Childbirth that begins at 31 weeks of pregnancy is considered premature, since nature allocates 39-40 weeks for the baby to fully develop and prepare for life outside the womb. Many expectant mothers panic when they feel the first contractions so early, but modern medicine has the ability to stop the birth process and prolong pregnancy to its due date. If you can't do this, you still shouldn't worry too much. At 31 weeks, the fetus is considered mature enough to be raised in a warm and caring environment until it can breathe and eat on its own.
Mommy. 31 weeks pregnant
Probably the most joyful event of this period is going on maternity leave. There will be more free time and you can fully enjoy your condition and fully understand your future role.
The child is already moving very actively and the pregnant woman is establishing an emotional connection with him and, to some extent, mutual understanding. If you talk to him or stroke his tummy, he will push in response, thus communicating.
The changes that have occurred in the pregnant woman’s body are already obvious and quite noticeable: posture and gait change, and under the influence of the hormone relaxin, the pelvic bones relax (so that the baby can freely pass through the birth canal during childbirth).
If earlier walks and light physical activity were easy, now it’s hardly possible, because shortness of breath appears. This is due to the fact that the growing toddler no longer fits in the lower abdomen and puts pressure on the diaphragm.
You may feel some fatigue
The thirty-first week of pregnancy is the moment when you can begin preparations: look for a stroller, a cradle, cute first toys and clothes for the little one.
Changes at 31 weeks of pregnancy
The tummy has already noticeably rounded, and is growing more and more every day. This causes some clumsiness in movements and sometimes a disruption of previous coordination. The waist grows by about one centimeter per week. This indicates that the child is actively gaining weight.
If your stomach itches, this is a clear sign that stretch marks may appear. If you use a special moisturizer or olive oil, you can prevent their appearance. Another nuance of this period is a protruding navel (do not be afraid or worry, soon after the birth of the baby it will become the same).
A completely normal occurrence is the appearance of heartburn (if it causes significant discomfort, the only acceptable option is to inform your gynecologist about this) and frequent urination. Some representatives of the fair sex also experience constipation and bloating.
The breasts also undergo significant changes: they increase in size, a venous network appears, and colostrum (a clear or yellowish liquid) may appear. You can’t express it, and to avoid leaving marks on your underwear, you need to buy special lactation pads.
During sleep or after sex, the amount of colostrum may increase. This is the norm, because this is how the body prepares for breastfeeding.
At 30-31 weeks of pregnancy, the fundus of the uterus rises approximately 30 cm above the pubis. This measurement should be carried out by an obstetrician-gynecologist during a routine examination. The baby doll is already quite large and can put pressure on the internal organs, so the optimal sleeping position is on the side.
Another feature of this stage is false Braxton-Hicks contractions. The uterus begins to contract and this causes a slightly painful (or rather pulling) sensation in the lower abdomen and in the transverse region of the back.
There is no need to be nervous, because this is a dress rehearsal, and it does not pose a danger (unless accompanied by other accompanying alarming symptoms).
Women's consultation
The pregnant woman receives her exchange card (this is a mandatory attribute that is always better to have with you in case labor begins). It records absolutely all information about the condition of the mother and fetus.
During a visit to your specialist, you need to undergo mandatory tests: a general urine test, blood test and a vaginal smear. The doctor will also listen to the baby’s heartbeat.
The doctor may refer you for an ultrasound
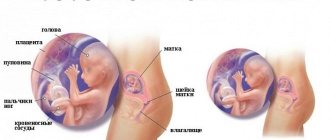
Baby. 31 weeks pregnant
The child has his own daily routine, that is, he sleeps and wakes at certain intervals. Often, the main sleep time coincides with the mother's rest.
A baby at 31 weeks of pregnancy is already quite large: its weight varies from 1500 to 1700 grams, and its height is approximately 35-40 cm. There is already not enough room for it in the mother’s tummy. In addition, from now on, on average, he will gain 200 grams per week.
He takes the position required for birth - head down. Throughout the day, the baby must perform at least 10 episodes of movements (this must be carefully monitored and if the indicator differs to a lesser extent, it is important to inform a specialist). In the photo and video of a child at 31 weeks of pregnancy you can see:
- his facial features (roughly determine which of his parents he is more like);
- that he actively blinks, squints and rubs his eyes with his fists;
- the parameters and ratio of body parts are almost like those of a newborn;
- Marigolds have already formed on the arms, and hair is growing on the head.
Imperceptible to our eyes are the developmental processes associated with the improvement of the brain, central nervous system and the preparation of the lungs to provide the baby with oxygen outside the womb. The liver begins to produce bile, and the pancreas begins to produce insulin.
You can do an ultrasound at home
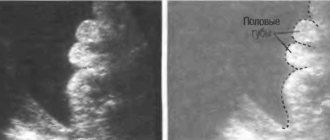
Ultrasound at 31 weeks of pregnancy
This ultrasound diagnostic is the last screening test, but no less exciting than the first. After all, the child has grown up significantly and it is so interesting to see how he is doing. The amount of amniotic fluid and the quality of the placenta are assessed, namely the degree of maturity and the level of fetoplacental blood flow.
These are important indicators that determine how effectively and correctly the toddler receives useful nutrients. Ultrasound at 31 weeks of pregnancy, or rather its protocol contains the following indicators (in millimeters):
- Biparietal skull size (73-87);
- Fronto-occipital size (93-109);
- Head circumference (215-273);
- Abdominal girth (247-301);
- Thigh (55-65);
- Shoulder (50-60);
- Forearm (45-53);
- Shin (50-60).
The four chambers of the heart (2 atria and the same number of ventricles), all valves and great vessels should also be clearly visible. The rhythm is noted as normal at a value from 120 to 160 beats per minute.
Tips and tricks
There is absolutely nothing left until day X - some 10 weeks, which in light of the preparatory bustle will pass very quickly. You can start attending courses for expectant mothers and fathers. This will help not only to prepare psychologically for the upcoming birth, but also to learn how to behave correctly during this difficult process.
You can learn breathing techniques and relaxation techniques that will help you concentrate. If a pair birth is planned, the father should also be informed about the progress of the birth process.
If you feel drowsy at the 31st obstetric week of pregnancy , this is a clear sign of a lack of oxygen and you need to spend more time in the fresh air, walking and just sitting on a bench in the park.
The main recommendations for this period include:
- control of weight gain;
- passing all scheduled tests on time and undergoing examinations prescribed by the doctor;
- visiting your gynecologist on the days when he schedules a consultation;
- consultation with a dentist at least once every two months;
- sleep should be at least 8 hours a day (and more if necessary);
- maintaining intimate hygiene;
- comfortable, loose clothing and shoes.
Nutrition at 31 weeks of pregnancy
While on maternity leave, you can spend more time on your diet and make your diet more balanced to meet all the needs of the fetus. The baby actively swallows amniotic fluid, because it tastes like food that a woman eats.
Carefully select foods in your diet
In view of this, dishes should be similar to children's: fruits, juices, vegetables, dairy products, lean fish and meat.
For breakfast you need to eat something light so as not to overstrain your stomach at the dawn of the day (homemade yogurt or cottage cheese, milk porridge).
Grated carrots and apples with sour cream, as well as nuts (it is important to be careful with them, because they are strong stimulants of allergic reactions) and dried fruits are perfect for snacks.
For lunch, a salad of fresh vegetables, seasoned with oil, light soup, boiled or steamed meat, a side dish (potatoes, rice, buckwheat) and compote (can be made from sushi) are suitable. The second snack is cheesecakes or jelly.
Breakfast should be hearty, don't skip it
Dinner – fish, baked vegetables and milk/cocoa with lean cookies. This is an approximate nutritional model; it is fashionable to make adjustments to it in accordance with personal taste preferences. You need to minimize spicy and overly salty dishes and seasonings.
It is advisable to completely exclude: smoked meats, processed foods, fast food, sweet carbonated drinks, chips, crackers, seafood, exotic fruits.
Vitamins
The bodies of mother and baby simply need vitamins and minerals. And this is especially important if a woman belongs to the “age” category (after 30 years) or has a history of miscarriage.
The main necessary vitamin elements: folic acid (veal liver, legumes, spinach, asparagus, flaxseed oil), calcium (dairy products: cottage cheese, feta cheese, milk, yogurt), iron (lentils, white beans, chickpeas, oatmeal, wheat products) , iodine (sea fish, apples, greens).
Vitamins of group B (buckwheat, eggs, rye bread, potatoes, tomatoes, broccoli, meat), as well as A (apricot, pumpkin, carrots, bell peppers, avocado) are needed.
Don't forget about vitamin C (rose hips, currants, cabbage, orange, radishes, strawberries), D (corn oil, sour cream, salmon, butter, liver, milk), E (peas, parsley, olives, turnip greens, mustard) .
As for pharmacy complexes, you should exercise caution and, first of all, consult with your gynecologist.
Weight at 31 weeks of pregnancy
In fact, many mothers underestimate the importance of nutrition, and in vain. The diet affects all vital processes, as well as: the appearance of edema, dizziness, thrush, constipation, bloating and even cramps in the calf muscles. And the most important thing is the woman’s weight.
Eat more vegetables and fruits
The kilograms that the expectant mother has gained are: amniotic fluid, placenta, baby and quite a bit of fat so that there is a reserve to be used up during childbirth. Therefore, you cannot eat for two.
It is important to eat balanced, small meals and not overeat. Weight gain at 31 weeks should range from 10 to 12.5 kg. This is taking into account that the initial weight was normal. If you are overweight or underweight, these numbers will be slightly different.
Alcohol at 31 weeks
Alcoholic drinks are contraindicated during the entire gestation period. Although the placenta acts as a barrier, it does not in this case. In addition, at this stage the permeability increases, and almost all the ethanol directly reaches the child.
It is known that it has a negative effect, because although the baby’s liver and kidneys are already formed, they are not yet designed to process such harmful substances.
Alcohol also worsens the quality of blood flow to the fetus, and this is fraught with oxygen starvation, and as a result, possible developmental disorders. The period when a small miracle grows inside is very important and it is better to take it seriously and with full responsibility, because the foundation of good health is laid in the womb.
If you want chocolate, you can eat bitter
Sex at 31 weeks pregnant
At this time, in the absence of contraindications (risk of miscarriage, softening of the cervix, leakage of amniotic fluid, infectious diseases in a partner, placenta previa), you can still indulge yourself in the joys of married life.
The only forbidden area is the breasts, because its stimulation can lead to contraction of the uterine muscles and premature birth. There are a number of positions that are designed specifically for such a case, so that both partners feel comfortable. The most comfortable: the woman lies on her side, and the man behind.
But it often happens that the wife feels unattractive or the man is worried about the child, as well as the condition of his beloved, and cannot relax at this moment. In this case, both spouses decide to end the sexual relationship.
But we should not forget that, despite this, emotional contact in a couple and support are very important. By the way, the baby will also feel harmony, trust and love between the parents.
Possible complications
In the third trimester, the body of the expectant mother is subjected to great stress. Chronic diseases may worsen, and problems associated with disruption of the functioning of internal organs may arise. Weakened immunity becomes an aid for the development of infections. The comforting fact is that the baby is already fully formed and is least susceptible to negative factors compared to the previous gestation period. Even if he is born prematurely now, most likely he will survive, and after intensive care in the maternity hospital he will be healthy. Nevertheless, the mother’s task is to take care of the baby now, and the doctors are to do everything possible so that the baby can mature in the womb, and not in the hospital. Let's take a closer look at the possible complications of pregnancy at this stage and their symptoms.
Arrhythmia
Heart rhythm disturbances are called arrhythmia
Often, mothers first learn about this deviation in their well-being in the third trimester of pregnancy. The causes of heart rhythm disturbances can be pregnancy itself, when the cardiovascular system cannot cope with the increased load. This condition can also be provoked by:
- diseases of the heart and blood vessels;
- endocrine pathologies;
- genetic predisposition;
- stress;
- bad habits and other factors.
Arrhythmia happens:
- Extrasystole. Minor disruptions in the functioning of the heart, which are noticed by the mother. Shortness of breath and chest discomfort may occur.
- Flickering. During pregnancy, it may develop for the first time or be a consequence of chronic heart disease. This form of arrhythmia is dangerous for the fetus, threatens the development of hypoxia, and requires careful medical supervision. May manifest as increased heart rate, dizziness, and fainting.
- Sinus. Usually not a consequence of heart pathologies existing before pregnancy. Causes may include anemia or thyroid dysfunction. The heart rate either decreases or increases when staying in a stuffy room, during excitement, or after physical exertion.
The diagnosis is made on the basis of a cardiogram; in some cases, an ultrasound scan of this organ is required. Treatment depends on the form of arrhythmia; in severe cases, hospitalization and monitoring of the fetal condition are required. For minor arrhythmia, the doctor may prescribe medications that normalize heart function and are compatible with pregnancy, recommend avoiding stress and excessive physical activity, spending more time in the fresh air, following a daily routine and diet.
Preeclampsia
Late toxicosis is often called gestosis. This condition is typical only for pregnant women, and usually appears after the 30th week of gestation. Preeclampsia is a complex deviation in the functioning of internal organs and systems, which negatively affects both the well-being of the mother and the fetus. According to statistics, gestosis is more common in mothers carrying their first child; it occurs in approximately 20% of pregnant women. The later gestosis appears, the less negative its effect on the fetus. With the early appearance of gestosis (before the third trimester), there is a high probability of long-term difficulties in oxygen and nutrient exchange between mother and baby.
Signs of gestosis are:
- Swelling. To a mild to moderate degree, in the absence of other symptoms of gestosis, edema in later stages is considered normal. You should be wary of excess weight gain (more than 500 g per week), associated with stagnation of fluid in the tissues, swelling of the limbs, abdomen, body and face.
- Protein in urine. It is detected only by urine analysis and has no obvious symptoms. Serves as evidence of renal dysfunction caused by gestosis.
- Increased blood pressure. Normal blood pressure for each woman is determined based on the indicators of the first trimester. Comparing the pressure at the beginning of pregnancy with today’s, the doctor can establish hypertension when the upper number is exceeded by 30 units, the lower – by 15.
Scientists cannot determine the exact causes of gestosis, voicing many theories. What is known for certain is that the condition is provoked precisely by pregnancy itself. With gestosis, blood viscosity increases, which leads to the formation of blood clots, disturbances of blood flow in the placenta, and impairs the functioning of internal organs.
With a serious form of gestosis, the mother requires hospitalization. At the early stage of gestosis, a woman is recommended to undergo outpatient treatment: she needs to follow a diet, limit fluid intake, take diuretic herbs, drugs that improve blood circulation and strengthen blood vessels, normalizing blood pressure.
The most severe manifestation of gestosis is preeclampsia. Convulsions and seizures may occur, which lead to a stroke. Fortunately, such severe consequences of gestosis are extremely rare. If disturbances in the supply of oxygen and nutrition to the fetus are detected, a diagnosis of hypoxia is established. This is dangerous for the fetus and can lead to serious disorders and even death in the womb. If detected in the later stages, doctors decide whether to induce labor or perform a caesarean section. In this case, the risk of fetal death in the womb is higher than with premature birth.
Low water
This term refers to an insufficient amount of amniotic fluid. Cases of critical oligohydramnios (3 or more times less than normal) are observed extremely rarely; moderate oligohydramnios is more often diagnosed. It is possible that moderate oligohydramnios is caused by genetic factors and does not pose a serious threat to the baby. Perhaps this condition is a consequence of leakage of amniotic fluid due to a violation of the integrity of the amniotic sac. A mother may suspect leakage if she notices too thin, watery vaginal discharge. There are also special tests sold in pharmacies that can detect amniotic fluid in natural vaginal discharge. The reason may also be an infection that has entered the mother’s body, an inflammatory process, or premature aging of the placenta. In any case, oligohydramnios requires medical supervision.
Smoking by the mother can be a factor that provokes oligohydramnios during pregnancy
Negative consequences of oligohydramnios can be:
- risk of premature birth;
- weak labor activity;
- fetal hypoxia.
Often, oligohydramnios becomes the basis for a caesarean section. A doctor may suspect oligohydramnios if the height of the uterine fundus is insufficient and does not correspond to the gestation period. In addition, with oligohydramnios, the mother feels pain when the baby moves in the stomach. An insufficient amount of amniotic fluid is detected during an ultrasound.
Treatment of oligohydramnios involves taking medications that stabilize blood flow in the placenta and eliminate the causes of this phenomenon. In case of critical oligohydramnios, doctors can induce premature birth in order to stop the torment of the fetus in the womb and relieve it of oxygen starvation.
Hypertonicity of the uterus
This condition most often manifests itself as periodic, prolonged contractions of the uterus, causing pain. Abdominal pain can last for quite a long time, radiate to the lower back, and be accompanied by a feeling of heaviness and “petrification” of the uterus.
Hypertonicity of the uterus can cause premature birth
The reasons may be:
- hormonal deficiency;
- emotional and physical stress;
- inflammatory diseases of the reproductive system;
- high or low water levels;
- large fruit;
- abnormalities of the structure of the uterus and others.
Diagnosis of hypertonicity is made based on the woman’s sensations and is confirmed by ultrasound. Hypertonicity threatens premature birth when tension in the uterine walls leads to fetal rejection. For treatment, it is necessary to remain in bed, take herbal sedatives, antispasmodics, and, if necessary, hormonal medications that support pregnancy. To alleviate the condition, magnesium and vitamin B6 are usually prescribed. Treatment can take place on an outpatient basis or in a hospital, depending on the severity of the condition.
Isthmic-cervical insufficiency
This phenomenon often causes premature birth in the third trimester. Isthmic-cervical insufficiency (ICI) is characterized by softening, shortening and premature dilation of the cervix under the weight of the uterus pressing on it. Weak cervical muscles cannot cope with the load and relax, which, in the absence of medical help, ultimately leads to premature birth. The condition is also dangerous because the membranes of the amniotic sac descend into the perineum, where there is a high probability of infection.
Recent Entries
Is it possible to give a mirror: how to protect yourself from bad omens It became known about the influence of cell phone towers on human health Is it possible to eat bananas bought in Russia?
When the cervix is shortened, there is a risk of premature birth
ICI often does not have pronounced symptoms and is detected only during a gynecological examination. In the third trimester, this event is mandatory, because the risk of cervical dilatation increases.
The causes of ICI can be physiological - with an increased content of sex hormones in the blood, or insufficient production of progesterone. The risk of ICI is increased in multiple pregnancies and with uterine defects. The cervical canal may be too wide after previous abortions or miscarriages. After childbirth, scars may remain on the cervix, which prevent its full closure during subsequent pregnancies.
When ICI is detected, a woman is fitted with a pessary - a special ring made of medical material that supports the uterus and prevents the cervix from opening. The pessary is removed immediately before birth.
Premature birth
Doctors call births that occur between 28 and 37 weeks premature. They can occur unexpectedly, result from complications of pregnancy, or be caused by doctors in order to preserve the life of the fetus in case of serious pathologies. The incidence of preterm birth in the third trimester is about 10%. At the same time, not every maternity hospital can create conditions for nursing a baby born prematurely. Usually, when there is a threat of premature birth, a woman is sent to perinatal centers equipped with everything necessary to stabilize the condition of a premature baby. In general, the prognosis for the baby is satisfactory - at this stage, neonatologists usually save babies, and their health in the future may be full or with minor deviations. Nevertheless, if there is at least a minimal opportunity to maintain the pregnancy without risk to the fetus, doctors try to take measures to this end. At the 31st week, the baby’s organs and systems are still maturing and cannot function fully outside the womb.
Doctors place premature babies in special incubators
So, you should immediately consult a doctor if you have the following alarming symptoms:
- unusual vaginal discharge (bloody or brown, with an unpleasant odor, heterogeneous consistency, etc.);
- leakage of water from the vagina;
- discharge of the mucus plug (gray, greenish, yellow);
- absence of fetal movements for several hours;
- cramping pain lasting more than 30 seconds, repeating more than 5 times per hour;
- intense pain in the abdomen and back.
After visiting a doctor with one or more of the above symptoms, you should be sent for an ultrasound, examine the vagina, and evaluate possible dilatation of the cervix. If the amniotic sac has retained its integrity, there are no signs of hypoxia or other abnormalities in the condition of the fetus, and the placenta has not completely detached, doctors will try to stop the labor process with intramuscular injections of drugs that stop contractions. When the condition can be stabilized, the woman is admitted to a hospital and the reasons for the onset of premature labor are determined; further therapy to maintain the pregnancy depends on this. Mom undergoes blood tests, a vaginal smear is examined, Doppler measurements and CTG are performed. Depending on the condition of the mother and the fetus, doctors will soon send her home or leave her in the hospital until the birth, while the threat of the premature birth of the child remains.
Physical activity
Sports at 31 weeks of pregnancy are quite appropriate and even necessary to prepare the body for the upcoming action, which is just around the corner. Popular recommended activities include:
- water aerobics;
- specialized yoga, Pilates and Yogalates;
- walking for at least 1 hour;
- breathing exercises (it is studied in detail in schools for expectant parents; it will also be relevant during childbirth).
During any exercise, the main thing is to monitor the reaction of the inhabitant of the tummy and if he is worried, then it is better to interrupt the training.
Cold at 31 weeks of pregnancy
Note to all pregnant women: the flu, colds or acute respiratory viral infections are not as terrible as their complications and consequences. Therefore, at the first signs of illness, consulting a doctor is the only correct way out.
Take walks more often
If it is not possible to do this in the next few hours, then it is important to know that the temperature should not be allowed to rise to high levels. If the value has risen, it is better to use paracetamol or a children's antipyretic.
You can also drink a lot of liquid - tea made from currant, raspberry jam, for example, with the addition of rose hips. And the most important thing in this condition is bed rest.
You can’t put any more stress on your body, because it’s already weakened.
Causes of premature birth
Some women may go into preterm labor at 30 weeks. The reasons are as follows:
- Hypertonicity of the uterus;
- Severe stress;
- Chronic diseases;
- Sexually transmitted infections;
- Pathologies of the cervix.
The most common cause is hypertonicity of the uterine myometrium. Often, tone occurs in women who are carrying several babies or one large child at once.
Fetal development continues at 30 weeks, so if there is a threat of premature birth, doctors do everything possible to prolong the pregnancy until a safe period, when the baby is considered full-term.
Premature birth is quite common
Pain at 31 weeks of pregnancy
The uterus grows, body weight increases and this gives rise to some discomfort in the back (almost the entire load goes to it and the center of gravity shifts) and knee joints.
This situation requires taking some precautions: making sure to eat enough calcium-containing foods, not walking for long periods of time, sitting on chairs with orthopedic backs, wearing comfortable shoes and not sleeping on your back.
The uterus at this stage is quite large and puts pressure on the gastrointestinal tract. Therefore, constipation or intestinal colic may occur. In this case, it is recommended to eat more raw vegetables and fruits. This is important for the prevention of hemorrhoids, which often appear under such circumstances.
If you have pain, you need to see a doctor
Belly at 31 weeks of pregnancy: tugs, hurts
Abdominal pain of any nature at this period is more likely a pathology than the norm. They may indicate placental abruption or other abnormal processes. Especially if they are accompanied by bloody or brown discharge. You should not neglect such sensations and it is better to immediately inform your obstetrician about their presence.
Aching, nagging pain in the lower abdomen is most likely a manifestation of increased uterine tone. It can cause the birth process to begin.
Another dangerous condition is pain caused by gestosis (late toxicosis), which, in the presence of other negative signs (dizziness, nausea, “spots before the eyes”, loss of consciousness, convulsions) indicate the development of preeclampsia (later eclampsia, if you do not resort to therapy).
This condition is dangerous for mother and child and requires urgent, immediate hospitalization.
Management of preterm labor
As soon as there are signs that labor is approaching, you should immediately call an ambulance. Until medical help arrives, try to move less, calm down and tune in to a positive outcome. Take two tablets of no-shpa and two tablets of brown valerian. The ambulance will take you to the maternity hospital where there is a department for premature babies.
An examination will take place in the maternity hospital, as a result of which it will be determined whether premature labor is actually beginning. If this is the case, you will be prescribed special medications and will try to prolong the pregnancy. If it is not possible to maintain the pregnancy, or there is a threat to the life of the woman or the baby, labor is not stopped; on the contrary, additional stimulation is resorted to.
Usually, natural birth at 30 weeks goes quickly, since the baby is still small and the cervix opens quickly. Most often, doctors resort to pain relief through epidural anesthesia, and at the final stage they make an episiotomy (perineal incision) to speed up the birth of the child.
On a note! If dilatation does not occur, the woman loses strength, the fetal heartbeat worsens, and doctors decide to perform an emergency caesarean section.
Unfortunately, it may happen that the fetus dies in late pregnancy. In this case, doctors induce artificial labor.
If you experience symptoms of impending labor, you should go to the hospital immediately
Discharge at 31 weeks of pregnancy
This is another aspect that needs to be carefully monitored. The norm is light, homogeneous, without a pronounced odor. Their number may increase slightly. This indicates that blood circulation in the pelvic organs has increased.
Control your weight
But if they have changed their color or character (cheesy, foamy, with a sour or purulent odor), you should urgently go for examination. These changes may be the cause of infections. And it is important to diagnose the pathological process in time and carry out treatment procedures (only a qualified specialist can prescribe them).
Self-medication in such a situation is not only inappropriate, but can also be dangerous.
If blood is released (placental abruption) or yellowish liquid (most likely a sign of leakage of amniotic fluid), then a visit to the doctor should be urgent. Such conditions require immediate hospitalization.
Childbirth at 31 weeks of pregnancy
Premature birth is one of the fears of all expectant mothers. It is important to identify the symptoms at the initial stage so that this process can be avoided. Precursors include:
- heaviness in the lower abdomen, in the vagina and anus;
- frequent urge to urinate;
- discharge of mucus streaked with blood (plug discharge);
- obvious leakage of amniotic fluid;
- brown spotting discharge.
Swimming is very beneficial
If any of them appears, you must call emergency medical help. There are times when it is impossible to prevent labor. This, of course, is a risk for the baby, but now there is all the necessary equipment designed to care for babies who were born a little prematurely.
The reasons for early birth can be: physical activity, stress, the presence of infectious diseases, a history of abortion or miscarriage. Also bad habits (smoking, drug or alcohol use by one of the parents at the planning stage, and by the mother during pregnancy), age (before 18 or after 30 years), lack of the hormone progesterone.
Treatment for threatened preterm birth
If there are signs of early labor beginning, the doctor may prescribe medications, as well as prescribe the following non-drug treatment to the pregnant woman:
- Complete sexual rest;
- Physiotherapeutic procedures;
- Bed rest, in which the legs should be slightly raised up;
- Emotional calm, lack of physical activity.
Medications are usually prescribed to help the walls of the uterus relax and stop the onset of labor. Sometimes sedatives are added to make the expectant mother calm down and stop being nervous. A woman’s psychological and emotional peace is very important during pregnancy, especially when problems arise.
The medications are initially administered to the pregnant woman intravenously, and then she can take the medications in the form of tablets. For treatment to be successful, when the first signs of impending labor appear in the early stages, the woman is hospitalized. Throughout the entire treatment period, she must be under the supervision of doctors in a hospital setting. If a woman is expecting twins, obstetricians and gynecologists often play it safe and send the expectant mother at 30 weeks to the hospital under the supervision of doctors.
If there is a threat of premature birth, the doctor may prescribe bed rest