s vein, the serum is separated, which is used for work. Blood, as with all biochemical studies, is donated on an empty stomach, usually in the morning, so it is assumed that the person will be hungry for at least 8 hours. Antibiotic therapy should be excluded 3-4 weeks before the test , otherwise false negative results may be obtained.
When carrying out PCR on other biological media (urine, secretions from the genital tract), the range of rules significantly expands. To obtain reliable results, the person being tested is offered:
- Avoid sexual intercourse the day before the examination;
- Do not urinate 2 hours before receiving the material:
- Do not use intimate hygiene products, douche;
- Take the test immediately after your period (if planning pregnancy).
The doctor, as a rule, informs the patient about all the nuances or gives a specially designed reminder so that the person does not forget anything.
Rubella
This is an infectious disease of a viral nature, which is transmitted by airborne droplets from sick people to healthy people. Rubella is considered a harmless childhood disease that does not cause any particular complications.
The disease manifests itself as a pink rash and an increase in temperature. In this case, the patient feels satisfactory. People only get sick with rubella once, because after the infection immunity is developed.
However, when carrying a baby, rubella turns into a rather dangerous infection, since it leads to damage to the baby’s heart, as well as the tissues of the nervous system and eyes.
If the expectant mother becomes infected with rubella in the first trimester of expecting a baby, the pregnancy is often terminated. If the infection is detected in the second or third trimester, the baby may have growth retardation and developmental delays.
This is interesting. If rubella occurs in a woman in the last month of pregnancy, the baby may be born with a rash on the body. His rubella course is the same as in babies who become infected after birth.
To protect yourself from rubella, it is necessary to get a preventive vaccination before conceiving a baby, especially if the woman has not had this disease before.
How to understand the results?
Considering that ELISA is the most popular method for identifying TORCH, readers may be interested to know what the unfamiliar Latin symbols and numbers in the answers mean. Of course, a positive and negative result is always clear, but how to interpret it, whether it is good or bad, whether you should still be afraid of the disease or whether it already exists , only its course is hidden, what does the designation IgG or IgM mean and much more.
Example of test results for the TORCH complex with detected toxoplasmosis
Antibodies produced against a foreign antigen at some stage of the disease are called immunoglobulins and are designated Ig. Depending on the period of the disease when antibodies appear, they are classified into different classes: A, E, M, G, D, etc. In the case of TORCH infections, the appearance of immunoglobulins of classes M and G (IgM, IgG) is considered.
Class M immunoglobulins are produced in the early stages of the infectious process, and class G immunoglobulins appear later and indicate a state of remission or the presence of immunity. In addition, when testing serum for these pathogens, the antibody titer and avidity index are often indicated. However, it should be noted that full interpretation of the results is allowed only to the doctor, so we will focus only on positive and negative responses in immunoglobulin studies.
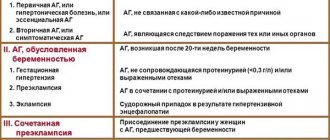
Indicators of TORCH infections – immunoglobulins of classes M and G
Tests for identifying the causative agent of a particular infectious process are based on determining the level of antibody titers to the antigen of this pathogen:
- Class M immunoglobulins, which appear in the acute period of the disease;
- Immunoglobulins class G, indicating remission or the presence of immunity.
For cytomegalovirus, toxoplasmosis, rubella virus, and herpes infection, test results may look like this:
The absence of IgM and IgG indicates that although there is no infection, there is no immunity, therefore during pregnancy measures to prevent these diseases should be strengthened:
- Toxoplasmosis – communicate less with cats and dogs, wash vegetables and fruits thoroughly, do not eat meat products that have not been thermally processed;
- Rubella - a negative result indicates a lack of immunity, therefore, when planning, vaccination is possible, then control of IgM and IgG after 2 - 2.5 months (not earlier). During pregnancy - a risk group, control of immunoglobulins of both classes every month in case of contact with a sick child;
- Cytomegalovirus infection – there were no encounters with infection. During pregnancy - a risk group. Monitor Ig of both classes every month. Prevention measures: vitamins, microelements;
- Herpes – there were no encounters with infection. During pregnancy - a risk group. Monitor Ig of both classes every month. Strengthening the body's defenses, vitamin therapy;
IgM – positive result, IgG – negative – a sign of recent infection:
- Toxoplasmosis, rubella - the results correspond to the initial phase of an acute infection or a false-positive reaction, so one way or another, the analysis should be repeated after a couple of weeks;
- Herpes, CMV - possible manifestations of primary infection. Repeated control after 2 weeks. When planning pregnancy, general restorative therapy is recommended; if pregnancy is present, consultation with an infectious disease specialist. Tactics are determined by the doctor monitoring the pregnant woman, who, depending on the period, chooses treatment;
IgM – negative, IgG – positive, this result means:
- Toxoplasmosis – infection occurred more than a year ago, immunity currently exists, so there is no threat to the child’s health;
- Rubella - a similar result may indicate the presence of immunity and, accordingly, the absence of a threat to the fetus, if the IgG level is > 10 IU/ml. However, in the case of low IgG levels (< 10 IU/ml) when planning pregnancy, revaccination with monitoring of immunoglobulin levels is recommended after 2 - 2.5 months;
- Herpes, CMV - indicators indicate remission of the disease, therefore constant monitoring of changes in AT titer is necessary;
IgM and IgG are present in the patient’s blood in sufficient concentrations :
- Toxoplasmosis is possibly the development of an acute infection or the presence of “delayed” IgM, therefore, to clarify, repeat monitoring of immunoglobulins of both classes after 14-15 days. If there is pregnancy, consult an infectious disease specialist, monitor the level of immunoglobulins of both classes after 14-15 days, conduct additional tests for avidity of class G antibodies;
- Rubella - the result may correspond to the acute phase of the infectious process. A consultation with an infectious disease specialist and re-examination after 2 weeks are indicated;
- Herpes, CMV – reinfection or development of acute infection is possible. To clarify the duration of the process, repeat analysis after 14 days (rubella) and an additional test for avidity of class G immunoglobulins (CMVI). During pregnancy, tactics are determined by the gynecologist observing the woman, depending on the clinical picture and laboratory diagnostic data.
table: TORCH test results and possible diagnoses
Examination during pregnancy
| IgG | IgM | |
| Discovered | Not detected | If the test is taken in the very early stages of pregnancy, the body’s encounter with this pathogen has already taken place, and this pathogen does not pose a serious danger to the unborn child. If the test is not taken at the earliest stages, the presence of IgG may be associated with a recent infection, already during pregnancy. In this case, additional examination methods are recommended (see IgG avidity below). |
| Not detected | Not detected | Exposure to this infection during pregnancy can pose a threat to the unborn child. The analysis should be repeated once a month. |
| Discovered | Discovered | The presence of IgG and IgM may be associated with a recent infection, already during pregnancy. But it also does not exclude infection before pregnancy. In this case, additional examination methods are recommended (see below: avidity, immunoblot). |
| Not detected | Discovered | The presence of IgM may be associated with a recent infection, as early as during pregnancy. But it also does not exclude reactivation of the infection, which is not dangerous during pregnancy. In this case, additional examination methods are recommended (see immunoblot below). |
In CIR clinics:
after receiving test results, you can consult with an experienced specialist and draw up an action plan!
Treatment of TORCH infection
Treatment of TORCH infections directly depends on whether the woman is currently planning a pregnancy or is already in an “interesting situation.” In addition, the primary task is to identify the pathogen, because each infection requires its own, individual approach.
Treatment of a pregnant woman is fraught with certain difficulties, since many drugs that have proven themselves remarkably effective in the fight against infections can simply have a detrimental effect on the developing fetus. That is why it is recommended that all therapeutic measures be carried out before pregnancy , that is, while planning it. However, anything can happen in life, so infected pregnant women periodically appear. In such cases, the attending physician prescribes the necessary examinations, consultation with an infectious disease specialist, and in treatment proceeds from the position of the least risk with the addition of targeted medications, immunomodulators and restorative vitamin complexes.
Signs in a newborn that may indicate a TORCH infection:
Any of the above signs may be a cause for concern, so if there is minimal suspicion, it is recommended to consult a doctor immediately.
Why is the examination carried out?
It is before pregnancy (or in the early stages) that we need to find out whether there was an infection or not. If there was, you don’t have to worry, this infection is not dangerous for a pregnant woman. If not, then the doctor will tell you about a set of preventive measures (for example, if we are talking about rubella, then you can get vaccinated, if we are talking about toxoplasma, you can follow certain rules to reduce the risk of infection, etc.). In addition, for those infections for which there are no protective antibodies, it is important to conduct regular monitoring so as not to miss an infection during pregnancy.
What is the danger
The fact is that if the mother’s body has not previously been infected with a torch infection, which is the danger, then it has not developed immunity. And during primary infection, many microbes begin to circulate in the blood and can penetrate the child’s body, disrupting its development.
The important thing is that the symptoms of the disease may not be expressed or may be insignificant. Thus, even without suspecting an infection, a woman will not be able to recover in time. And the infection at this time will negatively affect the pregnancy and the condition of the fetus.
An encounter with any of these infections can have a detrimental effect on the fetus. The virus is capable of infecting all systems of a small organism, and especially its central nervous system. Therefore, the detection of Torch infections is very often an indication for artificial termination of pregnancy. Otherwise, there is a risk of giving birth to a defective or dead child, and the child may also have developmental defects and even disabilities.
In this situation, it is the primary infection with the virus that is very dangerous, since the woman’s body does not have immunity to it and will not be able to cope with the disease. A secondary encounter with the virus is not so dangerous, for the reason that the body has already produced antibodies to it before and has a developed immunity.
Cytomegalovirus (video)
This disease was discovered only in the twentieth century. It is transmitted sexually, through blood, during breastfeeding. The effect of CMV on the human body depends on the state of its immune system. If it is weakened, the cytomegalovirus “wakes up” and begins to attack many systems and organs. Antibodies to this disease are formed immediately after recovery, so re-infection does not occur.
During pregnancy, CMV causes enormous harm to the fetus. Infection of the baby can occur not only from the mother herself - through the placenta and membranes, but even from the father at the time of conception, since this virus can also be contained in sperm. In addition, infection is also possible during labor. Intrauterine infection can lead to the fact that the fetus may not survive or the baby will be born with this disease. In this case, he may experience hepatitis, pneumonia, congenital deformities, hydrocele, heart defects, and jaundice. In addition, the baby may be diagnosed with deafness, muscle weakness, epilepsy, and mental retardation. That is why this disease is an indicator for artificial abortion.