The mechanism of formation and causes of blood clots
During the course of life, every person has had cases of cuts, bleeding wounds and abrasions.
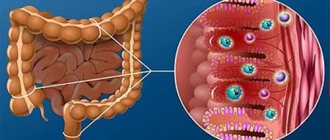
The hemostasis system, which is divided into two large groups: thrombus-forming and thrombolytic systems, saves us from prolonged bleeding and massive blood loss.
Damage to the vascular wall leads to the release of biologically active substances into the bloodstream, triggering a cascade of reactions aimed at blocking the damage and stopping bleeding.
First, blood cells that look like small white plates (called platelets) are sent to the site of injury and form a platelet thrombus. It is not persistent and is formed only as a result of aggregation (sticking together) of blood cells.
Depending on the volume of damage, fibrin fibers are layered on the platelet mass, so-called coagulation occurs, a dense and large fibrin clot is formed, strengthening the primary thrombus.
Gradually, regeneration of the injured area occurs and the thrombolytic system is activated, aimed at resolving the blockage and restoring the anatomical structure of the vessel.
The formation of blood clots occurs regularly in the body, but, being in balance, the thrombus formation and thrombolysis systems prevent serious complications in the form of tissue ischemia, prevent the blood clot from breaking off and migrating through the vessels.
If there are malfunctions in the operation of at least one of these systems, this can lead to catastrophic consequences.
External causes of blood clots are:
- Injuries accompanied by damage to the vascular wall (cuts, hematomas).
- Surgical interventions.
- Injections. Particularly dangerous are post-injection thrombophlebitis, which occur at the site of installation of venous catheters or as a result of the administration of drugs that irritate the vascular wall.
- Childbirth.
- Menstruation and so on.
The causes of internal thrombosis are:
- Vascular diseases.
- Anomaly of the thrombolytic system. Congenital and acquired pathologies of the anticoagulant system.
- Endocrine diseases. Hormonal imbalances also provoke thrombus formation.
Vascular diseases include:
- Phlebeurysm. Dilated veins lead to the retention of a large amount of blood, disrupting its movement through the vessels. This causes aggregation of formed elements and thrombus formation.
- Deep vein thrombosis of the lower extremities. Dilatation of the deep veins of the lower extremities is more dangerous than superficial varicose veins, since most often it is asymptomatic or with minor manifestations in the form of increased fatigue and a feeling of heaviness at the end of the working day, periodic spasms of the calf muscles, and swelling in the legs in the evening. Moreover, with an increase in coagulation factors in the blood (after surgery or massive trauma), blood clots can form in the veins, which easily break off and migrate through the vessels.
- Vascular atherosclerosis. High cholesterol levels lead to the formation of plaques, the covering of which can be damaged, causing blood clots.
- Vasculitis of various etiologies. Inflammation of the vascular wall most often occurs as a result of autoimmune processes and is a manifestation of systemic lupus erythematosus, rheumatoid processes, and so on.
- Condition after vascular surgery or heart surgery, especially in the presence of foreign objects (pacemakers, artificial valves, stents, etc.).
The appearance of a blood clot threatens not only blockage of the arterial vessel and tissue ischemia, but also possible rupture of it. Due to the detachment of part or all of the blood clot, it migrates along the bloodstream and completely occludes vessels of smaller diameter - this condition is called embolism.
The most dangerous is thromboembolism of the branches of the pulmonary artery, which causes a lung infarction and can lead to death, since part of the lung is completely switched off from the bloodstream. The vessels of the eyes, renal, cerebral and coronary arteries are also often affected.
Complications
Gangrene may appear
Up to 15% of patients die due to complications of the disease. If thrombosis is not treated, the blood clot begins to move through the vascular system. Its entry into the pulmonary artery causes death. Complications that reduce quality of life include:
- myocardial infarction;
- gangrene;
- hypovolemic shock;
- cardiac ischemia;
- chronic venous insufficiency;
- trophic ulcers;
- embolism.
As a result of thrombosis, the uneven outlines of the veins rise above the surface of the skin. Their appearance is accompanied by pain. Any physical activity affects the patient’s well-being. Heaviness and swelling appear in the legs. With increased stress on the legs, cramps periodically occur.
Risk group
The following categories of patients are at risk for the development of thrombosis:
- Obese people.
- Patients of the endocrinologist (patients with diabetes, thyroid diseases, and so on).
- Cancer patients undergoing radiation and chemotherapy courses.
- Women during pregnancy, especially in the later stages.
- Elderly people.
And also the risk of developing thrombosis increases due to smoking and drug addicts. The risk group includes people leading a sedentary lifestyle, eating improperly (frequent overeating, predominance of fatty foods, fast food, and so on).
Preparations for prevention
Prevention of thrombosis is carried out using two main groups of antithrombotic drugs:
- Antiplatelet agents.
- Anticoagulants.
The first group is aimed at blocking the first cellular link of hemostasis and helps prevent platelet aggregation, which is necessary in order to avoid the formation of blood clots.
These medications include:
- a group of non-steroidal anti-inflammatory drugs (the main drugs are Acetylsalicylic acid and branded drugs containing it: Kardiask, Aspirin-cardio, Cardiomagnyl, etc.);
- thienopyridines or ADP receptor blockers (Clopidogrel, Prasugrel and others);
- phosphodiesterase blockers (these include Curantil or Dipyridamole, Pentoxifylline).
The most popular tablets are Aspirin, the active ingredient of which is Acetylsalicylic acid. Its main advantages are efficiency and low cost. It is used for people suffering from chronic diseases and requiring regular medication. The main side effect of the drug is the likelihood of damage to the gastric mucosa and the development of erosive processes.
Curantil is also used to prevent the formation of blood clots, but unlike aspirin, it does not damage the mucous membrane as much. Its use should be monitored by regular blood clotting tests. It is also long-lasting, often lifelong. The dose of the drug is selected by the attending physician depending on laboratory test data (coagulogram, PTI).
In postoperative patients, Ketorol is most often used for pain relief. The drug allows you to perform two important actions simultaneously: it reduces pain and prevents the development of postoperative thrombosis.
The second large group of drugs, anticoagulants, are aimed against the formation of fibrin dense blood clots. Both direct-acting anticoagulants (Heparin, Fraxiparin) and indirect-acting anticoagulants (Warfarin, Neodicoumarin) can be used. Typically, the products are used in courses according to strict indications and in the dosage calculated by the doctor. Long-term use is possible only with local application. Heparin is most often used for varicose veins of the lower extremities in the form of heparin-based creams or gel (heparin ointment, dolobene, thrombless and others).
Symptoms of deep vein thrombosis of the lower extremities
Most deep venous thrombi occur in the small veins of the leg and are asymptomatic. When symptoms appear (eg, vague aching pain, tenderness along the veins, swelling, erythema), they are nonspecific, vary in frequency and severity, and are similar in the arms and legs. There may be visible or palpable dilatation of the collateral superficial veins. Discomfort in the legs, detected when the leg is flexed at the ankle joint with the knee straight (Homans sign), is sometimes detected with deep venous thrombosis of the distal segments of the leg, but it does not have sensitivity and specificity.
Traditional methods
Traditional medicine has been known to people since ancient times and is based on the use of natural products for the treatment and prevention of various diseases. Before using a particular method, it is necessary to approve its use from a doctor, since herbal and animal preparations may not combine well with the main therapy.
In order to combat the appearance of blood clots, the following folk remedies are the most popular:
- Decoction of willow bark. Before use, dry and grind the bark, then add 10 tablespoons to one liter of cold water, boil over low heat and let simmer for 30 minutes. Cool the broth, and it is ready for use: after straining, take a tablespoon for a long time three times a day.
- Infusion of raspberry leaves. Pour 2 tablespoons of crushed raspberry leaves into a glass of boiling water and let it brew for two hours; after straining, the infusion is ready for use. Take half a glass once or twice a day. It is recommended to carry out treatment in courses of 3 months with a one-month break, this will help protect against thrombosis.
Physical exercise
One of the important aspects in prevention is the elimination of physical inactivity. An active lifestyle helps prevent the formation of pathological blood clots, as it not only strengthens the cardiovascular system, but also helps in the fight against excess weight.
To prevent vascular accidents, it is necessary to select an adequate dose of physical activity.
Here's what physical therapy instructors recommend doing to prevent blood clots:
- Take daily walks in the fresh air, ride a bike, or go for morning jogs.
- During breaks at work, spend 5-10 minutes doing breathing exercises.
- Visit the pool 2-3 times a week.
- Perform physical therapy exercises (walking on tiptoes, rolling from heel to toe, doing squats).
- Stretch gymnastics or yoga, Pilates are useful.
The level of physical activity should be adequate to the physical condition of the person; you should not get too involved in sports. In the postoperative period, to prevent deep vein thrombosis of the lower extremities, it is recommended to try to get up from the first days and perform breathing exercises.
Diagnostics
The disease “thrombophlebitis”, as a rule, does not cause any particular difficulties in diagnosis. Today the following instrumental research methods are used:
- Doppler ultrasound using color contrast. This study allows you to fully assess the condition of the vein walls, determine the presence of thrombotic masses and the true extent of the disease.
- Rheovasography.
Laboratory diagnostic methods are used extremely rarely, since a regular blood test can only confirm moderately expressed signs of the inflammatory process.