Bronchial asthma is a chronic disease, prone to relapsing. Its main symptom should be considered attacks of suffocation, during which spasm of the smooth muscles of the affected bronchi occurs, increased secretion of thick, viscous mucus and swelling of the mucous membrane of the respiratory tract. A woman should remember this if she experiences the disease for the first time during pregnancy or if she already has it by the time she contacts an obstetrician-gynecologist. Such cases are not uncommon, because most often the disease manifests itself in early or teenage years, which leads to an increase in asthmatics of childbearing age. However, one should not think that bronchial asthma and pregnancy are incompatible. Of course, the patient will need increased attention from medical personnel, but this does not mean that pregnancy is contraindicated for bronchial asthma.
Mainly bronchi of different calibers (sizes) are affected. Their wall is inflamed. The sputum is thick, viscous and transparent. The mucous membrane of the respiratory tract is swollen.
Risk factors
One of the main risk factors influencing the development of the disease is the poor ecology in the region of residence, as well as difficult working conditions. Statistics show that residents of megacities and industrial centers suffer from bronchial asthma many times more often than residents of villages or villages. For pregnant women, this risk is also very high.
In general, a variety of factors can provoke this disease, so it is not always possible to determine the cause in any particular case. These include household chemicals, allergens found in everyday life, inadequate nutrition, etc.
For a newborn, the risk is poor heredity. In other words, if one of the two parents had this disease, then the probability of its occurrence in the child is extremely high. According to statistics, a hereditary factor occurs in one third of all patients. Moreover, if only one parent has asthma, then the probability of the child developing this disease is 30 percent. But if both parents are sick, then this probability increases significantly - up to 75 percent. There is even a special definition for this type of asthma - atopic bronchial asthma.
Pathogenesis of the development of gestational complications
The occurrence of complications during pregnancy and the perinatal period depends on the severity of the disease in the woman and adequate therapy carried out to relieve acute attacks and ongoing treatment.
In patients who suffered an asthma attack during pregnancy, the risk of perinatal pathology increases 3 times compared to patients with stable asthma.
Complications of bronchial asthma are possible for a number of reasons, which include:
- hypoxia;
- malfunctions of the immune system;
- violation of hemostatic homeostasis;
- metabolic changes in the body.
Provided that adequate therapy is carried out in pregnant women, providing specific treatment for asthma, it has virtually no effect on the general condition of the patient.
If treatment is carried out incorrectly or completely absent, the following complications are possible:
- the occurrence of secondary toxicosis, accompanied by nausea and vomiting;
- development of eclampsia, when convulsive syndrome is possible against the background of high blood pressure;
- fetoplacental insufficiency (disruptions in placental function that prevent the child from receiving nutrients). Hypoxia can be directly related to the severity of asthma in pregnant women and requires the fulfillment of all conditions that require adequate treatment;
- An important factor in the occurrence of placental disorders in patients with asthma during pregnancy is a failure in metabolic metabolism. Diagnostics confirm that asthmatics have increased lipid oxidation, but the activity of the oxidation process in the blood decreases.
Failures in the immune system contribute to the emergence of an autoimmune process, as well as the neutralization of antiviral protection. The result of placental insufficiency is hypoxic disturbances in the development of the fetus as a result of disturbances in placental blood microcirculation. These reasons contribute to intrauterine infection of women with bronchial asthma and the birth of premature babies weighing less than 2.6 kilograms.
The effect of bronchial asthma on pregnancy
Many doctors agree that treating bronchial asthma in pregnant women is a very important task. A woman’s body already endures various changes and increased stress during pregnancy, which are also complicated by the course of the disease. During this period, women experience weakened immunity, which is a natural phenomenon during pregnancy, and this also includes changes in hormones.
Asthma can cause a mother to experience a lack of air and oxygen starvation, which already poses a danger to the normal development of the fetus. In general, bronchial asthma in pregnant women occurs only in 2% of cases, so it is impossible to talk about any connection between these circumstances. But this does not mean that the doctor should not respond to this disease, because it can really harm the unborn baby.
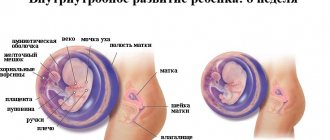
The tidal volume of a pregnant woman increases, but the expiratory volume decreases, which leads to the following changes:
- Bronchial collapse.
- Inconsistency between the amount of incoming oxygen and blood in the breathing apparatus.
- Against this background, hypoxia also begins to develop.
Fetal hypoxia is a common occurrence if asthma occurs during pregnancy. A lack of carbon dioxide in a woman’s blood can lead to spasms of the umbilical vessels.
Medical practice shows that pregnancy caused by bronchial asthma does not develop as smoothly as in healthy women. With this disease, there is a real risk of premature birth, as well as death of the fetus or mother. Naturally, these risks increase if a woman is negligent about her health without being observed by a treating specialist. At the same time, the patient becomes progressively worse at about 24-36 weeks. If we talk about the most likely complications that arise in pregnant women, the picture looks like this:
- Preeclampsia, which is one of the most common causes of death in women, develops in 47 percent of cases.
- Fetal hypoxia and asphyxia during childbirth - in 33 percent of cases.
- Hypotrophy - 28 percent.
- Insufficient development of the baby - 21 percent.
- Threat of miscarriage - in 26 percent of cases.
- The risk of premature birth is 14 percent.
It is also worth talking about those cases when a woman takes special anti-asthmatic drugs to relieve attacks. Let's consider their main groups, as well as the effect they have on the fetus.
How to plan a pregnancy
When carrying a child, it is very important to constantly monitor the pregnant woman and monitor her condition. When planning pregnancy or at least in its early stages, it is necessary to take all measures to achieve control of the disease. These include both the selection of therapy and the elimination of allergens. The patient must follow recommendations for lifestyle changes, and in no case smoke or be exposed to tobacco smoke. Before a planned pregnancy occurs, a woman should be vaccinated against influenza, pneumococcal and Haemophilus influenzae type b. Vaccine prevention of rubella, measles, mumps, hepatitis B, diphtheria and tetanus, and polio is also desirable. This vaccination begins 3 months before the expected conception and is carried out in stages under the supervision of a doctor.
Effect of drugs
Adrenergic agonists
During pregnancy, adrenaline, which is often used to relieve asthma attacks, is strictly prohibited. The fact is that it provokes spasm of the uterine vessels, which can lead to hypoxia. Therefore, the doctor selects more gentle drugs from this group, such as salbutamol or fenoterol, but their use is only possible according to the indications of a specialist.
Theophylline
The use of theophylline preparations can lead to the development of rapid heartbeat in the unborn baby, because they are able to be absorbed through the placenta, remaining in the child’s blood. Theophedrine and antastaman are also prohibited for use, because they contain belladonna extract and barbiturates. It is recommended to use ipratropinum bromide instead.
Mucolytic drugs
This group contains drugs that are contraindicated for pregnant women:
- Triamcinolone, which negatively affects the baby's muscle tissue.
- Betamethasone with dexamethasone.
- Delomedrol, Diprospan and Kenalog-40.
Treatment of asthma in pregnant women should be carried out according to a special scheme. It includes constant monitoring of the condition of the mother’s lungs, as well as the choice of method of birth. The fact is that in most cases he decides to perform a caesarean section, because excess tension can provoke an attack. But such decisions are made individually, based on the specific condition of the patient.
As for how exactly asthma is treated, several points can be highlighted:
- Getting rid of allergens. The idea is quite simple: you need to remove all kinds of household allergens from the room where the woman is. Fortunately, there are various hypoallergenic underwear, air purifying filters, etc.
- Taking special medications. The doctor collects a thorough medical history, finding out about the presence of other diseases, allergies to certain drugs, i.e. conducts a complete analysis to prescribe appropriate treatment. In particular, a very important point is intolerance to acetylsalicylic acid, because if it is present, then non-steroidal analgesics cannot be used.
The main point in treatment is, first of all, the absence of risk for the unborn child, on the basis of which all drugs are selected.
Peak Flowmetry and Asthma Action Plan
For self-monitoring of asthma, a device called a peak flow meter has been developed. The indicator it records—peak expiratory flow, abbreviated PEF—allows you to monitor the condition of the disease at home. PEF data is also used as a guide when drawing up an Action Plan for Asthma: detailed doctor’s recommendations that outline basic therapy and necessary actions in case of changes in condition. PEF should be measured 2 times a day, morning and evening, before using medications. The data is recorded in the form of a graph. An alarming symptom is “morning dips”: periodically recorded low readings in the morning. This is an early sign of deteriorating asthma control, ahead of the onset of symptoms: if taken early, you can avoid the development of an exacerbation.
Treatment of pregnancy complications
If a woman is in the first trimester, then treatment for possible pregnancy complications is carried out in the same way as in normal cases. But if there is a risk of miscarriage in the second and third trimester, then it is necessary to treat the pulmonary disease, and it is also necessary to normalize the mother’s breathing.
The following drugs are used for these purposes:
- Phospholipids, which are taken as a course, along with multivitamins.
- Actovegin.
- Vitamin E
Preventive actions
- To prevent acute attacks of the disease and various complications of asthma during pregnancy, women should give up bad habits such as smoking (passive and active) and alcohol.
- It is important to adhere to a healthy lifestyle and proper nutrition, following a hypoallergenic diet. In addition, you need to exclude highly allergenic foods, as well as fatty and salty foods from your diet.
- It is recommended to spend more time outdoors, doing moderate physical activity and especially walking. In addition, it must be taken into account that during pregnancy it is necessary to avoid contact with various allergens, especially during the flowering period of plants.
Compliance with recommended preventive measures, strict adherence to all medical recommendations and timely treatment allow a woman to safely carry and give birth to a baby. It should be noted that asthma and pregnancy may well coexist and the presence of this disease in a woman’s history is not an obstacle to motherhood.
Childbirth and postpartum period
At the hour of labor, special therapy is used to improve blood circulation in the mother and her baby. Thus, drugs are introduced that improve the functioning of the circulatory systems, which is very important for the health of the unborn baby.
To prevent possible suffocation, glucocorticosteroids are prescribed by inhalation. The administration of prednisolone during labor is also indicated.
It is very important that a woman strictly follows the doctor’s recommendations, not stopping therapy until the birth itself. For example, if a woman takes glucocorticosteroids on an ongoing basis, then she should continue taking them after the birth of the baby during the first 24 hours. The dose should be taken every eight hours.
If a caesarean section is used, epidural anesthesia is preferred. If general anesthesia is advisable, the doctor must carefully select the drugs to administer, because carelessness in this matter can lead to attacks of suffocation in the child.
After childbirth, many suffer from various bronchitis and bronchospasms, which is a completely natural reaction of the body to labor. To avoid this, you must take ergometrine or any other similar drugs. You should also be especially careful when taking antipyretics that contain aspirin.
Breast-feeding
It is no secret that many medications pass into mother's breast milk. This also applies to asthma medications, but they pass into milk in small quantities, so this cannot be a contraindication for breastfeeding. In any case, the doctor himself prescribes medications for the patient, keeping in mind the fact that she will have to breastfeed the baby, so he does not prescribe medications that could harm the baby.
How does childbirth occur in patients with bronchial asthma? Labor during bronchial asthma can proceed quite normally, without visible complications. But there are times when childbirth is not so easy:
- The water may break before labor occurs.
- Childbirth may happen too quickly.
- Abnormal labor may occur.
If the doctor decides on spontaneous childbirth, then he must perform a puncture of the epidural space. Then bupivacaine is injected there, which helps dilate the bronchi. Labor pain relief for bronchial asthma is carried out in a similar way, by administering drugs through a catheter.
If a patient experiences an asthma attack during childbirth, the doctor may decide to perform a cesarean section to reduce the risks for mother and baby.
Let's talk about childbirth
How to make it easier
An asthmatic woman should be under the supervision of a doctor already at the stage of pregnancy planning. At the initial stage, it is important to minimize all external stimuli that provoke attacks. You can learn to control them or make them less debilitating and dangerous.
Expectant parents are sometimes so worried that they ask whether it is possible to give birth with asthma, and are afraid to even plan the appearance of a long-awaited child.
Asthma is not a contraindication for pregnancy and childbirth.
BA responds well to therapy. In order for the gestation process to be as successful as possible, it is necessary to take preventive measures:
- maintain cleanliness at home;
- do not have pets;
- stop using chemicals;
- remove all things on which dust accumulates;
- take balanced vitamin complexes (must be prescribed by a doctor);
- replace bedding with synthetic ones (you may be allergic to down and feathers);
- spend more time in the fresh air, create and follow a set of physical exercises suitable for pregnant women.
Registration at the dispensary with your therapist is also required. A woman’s task is to improve her health, and then childbirth will take place without difficulty and risks.
Process Features
Since the baby may be born prematurely, it is recommended to be hospitalized several weeks before the birth process begins.
Frequent complications in asthmatic women in labor:
- early discharge of amniotic fluid;
- sudden and rapid birth.
During normal childbirth, if a sudden attack of suffocation occurs, surgical intervention is prescribed. It is noted that asthmatic manifestations rarely occur, provided that the woman in labor took prescribed medications.
During normal childbirth, oxygen inhalation is performed. It is recommended to notify your doctor about the medications you are taking and take a regular inhaler with you. Humidified oxygen may be given to patients with asthma during labor and delivery. Even at birth, treatment will continue. If a woman has severe status asthmaticus, she may be kept in the intensive care unit or intensive care unit until discharge.