Modern women experience problems with conception, pregnancy and childbirth more and more often every year. There are many reasons for this: age, inflammatory diseases of the reproductive system, poor health. As a result, pregnancy is often difficult, and childbirth is scheduled by emergency or planned caesarean section, which leaves a scar on the uterus or its cervix.
Symptoms
A postoperative scar has no characteristic symptoms. It does not bother the patient until the uterus ruptures along the scar. This is a very serious pathology, manifested by the following symptoms:
- bleeding from the vagina;
- pain in the lower and middle abdominal cavity;
- irregular and strong contractions of the uterus;
- decreased blood pressure;
- rare pulse;
- pale skin;
- nausea, vomiting.
Clinical guidelines
To avoid the formation of a defective scar or to diagnose it in the early stages, women after cesarean need to undergo regular ultrasound, especially when planning another pregnancy.
If after a CS there are signs of endometritis (pain in the lower abdomen, heavy uterine bleeding, purulent vaginal discharge), you must immediately consult your doctor for diagnosis and selection of an adequate treatment method.
It is recommended to adhere to contraceptive measures for at least a year after the CS to allow damaged tissue to recover. The appropriate method of contraception should be selected together with your doctor. The use of intrauterine devices is prohibited.
Causes
More often, a scar appears on the cervix after childbirth. Today, the frequency of cesarean sections in maternity hospitals reaches 25%. In addition, scar defects on the female organ occur as a result of:
- perforation of the uterus during intrauterine examination or artificial termination of pregnancy;
- gynecological surgery to treat adenomyosis or remove fibroids;
- ectopic pregnancy;
- plastic surgery to remove the intrauterine septum or correct a bicornuate or saddle-shaped uterus.
Diagnostics
A woman with a suture on the uterus when planning a child should be examined before conception. Outside of pregnancy, it is necessary to evaluate the consistency of the scar in patients who have undergone operations with opening of the uterine cavity: cesarean section, suturing of the perforation, myomectomy and others. First, the doctor palpates the contours of the walls of the uterus, evaluates the suture, and determines its size.
Further examination is carried out using hysterography (examination using an ultra-precise optical device), hysterosalpingography (X-ray with a contrast agent) and ultrasound. Laboratory tests are also carried out:
- general urine and blood tests;
- blood chemistry;
- hemostasiogram, coagulogram;
- hormonal status of FPC.
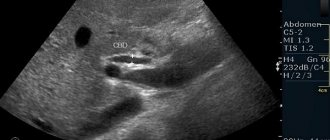
Ultrasound of the scar
If a woman is pregnant, then the uterine cavity is examined for the consistency of the scar only using ultrasound. Ultrasound helps to find out the exact dimensions of the suture, the thickness of the uterine wall in this area, the presence of niches, ligatures, unfused areas and the shape of the lower uterine segment. The results will help doctors predict the likelihood of complications during pregnancy. If an ultrasound scan of the uterine scar is performed after a cesarean section or at the planning stage of conception, then days 10-14 of the menstrual cycle are more suitable for this.
Normal myometrial thickness in the scar area
The failure of the suture on the uterus after cesarean can be determined by comparing the indicators with the norm. According to the rules, the thickness of the scar after artificial delivery should be from 5 mm. If there is thinning up to 1 mm, then this indicates its failure. During pregnancy the norms are different. Since the scar becomes thinner due to the enlargement of the uterus, at the end of the term even a thickness of 3 mm will be considered normal.
Treatment options
A scar, full or not, has no significant symptoms and does not cause concern if the woman is not pregnant. Therefore, no special treatment is required. The exception is defective scars complicated by inflammation. If they are present, suitable drug therapy or surgical intervention is selected.
When planning a pregnancy, an uncomplicated scar can be removed by metroplasty. This is an operation to restore the integrity of the muscle layer of the reproductive organ. During the intervention, scar tissue is excised to form a full-fledged scar. The procedure is carried out in three ways:
- transvaginally: through the vagina;
- laparotomy: with dissection of the peritoneum;
- laparoscopically: with the introduction of a camera and a manipulator into the pelvic area through small punctures in the abdominal cavity.
Pregnancy and scar
It takes about two years for a strong suture to form in the uterine cavity. During this time, doctors advise women to wait and not plan a pregnancy. However, a break that is too long is not the best option, because four years after the scar has healed, it begins to lose elasticity. For this reason, planning and the course of pregnancy with a suture on the cervix or other part of the female organ should take place under the special supervision of a doctor.
Possible complications of pregnancy
Thinning of the uterine scar during pregnancy is normal. However, its presence can affect the condition of the fetus. Due to the atrophied area, partial, marginal or complete presentation sometimes occurs. Placenta accreta may also appear at any level of the uterine wall. If implantation of the fertilized egg occurs in the area of the connective scar, then this is also a bad sign - in this case there is a very high risk of premature birth or termination of pregnancy.
The most dangerous complication of pregnancy is uterine rupture due to severe thinning of atrophied tissue. This is preceded by certain symptoms:
- hypertonicity of the uterus;
- pain when touching the abdomen;
- arrhythmia in the fetus;
- bleeding from the vagina;
- arrhythmic spasms of the uterus.
After uterine rupture, more serious symptoms are observed: sharp pain in the abdominal cavity, nausea and vomiting, a drop in hemodynamics, and cessation of labor. For the woman and the fetus, these consequences are disastrous. As a rule, the child experiences hypoxia, which leads to his death. A woman suffers from hemorrhagic shock. If measures are not taken in time, there is a high probability of death for the woman in labor. To save a woman, emergency hospitalization, surgical opening of the cavity with a transverse incision and curettage of the uterus are required.
Normal and pathological scar
If the incision on the uterus has healed well, then during an ultrasound the scar will be barely noticeable or even invisible.
Normally, its thickness is at least 4-5 mm. During pregnancy, this indicator changes. At 32-33 weeks, the normal thickness of the scar is 3.5 mm, at 37-38 – 2 mm. Incompetent scar on the uterus
A defective scar on the uterus is thin. The thickness of the lower segment of the organ is less than 3 mm. Cicatricial changes are noted. If the damage is replaced by connective tissue, the muscular layer of the uterus cannot fully stretch with the growth of the fetus, and ruptures are likely. Moreover, changes can also occur in a scar of normal thickness. In this case, he will also be considered insolvent.
Immediately after surgery, constant monitoring is required. Specialists watch the patient’s standing and carefully monitor the amount and nature of discharge from the uterus. In the first 5-7 days, they resemble discharge during menstruation, but are more abundant (up to 500 ml). The discharge is usually red and contains clots.
Over time, the number of lochia decreases and their color becomes darker. By 4-5 weeks there are very few of them. The color of the discharge is dark. The process of restoration of the uterine mucosa ends by 6-8 weeks. By this time, the discharge should not differ from the discharge before pregnancy.
Childbirth with a scar on the uterus
The uterine cavity is opened in two ways: a transverse one, which is made in the lower segment during a full-term pregnancy in a planned manner, and a corporal incision, performed in case of bleeding, during emergency surgery, hypoxia, or in case of premature delivery (up to 28 weeks). When pregnant with a scar in the uterine cavity, a woman usually undergoes a repeat cesarean section. However, medicine does not stand still, and in recent years, more and more women with a scar on the female organ after planned prenatal hospitalization are sent to give birth through natural means.
When is vaginal delivery allowed in the presence of a scar?
In the absence of contraindications, after a comprehensive examination and prenatal hospitalization at 37-38 weeks of pregnancy, a woman is allowed to have a natural birth with a suture on the uterus. However, for this to happen the following conditions must be met:
- the presence of one wealthy scar;
- the first operation was carried out exclusively for relative indications (fetus over 4 kg, weak labor, intrauterine hypoxia, transverse or breech presentation, infectious diseases that worsened shortly before birth);
- the first operation was performed through a transverse incision and was without complications;
- the first child has no pathologies;
- this pregnancy proceeded well;
- There are no signs of an incompetent scar according to ultrasound results;
- the estimated fetal weight does not exceed 3.8 kg;
- no pathologies are observed in the fetus.
Signs of suture dehiscence on the uterus after cesarean section
It is difficult to understand from clinical signs that the suture on the uterus begins to diverge after a cesarean section, because:
- at an early stage they may be absent;
- pain in the lower abdomen occurs not only during rupture (it looks like an incipient miscarriage);
- Possible non-typical symptoms – fever, pain only when urinating.
Therefore, women with a uterine scar from the 2nd trimester during a second pregnancy should be under constant medical supervision. When a rupture begins, it is necessary to be able to perform an emergency caesarean section.
Dehiscence of the suture on the uterus after cesarean can be suspected based on the symptoms:
- pain in the abdomen (usually in the lower part, but also in other parts);
- unpleasant sensations in the uterine area - burning, tingling, numbness, crawling “goosebumps”;
- an increase in pain during movements of the woman or fetus, emptying the bladder or bowels;
- spasms, contractions;
- increased blood pressure, temperature, pulse rate;
- bloody vaginal discharge.
Vaginal discharge of a bloody nature.
If a cesarean section was performed urgently and the scar is longitudinal, then a sudden rupture occurs without warning.
One of the first signs of suture dehiscence after cesarean section is the appearance of pain of varying strength in the pregnant woman’s lower abdomen, lower back, and upper part. Usually, the uterine tone increases at the same time (there is a feeling of compression of the uterus), and any touch to the anterior abdominal wall becomes sensitive and painful.
Symptoms of a rupture that has already occurred:
- painful contractions;
- discharge of blood or ichor from the genital tract;
- blood in the urine;
- excitement, intense fear.
If the integrity of the wall is completely violated, the pain at the height of the contraction reaches a maximum, and then labor stops.
At this time, signs of massive blood loss come to the fore:
- pressure drop;
- pale skin;
- fainting;
- shallow breathing;
- vomit;
- weak pulse (thread-like).
Scar after cesarean section
The scar after artificial delivery surgery heals in several stages. In the first week, the primary suture is formed, bright red in color with clear edges. Movement causes severe pain. The second stage is characterized by thickening of the scar. It changes color to a less bright one, it still hurts, but less than in the first week. This stage lasts a month after the operation, by the end of which pain when moving stops. The last phase lasts about a year. The scar changes color to pale pink, looks almost invisible, and becomes elastic. Healing occurs through the production of collagen.
Inconsistency of the uterine scar after cesarean section
The scar after opening the uterine cavity does not always heal well. A complication is an incompetent scar, which is improperly formed tissue at the incision site. The pathology is characterized by unfused cavities, insufficient thickness and the presence of a large amount of scar tissue, which prevents the female organ from stretching normally during the next pregnancy. The pathology is a threat to the full bearing of a child, since there is a strong displacement and change in the shape of the uterus, and a violation of its contractile activity.
Treatment of uterine scar dehiscence
Before making a decision and making a diagnosis, the woman undergoes an ultrasound. During the examination, the doctor can confidently say in what condition the suture is after the CS. If there is a divergence of scar tissue on the uterus, urgent surgical intervention is necessary. Abdominal surgery will be required so that doctors can assess the extent of the rupture, stop the bleeding and re-suture the suture.
Today, some clinics perform suturing of the scar on the reproductive organ using the laparoscopic method. However, most often an open operation is necessary: an incision in the abdominal wall and subsequent suturing of the uterine wall.
If a woman has lost a large amount of blood, she may need a transfusion. After the operation, the young mother is left in the intensive care unit for several days under the constant supervision of doctors. Further treatment includes the use of antibacterial drugs. In some cases, hormonal therapy is also necessary. The treatment regimen during the rehabilitation period is developed by the doctor depending on the patient’s condition and the presence or absence of postoperative complications.
After discharge, the woman must come for routine examinations to the gynecologist. At each appointment, the doctor will definitely perform an ultrasound to monitor the healing of the uterine scar.
Treatment
If pregnancy and childbirth proceed normally, then the uterine scar does not require treatment. In the case of an incompetent scar, the woman is advised not to plan subsequent pregnancies in order to avoid obstetric complications. The only effective treatment for this pathology is laparoscopic metroplasty. Medication or any other schemes for eliminating a failed scar in the uterine cavity are ineffective. Due to the fact that the uterus is located in the abdominal cavity behind the internal organs, it is impossible to resort to a more gentle technique.
Metroplasty after caesarean section
The indication for this operation is thinning of the myometrial walls up to 3 mm and deformation of the suture in the area of the postoperative scar. Its formation is mainly a complication of cesarean section. The essence of laparotomy metroplasty is the excision of a thin scar followed by the application of new sutures. Open surgery is determined by the need to provide access to the defect, which is located under the bladder in an area of strong blood supply. This is associated with the risk of severe bleeding during surgery.
Metroplasty is accompanied by the isolation of large vessels and the application (temporary) of soft clamps to them in order to stop blood flow. After excision of the failed scar, plastic surgery is performed, then the clamps are removed. The advantage of the laparoscopic method is the low degree of invasiveness of surgical intervention and the low risk of formation of adhesions in the abdominal cavity. The method provides short rehabilitation times and a good cosmetic effect.
Why is caesarean section dangerous - consequences and complications after surgery for the child and woman
Many women are afraid of the pain that occurs during childbirth, so they often decide to have a caesarean section. This method of delivery is used both for medical reasons and at the request of the pregnant woman.
Today, about 15% of births occur by cesarean section. Despite the fact that the procedure is performed quite often, each such operation can cause complications. Moreover, after a caesarean section, the consequences are of different nature.
Negative consequences occur both during natural delivery and in cases where the newborn is born by caesarean section. Therefore, it is quite difficult to predict in advance the degree of influence of the surgical method on the baby or mother.
According to statistics, negative consequences during natural childbirth occur 12 times less often than in cases where doctors are forced to perform a caesarean section. The female body experiences severe stress during surgery and needs more time to fully recover.
However, pregnancy and childbirth do not always go smoothly. In some cases, surgery is performed to prevent negative consequences for the mother and fetus.
The following indications for caesarean section are distinguished:
- malposition;
- pathologies of the fetus or large size of the child;
- damage to the uterine wall, tissue rupture;
- premature placental abruption;
- complicated birth process;
- problems with the placenta;
- diseases of the reproductive system in the mother;
- narrow pelvis;
- oncological processes.
Today, the risk posed by the procedure to mother and child is minimized, especially with a planned caesarean section. However, it is important to understand that surgery is not a completely safe method of delivery.
The risks associated with surgical delivery increase with each cesarean section.
This is explained by the fact that during the procedure the tissues that make up the internal organs of the abdominal cavity and pelvis are damaged. Because of this, the tone of the muscle fibers decreases, as a result of which the likelihood of developing prolapse (loss) of the walls of the vagina and uterus increases.
Also, complications after cesarean section often develop due to medical errors.
Failure to comply with the surgical technique leads to several consequences:
- infection of the pelvic organs;
- internal bleeding;
- endometriosis;
- endometritis;
- weakening of the abdominal muscles;
- problems with urination and bowel movements.
The use of anesthesia during caesarean section contributes to the development of nervous disorders. Women experience headaches a day after the procedure, attacks of dizziness and nausea. Due to general anesthesia, confusion may occur for some time.
After a caesarean section, the consequences for the mother often affect the internal organs. Once the procedure is complete, a suture is placed in the uterus and abdomen, leaving a noticeable scar.
- The presence of a scar on the abdomen after surgery imposes certain restrictions on life activities. For a month after surgery, you should avoid lifting heavy objects and limit your consumption of certain foods. This practice will help you avoid negative consequences in the form of pelvic organ prolapse. To prevent infection, antibacterial drugs are prescribed.
- A thinned scar on the uterus in the future can cause miscarriage or organ rupture. Moreover, signs of seam divergence cannot always be detected in a timely manner. Therefore, several months after the operation, the woman is sent for ultrasound diagnostics. Typically, fallopian tube ligation is recommended for reoperation. During the third pregnancy, this procedure is carried out according to vital signs. Otherwise, the consequences of the operation pose a serious threat to the patient’s health.
- Due to improper suturing of the uterine cavity, hernias in the pelvic area also often occur. This leads to a decrease in muscle tone, which subsequently becomes the cause of prolapse of the organs of the reproductive system. To avoid the development of such consequences, it is recommended that after surgical delivery you regularly perform Kegel exercises to strengthen the pelvic tissues.
Endometriosis
It is impossible to predict in advance what complications may arise after surgical delivery. Unpredictable consequences include endometriosis.
This disease develops when endometrial cells (the uterine lining) grow in atypical areas - muscle fibers and the serous layer. An important feature of the pathology is that it first manifests itself years later.
The disease causes severe pain, the intensity of which varies depending on the phase of the menstrual cycle. Infertility often develops after edometriosis.
Endometritis
Endometritis is another reason why having a cesarean section is dangerous for a woman. The pathology is characterized by the course of the inflammatory process in the inner mucous layer of the uterus. Diseases develop due to infection of tissues by pathogenic bacteria.
The consequences of endometritis are dangerous for unborn children. The disease causes miscarriages and placental insufficiency. In addition, the inflammatory process from the tissues of the uterus eventually spreads to other pelvic organs, provoking the development of adhesive disease.
When planning to become a mother, a woman should understand that the course of pregnancy is sometimes accompanied by amniotic fluid embolism. This pathological condition poses a threat to the life and health of the patient. It occurs due to the penetration of amniotic fluid into the bloodstream.
In women, embolism provokes consequences in the form of:
- increased venous pressure;
- bleeding disorders;
- thromboembolism.
There are many reasons for embolism, including medical errors made during surgery. About 70% of patients die due to this pathology. The likelihood of an embolism does not depend on whether the caesarean section is performed for the first time or again.
Bleeding
Bleeding is a common consequence of caesarean section. Its appearance is explained by the fact that during the operation the vessels are injured, and blood accumulates inside the uterine cavity. Within 4-6 weeks, the body eliminates this consequence on its own.
However, if seam separation occurs, this process continues. In this case, a repeat operation is required to eliminate internal bleeding, which must be performed within 24 hours.
Doctors identify several types of consequences of a cesarean section for a child. As they pass through the birth canal, children gradually adapt to external conditions. At this moment, physiological processes in the child’s body slow down.
Children after cesarean section experience severe stress. This is explained by the fact that the level of external and intrauterine pressure is different, which is why micro-effusions occur in the brain.
Caesarean section is also dangerous for a child because negative consequences sometimes develop several years later.
Early complications
The operation affects the child in different ways:
- The danger of a caesarean section for a child is that painkillers are used during the procedure. The components of the medicine penetrate the baby’s body through the bloodstream. Under the influence of anesthesia, the work of the respiratory center is inhibited, resulting in asphyxia (suffocation). In addition, due to medications, children often do not eat well during the first day.
- The second danger of the procedure is that the baby’s lungs are filled with mucus, which is pushed out of the organs during natural childbirth. But during delivery through surgical intervention, the fluid penetrates into the local tissue, which subsequently develops hyaline membrane disease and pathologies of the respiratory system.
- Some children, due to stress caused by pressure changes, do not produce catecholamines, which are responsible for the baby’s adaptation to external conditions.
Late complications
The consequences of the procedure may take several months or years to appear. The born child then gains weight poorly.
In children after cesarean section there are:
- hyperactivity;
- increased excitability;
- food allergies.
Due to the fact that the operation is performed under local or general anesthesia, babies are fed formula for several days after birth, since breastfeeding during this period is harmful. Therefore, in the future, children refuse mother's milk.
Among the consequences of the procedure, it should be noted the lack of psychological connection between a woman and her child that occurs at the time of birth and latching. In this case, doctors can place the baby on the body of the father or a close relative.
To prevent the development of negative consequences in the future, a woman needs to:
- undergo a control examination using ultrasound;
- regularly treat sutures with antiseptics;
- wear a bandage for several weeks;
- to live an active lifestyle;
- adjust your diet.
Compliance with these rules reduces the likelihood of seam divergence and other negative consequences.
If unpleasant sensations or other phenomena occur that indicate dysfunction of internal organs in both the mother and the child, it is recommended to consult a doctor.
The body recovers completely after surgery within 2 years. During this period, reconception is contraindicated for medical reasons.
Statistics
- It is not always possible to prevent the development of negative consequences. Often pregnant women undergo an emergency caesarean section due to vital signs.
- Delivery through surgery is carried out mainly for medical reasons. The number of such operations should not exceed 10-14% of the total number of births.
- Frequent caesarean sections at 37 weeks have a negative impact on children's health indicators.
Prevention
To prevent complications from occurring during pregnancy or childbirth in women with a scar in the uterine cavity, prevention is needed, which includes:
- assessment of the condition of the scar at the stage of pregnancy planning;
- determining the location of the placenta during pregnancy;
- formation of normal conditions for scar healing after cesarean section;
- timely treatment and prevention of pathological complications;
- fetal monitoring during labor;
- CTG and ultrasound control during pregnancy;
- a balanced approach to making a decision about natural childbirth with a scar in the uterine cavity.