Throughout pregnancy, changes constantly occur in the female body. To determine whether everything is normal, doctors prescribe various tests. They determine not only the health of the baby or his mother, but also possible pathologies that can be prevented at an early stage.
One of the most important tests of this type is the determination of hemostasis or blood clotting. A hemostasiogram during pregnancy is a mandatory planned study, but sometimes it is prescribed unplanned. What is this analysis? How is it carried out? What diseases can be detected with its help? You will find detailed answers to these and other questions in the article.
What is hemostasis
Hemostasis is the name given to the blood clotting system. Everything in the body is interconnected and aimed at protecting it. Thanks to this system, the blood is constantly in a liquid state, and when the walls of blood vessels are damaged, blood clots form, stopping the bleeding. After performing their function and healing the wound, the blood clots dissolve. This is how protection against blood loss occurs.
In order for the mechanism to work properly, you need to monitor its condition. Women are subject to special observation when planning pregnancy and during the period of bearing a baby. For this purpose, the doctor refers the woman to a hemostasiogram or, as it is also called, a coagulogram. This is a comprehensive analysis that allows you to detect any abnormalities in the coagulation system.
A hemostasiogram is a combination of several indicators that allow the doctor to judge the normal functioning of the coagulation system.
The coagulation system is divided into three parts:
- Coagulant - preventing bleeding, thickens the blood in the damaged vessel (coagulation).
- Anticoagulant - responsible for maintaining blood in a liquid state.
- Fibrinolytic - destroys formed blood clots.
All these systems must be in balance in order to protect the body from blood loss during injury and not cause blockage of blood vessels.
With low rates of hemostasis, even a small wound leads to heavy bleeding. And high levels are dangerous due to increased thrombus formation in the blood vessels, which is fraught with complications for the woman and child.
What are the consequences of impaired hemostasis - watch the video:
What is a hemostasiogram
Hemostasiogram - what kind of study is this? A blood test determines the indicators responsible for the blood clotting process - platelets, plasma proteins. The collection of these cells and proteins is called the hemostatic system. This is a complex process that takes place in several stages.
Hemostasis is needed to maintain the fluid state of the blood. In trauma, hemostasis is altered to stop bleeding by forming a blood clot. Damage to blood vessels and bleeding triggers the coagulation cascade. It includes several stages:
- platelet adhesion and plug formation at the site of injury - primary hemostasis;
- activation of plasma proteins and formation of fibrin - coagulation hemostasis, secondary;
- saturation of the platelet plug with fibrin and the formation of a blood clot that clogs the damaged vessel wall.
If blood clots form in the body for no reason, the process of their destruction is activated - fibrinolysis. Anticoagulants that dissolve fibrin are involved in this.
Hemostasis changes depending on internal processes in the body and environmental factors. It is influenced by:
- age and gender;
- nutritional features;
- presence of bad habits;
- taking medications;
- chronic diseases;
- injuries;
- pregnancy.
Hemostasiogram analysis is needed for patients with chronic cardiovascular diseases, liver cirrhosis, and oncology. It is performed on pregnant women in preparation for surgery, to monitor treatment with anticoagulants.
What are the consequences of impaired hemostasis during pregnancy?
During the period of bearing a child, a disturbance in the coagulation system is fraught with such undesirable consequences as placental abruption or heavy bleeding at the time of birth if there is a low level of hemostasis.
And the predominance of the coagulation link carries the risk of blood clots in the placental vascular system, which can lead to pathologies such as:
- fetal hypoxia;
- anemia of the mother or child;
- premature aging of the placenta;
- fetal freezing;
- gestosis and so on.
Blockage of the placental vessels also leads to insufficient supply of nutrients to the baby, which can affect its development and lead to new complications. Therefore, pregnant women are required to undergo a hemostasiogram.
If violations are identified, it is necessary to undergo a course of therapy to stabilize hemostasis. Sometimes the patient even needs a blood transfusion to save her or the baby.
Description and characteristics of the study
A hemostasiogram or coagulogram is a category of clinical research that gives an idea of the state of a woman’s coagulation and anticoagulation systems. If the hemostasiogram readings during pregnancy are too low, then any, even the smallest scratch on the pregnant woman’s body can turn into heavy bleeding. Excessive hemostasis, on the contrary, leads to the formation of blood clots and, as a consequence, to heart attacks and strokes.
The complex hemostasis system in the human body performs two functions:
- maintains blood in liquid form inside the vessels;
- immediately responds to capillary damage, forms blood clots to stop bleeding.
The process of blood clotting involves vascular walls, blood cells and plasma proteins. Plasma hemostasis involves the systems of coagulation, anticoagulation (anticoagulation) and blood clot dissolution. The coagulation indicator is a cascade process leading to the formation of a special protein located at the heart of the blood clot. Violation of this natural process leads to the following consequences:
- decreased blood clotting (bleeding that is difficult to stop);
- increased coagulability (appearance of thrombosis);
- thrombophilia (appearance of blood clots).
A hemostasiogram helps to understand the state of a person’s coagulation system. It not only shows the content of blood cellular elements, but also certain indicators of a general blood test. Thanks to this, you can see the entire clinical picture, as well as correctly interpret various deviations in the analysis.
Disturbances in the blood coagulation system during pregnancy are a regular and quite dangerous phenomenon, since they lead to the following consequences:
- activation of the coagulation unit, as a result of which the likelihood of blood clots in the vessels of the placenta increases;
- the predominance of the anticoagulant system, which increases the likelihood of placental abruption and postpartum hemorrhage.
The need for a hemostasiogram during pregnancy is that it reflects fibrinogen levels. This is a protein that is one of the blood clotting factors. At high concentrations, increased blood clotting is observed, at low concentrations, the opposite is true. To stabilize this indicator, a blood transfusion is given. An important mark in the hemostasiogram graph is the number of prothrombin protein. If its index is less than 80%, then there is a high risk of bleeding, which is difficult to stop. At 100%, the use of direct or indirect anticoagulants is prescribed.
According to gynecologists, taking a hemostasiogram analysis during pregnancy is simply necessary, since this study allows doctors to constantly monitor blood coagulation processes in order to avoid unpleasant consequences and large blood losses during the birth process. A hemostasiogram in this case is an indicator of the health status of a pregnant woman.
When is a hemostasiogram prescribed?
A hemostasiogram is definitely prescribed when planning a pregnancy, especially if the woman has a history of problems such as:
- Freezing of the fetus.
- Pathologies during pregnancy.
- Miscarriage.
- Disorders in the cardiovascular system.
- Anemia.
In the normal course of pregnancy, testing for hemostasis is routine, and it is taken three times during the entire period:
- 1st trimester – upon registration, up to 12 weeks of pregnancy;
- 2nd trimester – at 22–24 weeks;
- 3rd trimester – at 30–36 weeks.
If health problems occur in a woman or fetus, a coagulogram is prescribed more often.
This test is also often performed on pregnant women who are at risk or have the following problems:
- Liver diseases.
- Nosebleeds.
- Long-term infertility.
- IVF pregnancy.
- Multiple births.
- The presence of autoimmune pathologies.
- History of frozen pregnancy.
- Past clotting problems.
- Uterine hypertonicity.
- The presence of signs of gestosis - swelling of the arms and legs, high blood pressure, protein in the urine.
- Close relatives have diseases - varicose veins, heart attack, stroke, thrombosis.
- The woman has led or is leading an unhealthy lifestyle.
Indications for examination
Leading gynecologists have not yet come to a consensus when it is necessary to prescribe a blood test for a hemostasiogram. There are two opposing points of view:
- A hemostasiogram is prescribed to all pregnant women without exception. A blood test serves as a screening to identify possible pathologies.
- A hemostasiogram is indicated only if there are risk factors.
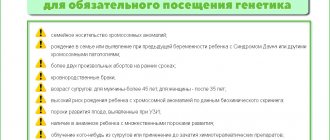
In the first case, the gynecologist prescribes a test at the first registration. In the second situation - if there is evidence:
- A burdened obstetric history - termination of pregnancy at any stage, regressing pregnancy, antenatal fetal death, stillbirth. Such conditions may be associated with pathology of the blood coagulation system.
- Maternal diseases with a high risk of thrombosis. A hemostasiogram is indicated for heart valve defects, varicose veins of the lower extremities, vascular pathology of the brain, hypertension, etc.
- Complications of real pregnancy. A hemostasiogram is prescribed for gestosis, placental insufficiency and disruption of uteroplacental blood flow, and delayed fetal development. If there is a threat of interruption and bleeding at any time, this analysis is also indicated.
- Hereditary pathology of the hemostatic system. If there are such cases in the family, you need to get tested.
Indications for examination are determined by the gynecologist after examining and interviewing the patient.
What will such an examination tell you?
Now let’s look at why you need to undergo a hemostasiogram and what consequences it can prevent.
A coagulogram most accurately provides the doctor with information about the patient’s health, which is related to the coagulation system.
There are several main research parameters by which the state of hemostasis is determined:
- APTT – activated partial thromboplastic time. This parameter shows the time required for blood clotting. If it is less than normal, it means that coagulation occurs too quickly, which threatens DIC syndrome. Inflated values indicate poor clotting, which means there is a risk of bleeding after childbirth.
- Prothrombin (or factor II) - indicates the quality of coagulation, determined as a percentage. Normally, the results of the prothrombin index are considered to be from 78 to 142%. Numbers less or more than normal indicate decreased or increased coagulation.
- Fibrinogen is a blood clotting protein. Its high concentration indicates increased coagulability. If the results are significantly abnormal, the patient is prescribed a blood transfusion to stabilize fibrinogen.
- Antithrombin III is the name of a protein that inhibits clotting. That is, it keeps the blood in a liquid state. If its levels are high, this can lead to bleeding after childbirth. A low reading indicates a risk of blood clots.
- Thrombin time (TT) - indicates the time of the final stage of coagulation. As with APTT parameters, a deviation from the norm towards a decrease leads to DIC syndrome. Exceeding the readings warns of possible bleeding.
- D-dimeter is one of the most important parameters indicating the thickness and viscosity of blood. If its level exceeds the average permissible norm, there is a tendency to form blood clots in the vessels.
- SFMC (soluble fibrin-monomer complexes) - indicates intravascular coagulation. If its parameters are too high, this indicates DIC syndrome.
- Lupus anticoagulants are certain antibodies responsible for clotting. Normally they should be absent. If this indicator is present, there is a risk of autoimmune diseases, AIDS, lupus erythematosus and other pathologies associated with a lack of blood supply due to thrombosis.
These parameters are considered basic in the standard hemostasiogram procedure. The extended study includes more meanings.
Thromboelastogram in some laboratories is included in the main analysis. This definition has slightly different interpretations and is carried out using a special device - a thromboelastograph.
Interpretation of hemostasiogram indicators
The hematologist interprets the hemostasiogram parameters. Blood hemostasis is maintained by platelets and plasma proteins. Platelets are responsible for platelet hemostasis, proteins are responsible for plasma hemostasis. Both of these processes occur simultaneously, and if one or both are disrupted, a person has a tendency to bleed or develop blood clots.
A standard hemostasiogram includes:
- platelets;
- INR;
- fibrinogen;
- plasminogen;
- thrombin time;
- APTT.
Platelets are platelets of blood produced in the bone marrow. Their function is to detect damage to blood vessels and close them by forming a blood clot. The normal platelet count is 180-360*109/liter. Reduced risk of bleeding. Increased risk of blood clots.
Plasminogen is a protein produced in the liver. Responsible for the last stage of hemostasis - dissolution of the blood clot. Normally it is 80-120%. An increase is observed during pregnancy. Decreased in DIC syndrome and hereditary diseases.
APTT —activated thrombin time. This is the time during which a clot forms in a test tube with blood and an added calcium chloride solution. Normally it is 25.4-36.9 seconds. Increases with insufficient coagulation. Decreases in DIC syndrome.
INR , or prothrombin, is an indicator indicating the onset of blood clot formation. The norm is 0.8-1.15. An increase is observed in hereditary blood clotting disorders, DIC syndrome. A decrease indicates an increased risk of thrombosis.
Thrombin time is an indicator of the final stage of thrombus formation. This is the time during which fibrinogen is converted into fibrin. The norm is 14-20 seconds. Lengthening the time indicates a risk of bleeding, and shortening it indicates the risk of thrombosis.
Fibrinogen - fibrin is formed from it, which secures the blood clot. The content norm is 2-4 g/liter. The level of fibrinogen increases during pregnancy, long-term use of hormonal contraceptives, hypothyroidism, and acute infections. Accompanied by a high risk of thrombosis. A decrease in fibrinogen is observed in DIC syndrome, liver diseases, and is accompanied by the risk of bleeding.
Tests for mutations in hemostasis genes include:
- G2021OA - responsible for prothrombin proteins, the mutation is accompanied by a high risk of thrombosis and miscarriage;
- G1691A - responsible for coagulation factor 5, the mutation leads to intrauterine fetal death;
- FGB G455A - responsible for fibrinogen, the mutation leads to the development of thrombophlebitis;
- PAI-1 4G/5G - responsible for plasminogen, the mutation is accompanied by the risk of placental abruption and miscarriage.
Those who have a family history of coagulation disorders should be tested for polymorphism. The analysis is also recommended if no abnormalities were found during routine studies, but there are symptoms of coagulation disorders.
Polymorphism options:
- homozygous - a gene mutation was passed on from both parents, a more dangerous option;
- heterozygous - the mutation was passed on from one parent, less dangerous.
Only a geneticist can correctly decipher the result.
Advanced blood test for hemostasis
The extended hemostasiogram includes additional criteria:
- study of platelet aggregation function;
- D-dimers;
- proteins C and S;
- antithrombin.
An extended hemostasiogram provides more information about the coagulation system. It is prescribed for diagnostic difficulties, as well as for pregnant women.
D-dimer is the part of fibrin that appears when it breaks down. Therefore, the amount of D-dimer can be used to judge the presence of blood clots in the vessels. The norm is less than 286 ng/ml. An increase in D-dimer is observed in DIC syndrome, deep vein thrombosis, pulmonary embolism, infectious and oncological diseases, after injuries and operations.
Antithrombin is a plasma anticoagulant protein. Prevents thrombus formation. The normal amount is 80-125%. An increase in the indicator is a sign of increased bleeding. Decreased – high risk of thrombosis.
Protein C inhibits blood clotting. The norm is 70-140%. Its activity is enhanced by protein S. The amount decreases in genetic disorders and liver diseases. Accompanied by a high risk of thrombosis.
Preparation for a hemostasiogram
Before taking a hemostasis test, you must follow certain rules for more accurate indicators:
- a few days before the hemostasiogram, you should not drink tea, coffee and carbonated chemical drinks. Alcoholic drinks and smoking are strictly prohibited;
- 5–7 days before the test, you should stop taking medications that affect clotting. If it is impossible to cancel the appointment, then be sure to notify the specialist from the laboratory;
- take the test in the morning, on an empty stomach;
- in the evening, on the eve of going to the laboratory, you should have dinner with easily digestible low-fat foods;
- Before taking the test, it is recommended to drink one glass of water.
The reliability of the results is also influenced by the woman’s emotional state. Therefore, a couple of days before the coagulogram you should not be nervous. If there have been stressful situations, you need to calm down before going to the laboratory.
Indications for the procedure
Indications for re-analysis are the following circumstances:
- liver and kidney diseases;
- decreased elasticity of veins;
- autoimmune imbalance;
- pathologies in the functioning of the cardiovascular, endocrine, and genitourinary systems;
- abnormalities in previous hemostasiogram results;
- inability to conceive a child;
- miscarriage that occurs repeatedly;
- smoking abuse;
- late gestosis or intrauterine growth retardation;
- phytoplacental insufficiency;
- previous in vitro fertilization procedure;
- multiple pregnancy;
- swelling;
- risk of miscarriage;
- frequent bleeding from the nose and gums.
You should also know that 7 days before going to the laboratory, it is not recommended to drink alcohol and drugs with aspirin, since these substances can further thin the blood. As a result, the results of the analysis may be incorrect.
During the entire period of bearing a child, a woman must donate blood for testing several times:
- immediately after conception occurred and the gynecologist registered the woman;
- around the 5th or 6th month of pregnancy;
- from the 8th to 9th months of the gestational period.
Sometimes, usually before giving birth and depending on the health of the pregnant woman, the doctor may recommend additional testing. This need increases if a woman is predisposed to varicose veins, liver problems, and various immune diseases.
Patients with a negative Rh factor are also at risk, since throughout pregnancy their immune system will try to reject their own antibodies and perceive them as foreign. Pregnant women with high blood clotting will also be sent for a repeat test.
How is the examination carried out?
The hemostasiogram procedure is, in fact, the same drawing of blood from a vein. If all the requirements for preparation for the analysis recommended by the doctor have been met, the indicators will be as reliable as possible.
The analysis is deciphered by a specialist, since the indicators are influenced by a lot of factors that he takes into account during the examination. For example, after a frozen pregnancy there will be some results, but in the first trimester - completely different. Some diseases, lack of vitamins, injuries and much more also affect the indicators.
Despite the fact that a hemostasiogram can be done in many laboratories, the price for it varies, ranging from 400 to 1300 rubles. This depends on the quality of the equipment and the availability of the necessary reagents for the analysis. A detailed coagulogram costs significantly more than a basic one. But for pregnant women, such examinations are often done free of charge.
Why is it important to do a coagulogram during pregnancy? Preparing for analysis
Determination of a coagulogram is a mandatory screening test during pregnancy. As a rule, it is carried out at least 3 times - one for each trimester. If there are risk factors for thrombus formation disorders or pathological changes in test results, the doctor may prescribe more frequent determination of hemostasiogram parameters.
Physiological changes in a woman’s body during pregnancy affect the coagulation and fibrinolysis system. The level of many blood clotting factors increases during pregnancy, and the activity of the anticoagulant and fibrinolytic systems decreases. Because of this, pregnant women experience a hypercoagulable state, which is an adaptive mechanism of the body aimed at reducing bleeding during and after childbirth.
Unfortunately, the other side of increased blood clotting is an increased risk of blood clots. Venous thromboembolism is one of the leading causes of mortality during pregnancy. Blood clots form especially often in the deep veins of the legs or pelvis.
The danger of their formation increases when:
- presence of blood clots in the past;
- hereditary predisposition to the formation of blood clots;
- obesity;
- prolonged immobility (for example, bed rest, traveling long distances);
- multiple births;
- increasing age of the pregnant woman;
- the presence of other diseases (for example, cancer, infectious processes).
The risk of blood clots during pregnancy dictates the need for careful monitoring of the hemostatic system in expectant mothers.
To determine hemostasiogram parameters, venous blood of the pregnant woman is required. Typically, the sample is collected in the morning. Before taking the test, a woman should not eat for 6-8 hours. No other special preparation is needed.
How to read a hemostasiogram - deciphering the results
The results of a coagulogram are not constant and vary depending on various factors. The doctor always takes this into account when interpreting the examination. At different periods of pregnancy, the average permissible norms will change.
The table shows the average normal values for the 1st, 2nd and 3rd trimesters of pregnancy and for women who are not pregnant. But the result is also influenced by other factors that the observing doctor should be aware of.
Indicator table:
| Study parameter name | Before pregnancy | I trimester | II trimester | III trimester |
| APTT | 26.3–39.4 sec. | 24.3–38.9 sec. | 24.2–38.1 sec. | 24.7–35.0 sec. |
| Prothrombin time (PTT) | 12.73–15.4 sec. | 9.7–13.5 sec. | 9.6–13.4 sec. | 9.5–12.9 sec. |
| Fibrinogen | 2.3–5.0 g/l | 2.4–5.1 g/l | 2.9–5.4 g/l | 3.7–6.2 g/l |
| Antithrombin III | 70–130% | 89–114% | 88–112% | 82–116% |
| D-diameter | 0.22–0.74 µg/ml | 0.05–0.95 µg/ml | 0.32–1.29 µg/ml | 0.13–1.7 µg/ml |
| Platelets | 165–415 x109/l | 174–391 x109/l | 155–409 x109/l | 146–429 x109/l |
| INR | 0.9–1.04 sec. | 0.89–1.05 sec. | 0.85–0.97 sec. | 0.80–0.94 sec. |
If there is a deviation from the indicators, the doctor prescribes treatment aimed at stabilizing a certain hemostasis parameter. In some cases, with severe abnormalities, the pregnant woman is given an urgent blood transfusion.
The advantage of this analysis is its availability and low cost. However, not a single research parameter provides a 100% determination of the cause of disturbances in the functioning of the coagulation system. In addition, it takes some time to decipher the parameters, but sometimes urgent diagnostics are required, which this research method cannot allow.
Hemostasiogram when planning pregnancy
It will never be superfluous to undergo this analysis at the stage of preparation for fertilization in order to promptly correct the results in case of deviations.
If you or your blood relatives have encountered venous problems: blockage or thrombosis, then do not be lazy and get tested to determine hemostasis. Keep your health under control, as ignoring this research can lead to problems such as:
- thrombophilia, when the risk of developing thrombosis during pregnancy is increased by 6 times;
- changes in placental blood flow. When the blood is too thick, the blood flow system of the maternal placenta is disrupted. As a result, the child does not receive enough nutrients. This is fraught with his death or developmental delay;
- pronounced gestosis in the second and third trimesters. Swelling appears and blood pressure rises.
Disturbances in the functioning of the hematopoietic system occur for various reasons, which is why it is so important to identify possible abnormalities even before the fertilized egg attaches to the walls of the uterus.
When planning a pregnancy, the following categories of women must undergo a hemostasiogram:
- if close relatives suffer from thrombosis, suffered strokes or heart attacks;
- in the female line there are problems with the elasticity of the veins;
- after the fading of a previous pregnancy or abortion;
- with various problems of the circulatory system.
The results of a hemostasiogram and their correct interpretation allow timely detection and treatment of all abnormalities before and during pregnancy. An important point in this regard is the use of safe drugs, which significantly increase the chances of successful pregnancy and birth of a full-fledged child.
Prevention of violations
For the health of the baby and his mother, gynecologists recommend:
- Eat right - eat more vegetables, fruits and other foods rich in vitamins and microelements, drink more water.
- Eliminate bad habits - alcohol, smoking, coffee.
- Walk more in the fresh air and do special exercises for pregnant women.
- Follow all doctor's recommendations and undergo examination on time.
All this in most cases helps prevent the occurrence of disorders in the circulatory system. However, pregnancy is a very delicate process associated with changes in the functioning of the entire female body. Therefore, there are not isolated cases of hemostasis problems. If violations are detected, the doctor prescribes treatment in accordance with the diagnosed causes.
Medicines to normalize hemostasis are safe for a pregnant woman and baby. But only a doctor can prescribe them.
For more information about the hemostasiogram and various diseases that lead to disturbances in the hemostasis system, see the video.
Why should a hemostasiogram be included in the list of mandatory tests for pregnant women?
To carry out its functions in our body, blood must be in a certain liquid state, which, on the one hand, maintains hemostasis (blood coagulation system), and on the other, the anticoagulant system. The coordinated work of these two systems ensures the normal state of the blood. But a failure in this work towards the activation of one of them can lead either to an increase in blood density and the formation of blood clots, or to its too thin state and bleeding.
During pregnancy, physiological changes in the hemostatic system occur in a woman’s body due to the appearance of an additional uteroplacental circulation, changes in hormonal levels and preparation for natural blood loss during childbirth. A significant increase in blood clotting can lead to the development of DIC (disseminated intravascular coagulation), which in turn can cause disruption of placental blood flow, as well as pregnancy failure and fetal death.
The other extreme of an imbalance in the coagulation and anticoagulation systems is too much blood thinning, which can lead to severe bleeding during childbirth.
In order to avoid the problems listed above, a study of blood coagulation parameters or a hemostasiogram is carried out. As a rule, a hemostasiogram is performed several times throughout pregnancy for timely treatment of possible hemostasis disorders. In addition, this analysis is required in the following cases:
- the woman had several missed pregnancies or miscarriages;
- there are signs of gestosis: swelling of the arms and legs, high blood pressure, the presence of protein in the urine (it is better to prevent gestosis - take a hemostasiogram before pregnancy or in its early stages);
- there is a threat of miscarriage (hypertonicity of the uterus).
Indications for an additional coagulogram during pregnancy
Additional parameters are aimed at expanding the study of hemostasis. The indications are:
- Late gestosis;
- Multiple thrombosis;
- Thrombosis of the extremity veins;
- Thromboembolism;
- Increased APTT;
- Threat of miscarriage.
Before an extended analysis, the main parameters are subject to examination, and in case of deviations from the norm, additional research is carried out.
Author: Elena Yuryevna, obstetrician-gynecologist of the highest category Specially for the site kakrodit.ru
What are the differences between a regular and extended hemostasiogram?
An extended hemostasiogram is very rarely prescribed to women during pregnancy. The main difference between this analysis and the usual one is that the laboratory technician determines several additional parameters during the blood test. A detailed hemostasiogram is more labor-intensive, so its implementation is not always advisable.
Usually, during this study, doctors determine several of the most basic indicators, on the basis of which a conclusion can be made about the state of the blood coagulation system. These include:
- prothrombin, thrombin time;
- the number of blood cells such as platelets;
- parameters INR, RKMF;
- fibrinogen concentration;
- prothrombin level.
In the case of an extended hemostasiogram, antithrombin III, D-dimer, and lupus anticoagulant are additionally determined.
What are the dangers of hemostasis disorders during pregnancy?
Disturbances in the functioning of hemostasis can adversely affect the health of the expectant mother and child. Thus, when the blood thickens excessively, blood clots form in the vessels, blocking the access of oxygen to the fetus. Its lack causes hypoxia in the baby, which negatively affects its development. The child may be born defective.
Very thin blood leads to uncontrolled bleeding, which can cause placental abruption. This process creates a particular risk during childbirth, when the woman in labor may lose a lot of blood. Doctors consider the most dangerous syndrome to be disseminated intravascular coagulation, in which in the first phase of the disease the blood becomes very thick, and in the second it becomes critically thin. The result of the pathological process is initially a lack of nutrition for the fetus, and during childbirth - massive blood loss, which creates a serious danger to the life of the woman and child.
Timely hemostasiogram allows doctors to prevent a number of complications during pregnancy. Failure of hemostatic functions causes:
- deficiency of nutrients in the fetus,
- anemia in the expectant mother and child,
- premature aging of the placenta,
- freezing of the embryo or its death,
- impossibility of performing a caesarean section,
- deterioration in the general health of the pregnant woman.
Having received the results of the hemostasiogram, the doctor diagnoses abnormalities and develops a treatment plan. Medications prescribed to normalize blood parameters do not have a harmful effect on the fetus and are safe for the expectant mother.
As a rule, timely treatment significantly changes the picture of hemostasis in a positive direction, and the woman successfully bears the child. Refusing treatment for fear of taking any medications is stupid. Modern gynecology has all the tools to solve even such complex problems as restoring the process of hematopoiesis.
Hemostasiogram in pregnant women: explanation, how to take it
The period of carrying a baby becomes a serious test for most women. Unfortunately, lately there have been fewer and fewer problem-free pregnancies.
Due to the fact that the load on the body increases sharply, constant monitoring of the condition of a pregnant woman is required. Therefore, doctors prescribe a large list of tests that will promptly help identify the problem and prescribe the necessary treatment.
One of the most important studies is a hemostasiogram during pregnancy. What this is, we will try to analyze in detail in the article.
Safe carrying of a baby, and then successful delivery, depends on many factors. One of them is the ability of blood to clot perfectly so that thrombosis does not occur, but at the same time the risk of severe bleeding is minimal. This is called hemostasis.
The coagulation process involves several stages:
- the body clogs minor damage to blood vessels by accumulating the required number of platelets at the wound site.
- the formation of a plug and the appearance of a thin film covering the damage.
- the process of normal blood circulation and resorption of protective plugs is established.
The blood clotting system must work perfectly - blood that is too thick or, conversely, too thin is equally dangerous to the health of the pregnant woman and the fetus.
To avoid troubles with the circulatory system, a hemostasiogram is prescribed.
What are the consequences of impaired hemostasis during pregnancy?
Pathological disorders of hemostasis can occur even in an expectant mother who did not know about blood clotting problems before pregnancy.
Nature arranges it in such a way that a pregnant woman’s body becomes more vulnerable and, accordingly, weakened against the background of ongoing pregnancy and ongoing hormonal changes. It is very important to get tested early.
This is the only way to prevent the irreversible consequences of a malfunction of the circulatory system.
| Increased clotting | Decreased clotting |
|
|
A hemostasiogram, or coagulogram, is a laboratory research method aimed at identifying pathologies related to blood clotting.
- Coagulogram during pregnancy: norm and interpretation
This test determines how accurately a pregnant woman's clotting and anti-clotting systems are working. Any deviation in the analysis is a cause for concern and a visit to the doctor managing the pregnancy.
A hemostasiogram is prescribed three times during the entire period of gestation:
- For up to 12 weeks.
- From 22 to 24 weeks
- 30-36 weeks
A coagulogram is mandatory for everyone. There is a category of women for whom a hemostasiogram is performed more often than during the normal course of pregnancy. Risk groups include:
- women with liver diseases
- for persistent nosebleeds
- long-term infertility
- pregnancy with IVF
- multiple pregnancy
- for autoimmune diseases
- There have already been abnormalities in the blood clotting test
- unhealthy lifestyle during pregnancy
Rules for submitting biomaterial for research
- It is recommended to avoid eating 12 hours before the examination. You are allowed to dine on light, low-fat dishes.
- Before donating blood, you should drink a glass of clean water.
- The consumption of alcoholic and caffeinated drinks is prohibited.
- Avoid smoking.
- Temporarily stop taking all medications. If this is not possible, tell your doctor what medications you are using.
- It is important to have a positive attitude, as stress and other emotional experiences can negatively affect the results of the examination.
Norms and deviations. Interpretation of a blood test for coagulation
| Index | Norm | Reasons for rejection |
| APTT – time of clot formation after administration of special chemicals | from 17 to 20 seconds | Increased in hemophilia and antiphospholipid syndrome Decreased - the initial stage of the pathology of the coagulation system |
| Platelets | 131-402 *109 cells per microliter | Promotion. Inflammation process, iron deficiency, consequences of heavy stress Decreased – diseases of the hematopoietic system, abnormal processes of spleen development |
| Fibrinogen | Up to 6.5 g/l | Promotion. Infectious diseases in the acute stage. A decrease indicates toxicosis, vitamin deficiency |
| ||
| Lupus anticoagulant | negative | The detection of lupus anticoagulant in the blood of a pregnant woman is often a sign of lupus erythematosus, HIV, and cerebral circulatory disorders. |
| Thrombin time | 18-25 seconds | An increase is a sign of renal pathology. A decrease is the initial stage of DIC syndrome. |
| Prothrombin | 78 – 142 % | Increases with drug treatment Decreases when there is not enough vitamin K |
| D-dimer | At the beginning of pregnancy - 500 ng/mg. In later stages, an increase to 1500 ng/mg is permissible | Increases with severe gestosis and diabetes mellitus Decreases with thrombosis |
| ||
| Antithrombin | 70-115% | Increased: liver disease, vitamin K deficiency Decreased - tendency to thrombosis |
When changes are encountered during the interpretation of the coagulogram, the doctor prescribes appropriate treatment to prevent undesirable consequences. The goal is to preserve the health of the woman and baby.
//www.youtube.com/watch?v=10yMPKY7KkA
Such a survey is as informative as possible. It can tell in the smallest detail not only about blood clotting, but also indicate the general ailments of a woman during pregnancy.
There is no need to panic even if the coagulogram results are poor. Modern medicine is so widely developed that all the drugs prescribed to you are absolutely harmless to the baby.
Compliance with all the instructions of the attending physician increases the chance of having a completely healthy baby.
Source: //pro-analiz.ru/beremennost/analiz-na-gemostaz-pri-beremennosti.html
When and how to donate blood for a coagulogram for pregnant women
Pregnant women donate blood for a coagulogram several times during the entire gestation period.
In severe pregnancy and frequent hospitalizations, the number of coagulograms increases along with other laboratory tests.
Pregnant women in whom the cause of hemostasis disturbance has been identified and established are specially registered. For example, a genetic factor.
The test is prescribed by the attending obstetrician-gynecologist, and in some cases by a hematologist, if there are obvious blood clotting disorders.
Taking a blood test for a hemostasiogram
- blood is donated in the first half of the day on an empty stomach;
- in the morning you can drink a glass of water (not tea or coffee);
- when using medications, inform the nurse, who will make the appropriate mark on the analysis form;
- Blood is drawn from a vein using a vacuum system (not through a needle and syringe). It has been proven that the preanalytical stage (preparatory) has a further influence on the process of sample preparation and analysis. The result obtained depends on these factors;
- venous blood is placed in a test tube with the reagent and must be mixed.
The following are not subject to analysis:
- hemolyzed blood;
- clots in the sample;
- incorrect ratio of reagent and biological material.
Coagulogram
- Execution frequency
- Preparation
- Norms
- Decoding
Coagulogram (syn. hemostasiogram)
is a venous blood test that helps determine the state of the coagulation system.
Physiological pregnancy is characterized by an increase in the activity of the blood coagulation system, which is a natural process for this period. The woman’s body thus adapts to blood loss during childbirth and the appearance of an additional (uteroplacental) circulation.
Frequency of coagulation tests during pregnancy
During physiological pregnancy, a woman undergoes a hemostasiogram three times
:
- When registering;
- In the second (22-24 weeks);
- Third trimester (30-36 weeks).
information In some cases, the doctor will recommend taking a repeat test immediately before giving birth.
If there are diseases, the analysis may be ordered additionally at different stages of pregnancy.
:
- Phlebeurysm;
- Liver diseases;
- Pathologies of the cardiovascular, endocrine, urinary, circulatory systems;
- Autoimmune diseases;
- Deviations from the norm when performing previous hemostasiograms;
- Habitual miscarriage or a history of long-term infertility;
- Complicated pregnancy (gestosis, placental insufficiency, intrauterine growth retardation, multiple pregnancy, pregnancy after IVF, etc.);
- Bad habits of the mother;
- Periodic nosebleeds, bleeding gums, a tendency to “bruise” with minor bruises.
Preparing for the study
To study the coagulation system, blood is taken from a vein. The test must be taken on an empty stomach (at least 8 hours after eating), excluding the intake of any liquid other than clean water.
If you take any medications less than a day before the test, you must inform the laboratory assistant taking the blood or write the data on a form.
Coagulogram norms during pregnancy
| Basic indicators | Normal during pregnancy | Analysis transcript |
| APTT | 17-20 s | APTT is the length of time it takes for a blood clot to form after chemicals are added to the plasma. |
| Fibrinogen | By the end of pregnancy it increases to 6.5 g/l | Fibrinogen is the first factor of the blood coagulation system. It is a precursor of fibrin, from which a blood clot is formed. |
| Lupus anticoagulant | Normally absent | Antibody against blood enzymes |
| Platelets | 131-402 thousand/µl | Blood cells |
| Prothrombin | 78-142 % | ProteinAn important component of the blood coagulation system (factor 2) |
| Thrombin time | 18-25 seconds | Time required for clot formation in plasma |
| D-dimer | There is a significant increase during pregnancy First trimester: less than 500 ng/ml Second trimester: less than 900 ng/ml Third trimester: less than 1500 ng/ml Lower limit: not less than 33 ng/ml | A breakdown product of fibrin, which is part of a blood clot. |
| Antithrombin 3 | 70-115 % | Specific protein of the coagulation system |
Interpretation of hemostasiogram during pregnancy
| Basic indicators | Deviation from the norm | Possible diseases |
| APTT | Decreased APTT | Phase 1 of DIC syndrome |
| Increased APTT | Antiphospholipid syndromeHemophiliaReduced blood clotting2 and 3 phases of DIC syndrome | |
| Fibrinogen | Decrease in fibrinogen | Severe toxicosis Liver diseases DIC syndrome Taking anticoagulants Lack of vitamins B12 and C Chronic myeloid leukemia |
| Increased fibrinogen | Infectious diseases in the acute stageHypothyroidismMyocardial infarctionStrokePneumoniaSurgical interventionsBurnsOncological diseases | |
| Lupus anticoagulant | Positive result | Antiphospholipid syndromeAutoimmune diseases Systemic lupus erythematosusHIVCerebral circulatory disorders |
| Platelets | Increase in platelets | Inflammatory diseasesRemoval of the spleenAnemiaOncological diseasesBlood diseasesPhysical overexertionblood loss |
| Decreased platelets | Congenital diseases with platelet disordersInfectious diseases Systemic lupus erythematosus Thrombocytopenic purpura Blood diseases Enlarged spleen DIC syndrome | |
| Prothrombin | Increased prothrombin | Taking certain medications (aspirin, corticosteroids, barbiturates) Diseases of the circulatory system Thrombosis Oncological diseases |
| Decreased prothrombin | Hereditary diseases of the circulatory system Taking certain medications (antibiotics, laxatives, etc.) Leukemia Diseases of the pancreas, liver and gallbladder Vitamin K deficiency Intestinal dysbiosis DIC syndrome | |
| Thrombin time | Increased thrombin time | DIC syndrome Liver disease Taking heparin Significant decrease or increase in fibrinogen |
| Decreased thrombin time | Stage 1 of DIC syndromeTaking heparin | |
| D-dimer | Increased D-dimer | Severe gestosisDiseases of the urinary systemDiabetes mellitusDIC syndromeInfectious diseasesOncological diseasesDeep vein thrombosisDiseases of the cardiovascular system |
| Decreased D-dimer | An extremely rare occurrence (possibly due to thrombosis) | |
| Antithrombin 3 | Increased antithrombin 3 | Taking anticoagulants Liver diseases Inflammatory diseases Vitamin K deficiency |
| Decreased antithrombin 3 | Tendency to thrombosis Late pregnancy |
Source: //baby-calendar.ru/obsledovaniya/analizy-krovi/koagulogramma/
Hemostasiogram and coagulogram
One may mistakenly think that a hemostasiogram does some additional research and includes an analysis of the plasma system, but this is not the case. Laboratory actions for hemostasiogram and coagulogram are identical. But hemostasiogram and coagulogram differ in parameters, measurement methods and information content among laboratories.
Why do you need to do a hemostasiogram? The hemostasiogram reflects normal blood flow; in case of abnormalities, a shift in blood flow towards thickening or the risk of hemorrhage. Based on the results, you can understand what a person may suffer from - increased blood clot formation or blood loss. This procedure must be carried out before surgery to assess the risk of possible complications. Analysis during pregnancy will allow you to avoid complications throughout the entire period and how to better prepare for the birth process.
How to decipher the results of this study?
After taking this test, after some time, a person receives the results in the form of a table, which contains different numbers indicating the characteristics of the functioning of the blood coagulation system. It is quite difficult to analyze these indicators on your own. Therefore, with the results of the analysis, you need to contact your doctor, who will determine the presence or absence of any pathologies.
Typically, the test results form contains the following:
- APTT. Using this indicator, you can determine the state of the internal blood coagulation pathway. Normally it is 24-36 s. If the detected value is lower, there is a risk of thrombosis. With indicators that are higher than normal, there is a high probability of intense bleeding;
- prothrombin time. Using this indicator, the overall state of hemostasis is assessed. Normally, it should be in the range of 11-16 s;
- INR. During the study, the patient's blood clotting parameters are compared with a sample (specially prepared plasma), the parameters of which fully comply with certain standards. In a healthy person, the INR ranges from 0.85-1.35;
- fibrinogen concentration. Normally it should be 2-4 g/l;
- thrombin time. This indicator should fluctuate between 11-18 s;
- platelet count. In healthy people, this figure should be 150-400 thousand cells per 1 μl;
- D-dimer. This is a breakdown product that is formed when a blood clot breaks down. This compound is called a dimer because it contains 2 protein fragments. Normally, its value is less than 248 ng/mg. If the D-dimer is higher, this indicates that the blood being tested is thick enough. This indicates a tendency to thrombosis. Anticoagulant therapy is used to reduce D-dimer.
There may also be other indicators on the results form. Very often their normative meaning differs from the generally accepted one. Typically, each laboratory indicates its standard in the table opposite each parameter.