The placenta supplies the baby with oxygen, vitamins and microelements, and cleanses the amniotic fluid from waste products. Its formation begins at 10–12 weeks of gestation, but attachment to the lining of the uterus occurs much earlier, at the chorion stage. Low placentation during pregnancy occurs due to the placement of the placenta in the lower region of the uterus, which threatens a number of complications both during gestation and at the time of birth.
The transformation of the chorion into the placenta lasts until 16–17 weeks. However, the growth of the organ, which is important for the baby, continues in parallel with the development of the baby - until the 36th week. The low location of the placenta may move upward by the time of birth, then the risk of negative consequences will decrease. But if the placenta shifts towards the internal uterine os, is located less than 5-6 cm from it, or partially or completely blocks the lumen, this will already be called low placenta previa. Then the danger will increase.
Classification
In the third trimester of pregnancy, placenta previa occurs in 2-3% of women. In the second trimester, during an ultrasound, a low position of the baby's place can be detected more often.
information This is due to the phenomenon of placenta migration: as the uterus grows, the placenta moves upward and takes a normal position.
There are two classifications of placenta previa
, which are determined during pregnancy and in the first stage of labor.
Presentation during pregnancy
is determined using ultrasound:
- complete
(the internal os of the cervix is completely blocked by the placenta); - partial
(the placenta partially covers the internal os); - low
(the placenta is located at a distance of less than seven centimeters from the internal os).
Placenta previa during childbirth
determined when the cervix is 4 cm or more open by vaginal examination:
- Central
(the internal os is completely covered by the placenta, the fetal membranes are not visible). - Marginal
(in the area of the pharynx, only the membranes are identified, the placenta is located at the edge of the internal pharynx. - Lateral
(in the area of the internal os, the lower part of the placenta and fetal membranes are determined).
Recently, this classification is practically not used, because the presence of ultrasound provides more accurate data on the location of the placenta. During an ultrasound, four degrees of placenta previa are also determined:
- First degree
. The placenta is located in the lower part of the uterus at a distance of at least three centimeters from the internal os. - Second degree
. The placenta is located near the internal os, but does not overlap it. - Third degree
. The internal os is covered by the lower edge of the placenta, the rest of the baby's place is located asymmetrically on the anterior and posterior walls of the uterus. - Fourth degree
. The central part of the placenta covers the internal os of the cervix, the edges are located symmetrically on the walls of the uterus.
Normal location of the placenta
From a physiological point of view, the most optimal is the attachment of the placenta along the posterior wall. The fact is that during pregnancy the walls of the uterus stretch unevenly. As the child grows, the front wall increases in size and stretches, while the back wall retains its density and stretches much less.
The front wall becomes thinner as it stretches. From here it becomes clear that for the normal functioning of the placenta, a location along the rear wall is more advantageous, since this way it is exposed to a minimum of stress.
Advantages of location on the rear wall
- The placenta is ensured immobility - placenta previa on the posterior wall is extremely rare, the placenta does not descend down and there is no threat to pregnancy.
- Uterine contractions and increased tone will not increase the risk of placental abruption.
- The placenta is less exposed to blows and jolts from the baby when it moves.
- Lower risk of increment.
- There is a lower risk of injury to the placenta due to an accidental blow to the abdomen.
- There is a lower risk of bleeding with a caesarean section.
Causes of placenta previa
Additionally, the main reasons for the pathological location of the placenta
are changes in the endometrium (inner layer of the uterus), as a result of which the embryo does not implant correctly in the uterus.
Such changes in the endometrium can cause:
- Chronic inflammation of the uterus
(endometritis). - Repeated curettage of the uterus
(abortions, diagnostic procedures). - Uterine fibroids
. - Multiple births
. - Endometrium
h. - Multiple pregnancy
. - History of caesarean section
.
Symptoms and complications
The main symptom of placenta previa
is the sudden occurrence of bleeding from the genital tract.
Most often, spotting occurs in the third trimester, but with a significant degree of presentation it can occur earlier. Bloody discharge can vary in the amount of blood flowing out: from minor spotting to heavy bleeding. The discharge, as a rule, has a bright scarlet color and completely flows out of the vagina without forming hematomas in the uterus. The uterus is in normal tone and painless. Complications of placenta previa
:
- Anemia due to repeated bleeding.
- Premature termination of pregnancy.
- Incorrect presentation and fetal position.
- Chronic fetal hypoxia and, as a consequence, intrauterine growth retardation.
What are the dangers of placenta previa?
Incorrect position of the placenta is a rather dangerous condition that can provoke the following consequences:
- premature birth;
- partial placental abruption - as a result of this condition, the child does not receive the required amount of oxygen and nutrients, which may result in the development of serious pathologies;
- bleeding - bleeding is dangerous not only due to early labor or hypoxia for the fetus, but also poses a direct threat to the mother, since heavy loss of blood during childbirth can lead to loss of consciousness;
- complications during childbirth - very often the movement of the child through the birth canal is complicated by the placenta, which covers part of the internal os.
important Placental malposition requires careful monitoring. It is necessary not only to carefully follow any recommendations of a specialist, but also to regularly undergo all kinds of examinations to assess the condition of both the placenta and the child. An ideal option for a pregnant woman would be the opportunity to go to the hospital several weeks before the expected date of birth.
How to determine the type of presentation
Diagnosis of fetal presentation before the onset of active labor is carried out in antenatal clinics and maternity hospitals. Doctors make the most reliable conclusion about the presentation of the fetus after 35 weeks, since before this period there is a possibility that the child will independently take the proper position before birth. If the presentation is incorrect (oblique, pelvic, transverse), gynecologists advise the woman to perform special exercises that can contribute to the rotation of the fetus. After the 36th week of pregnancy, there is practically no room for the baby to move, and he takes the position in which he will be born.
How to determine fetal presentation? The diagnosis is made by a gynecologist based on the results obtained. The expectant mother must undergo a vaginal and obstetric examination. In addition to objective data, the woman needs to have an ultrasound, preferably three-dimensional echography. This type of study is most important for breech presentation, to determine its type.
Determining the presentation of the fetus is an integral point in the management of pregnancy. This is necessary to make a decision on the method of delivery, as well as to prevent the occurrence of complicated labor. In case of breech presentation, it is very important to determine what type it is. In case of headache, doctors pay attention to the position of the head and the degree of extension of the neck, since excessive extension of the neck can lead to serious injuries during passage through the birth canal. For example, injury to the spinal cord, cerebellum and other injuries.
Diagnostics
You can find out that there is something wrong with the placenta and that there is a threat to the health of the baby and the expectant mother already in the first trimester during a routine ultrasound. In a number of cases, a situation arises where the “baby seat”, located incorrectly, fell into place by the 20th week. This is due to the fact that the final formation of the placenta is completed just by this time, which means that if you hear a sad diagnosis before 20 weeks, you should not despair, since after a few weeks everything can return to normal.
Central placenta previa
In this case, the center of the placenta completely covers the birth canal. With central placenta previa, the baby's place cannot take the correct position even over time, which is why this condition requires careful medical supervision.
It is for these reasons that this type of arrangement is most often diagnosed in women giving birth for the second or third time.
Symptoms
- sensation of stretching in the lower back;
- uterine tension;
- impaired blood supply, resulting in drowsiness and fatigue;
- spotting or fairly heavy bleeding that does not cause any discomfort and can be provoked either by a routine gynecological examination or by sexual intercourse.
Recommendations for central placenta previa
Since in this case the placenta does not move into place even over time, the main task of doctors is to carefully monitor the pregnant woman. If a woman experiences discomfort in the uterine area or notices spotting, then from that time on she is recommended to go to the hospital, where she will have to stay until the time of birth.
important Natural childbirth in this case is simply impossible, since the baby’s place completely blocks the birth canal, preventing the birth of the child.
Anything can cause central placenta previa, from an unhealthy lifestyle to frequent abortions. Any deviations associated with the position of the placenta most often befall multiparous women who suffered any injuries or complications during their first birth.
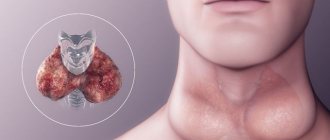
What is the placenta and how is it normally attached?
The placenta is an organ that appears and develops in a woman’s body after the appearance of the fertilized egg. In appearance, it is similar to a disc, which is located between the membrane of the fetus and the walls of the uterus . The placenta is the connection between the mother and the child and performs the following functions:
- supplies the child with nutrients;
- purifies his blood;
- removes toxins and waste;
- provides the fetus with oxygen;
- protects against infections.
The placenta begins to develop on days 10–12 from the moment of conception and is finally formed by the 15th week. Ideally, the placenta should be attached in the upper part of the uterus , along the back wall with transition to the sides. These areas have the best blood supply to the walls of the uterus and the least possibility of any injury.
Regional presentation
In marginal placenta previa, the anterior part of the baby's place is located, as it were, on the edge of the birth canal. Typically, symptoms indicating a marginal location are:
- quite severe bleeding;
- slight bleeding from the vagina during bowel movements or when lifting heavy objects.
The danger of placing the “baby seat” on the edge of the pharynx is fraught with the fact that during childbirth, the sector where it is attached is most actively involved in the birth process, due to which its rapid contraction occurs. As a result of this, the vessels connecting the baby's place with the uterus rupture, causing severe bleeding, which is fraught with dangerous consequences in the form of anemia for the mother and severe hypoxia for the child. Diagnosis of marginal placenta previa occurs by ultrasound.
Recommendations for marginal placenta
- It is important to wear a special bandage.
- Special physiotherapeutic procedures.
- Taking a laxative.
- Refusal of physical activity.
- Exercises in the knee-elbow position.
- Complete abstinence from sexual contact during pregnancy.
- Bed rest and absence of stressful situations.
important Childbirth in this case most often takes place by caesarean section.
Oblique position of the fetus during pregnancy
Usually, the fetus is forced into this position if there are abnormalities in the structure of the uterus or tumor, or obstacles. In this position, childbirth is definitely carried out surgically; it is simply impossible for the child to pass through the natural birth canal in this position.
In this case, the presentation of the fetus is not determined - there is no presenting part.
If there are no apparent reasons for the fetus to adopt this position, it is worth carrying out exercises to stimulate the turning of the baby, described below. With an oblique position of the fetus, you need to lie as much as possible on the side towards which the back of the fetus is facing.
With a stable oblique or transverse presentation, the woman is admitted to the maternity hospital two weeks before giving birth and the issue of delivery is decided, which will be the most favorable in this situation - a cesarean section.
Previously, manual correction of malpresentation of the fetus was practiced by externally rotating the fetus. The doctor tried to move the fetal head down through the anterior abdominal wall. Today, such actions have been abandoned as ineffective, having a high percentage of complications in the form of premature birth, disorders of the child’s condition and placental abruptions.
Lateral placenta previa
Lateral placenta previa is one of the most common cases of incomplete location. In this situation, part of the placenta is located in the area of the internal os, but does not completely cover it.
Information The main danger of lateral placenta previa is the possibility of severe bleeding during childbirth, as well as difficulty in the passage of the fetus through the birth canal. As for the lateral location, according to statistics, it most often occurs in women over 35.
Symptoms
The main symptoms of lateral crouching are bleeding, which can occur even as a result of a normal cough. In addition, the obstetrician may be alert to the atypical shape of the abdomen.
Recommendations for lateral presentation
- limiting physical activity;
- bed rest in the second half of pregnancy;
- if the situation worsens, experts recommend that the woman go to hospital.
With lateral presentation and no bleeding, childbirth occurs naturally. However, if a woman has had even slight discharge in recent weeks, a cesarean section is performed.
Why is it dangerous?
If at the beginning of pregnancy a presentation of 1-2 degrees was diagnosed, but until the 24-26th week of pregnancy the placenta has not changed its position, low presentation may lead to new complications.
The dangers that arise at the end of the second and beginning of the third trimester are associated with the pressure of the placenta itself and the growing fetus on the cervix. They can threaten the mother, baby or complicate the course of childbirth:
- recurrent bleeding can lead to anemia in the mother;
- anemia causes hemorrhagic shock (threat to the life of the fetus);
- Possible deterioration of blood flow due to compression of blood vessels, and this leads to fetal hypoxia;
- partial detachment of the edge of the placenta (can also cause fetal hypoxia);
- low placentation may prevent the fetal head from descending into the pelvis. As a result, an incorrect (lateral) position of the fetus is diagnosed, and breech presentation is also possible. This makes natural childbirth difficult;
- Even when the birth canal is clear, the placenta can shift during contractions during natural childbirth and make it impossible. In this case, an emergency CS is performed;
- the location of the placenta on the anterior wall of the uterus can lead to large blood losses during the delivery operation. In this case, the CS is performed according to a special algorithm, which allows the baby to be born faster, and then provide the mother with the necessary therapy.
In case of heavy or recurrent bleeding, or intrauterine fetal hypoxia, the woman remains in the hospital until delivery.
Doctors try to maintain the pregnancy until 36 weeks, while administering antispasmodics, vitamin and vascular medications to the mother, as well as drugs to accelerate the maturation of the baby’s lungs.
By 36 weeks, after assessing fetal maturity, a cesarean section is prescribed. If necessary, delivery is carried out earlier.
Low placenta previa
This is one of the safest options for placenta previa. In this case, the risk of complications and bleeding is minimal. Low location is a condition when the placenta is located less than 7 cm from the edge of the internal os at 26 weeks.
The causes of pathology differ little from those described above. In other words, in order to avoid such a fate, it is best to adhere to the right lifestyle and plan your pregnancy in advance, excluding all kinds of infections.
Information It is important to note that in rare cases the placenta may overlap the edge of the internal os, which is a serious complication and requires careful monitoring of the pregnant woman's condition.
Recommendations for low presentation
- refusal of intimate relationships;
- taking necessary medications;
- lack of physical activity;
- compliance with the rest regime.
Four degrees of low presentation
- Stage 1 - the baby's place is at least 3 cm from the edge of the internal pharynx.
- Stage 2 - the baby's place reaches the cervix, but the birth canal remains open.
- Stage 3 - the baby's place partially covers the cervix;
- Stage 4 - the baby's place completely blocks the birth canal.
The method of treatment and delivery is selected based on the degree of presentation. It is important to note that stages 3 and 4 account for only 1% of pregnant women.
Discharge due to placenta previa
Discharge during placenta previa is the main symptom indicating the development of pathology. So, depending on the type of position of the child’s seat, the allocations may be as follows:
- spotting - indicate partial passage of the placenta in which small vessels rupture. Most often, such bleeding occurs in women during the 2nd trimester and can be triggered by a simple trip to the toilet or sneezing;
- abundant - indicate that the degree of placental abruption is much wider, and therefore the number of torn vessels is greater;
- abundant with clots - may indicate the presence of infection. Requires immediate hospitalization;
- Frequent spotting indicates partial separation of the placenta, which will continue to progress slowly.
Please note that any discharge during pregnancy, especially when a diagnosis of placenta previa is made, requires immediate examination and consultation with a specialist.
Sex with placenta previa
As a rule, obstetricians recommend abstaining from sexual intercourse even for women whose pregnancy proceeds without visible pathologies. As for the diagnosis of “placenta previa,” in this case, women are not allowed to have sex for the following reasons:
- First of all, during sex, the risk of injury to the cervix increases. In this case, a hematoma is formed, which over time leads to serious complications;
- in addition, sexual arousal greatly increases the tone of the uterus and the place where the placenta is attached, as a result of which the risk of its detachment increases;
- the possibility of causing premature birth.
What not to do with low placentation
Certain features of pregnancy force a woman to more closely monitor her health. In order not to aggravate the circumstances and lead to even greater prolapse, it is necessary to follow the doctor’s recommendations.
With this diagnosis the following are contraindicated:
- sudden movements;
- excessive physical activity;
- vaginal procedures;
- lifting weights;
- stress and overwork.
It is not recommended to sit with your legs crossed, as this position interferes with normal blood circulation. You also need to lie down and get up carefully, without jerking. Even coughing and sneezing can cause bleeding. Riding on public transport is also not advisable, especially during rush hour.
Sex with low placentation is possible only in the absence of obvious symptoms and contraindications - detachment of the placental organ, pain, bleeding.
When having sex with a partner, it is important to take basic precautions:
- Maintaining hygiene. Be sure to visit the bathroom before starting intimacy;
- No sudden movements. Strong shocks can cause harm, so friction must be done gently and penetration is shallow.
- Position selection. There will be less pressure on the uterus if the woman lies on her side.
If there is a threat of miscarriage or low placental presentation, sexual intercourse is contraindicated. During this period, even masturbation and anal sex can cause serious complications due to contraction of the uterus during orgasm, which will lead to placental abruption. Therefore, you also need to masturbate with caution if there are no prerequisites for pathology.
Management of pregnancy and childbirth with placenta previa
The management of pregnancy with placenta previa depends on the following factors:
:
- gestational age;
- presence of bloody discharge from the genital tract;
- volume of bleeding.
If the pregnancy is less than 37 weeks, there is no bleeding or minor spotting, the pregnancy can be continued. The woman must be hospitalized in a hospital, where the following treatment is carried out:
:
- Strict bed rest.
- Constant supervision by medical staff.
- Daily fetal CTG monitoring.
- Vitamin therapy.
- Drugs that reduce uterine tone (Papaverine, No-shpa, Magnesia sulfate).
- Iron supplements for the prevention and treatment of anemia with monitoring of a general blood test.
- Drugs to improve uteroplacental blood flow (Actovegin).
important In case of placenta previa, delivery is carried out by planned cesarean section at 37-38 weeks of pregnancy. If there is heavy bleeding from the genital tract, pregnancy is urgently terminated surgically, regardless of gestational age.
If bleeding does not stop during a cesarean section, ligation of large vessels (uterine and internal iliac arteries) is performed. If there is no effect from the dressing, extirpation (removal) of the uterus is performed.
Oblique or transverse presentation
The presentation of the fetus during pregnancy can change repeatedly. It depends on the activity of the child and the anatomical structure of the mother's body. With an oblique presentation, there is a possibility that the baby will change position during active labor, but doctors recommend that the woman not take risks and give birth by cesarean section.
If the fetus is transversely presented, then natural delivery is impossible. In this case, the axis of the child and the axis of the woman’s uterus intersect at a right (90 degrees) angle, and the largest anatomical parts of the fetus are located above the crests (edges) of the ilium. In very rare cases, with the help of doctors, the child can be turned around, but this usually leads to injury to the fetus.