The marginal attachment of the umbilical cord to the placenta is a relatively rare cause for concern for the expectant mother. However, such an anomaly in the fixation of the umbilical cord in some cases (especially if complicated by other problems) can cause heavy bleeding during childbirth and fetal death. To reduce the risks, a pregnant woman may be advised to deliver by caesarean section.
Tricky loop
One of the most frightening cases for all expectant mothers is the umbilical cord entwining the baby.
Two factors lead to this problem: increased motor activity of the unborn baby and increased length of the umbilical cord. Hyperactivity can be caused by polyhydramnios and increased adrenaline levels in the blood due to stress. The reasons for excessive elongation of the umbilical cord have not yet been precisely established, but a genetic predisposition is clearly visible.
https://www.youtube.com/watch?v=ytaboutru
If the mother had a long umbilical cord, then it is very likely that her daughter will have the same. It is almost impossible to determine the length of the umbilical cord during pregnancy, since it is “coiled” in the tight space between the baby’s body and the wall of the uterus. It is possible to find out about its size only after the fact.
Fact! The umbilical cord consists of 3 vessels: arterial blood flows through one from mother to fetus, and through the other two, the baby’s venous blood removes waste products.
How the umbilical cord attaches to the placenta
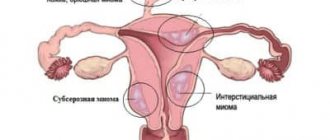
The normal option for fixation is the departure of the umbilical cord from the center of the child's place. Anomalies are called lateral, marginal, shell attachment of the “cord”. It is best to examine them in the 2nd trimester using ultrasound diagnostics, when the placenta is on the anterior or anterolateral uterine wall.
When it is localized on the posterior wall, it may be difficult to determine. The use of color Dopplerography makes it possible to recognize the exact variant of the pathological exit of the cord to the child's place.
Let's consider several types of abnormal fixation of the umbilical “cord”:
- Central - in the middle of the inner surface of the placenta. Occurs in 9 out of 10 pregnancies and is considered a normal option.
- Lateral (eccentric) - not in the center, but on the side of the embryonic organ, closer to its edge.
- Marginal - from the edge of the placenta. The umbilical arteries and vein pass to the child's place close to its periphery.
- Tunicale (pleated) - attached to the membranes of the fetus without reaching the placenta. The vessels of the umbilical cord are located between the membranes.
Norm
A normal, healthy umbilical cord has three vessels: two arteries and one vein. Through a vein, the baby receives maternal blood enriched with oxygen, vitamins, and microelements that are necessary for the growth and development of the fetus. Through the arteries back to the placenta, and from there, the products of the child’s metabolism (creatine, carbon dioxide, urea, and so on) are removed into the mother’s body.
Normally, the umbilical cord is about 50-70 centimeters long. A longer umbilical cord creates a risk of entanglement and suffocation of the fetus during active movements. A shorter one limits the baby’s movements and also poses a danger during childbirth: its tension can provoke placental abruption, bleeding and acute fetal hypoxia.
One side of the umbilical cord is adjacent to the anterior abdominal wall of the fetus, and the other is adjacent to the placenta. Central attachment of the umbilical cord is considered normal. With it, the umbilical cord is attached to.
Umbilical cord entanglement during pregnancy
Often a woman hears that the child is entangled in the umbilical cord. This leads many expectant mothers into a state of panic. But do not be alarmed; in most cases, this pathology does not pose a threat to the health of the fetus. Most often seen during pregnancy is the umbilical cord around the baby's neck.
Why does the umbilical cord wrap around the baby? Experts point to the following reasons for this condition:
- The length of the umbilical cord is more than 70 cm. In this case, umbilical cord loops can form around the fetal body.
- Hypoxia. In the event of a deficiency of oxygen supplied by the mother, the child may begin to move quite a lot and, thus, falls into the formed loop.
- Polyhydramnios. With a large amount of amniotic fluid, both the fetus and the umbilical cord float freely. This increases the risk of getting entangled in the umbilical cord.
But all of the above conditions do not always contribute to umbilical cord entanglement during pregnancy. In addition, sometimes this can happen completely by accident.
Possible danger
Until the 37th week of pregnancy, doctors do not focus on this condition. Until this time, it may appear and disappear more than once. The danger comes from double or multiple tight entanglements around the baby’s neck.
In this condition, the fetus experiences hypoxia. Lack of oxygen leads to disturbances in intrauterine development. In the fetal body, metabolic processes are disrupted, the nervous system is damaged, and adaptive capabilities are reduced.
The degree of damaging effects of oxygen deficiency depends on the duration of hypoxia. In addition, strong tension of the umbilical cord often leads to premature placental abruption and premature birth.
During pregnancy, the umbilical cord around the baby's neck or other parts of the body is diagnosed by ultrasound.
What to do
If such a pathology is detected, the expectant mother should listen to the doctors and undergo all examinations on time. Thanks to them, it is possible to prevent the dangerous consequences of this condition.
If necessary, the doctor can prescribe special medications to the woman that support uteroplacental circulation. If repeated entanglement of the baby's neck is diagnosed, a cesarean section is usually performed at 38-39 weeks of pregnancy.
There is nothing wrong with the entanglement itself. Ultrasound specialists know: almost 80% of all unborn babies have an entwined umbilical cord. This does not lead to disturbances in the intrauterine state of the fetus. While in the uterus, the baby still does not breathe through the lungs, so squeezing the neck is not at all dangerous for him.
However, only a fifth of babies are born with the umbilical cord entwined. The rest “untie themselves” on their own. Therefore, ultrasound is only an additional diagnostic tool - well, a nodule and nothing more.
DETAILS: The umbilical cord has 2 vessels
Problems can arise when blood flow is disrupted due to tension or compression of the umbilical cord due to repeated or tight entanglement. This is about 1% of all “entwined” babies.
- Cardiotocography allows you to determine the baby’s heart rate, his reaction to his own movements (during pregnancy) and to an increase in the tone of the uterus (during childbirth). This will allow you to accurately determine how well the baby is feeling at the moment.
- Doppler measurements will help diagnose the speed of blood flow in various vessels of the uterus and placenta.
Diagnostics
Complete placenta previa is diagnosed, usually by ultrasound, but can also be detected during a routine gynecological examination.
Observation and treatment
As such, there is no medical treatment for complete placenta previa. All that doctors can do is to carefully monitor the condition of the expectant mother and keep her other diseases under control, since many factors can provoke complications of the pathology. If a woman is not bothered by bleeding, then observation can be carried out on an outpatient basis.
Otherwise, from 24 weeks until the very moment of birth, she will have to stay in the hospital. Typically, in such a situation, the pregnant woman is prescribed strict bed rest, restorative medications, iron supplements (for anemia), as well as medications to relieve uterine tone and improve blood supply in order to prevent fetal hypoxia
They always try to prolong pregnancy as long as possible, at least until the moment when the child can be saved and delivered.
Behavior rules
A few simple rules will help you alleviate your condition and avoid irreparable complications.
- Minimum physical activity. You cannot understand the severity and make sudden movements that displace the uterus, as this is fraught with placental abruption. Spend time in the fresh air more often, but if peace is prescribed, then it is advisable to exclude walks, but you can sit with a book in the park;
- Try not to worry and completely avoid intimacy, as all this leads to uterine tone and can cause bleeding;
- Eat right, we already talked about this above;
- If possible, visit crowded places as little as possible so as not to be at risk of becoming infected with something. In addition, you may be accidentally pushed in a crowd;
- Don't take long trips. It will be better if, if bleeding occurs, you have the opportunity to easily get to your doctor. If you are going somewhere, be sure to take an exchange card with pathology data.
Peculiarities of childbirth with velamentous umbilical cord attachment
The umbilical wound requires attention and care, but you should not concentrate too much on it. As a rule, the belly button heals quickly and without problems. To treat it in maternity hospitals “the old fashioned way” they use a thick solution of potassium permanganate; pediatricians recommend brilliant green.
- It is important to keep the umbilical cord clean and dry. After bathing or washing, dry it with a dry cloth. Give your baby's skin the opportunity to breathe - this will not only speed up the healing of the navel, but also prevent the appearance of diaper rash. Dress your baby in clothes made from natural fabrics. Cotton does not create a greenhouse effect and promotes wound healing.
- Bloody discharge in the navel area can be observed until it has completely healed in the newborn - there is nothing wrong with that. The diagnosis of “untied navel,” which frightened great-grandmothers, does not exist in medicine. You should contact your pediatrician if symptoms of inflammation appear: redness, swelling, unpleasant odor, purulent discharge.
Fact! The veins and arteries that ran inside the umbilical cord become blocked and pulled inward after birth. Gradually, the navel becomes small and convex. Over time, the umbilical ring will narrow completely, and it will take the same shape as that of an adult.
Anomalies in obstetrics include any structural changes in the umbilical cord: changes in the number of vessels, the presence of blood clots, insufficient or excessive length, as well as the presence of nodes, cysts and variants of umbilical cord attachment that are not considered normal.
There are several types of abnormal attachment of the umbilical cord to the placenta:
- Regional. With this attachment, the cord docks with the placenta along its peripheral edge.
- Shell. With this attachment, the umbilical cord connects to the membranes.
With marginal attachment, the vein and two arteries that provide the child’s vital functions are attached too close to the edge of the “child’s place.” This type of attachment does not pose any great danger; in most cases it does not affect pregnancy in any way. Doctors' opinions regarding marginal attachment are usually similar: a woman can give birth naturally. Caesarean section, if there are no other indications for it, is not required.
The only threat that the marginal (lateral) attachment of the umbilical cord can create is incorrect actions of the obstetric team during childbirth. At birth, doctors sometimes help by tugging on the umbilical cord. In the case of marginal attachment, such actions can lead to separation of the cord, and the placenta will have to be removed manually.
Shell (or shell) attachment of the cord to the umbilical cord in the womb is quite rare - in approximately 1-1.5% of cases. The cord itself is adjacent to the membranes, which are distant from the placenta. Over this same distance, the umbilical vessels are completely unprotected; they approach the placental disc directly. This is a more dangerous abnormality of the placenta than marginal attachment.
With the membrane type, the child quite often develops developmental delay syndrome (due to insufficient nutrition and oxygen supply during gestation). Such babies are often born low birth weight. Chronic hypoxia, to which babies are exposed in the womb, often leads to a delay in not only physical but also mental development, as well as to disorders of the central nervous system.
In almost 9% of cases of detection of the umbilical cord attachment, the child is diagnosed with developmental defects: absence of the esophagus, cleft palate, congenital dislocation of the hip, abnormal head shape, and so on.
Such attachment is very dangerous not even during pregnancy, but at the time of childbirth. If the integrity of the fetal bladder is damaged, the umbilical cord is severed, which leads to bleeding and can result in the death of the fetus. Doctors try to deliver such an abnormal umbilical cord by cesarean section to minimize risks.
DETAILS: What to drink to improve cerebral circulation
These two main types of umbilical cord abnormalities are also called eccentric attachments. If the cord is attached to the umbilical cord in the central part, but is slightly shifted in any direction, they speak of a paracentral attachment, which is considered a normal variant.
Marginal deviation means fixation is not in the central zone, but in the peripheral zone. The umbilical arteries and vein enter the child's place too close to the very edge. Such an anomaly usually does not threaten the normal course of pregnancy or childbirth, being considered a feature of a specific period of gestation.
Experts say that marginal discharge is not an indication for a cesarean section: natural delivery is carried out. This attachment does not increase the risk of complications for the mother or baby.
Such an anomaly in the origin of the cord is accompanied by a high risk of damage to the umbilical vessels, followed by fetal bleeding and rapid death of the child. To prevent their rupture and death of the baby, timely recognition of the pathological variant of the “cord” exit is necessary.
Natural childbirth requires good specialist skills and constant monitoring of the baby’s condition due to the high risk of death of the mother and baby. Childbirth should be quick and gentle. Sometimes the doctor can feel the pulsating arteries. The doctor opens the amniotic sac in a place so that it is distant from the vascular zone.
If there is a rupture of the membranes with blood vessels, a pedunculated rotation and extraction of the fetus are used. When the head is in the cavity or pelvic outlet, obstetric forceps are used. These benefits can only be applied when the child is alive.
On many forums, expectant mothers ask themselves the question: how to get rid of the pathological discharge of the umbilical cord. During gestation, it is impossible to eliminate the anomaly: it cannot be treated either with medication or surgery.
There are no exercises to correct the abnormal attachment of the cord between mother and baby. The main goal of the specialist is to prevent the rupture of the membranes and the subsequent death of the baby at birth.
Treatment
Unfortunately, medicine today cannot offer a single method of treating abnormal attachment of the umbilical cord to the placenta. During pregnancy, pathology cannot be eliminated with medications, exercises, diets, or surgery. There is no way to influence the location of the umbilical cord. For this reason, doctors, when diagnosing deviations in the location of the umbilical cord, adopt the tactic of wait and watch.
A woman with marginal or membrane attachment is recommended to visit the antenatal clinic more often, have an ultrasound scan more often, and at a later date - CTG to make sure that the child does not experience hypoxia. If signs are detected that indicate fetal distress (impaired condition and heartbeat according to CTG, developmental delay on ultrasound), early delivery can be carried out: by cesarean section with a membrane or naturally with a marginal attachment.
If the gestational age is not sufficient for doctors to be confident in the viability of the fetus (not 36 weeks), the woman is hospitalized in a hospital, where standard maintenance therapy is carried out in such cases. These are antispasmodics to relieve symptoms of uterine tone, vitamins and drugs that improve uteroplacental blood flow.
A diagnosis of “abnormal umbilical cord attachment” based on the edge or shell principle means not only that the woman will receive a lot of attention from the attending physician, but also that she will have to go to the maternity hospital earlier than others. At 37-38 weeks, they try to hospitalize such patients in order to decide on delivery tactics. With membrane attachment, it is important to prevent spontaneous rupture of the membranes, and therefore a cesarean section is performed in advance, before the onset of independent labor.
There is good news: in most cases, with abnormal attachment, if it is not accompanied by fetal malformations and genetic pathologies, as well as other anomalies of the umbilical cord and placenta, women safely give birth (either themselves or with the help of surgeons) to completely normal children, and the postpartum period proceeds without features. It is only important to follow all the doctor’s recommendations while carrying the baby.
For information on hypoxia and fetal umbilical cord entanglement, see the following video.
medical reviewer, psychosomatics specialist, mother of 4 children
The placenta is one of the most important organs that appears during pregnancy. It is thanks to it that the child’s nutrition and breathing, as well as the removal of metabolic products, are possible. In addition, placental tissue produces hormones necessary for the normal course and development of pregnancy.
Placenta previa is a pathology caused by the placenta being attached and developing in the wrong place.
Normally, it is located on the bottom of the uterus , in the part that is least susceptible to changes. If the placenta is located on the side of the pharynx , then they speak of presentation. It can be partial, when the uterine os is covered by the placenta by 1/3 or 2/3, or complete, when the center of the placenta is compatible with the uterine os. According to statistics, complete is almost 5 times less common than incomplete.
In the case of incomplete presentation (lateral or marginal), there is hope that the placenta will independently move to the correct area closer to the day of birth. In the case of complete presentation, unfortunately, this option is completely excluded.
What is the marginal attachment of the umbilical cord?
The umbilical cord can attach to the placenta in different ways. Most often - in the center, in other cases - on the side. Sometimes the umbilical cord is attached to the membranes without reaching the placenta itself. In these cases, the vessels of the umbilical cord approach it between the membranes.
Such attachment of an embryonic organ is also normal, but carries some risk of placental insufficiency. In this case, pregnancy will require a little closer monitoring.
Causes
The reason for the marginal attachment of the umbilical cord is anomalies in the development of the umbilical cord even at the stage of placenta formation. Most often, this anomaly appears in women who are carrying their first child, as well as in expectant mothers who became pregnant at a fairly young age (from 18 to 23 years).
Not least among the causes of abnormal attachment of the umbilical cord are pregnancy pathologies: polyhydramnios and oligohydramnios, placenta previa, abnormal position of the fetus in the uterus. Most often, the marginal attachment is combined with other pathologies of the umbilical cord: with nodes, a violation of the arrangement of blood vessels inside.
The reasons for the membrane attachment of the umbilical cord are still not completely clear, but observations show that most often the pathology is characteristic of women who are carrying twins or triplets, as well as women who give birth a lot and often.
Among the causes of abnormal membrane (pleated) attachment, genetic pathologies of the fetus are also considered. Very often, with Down syndrome, the child develops a membrane attachment of the umbilical cord.
Experts consider the main cause of pathological attachment to be a primary defect in the implantation of the umbilical cord, when it is not localized in the area of the trophoblast that forms the baby's place.
Risk factors for anomalies are:
- First pregnancy;
- Young age, not exceeding 25 years.
- Excessive physical activity combined with a forced vertical position of the body.
- Obstetric factors - oligohydramnios, polyhydramnios, weight, position or presentation.
Most often, abnormal fixation of the umbilical cord occurs simultaneously with several variants of cord pathology - true nodes, non-spiral arrangement of vessels.
Associated genera
If, after carrying out the entire complex of examinations, it is determined that the baby feels satisfactory, then the fact that the umbilical cord is entwined is not an indication for surgical delivery. A woman is referred for a cesarean section only if there are signs of oxygen deficiency in the fetus.
Special tactics for managing childbirth are also required when entanglement is combined with other difficulties: age over 35 years, infertility treatment, use of assisted reproductive technologies for conception, breech presentation.
https://www.youtube.com/watch?v=ytpressru
DETAILS: Hypoxemia index is normal
In other situations, a baby with entanglement (both single and multiple) is taken in the usual way. During childbirth, cardiotocography is used, which allows you to monitor the number of heartbeats, or listen to the fetal heartbeat using a stethoscope.
In rare cases, repeated entanglement can cause certain difficulties: a short umbilical cord tied in knots, stretching with each contraction, can lead to premature placental abruption, which leads to the need for emergency surgical delivery.
What is the danger of diagnosis?
The marginal variant of the exit of the umbilical cord is not considered a serious condition. Doctors pay attention to such localization of the “cord” attachment in the case when the umbilical cord is located at a distance not exceeding half the radius of the child’s seat from the edge. This situation causes the development of obstetric complications.
The shell version poses a much greater threat. The disorder is more typical for multiple pregnancies. The vessels are located between the membranes, are not covered with Vartan jelly, and fibrous tissue is also less developed there. For this reason, they may not be protected from damage during childbirth.
When the arteries and veins are located in the lower segment of the fetal bladder, rupture of the membranes leads to bleeding. The baby's amniotic fluid compresses the blood vessels, leading to massive blood loss in the baby.
When the area of the membranes passes over the internal os of the cervix, located at the bottom of the presenting part of the baby, a diagnosis of vasa previa is made. This is a variant of the weaving type of “cord” departure.
The pathology is accompanied by rupture of amniotic fluid with bleeding. An emergency delivery is required. When a baby is born with moderate or severe anemia and hypoxia, blood products are transfused immediately after birth.
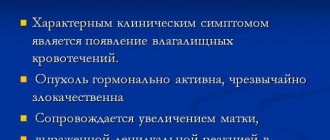
Symptoms and complications
Vaginal bleeding is a complication of placenta previa and its main symptom. In the case of complete presentation, heavy bleeding begins already in the second trimester and can occur periodically until childbirth.
Why does bleeding occur with placenta previa? In order to answer this question, you need to understand how the placental tissue is attached to the body of the uterus.
Placental tissue consists of villi - formations filled with conducting vessels. Some villi grow together with the uterus, others are immersed in the mother’s blood, which fills the so-called intervillous space (thickening of the endometrium in the place where the placenta is attached). Blood enters this space from small arterial vessels, the walls of which are partially destroyed by enzymes secreted by placental villi.
This entire complex mechanism works to ensure exchange between the organisms of mother and child: nutrients and oxygen come from the mother’s blood, and the placenta removes waste products from the fetus.
The child receives nutrition from the placenta through the umbilical cord, namely two arteries and a vein passing through it.
So, we see that the placenta literally fuses with the uterus . Time passes, the fetus develops, and the uterus increases in volume: this is especially noticeable in its lower part, where the pharynx is located, that is, exactly where the placenta is attached in the case of central presentation. Since the placental tissue is low-elastic, it “does not have time” to stretch after the rapidly enlarging uterus.
Partial placental abruption occurs . The connection is broken, and the vessels begin to bleed into the uterine cavity, pouring out from the genital tract with profuse bleeding, followed by spotting.
Usually, the first time this happens is when the woman is at rest or sleeping at night. As a rule, there is no pain during bleeding - this distinguishes it from bleeding during self-termination of pregnancy, when cramping pain in the lower abdomen is possible.
Closer to 30 weeks, bleeding can be caused by sex , other physical activity, or even an examination in a gynecological chair.
Divide in two
In order for the blood the newborn needs to flow from the placenta into his circulatory system, the obstetrician places the baby on a sterile tray placed at the level of the mother’s body. After the pulsation stops, the umbilical cord is cut (usually 1-3 minutes after birth).
Maintaining a connection with the mother for a longer period of time is not advisable: the baby may develop erythremia, a condition in which the baby has “too much” blood, which can cause increased bleeding. The remaining fragment of the umbilical cord, 2-5 cm long, wrinkles, darkens and falls off in about a week.
Anatomy of the iliocostalis dorsi muscle
The element belongs to the deep dorsal muscles. It starts from the iliac crest, the inner side of the superficial plate of the thoracolumbar fascia. It passes sideways and upwards and forms a kind of teeth at the end. Their place of attachment by thin tendons is the 8–9 lower ribs.
Innervation comes from the dorsal branches of the spinal nerve branches of the lower back. Blood supply is provided by the posterior intercostal and lumbar arteries.
Life source
Until recently, the placenta (placenta and umbilical cord with blood remaining in the vessels) was sent for “disposal.” Today in Ukraine, preservation (cryopreservation) of umbilical cord blood cells is quite common.
This is a unique source of stem cells designed to restore and regenerate the human body. Their benefits have not yet been fully studied, but it has been proven that the cells will help save the life of a child who is seriously ill.
Sometimes specialists use stem cells obtained from the umbilical cord of a newborn for his close relatives: there is a high probability that they will be suitable for the parents, brothers or sisters of the baby.
The cord blood collection procedure itself does not cause any harm to either the mother or the baby. It is absolutely painless and safe. The collected blood is frozen and stored in a special cord blood bank.
{social}