A logical continuation of the postpartum period is the beginning of lactation, during which serious changes occur in a woman’s body. In primiparous women, the mammary glands are not adapted to the production and accumulation of breast milk, so the initial stage of lactation may be accompanied by pain and a feeling of heaviness.
Under certain circumstances, a woman may experience intense pain in one or both breasts during breastfeeding. In addition to pain, increased body temperature and the presence of a lump in the breast area may be of concern.
Causes
Among the variety of pathological conditions that can arise during lactation, two main causes of pain in combination with an increase in body temperature can be identified.
Lactostasis
Increased production of breast milk contributes to overstretching of breast tissue. In situations where a woman produces excessive breast milk or its discharge is disrupted, stagnation (lactostasis) develops. Congestion causes the appearance of pain and a feeling of fullness in the mammary glands.
With the development of stagnation of breast milk, there is no increase in temperature, but delaying treatment can lead to the development of a more serious pathology, such as mastitis.
The initial stage of mastitis is no different from the symptoms of lactostasis, but it should be borne in mind that this disease threatens not only lactation, but also the health of the nursing woman. The main manifestations of mastitis are local soreness in the mammary gland, the presence of compaction and increased body temperature.
In places where the inflammatory process develops, foci of redness of the skin are formed. The initial cause of mastitis is lactostasis, which is accompanied by a bacterial infection. Breast milk from a diseased breast should be expressed regularly. It is unsuitable for feeding a child.
Causes of acute pain
Acute pain in the mammary gland often indicates the development of the disease. In this case, the mother should not self-medicate, but should consult a doctor for help as soon as possible. After the examination, he will determine the cause of the deterioration in health and prescribe the necessary treatment. This often requires stopping lactation until the woman has completely recovered.
Mastitis
Acute pain during breastfeeding occurs due to the development of pathological processes. And the most common cause here is acute mastitis. This is an inflammatory process in the tissues of the mammary gland, which occurs due to a violation of the patency of its ducts and the addition of bacterial flora. According to statistics, it is diagnosed in approximately 0.5% of lactating women, especially those who often experience lactostasis and have problems with their living conditions.
Mastitis develops quickly. A woman often experiences the following symptoms within a few days:
- the appearance of sharp bursting pain in the chest during lactation, which intensifies even with a simple touch;
- increase in local and general body temperature;
- the presence of mucous or purulent discharge;
- change in the shape of the gland due to swelling;
- hyperemia (redness of the skin);
- a feeling of general weakness and decreased performance.
If mastitis is not diagnosed in time and adequately treated, then its complications may develop: abscess (cavities with pus), phlegmon of the mammary gland and sepsis (generalized spread of the bacterial process). They require emergency surgery and intensive care in a hospital setting.
Fibrocystic mastopathy
Acute pain during feeding can also occur with fibrocystic mastopathy. This disease is characterized by the proliferation of connective tissue in the gland with the formation of small cavities (cysts). Its cause is a change in hormonal levels (an increase in the concentration of estrogen in the blood).
Among women over 30 years of age, it occurs in 10-15% of patients. Usually not accompanied by clinical signs, but during lactation it sometimes gives severe pain.
Oncological diseases
Although it is a common statement among both patients and doctors that the development of breast tumors is impossible during pregnancy and lactation, this is far from the case. Often the first sign of cancer is periodic sharp pain during feeding. Upon closer examination, the following symptoms may be detected in the patient:
- a dense knot in the tissues of the mammary gland that hurts on palpation;
- deformation of the nipple or organ shape;
- the appearance of blood impurities in breast milk;
- enlargement and pain of regional lymph nodes;
- erosions or ulcers on the skin of the gland that do not heal for a long time.
Symptoms
The main manifestations of stagnation of breast milk in the mammary glands include:
- the presence of a lump in a certain part of the mammary gland;
- the appearance of edema; pain when feeding the baby and when pressing on the chest;
- redness of the skin over the area of compaction;
- when expressing, the number of milk streams decreases significantly;
- an increase in body temperature when measured in the armpit on the side of development of lactostasis.
Mastitis
In case of acute inflammation of the mammary gland, which can develop after lactostasis, feeding is painful and undesirable. You need to urgently see a doctor or call him at home. A significant increase in body temperature is possible, inflammation can progress to the stage of formation of pus, after which treatment is carried out mainly surgically, and a return to breastfeeding is almost impossible.
Mastitis, just like lactostasis, develops due to non-compliance with the feeding regimen, damage to the nipples due to improper attachment of the child to the breast, inept pumping, or an incorrectly selected bra. Weakening of the body after a difficult birth increases the risk of developing mastitis.
Pain during feeding can occur for various reasons. Some of them are natural. Then after some time the problem resolves itself. But in any case, if breastfeeding a child is painful, you should carefully monitor the accompanying symptoms, and if necessary, consult a doctor for help and advice. It will help you find the true causes of pain and quickly eliminate them without interrupting breastfeeding.
Treatment
If during breastfeeding a woman is faced with the problem of mastitis, then treatment of this disease should be carried out under the guidance of a doctor. Drug therapy includes taking antibacterial drugs, non-steroidal anti-inflammatory drugs, antipyretics, absorbable agents for external use in the form of compresses and ointments. In this case, a nursing woman is recommended to regularly empty the diseased mammary gland through pumping.
If the process is one-sided, then feeding the baby should continue with a healthy breast. If mastitis is bilateral, then doctors, as a rule, recommend temporarily switching to artificial feeding.
For the treatment and prevention of lactostasis, every nursing woman is recommended to adhere to the following rules:
- Pay attention to the condition of the mammary glands. If areas of swelling and compaction are detected, it is necessary to use self-massage techniques. The purpose of the massage is to improve blood circulation in the mammary glands, dilate the milk ducts and facilitate the passage of breast milk.
- During breastfeeding, the baby empties only one mammary gland. In order to prevent congestion, a nursing woman is recommended to express milk from the second breast.
- Choose your underwear carefully. When choosing bras, you should pay attention to underwear without wires, which can put pressure on the mammary glands when worn. The best option is to wear sports tops or special bras with elastic bands.
- Protect the mammary glands from hypothermia. Whether indoors or outdoors, it is recommended to ensure that your chest is not exposed to drafts.
- Don't overdo it with pumping. Expressing breast milk is recommended only when necessary, when a woman begins to feel discomfort and a feeling of fullness.
- Drink no more than 1.5 liters of liquid daily.
- It is best to sleep on your side, avoiding the stomach position. Before putting the baby to the breast and after feeding, it is recommended to take a warm or contrast shower, avoiding hot water.
If a nursing woman has developed lactostasis or mastitis, then it is highly not recommended to warm up and vigorously massage the mammary glands. Exposure to high temperatures and excessive pressure on the breast provokes damage to the milk ducts and also creates a favorable environment for the development of pathogenic microorganisms.
If stagnation of breast milk was complicated by an increase in temperature and redness of certain areas of the breast, then it is strictly forbidden to deal with this condition on your own. It is better to entrust this question to a gynecologist or mammologist.
It would seem that the joy of motherhood cannot be overshadowed by any problems.
Moreover, the uncomfortable sensations of pregnancy and worries about the outcome of childbirth are long gone.
But young mothers quite often, with the birth of their baby, have a new problem associated with pain during feeding.
Various myths and medical illiteracy force women to refuse to breastfeed their children.
But there are many simple ways to get rid of breast pain when feeding.
Pathologies during breastfeeding: treatment
Having felt unpleasant phenomena in the mammary glands, the mother’s first thought is to stop feeding, however, this will only worsen the situation. You need to know about the causes of chest pain during breastfeeding: how to treat it in order to reduce pain as much as possible.
With lactostasis and mastitis, you need to continue feeding; during the process you can get rid of stagnation of milk, while doing this:
- Before feeding, you need to pump, otherwise the baby will not be able to suck milk;
- When feeding, you need to try to ensure that the baby sucks on the sore mammary gland more often and longer;
- To relieve pain, take a cabbage leaf and crush it, then apply it to the breast; such a compress is effective both before and after feeding;
- Before you start feeding, you need to take a warm shower, this will reduce swelling and reduce pain;
- You also need to remember about massage.
Usually, lactostasis is cured in a couple of days; if the pain only increases and does not go away, you need to consult a doctor.
If the pain is associated with infection, then antibiotics are taken according to a doctor’s prescription. If the doctor has prescribed antibiotics, then breastfeeding is postponed for a long period, during which mandatory pumping is carried out.
When treating vasospasm, massage will help if the disease is in the early stages. To do this, lubricate the nipple with oil and massage it; short-term compression of the nipple also helps, but if such actions do not help, this is a reason to consult a doctor.
If you have thrush, you will have to take antifungal medications; if the symptoms are noticeable in the baby, he also needs to lubricate his mouth. You should ask your doctor about what medications are needed to treat thrush; self-medication can lead to prolonged cessation of lactation and worsening thrush.
Breast pain in a nursing mother: physiological condition
Chest pain in a nursing woman does not always indicate the presence of some dangerous pathologies that require serious treatment or threaten the health of the baby.
Hormonal changes
Almost all breastfeeding women experience breast pain at the very beginning of feeding. This is due to the production of the hormone oxytocin, which is able to stimulate muscle tissue and cells in the breast, which enhances milk production. Active production of this hormone is observed during the first few days after birth. In the future, even thoughts about feeding stimulate the release of oxytocin. Such physiological reflexes are felt by all women in completely different ways. For some, the discomfort is expressed by a slight tingling or sensation of strong pricks, while others feel quite strong pressure in the chest, accompanied by pain. In the future, feeding becomes natural for the woman, and painful sensations become invisible.
Nipple shape
Women who have nipples that are unnaturally shaped for breastfeeding face the problem of pain during feeding. With inverted, flat or very large nipples, feeding often causes quite unpleasant sensations. In addition to the natural structure of the breast, nipples can become flat under the influence of stagnation of milk, certain ailments, and swelling of the breast.
To avoid pain during feeding in the future, it is necessary to properly prepare unnatural nipples for feeding during pregnancy.
Large volume of milk
Some women, with sufficiently high milk production, experience pain directly while putting the baby to the breast. Unpleasant sensations are concentrated deep in the mammary gland. This condition can be observed in the first 3 months of feeding. Subsequently, if feeding techniques are followed, milk production levels out and fully meets the baby’s needs.
Breast pain in such mothers may appear before and after feeding. Excess milk literally bursts the mammary gland. To get rid of such unpleasant feelings, you can express a little milk before feeding, which will relieve pressure and feeding will be painless. Pumping after feeding stimulates milk production. Therefore, doctors do not recommend resorting to complete breast release.
What not to do
Stop breastfeeding in the first days
In the first 3 days after birth, it is normal to experience mild discomfort in the nipples. If your nipples hurt during breastfeeding or cracks appear, most likely the reason is not that you did not prepare your nipples during pregnancy or that they are “too tender.” If in the first days of feeding a mother experiences cracked nipples, an emollient cream will help her.
Read Internet
Why is it better to learn application not from videos and pictures from the Internet? The correctness of such video tips depends on the professional level of the video creator. In addition, one cannot discount the individual characteristics of the baby and mother, which cannot be taken into account in the video. A nursing mother often simply does not have the time and energy to surf the Internet and search for information.
- 5 tricks for teaching your child to fall asleep on his own (you won’t have to struggle with getting to bed)
Listen to advice from nursing friends
Many moms breastfeed in unusual positions, but they may not work for you. A breastfeeding consultant usually shows universal three or four poses and adjusts them for a specific mother and child. In addition, a friend or relative is guided only by her own feeding experience, while the consultant is armed with both theoretical training and experience working with children.
Breast pain in a nursing mother: pathological causes of the problem
Often, breast pain during or after feeding occurs due to a problem with the nipples or the presence of a breast disease. In such cases, the problem will not disappear on its own, but requires special treatment, and in some cases, the help of a doctor.
Nipple problems
The appearance of cracks in the nipples, which causes unbearable pain during feeding, is associated with a violation of feeding technology and improper hygienic care of the breast.
If a woman places the baby incorrectly to the breast and the baby does not grasp the nipple halo, all the pressure during sucking falls on the nipple. In addition, women quite often make the mistake of trying to remove the breast from a child. Of course, the baby, not being satisfied, does not want to let go of the nipple and involuntarily bites it. To avoid this problem, just lightly pinch the baby and he will release the breast.
Cracks may appear if the skin on the chest becomes very dry. Therefore, it is important to wash off any remaining milk after feeding and wipe the area around the nipple with emollients.
Thrush
The appearance of thrush on the chest is associated with the spread of a fungal infection. Most often, pathogenic fungi enter the breast directly from the baby’s mouth. But a child can become infected with a dangerous disease from his mother.
Thrush appears on the chest:
Changing the color of the nipple to bright pink and shiny;
The appearance of blisters on the chest;
Intolerable itching;
Formation of cracks in the nipples;
Shooting pain in the chest.
In addition, pain not only accompanies feeding, but also appears after it. Dealing with the problem on your own is problematic. Quite often, treatment is required not only for the woman, but also for the baby.
Lactostasis
Overfilling of the breast and stagnation of milk in the ducts is always accompanied by unpleasant sensations. At the same time, the breasts increase significantly in size. Redness, hyperemia, pulsation and flattening of the nipples may also be observed. Sometimes lactostasis is accompanied by a slight rise in temperature.
The problem is related to the mother's inexperience in matters of feeding. Tight underwear, incorrect positioning of the baby during feeding, and drinking irregularities are common causes of lactostasis. Overzealous pumping can also provoke excess milk production and its stagnation in the inflows.
Mastitis
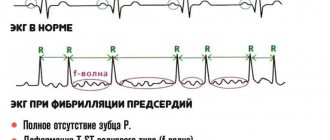
Perhaps the most dangerous reason that provokes chest pain in a nursing woman. This is an inflammatory disease of an infectious nature. Mastitis develops quite rapidly and manifests itself:
Chest tension;
Hyperemia of tissue on the chest;
The presence of pus or blood in the milk;
The presence of unnatural stripes or spots on the chest.
Increasing temperature.
The disease poses a threat to a woman's life. Therefore, it requires immediate treatment.
Torment or joy?
Alas, in most of our maternity hospitals they do not teach breastfeeding. Moreover, they teach how to turn breastfeeding into hellish torment. Judge for yourself. First, a nurse comes and in a stern voice tells the new mother to wash her breasts with soap and then wipe them dry. The breast should be presented to the baby in a “scissors” grip (the area around the nipple is pinched with the index and middle fingers). At the end of feeding, the instructions, which have passed all medical authorities, again require washing the breast with water, and if there is irritation, lubricate the nipple with brilliant green.
Where does this path lead? This can lead to drying out of the natural lubricant around the nipple, skin inflammation and cracks. It is not surprising that feeding according to such instructions becomes an inhuman feat in the name of motherhood. Biting the end of the blanket so as not to scream in pain, the young mother uses her last strength to feed her baby. How long will her heroism last?
If the skin around the nipple is red and inflamed, if there is no protective callus on the nipple and the pain intensifies during feeding, this is an alarming sign. In more advanced cases, the skin on the inflamed area becomes white (a water bubble appears) or dark red (this is a nipple abrasion). Both a water bubble and abrasion are forms of nipple inflammation that can occur for several reasons.
- Incorrect attachment to the breast. Almost all women who have had experience in the maternity hospital put their baby to the breast incorrectly. The same “scissors” grip has been brought to automaticity among millions of Russian women. Meanwhile, he is dangerous. Firstly, the breast is pinched, and milk, instead of flowing freely, stagnates in certain areas, as a result of which lactostasis often occurs. Secondly, in this position, the baby’s mouth “slides” from the peripapillary area onto the nipple itself. And this is absolutely unacceptable! In the baby’s mouth there should be not only a nipple, but also an areola. The position of the baby during feeding also matters. The physiologically correct position is lying down and under the armpit.
- Overdrying of the skin. It occurs as a result of washing the breast with soap, and even more so after using alcohol-containing solutions.
- Using waterproof pads for leaking milk. Such pads create a favorable environment for the development of inflammation.
- Incorrectly lifting the baby from the breast at the end of feeding. If the baby is torn from the breast while sucking, he will instinctively squeeze the breast with his gums and can injure it.
- Tight clothing constricting the chest.
Breast pain in a nursing mother: reasons not related to feeding
A breastfeeding woman may also have pain in her breasts for reasons that have absolutely nothing to do with breastfeeding. A woman may encounter a similar problem:
1. When wearing an uncomfortable bra. In order for the breasts to be properly supplemented with milk, it is necessary to select a bra whose seams are located on the sides and the cups do not squeeze the breasts. It is better to give preference to underwear designed for nursing women.
2. During the onset of menstruation. The restoration of the menstrual cycle is almost always accompanied by unpleasant sensations in the chest area. Similar symptoms appear at the beginning of menstruation and can bother a woman for a couple of weeks. The pain subsides after ovulation in the middle of the cycle.
3. In the presence of fibrocystic mastopathy. However, such an illness is not a reason to refuse feeding, but increases the risk of lactostasis.
Breast pain during feeding: treatment
In most cases, a woman can get rid of breast pain during feeding on her own. To do this, it is enough to learn how to properly put your baby to the breast, follow a feeding schedule and carry out hygiene procedures in a timely manner.
If you have problems with feeding, you can seek help from breastfeeding specialists who will help regulate the process and teach the correct feeding technique. During feeding, the baby should completely cover the nipple halo with his lips, and his chin should be adjacent to the breast.
Proper latching of the baby will also help cope with the problem of cracked nipples.
In addition, if there are cracks, you can use healing ointments that do not penetrate into milk and blood. For breastfeeding women, products are available in the form of Bepanten and Videstim. They must be applied to the damaged nipple immediately after feeding. Before the next feeding, the ointment is washed off the nipple.
If feeding causes very severe pain, you can stop breastfeeding for a while. If both nipples are damaged, you can use special pads that can distribute the load and reduce pain.
Thrush on the breast is a definite ban on breastfeeding. The woman will have to undergo treatment with antifungal drugs. If such a disease is detected, the baby must also be examined for the presence of infection.
With lactostasis, the best way to get rid of painful sensations is to continue feeding. You can alleviate the condition if you express a little milk immediately before feeding. This will reduce the pressure, and it will be easier for the baby to suck on the breast. You can also cope with blockage of the mammary glands with the help of massage, which must be carried out in a circular motion around the perimeter of the entire breast. A warm shower will help relieve swelling, and a compress made from chopped cabbage leaves with honey will help to cope with inflammation.
If mastitis is present, only a doctor can determine the advisability of continuing breastfeeding. Unlike lactostasis, pumping and massage for mastitis do not bring relief. Acute or serous mastitis requires the use of antibiotics. During the period of such treatment, feeding is prohibited, but you can use pumping to prevent lactation from stopping.
If mastitis has a purulent or infiltrative form, surgical intervention is inevitable, during which surgical cleaning of the mammary glands is performed. Usually, after such an intervention, lactation is no longer restored.
To avoid problems that arise during breastfeeding, including pain, a woman is recommended to take special courses during pregnancy. This will help you become familiar with the intricacies of proper breastfeeding.
There are many reasons that cause chest pain during breastfeeding. Most often, this is the child’s incorrect grip of the nipple, cracks, or inflammatory processes in the mammary gland.
Throughout pregnancy, the mammary glands prepare to produce milk.
The main growth of milk-producing cells occurs in the first months after birth. At the same time, the body undergoes serious hormonal changes. He no longer needs to provide the child with useful microelements, oxygen and protection from infections.
Pain during lactation can be natural or pathological.
In the absence of diseases, the chest hurts when:
- injury to the nipples - the nipple is very sensitive in the first month and needs special care, as the likelihood of cracks and inflammation increases;
- rapid milk flow - the sensations depend on individual pain sensitivity; the lower the pain threshold, the stronger the woman feels pain during milk flow.
The causes of pathological pain during lactation need to be known in advance.
These include:
- inflammatory processes and cracking of the nipple with subsequent infection by bacteria and fungal microorganisms;
- development of mastitis;
- lactostasis (stagnation of milk in the milk ducts with their subsequent blockage);
- Mastopathy is a common disease of the female breast, but not associated with breastfeeding.
It is important for a woman to learn to correctly characterize pain in order to understand why it appeared. This will allow dangerous pathologies to be detected in time and treated at an early stage. It is easier to prevent any pathologies by providing the necessary breast care during lactation and following the recommendations of doctors.
Preventing pain during breastfeeding
Of course, when talking about the causes of chest pain during breastfeeding: how to treat such manifestations, it is necessary to dwell on the prevention of chest pain during breastfeeding.
Let us remind you that a slight tingling sensation in the mammary glands is considered normal. To avoid pain in the mammary glands during lactation, you need to remember that:
- During pregnancy and lactation, you need to abandon the usual perfumed personal hygiene products in favor of baby soap, for example, or other natural-based products;
- Maintain reasonable hygiene, shower no more than twice a day and do not fanatically wash the mammary glands before feeding. The fact is that there are special glands on the skin that not only moisturize the nipples, but also disinfect them;
- You need to remember about the correct application of the baby to the breast: it must be completely turned towards the mother and capture the entire areola;
- If the baby is full, but does not release the breast, the little finger is inserted into his mouth and the mouth opens. If you pull out the nipple by force, this will lead to cracks;
- You need to walk topless for some time every day, so to speak, take air baths;
- It is good to follow the feeding schedule and not be late with it, then there will be no stagnation of milk in the mammary glands and you will avoid unpleasant sensations and even pain during feeding;
- Monitor the weather outside and dress accordingly to avoid hypothermia;
- After giving birth, you should not be embarrassed to ask medical staff for help feeding your baby. This way you will quickly learn how to feed your baby correctly;
- You also need to remember to express milk if there is a lot of it;
- When temporarily or partially transferring the baby to feeding from a nipple, you need to again monitor how he will attach to the breast;
Cracks in the nipples are not only a source of pain, and often unbearable, but also a gateway for infection, and there is not far to an inflammatory process, so they need to be treated; If any discomfort occurs, you should contact a doctor, remembering that now not only your health, but also the life of your baby depends on you.
Incorrect nipple latching
It is considered the most common cause of pain. Young and inexperienced mothers cannot always attach their baby to the breast correctly. As a result of this, the mammary gland hurts greatly, cracks and inflammation appear in the nipple area.
When feeding, the baby swallows a lot of air, he has tummy problems, and mothers quickly stop breastfeeding. Thus, not giving the baby the necessary mother’s milk, and causing problems during lactation associated with the baby’s lack of attachment to the breast.
To properly attach your baby, you need to follow the following recommendations:
- The baby should open his mouth wide. This will happen reflexively if you run your nipple across your lower lip, trying to move it away.
- The baby's head should be at nipple level. With proper grip, only a small part of the areola remains visible, while the nipple is located deep in the oral cavity, so it is impossible to injure it.
- If the baby is unable to latch onto the nipple, you need to help him. To do this, the thumb is placed on top of the areola, and the index finger is below, a fold is formed, and the nipple is placed in the baby’s mouth. After this, the fold straightens out and the nipple takes its right place.
If the baby latches on the nipple correctly, but the breast still hurts, it is worth consulting with a pediatric dentist to determine if there are any pathologies of the upper palate or tongue. It is also necessary to carefully monitor the lactation process, regularly observing feeding times and the number of times the baby is latched to the breast.
Pain with cracks
Injury to the nipple brings a lot of unpleasant sensations. To prevent this problem, you need to know why cracks appear.
They occur in several cases:
- when the baby is not attached correctly - when the nipple is pinched between the gums and the areola is located outside;
- in the presence of infection, pain is accompanied by burning and itching, felt not only during feeding, but also in the intervals between them;
- excessive breast care - advice from friends about thoroughly treating the mammary glands with soap or vodka solution not only provokes dry skin and increases its sensitivity, but also contributes to the appearance of severe irritation;
- if feeding is stopped incorrectly, you need to remove the nipple from the baby’s mouth very carefully, so as not to injure the nipple, you need to wait until the baby has eaten and releases the breast, but if this does not happen, you can remove the breast and insert your little finger into the mouth;
- Frequent use of a breast pump - overuse of pumping also causes irritation of the nipple and the appearance of cracks; you need to pump slowly, observing the rules of hygiene.
Cracks heal with the help of special ointments and creams, but you can coat the nipple with your milk several times after feeding. It is better to consult a doctor first to determine the exact cause of the cracks and learn how to prevent this problem.
Thrush
A common cause of pain during lactation is infection of the injured nipple by fungal microorganisms. In addition to the fact that the breasts hurt a lot, the woman feels itching and discomfort.
If thrush has spread to the milk ducts, the pain during feeding becomes unbearable. In addition, the baby can become infected from the mother. In newborn babies with a fragile immune system, the fungus can affect not only the oral cavity, but also the digestive tract, in particular the intestines. Such diseases are very dangerous for a child and are difficult to treat, especially in an advanced form.
You need to diagnose thrush as quickly as possible and begin treatment to protect yourself and your baby from exposure to fungi.
Lactostasis and mastitis - inflammation in the mammary gland
Manifested by blockage of the duct. In this case, the alveoli noticeably thicken, the mammary gland hardens, and breastfeeding is accompanied by pain and discomfort. A characteristic manifestation of lactostasis is hyperthermia of the mammary gland.
With this diagnosis, you should not stop feeding the baby; on the contrary, the number of feedings should be increased, then the breasts will become soft. Warm compresses will help relieve pain, but will not replace the treatment prescribed by the mammologist.
If lactostasis is not treated and left untreated, a woman will develop mastitis. This is an inflammatory disease that affects the mammary glands and makes breastfeeding impossible. Stopping lactation is done artificially and can take a long time.
The body temperature rises greatly, pus begins to form, which is removed through surgery.
Modern research has proven the undeniable benefits of breastfeeding for a newborn baby, and most mothers strive to feed their baby for as long as possible. Sometimes a barrier to this is chest pain in a nursing mother. In this case, the woman is forced to resort to formula milk and transfer the baby to artificial feeding. Modern infant formulas are maximally adapted, but they cannot fully replace breast milk, which contains a large amount of vitamins and microelements.
When a nursing mother's breasts hurt, this is a cause for alarm that should not be ignored under any circumstances.
In the initial stages, when the pain is insignificant, most women try not to pay attention to it, expecting the pain to go away on its own. Some women are mistaken in believing that minor pain when breastfeeding is a natural phenomenon. In fact, any unpleasant, let alone painful, sensations when putting a baby to the breast require contacting a specialist.
The most common cause of painful sensations in the breasts during feeding is a disturbance in the process of lactation. Violations can be of various types. Finding out their origin is very important, and your doctor or lactation consultant will help you with this. The following complications can create difficulties during lactation and cause sensations that make breastfeeding painful:
- Breast hardening;
- The appearance of single foci of lactostasis;
- The appearance of cracks in the nipples.
Hardening of a mother's breasts is often observed as a result of hypothermia, exposure to a draft, or emotional stress. One of the reasons may be stagnation of milk, which occurs if the child cannot cope with complete emptying of the mammary gland during feeding. This is almost always accompanied by certain symptoms: increased body temperature, increased size, hardening and engorgement of the breast. If you do not consult a specialist in a timely manner, mastitis may occur, which requires long-term drug treatment.
Single foci of lactostasis occur for no apparent reason and are also accompanied by painful sensations in the chest during feeding. When palpating the mammary gland, lumps are felt, causing chest pain. Body temperature often rises. The cause of seals is an incorrectly selected bra. For breastfeeding women, it is recommended to wear special underwear that does not compress the mammary glands (without underwires and with a comfortable cup). A single lactostasis can cause purulent mastitis.
Almost every nursing mother experiences the appearance of cracked nipples. This complication is very painful and dangerous, since pathogenic bacteria penetrate through cracks into the mammary gland, also causing mastitis.
Prevention of inflammation
- Make sure your baby is properly attached to the breast. If the baby latches onto the breast correctly, then the frequency and duration of breastfeeding is not limited. Do not allow the child to suck only the nipple, “drive” it back and forth or from side to side in his mouth, or bite his mother’s breast (even with a toothless mouth).
- Breasts are never dirty. In any case, if at this moment you are not lying bare-chested in the sandbox. Therefore, it is quite enough to wash it without soap once or twice a day.
- Do not use waterproof pads. At home, you can do without pads altogether, you just need to change T-shirts more often, and “on the go” buy ventilated pads with holes.
- Wean your baby correctly. Either wait until he releases the nipple on his own, or gently insert your little finger into the corner of his mouth. The baby will open his mouth slightly, and then you can painlessly remove your breast from him.
- If inflammation does occur, the injured nipple can be treated with Purelan, Bepanten, and Solcoseryl ointments.
Entrance gates for infections
If nipple inflammation is not treated in time, it can lead to cracks .
The cracks cause sharp, burning pain during feeding, ichor flows out of the crack, and blood may ooze out during feeding. Such a chest injury is dangerous, because an open wound becomes an entry point for infection, and from here it’s just one step to mastitis.
And therefore, if you have cracks, the matter cannot be delayed.
- The first thing to do is call a lactation consultant. He will determine how often you need to pump and for how long you will have to stop feeding from the sore breast. Unfortunately, it is impossible to resolve this issue over the phone; it is necessary to examine the chest and determine the scale of the disaster.
- During treatment, you need to stop feeding the baby from the sore breast. Depending on the size and depth of the crack, this can take from 12 hours to 2-3 days. During this time, milk from the sore breast must be expressed 3 to 6 times.
- The baby should be fed from a healthy breast. If necessary, you can supplement with expressed milk from a spoon . Under no circumstances use a bottle with a nipple for this purpose.
- Cracks require special treatment. The consultant will recommend gels for wound healing. It is very important that these are gels and not ointments. After all, we need the wound to heal as quickly as possible, and ointments can only worsen the condition.
- After the cracks have healed, you will have to once again learn how to put the baby to the breast, wean correctly and choose a comfortable position for feeding. It’s better to do this together with a consultant so as not to step on the same rake twice.
- By the way, during the treatment process and after resuming feeding, be sure to inform the consultant by phone about your condition. If there is a deterioration, then one or two more meetings will be needed to find out what is wrong.
Of course, any disease is easier to prevent than to treat. So please note
Ending breastfeeding
It is very important to end breastfeeding correctly. A fairly common phenomenon is the occurrence of chest pain at the end of the lactation process, especially in the case of forced interruption. The mother's mammary glands continue to produce milk in the same volume, but the child no longer consumes it. As a result, the mother stopped breastfeeding, and milk stagnation formed, the mammary gland hardens, acquires a reddish tint and becomes hot. Following simple rules will help you avoid this problem when finishing feeding:
- Firstly, it is advisable to extend the breastfeeding process until the age of one and a half years, when the body is ready to stop feeding. During this period, a woman begins to feel tired from feeding, both mentally and physically. Milk production is observed in small quantities and you may notice that the breasts have stopped filling.
- Secondly, weaning should occur gradually. Alternative nutrition will help with this, replacing one breastfeeding every day. It is advisable to remove night feedings last.
How to deal with pain
To reduce the severity of chest pain during breastfeeding, doctors advise adhering to the following recommendations:
- If the baby does not suckle enough, it is advisable to express the remaining milk manually or using mechanical suction.
- Check whether the baby completely covers the nipple during feeding, and whether the mother is pressing it too tightly to the breast.
- Continue to put the baby on the sore breast.
- After finishing feeding, apply ice to the breast for approximately 10-15 minutes. This will reduce the severity of pain.
- Between feedings, perform a gentle massage from the center of the gland to the periphery. All movements should be soft and without pressure. Carry out the procedure 4-5 times a day.
- 10 minutes before feeding, you can apply dry heat to the breast, which promotes the release of milk. This can only be done in a situation where bacterial inflammation is excluded.
- Sufficient water regime. The patient needs to drink at least 1.5-2 liters of liquid (still mineral water, juices, weak tea).
- Comfortable outer clothing that should not put too much pressure on the mammary glands.
Drug therapy
When prescribing pharmacological agents, it is necessary to understand that most of them pass into breast milk, and with it into the child’s body. Therefore, either drugs that are not toxic are prescribed, or it is necessary to suspend feeding during the period of therapy.
Non-steroidal anti-inflammatory drugs are used to reduce pain. Without fear of toxic effects for the child, paracetamol or ibuprofen can be used. Sometimes other analgesics are prescribed (diclofenac, ketoprofen, metamizole), but then lactation is temporarily stopped.
For acute mastitis or its complications, antibacterial drugs are prescribed. Preference is given to 3rd generation cephalosporins (ceftriaxone, cefotaxime, ceftazidime), which are administered intravenously or intramuscularly for 5-10 days. Alternatively, fluoroquinolones (ciprofloxacin, ofloxacin, levofloxacin) or carbapenems (imipenem, meropenem) are used.
If oncological pathology is found, then immediate cessation of lactation is required. The patient requires combination chemotherapy and radical surgery to remove the tumor and its metastases.
For hormonal problems, the use of estrogen or progesterone preparations is required. In such a situation, feeding must also be stopped.
Let's sum it up
If painful sensations of any nature appear in the mammary glands, you must immediately consult a doctor (mammologist, gynecologist, surgeon, therapist, lactation consultant). The sooner a specialist discovers the cause of pain, the easier and more effective the treatment will be. The early stage can be treated much faster and more painlessly. Self-medication can lead to the development of the disease and the need for surgical intervention.
Breastfeeding consultant Yulia Nikolaevna Mamon:
For successful breastfeeding and positive emotions from it, it is necessary to follow the rules of latching on to the breast, the order of breastfeeding, and try to adjust the time between feedings so that there is time for the mother to rest. Expressing during normal lactation is not required. It is necessary to monitor the nutritious, vitamin-rich diet of a nursing woman and spend more time in the fresh air. By following these simple recommendations and establishing a daily routine, breastfeeding will last a long time and bring a lot of positive emotions!
During lactation, the mammary glands undergo a serious test. Therefore, many nursing mothers complain of chest pain when feeding. This is usually a natural reaction caused by a change in the body. However, pain can also indicate the emergence of more serious problems. Let's look at the main causes of pain and ways to solve them.
From this article you will learn:
Lactostasis
One of the most common reasons why breasts hurt during breastfeeding. Lactostasis occurs in almost every woman during breastfeeding and is characterized by the following symptoms:
- In the mammary gland, you can feel a shaped lump with clear edges, painful when touched.
- The body temperature of a nursing mother rises rapidly and can reach 39 – 39.5 °C.
- Chest pain is also observed after feeding, if the lump does not go away.
There can be many reasons why milk stagnates in the milk ducts, the main ones being:
- Clothes that are too tight or the wrong bra size.
- Sleeping on your stomach.
- Incorrect breast latch by baby during feeding
- Compressing the breast with your hands when feeding, as a result of which the outflow of milk from the glands is disrupted.
- Unstable emotional state: stress, worries, overwork
- Bruises or blows to the area of the mammary glands can also lead to stagnation.
The very first and most effective way to combat lactostasis is to increase the frequency of the baby’s latching on the sore breast. It is better to apply it in such a way that the child’s chin is exactly above the lump; in this position, the most intensive resorption of the stagnant lump occurs.
If after several applications your breasts hurt during breastfeeding, then you can try to strain the lump yourself. This procedure should only be carried out with clean hands. Before expressing, it is very good to take a warm shower, while directing the flow of water to the seal to slightly relieve spasms in this area. Start with gentle stroking movements in the direction of the milk ducts (from the periphery to the nipple), and then use two fingers to press the area along the edge of the areola. You need to express milk until your breasts become soft and lumps are no longer felt.
If independent manual expression does not bring results, it is better to seek help from a lactation consultant or the emergency department of the maternity hospital. These specialists themselves will express the lumps for you, and all symptoms, including fever, will disappear in a few hours.
In any case, breast pain during feeding caused by stagnation of milk needs immediate relief by expressing the lump, otherwise you may face mastitis.
Main reasons
Almost every woman has encountered the problem of breast pain during feeding. Discomfort occurs immediately after childbirth and lasts from several days to several weeks, which is due to normal processes in the woman’s body.
The skin of the nipples is quite delicate, so time must pass for it to harden and for the woman to be able to feed the baby without pain. If the baby is properly applied to the breast and the feeding regime is followed, then very soon natural feeding will bring only joy and pleasure.
If the discomfort appears later, the cause of chest pain during feeding may be:
- Cracks in the nipple area.
Most often, cracks and abrasions appear due to improper attachment of the child. It can also be caused by the appearance of teeth in the baby or a sudden interruption of the feeding process, when the baby does not let go of the nipple, but is forcibly removed from the mouth. - Lactostasis.
The most common cause of discomfort in the chest area. This condition is due to the fact that milk does not leave the lobule of the mammary gland during feeding, so stagnation occurs. Diagnosing lactastasis is very simple - you should carefully feel your breasts and you will feel a small nodule or compaction. - Flushes of milk.
Many women feel a rush of milk right during feeding. This condition is nothing to worry about, but it can cause tingling, tingling or even severe pain. Over time, the sensations will become weaker, and many women stop feeling discomfort altogether. The same sensation can occur if the mother has too much milk. - Mastitis.
Inflammation and blockage of the milk ducts indicates mastitis. The disease is accompanied by redness of the skin of the chest and a strong increase in body temperature. The main symptom is severe pain when feeding. It is very important to continue breastfeeding your baby, but you should definitely seek medical help.
All of the above problems, not counting milk flow and excessive amounts of milk, require your attention
. For example, cracks in the nipples can cause infections, and lactostasis can turn into mastitis after some time.
Work calluses
Let's figure out why pain may occur during feeding and what it means.
So, when a newborn baby is put to his mother’s breast for the first time, new sensations arise not only for him, but also for his mother. This is especially true for first-born children. But even if a woman has already had experience of motherhood and breastfeeding, her breasts have already managed to “forget” how a tiny tongue and strong gums work. The skin on and around the nipple is very thin and delicate, so the mother is guaranteed quite strong sensations.
The baby instinctively “polishes” the mother’s nipple, and gradually the skin becomes harder and less vulnerable, and a kind of callus is formed. If you've ever learned to play the guitar, you probably remember how each string initially leaves an imprint on the soft pads of your fingers. Then the traces of the guitar strings simply “burn”, and finally the skin becomes rougher, and protective calluses allow you to play the guitar almost painlessly.
Something similar happens during breastfeeding. In the first days after childbirth, the skin may crack slightly, turn white, and white crusts may appear on it. This is how “labor calluses” are formed; this process can take from a couple of days to a couple of weeks.
Pain may occur when the nipple is latched. But as soon as the baby begins to actively suck, the painful sensations go away. Such pain (and sometimes not even pain, but just a strong sensation) occurs under the influence of hormones and does not require special therapeutic measures.
Treatment for chest pain
The first thing you should do if you experience discomfort is to consult with a specialist on how to properly attach your baby to the breast. It is incorrect attachment that is the main cause of all further problems with breastfeeding.
If cracks and abrasions are found, you should:
- Check your nursing clothes. There should be no seams or other hard elements that may come into contact with the nipples.
- Be sure to give your breasts air baths after feeding. This way, the skin cells will breathe and the gland muscles will relax.
- Use special gaskets and replace them regularly.
- Watch your baby take the nipple. It should capture both the nipple and the areola itself - it will be more comfortable for you.
- After feeding and short air baths, treat the cracked nipple with healing oil. Sea buckthorn oil with a wound healing effect is best suited.
Allergy
An allergic reaction that occurs to medications used for breast healing. In this case, the pain and inflammation of the skin of the nipples and areola not only does not go away, but also intensifies and can spread to areas of the skin behind the areola where the drug has entered.
Solution to the problem: When using external medications, it is necessary to test for the possible presence of an allergic reaction.
Having become familiar with the main causes of breast pain during feeding, you can analyze your situation and find the cause of pain during feeding specifically for you. The pain can also be caused by the baby, which is also important for solving the problem. If you still have difficulty determining the cause, finding an answer to correcting the condition or treatment, contact a specialist for help.