In the first year of life, intensive motor development occurs, which contributes to the maturation of the cerebral cortex. Therefore, the more you engage with your baby, the more chances you have of raising a child prodigy. You should take care of the timely stimulation of emotional communication, the development of visual perception, auditory perception and understanding of spoken speech.
In the first month
life, the baby’s flexor muscles are still in high tone, and his movements are limited. Only in the third month does muscle tension decrease and their development begins, which, however, occurs unevenly. First, the muscles of the neck become mature. This is manifested in the baby’s ability, lying on his stomach, to lift and hold his head for a short time. The muscles of the trunk, legs and arms gradually reach their functional maturity. At this time, the baby is already reacting to sound by turning his head, and also makes random isolated flexions and extensions of his arms and legs while lying on his back.
Two month old baby
still continues to lie curled up, as if in the womb. His muscles twitch involuntarily from time to time. The legs cannot withstand any load. His hands are tightly clenched into fists, he cannot yet hold a rattle, but he is already able to hold his head tightly, turn it freely, and when laying it on his stomach, lean on his forearms and vigorously move first one or the other leg.
By the beginning of the third month
The child's limbs constantly relax. He raises his head 45° and shakes it when someone supports him in a sitting position. Involuntary muscle twitching is observed less frequently. The baby's fists are partially open, he is actively “threshing” with his hands. By the end of the third month, he is already trying to reach out and grab something. The baby grasps an object that touches his palm or fingers, squeezes and unclenches toys or other things that you put in his hands, and follows the movements of his hand.
At the end of the third
- at the beginning of the fourth month, the child already begins to raise his head from a position lying on his back, tries to roll over from his back to his side, and while lying on his stomach, rests firmly on his elbows and forearms and even rises.
Lying on his back, the child is able to look at his hands for a long time. If you give him a rattle, he shakes it with pleasure.
At four months
the child lies on his stomach, resting on his forearms, bent at a right angle. The baby’s limbs can already straighten freely: he shakes a rattle placed in his hand, makes a “bicycle” and other movements in a free style. Lying on his stomach, he raises his head and examines the situation. Can't stand on his legs for long. Holds his head straight when someone supports him in an upright position. Rolls over from back to side.
At 4.5 months, while lying on his back, seeing an object, he reaches out to it, grabs it with both hands and pulls it into his mouth.
By the beginning of the fifth month
The child already knows a lot. Lying on his stomach, the baby freely raises his torso, resting on the palms of his outstretched arms, easily and
quickly rolls over from back to stomach. He moves his legs smoothly and steadily (“dances”) when his body is held. Coordination of movements also improves. The child directs his hands exactly to the object that interests him. At first he takes the toy with both hands, then tries to hold it with one. The child now not only holds the toy tightly, but examines it carefully and intently. At five months, the baby stands confidently with support and sits, leaning on his hands. Resting on his elbows, easily turning over from his stomach to his back. Reaches for objects with both hands. Collects hanging toys. He plays with clothes with interest and grabs his mother's breast.
At six months
The child accurately grasps the necessary objects, transfers them from one hand to another, touches and strokes the surface of the toy with his finger. During this period, the baby can already maintain a sitting position, holding tightly to the adult’s fingers; with the help of an adult, sit down, leaning on straightened arms and raising your torso; sit leaning on a pillow. He stands up, holding onto the support. Rolls over from stomach to back and back. Rocks while lying on his stomach (“airplane”). Raises itself, lifting the chest and part of the abdomen from the floor. Kicks. Stretches his neck to see better.
A six-month-old child, lying on his stomach, is able to lean on one hand, reaching for a toy with the other. While in the playpen, he can already crawl to the object that interests him. With the right and left hands equally active, the baby takes only one of the two outstretched toys, but if he puts another toy in his unoccupied hand, he will hold that one too. Lying on his back, the baby enthusiastically plays with his legs, while his head is raised. He intelligently moves toys from hand to hand and pushes them into his mouth. Starts playing with cubes.
By the end of the seventh month
The baby is already crawling well, standing strong and straight with the support of an adult. Having pulled himself up by the fingers of an adult or by the walls of the crib, he can already sit down and sits - although still uncertainly.
If a child has a toy in his hands, he no longer just waves it chaotically, but, holding it, rotates his hand, purposefully hits the toy against surrounding objects, moves it from hand to hand, and examines it carefully. When lying on his stomach, he can support his own weight on one hand and reach for an object with the other.
At 7-8 months
the child gets on all fours, can sit up from a lying position on his back, and can sit up and straighten up when sitting down.
Eight month old
the child sits steadily, tries to stand up, holding onto the walls of the playpen, stands with support from the hands, crawls. He examines toys, people and randomly moves his gaze from one object to another.
At nine months
The child can stand up from a sitting position by holding onto the railings of the crib. By the end of the ninth month, the child confidently and quickly crawls on his stomach forward and around himself, sits for a long time, with support from both hands (sometimes one), stands well on the entire foot and can even lift one or the other leg.
Ten month old baby
able to crawl on hands and knees. At the same age he begins to stand. Can grasp an object with 3-4 fingers. Holding one hand on a support or the hand of an adult, the baby takes steps towards the toy and sits independently on a chair.
At eleven months
The child walks for a long time with support from one hand and stands independently. At the age of 9-11.5 months, the baby plays with both hands, transfers an object from hand to hand. The thumb and the tips of the fingers are involved in grasping an object.
At 12 months
The baby is already confidently standing on his feet, walking with the support of one hand or independently.
Possible deviations in motor development
First month: being in an upright position, the child cannot hold his head for a short period of time.
Two months: lying on the back, unable to lift and hold the head. The movements of the arms and legs are chaotic and asymmetrical.
Three months: When lying on the stomach, the child is unable to hold his head up for a short time. Doesn't hold the head in a vertical position. While awake, does not examine his hands.
Four months: when lying on the stomach, does not lean on the forearms and does not lift the torso. If a baby lying on his back is lifted, held under the armpits, his head leans powerlessly back. When the baby is in an upright position and supported under the armpits, he does not rest his toes. Five months: When lifted by the arms from a supine position, the baby cannot hold his head firmly. Doesn't know how to confidently roll over from stomach to back.
Six months: unable to reach out and grab a toy from a prone position. Held under the arms in a vertical position, does not move his legs, does not “dance”.
Seven months: When supported by the hands, the baby does not try to sit up from a lying position.
Eight months: does not crawl back. Do not stand even for a short time with hand support. Unable to hold a button or other small object between the thumb and index finger.
Nine months: lying on the stomach, does not turn around its axis, does not try to crawl forward. He sits unsteadily and in this position cannot turn around his axis. Cannot drink from a cup independently.
Eleven months: does not crawl on all fours. Unable to sit with legs straight out. While holding onto a support, the child moves poorly or does not move at all. Twelve months: does not walk with hand support.
The child develops from two starting positions:
1. Lying on your back 2. Lying on your stomach.
Now we will look at the child’s motor development in detail, month by month. In this part of the article, the concepts of facial and occipital limbs will be used. Let's look at them first and give them an explanation. Facial limb - an arm or leg towards which the child’s face is turned (usually a supporting limb). Occipital limb - an arm or leg lying at the back of the child's head. It must be remembered that when assessing the motor development of a child in the first year of life, there are several axioms:
1. The main motor task of a child is the transition from a horizontal to a vertical position. 2. Any coordinated skill is formed from top to bottom: head-torso-arms-legs. Until the head is coordinated, there can be no talk of any coordination of arms and legs. 3. Inside the body there is a certain coordinate system, relative to which all movements are assessed - this is the longitudinal axis of the body. We obtain 4.99% of information about the child’s motor and functional state by assessing the child’s resting posture. First, we look at the position of the head, then the torso, then we evaluate the position of the head relative to the torso, then we look at the position of the limbs relative to the torso, and then we evaluate the whole thing. Moreover, such a thorough assessment must be carried out from two positions: lying on the back and lying on the stomach.
For the development of a child from a prone position, the center of gravity, or more precisely, its location, is of great importance. In a newborn baby, the center of gravity is at the upper edge of the sternum (a very large head relative to the body). In an adult, it is located in the pelvis. What influences the gradual downward movement of the center of gravity? Weight gain. As the child grows and gains weight, the center of gravity shifts downwards and, accordingly, the support area decreases.
0-1 month:
I.P. lying on the back: the head is turned to the side, the torso is compensatory bent, the front arm is half-bent in front of the face, the occipital arm is half-bent upward, the lower limbs are passively bent in all joints. This is the so-called “half-fencer” pose. The “fencer” pose is pathological, therefore we call this physiological pose for a child of this age the “half-fencer” pose (since it resembles a fencer in the main stance). When turning the head, the hands change their position (due to reflexes of oral automatism). Does not fixate gaze (0 months). Capturing an object with a “gaze”, i.e. wants to pick up an object with his gaze, but cannot with his hand (end of the first month). I.P. lying on the stomach: the head is compensatory turned to the side, the axis of the body is compensatory bent, the arms are brought to the body and maximally bent at the elbow joints, the hands are clenched into fists, the legs are bent in the sagittal plane (tucked under oneself). At the same time, the hip-femoral joints should not lie on the surface of the support. If the legs are in the “frog” position (spread out), then this is considered a sign of muscle hypotonia, and a birth injury of the cervical spine should be looked for.
2 months:
I.P. lying on your back: the head and torso are already located along the longitudinal axis, the arms are in the initial phase of the Moro reflex (to the sides, palms forward), the legs are in passive-active flexion (the active component is just beginning to appear). If the torso is deviated from the longitudinal axis, we may suspect the initial phase of scoliosis. I.P. lying on the stomach: the head and torso are along the longitudinal axis, the center of gravity is shifted to the middle of the sternum, the arms rest on the forearms, the legs are bent in a plane intermediate between the frontal and sagittal (the so-called flexion with abduction of 45 degrees).
3 months:
I.P. lying on your back: head and torso along the longitudinal axis, arms also “find” the longitudinal axis, legs passively-actively bent (the active component of flexion increases). He puts both hands in his mouth and examines his body with his hands - chest and stomach to the navel. Grabbing an object is not purposeful. What does it look like in practice to find the longitudinal axis with your hands? The baby begins to put his hands in his mouth. And the reason for this is the basic muscle stereotype of movement, which also relates to the reflexes of oral automatism. Therefore, we must give recommendations to the mother - not to “remove” her hands from her mouth, as this is a necessary stage of his motor development. I.P. head lying on the stomach, torso along the longitudinal axis, center of gravity in the middle of the sternum, arms resting on the forearms, legs bent in the frontal plane (flexion with abduction), hip joints rest on the surface of the support (this is the so-called Lawrence position 1). This position contributes to the correct and timely formation of the head of the hip joint.
4 months:
I.P. lying on his back with his head and torso along the longitudinal axis, the child begins to move his arm into the space of the “opposite” arm, his legs in a position of passive-active flexion (the active component continues to grow). Legs are bent at the joints 95°, feet close to each other; the child can turn on his side and back; examines his body with his hands below the navel. Gradually, the child begins to explore the space of the opposite one with one hand. Leaning his heels on the surface, raises the pelvis and moves it in different directions; If the placement of the arm occurred before 4 months (especially if this position is fixed), then some kind of neurological pathology can be suspected. I.P. lying on your stomach, support on your forearms, wrist joints and stomach; the child can raise one hand and reach for the toy; grip with the fourth and fifth fingers of the hand (monkey).
5 months:
I.P. head lying on the back, torso along the longitudinal axis, pulls hands into mouth, sucks them, actively moves both arms in opposite directions, legs - the passive component of flexion is completely absent, legs are actively bent in all joints up to 90 degrees. Examines his body with his hands up to his knees, knows how to transfer a toy from one hand to another. I.P. lying on the stomach with the head and torso along the longitudinal axis, the center of gravity shifts closer to the navel. The arms rest on the hands or wrist joints, the legs are actively bent to 90 degrees, the support is on the shins - the child periodically takes a standing position on all fours. The pelvis remains free. Grabs objects with 2-5 fingers.
6 months:
I.P. Lying on your back, your butt is lifted off the surface of the table, your legs find the longitudinal axis. How? The child pulls them into his mouth and sucks. If a child before 6 months crosses his legs and fixes them in this position, this is a sign of neurological pathology. The higher the crossover level, the worse the prognosis. I.P. lying on your stomach with your head and torso along the longitudinal axis, the center of gravity is at the level of the navel. Reliance on the hands and shins, the pelvis finds a fulcrum - thus, the child sits down. Standing on all fours, can raise one arm parallel to the floor; grasping an object with 2-3 fingers. A healthy child, provided his normal development, sits down from a standing position on all fours, by turning on his side or turning on his stomach. This is considered physiological. If a child by this age is not yet sitting, provided that he is otherwise not lagging behind in motor development (gets on all fours, crawls, stands up), then this can be considered a variant of the norm. The child has the right to sit down last (for example, he was walking, fell on his butt - sat down and learned to sit). Forcibly placing a child until he is ready for this is strictly prohibited. The load on the spine in a sitting position is a hundred times greater than in a standing position. An example of this is the treatment of compression fractures. It is allowed to adopt a “semi-lying” position for a short time (in case of feeding or in a stroller). But if we place a child in pillows and do this regularly, then in the future we will have problems with posture.
7 months:
I.P. lying on the back with the head, torso along the longitudinal axis, hands in the mouth or brought into the space of the opposite hand, legs in the mouth or brought into the space of the opposite leg. Thus, the arm and leg are turned to the side, and the child performs a coordinated (!) turn to the side (1st phase of rotation) and to the stomach (2nd phase). If a child turns onto his side and stomach before 7 months, then such a turn cannot yet be considered coordinated and independent, and is considered as an isolated case (or the mother actively helps him). “Garden gnome” pose (sitting on its side with support on a straight arm) photo 4; knows how to turn from stomach to back; can grasp objects in both hands at the same time. I.P. lying on his stomach, standing confidently on all fours, swaying in all directions; can crawl on its bellies (on its elbows, while its legs passively drag behind).
Photo 4
7-8 months:
I.P. Lying on his stomach, the child actively learns to crawl, and begins to do this after 6 months. At first, the child exhibits a symmetrical pattern of movement (the right arm and right leg move forward simultaneously). Then he changes his movement pattern to the opposite - right hand - left leg. As soon as a change in the movement pattern occurs, this is the trigger for verticalization, and we can “predict” with an accuracy of a few days that the child will soon stand on his feet. Raising your arm while on all fours more than 120°; grasping an object flat with the first and second fingers (tweezers grip).
9-10 months:
I.P. Lying on his stomach, the child crawls to a support and stands up. Up to two years of age, a child should normally stand up by turning on his side (this is the so-called mid-physiological standing up), only adults who “don’t mind their back” get up “with a jerk” from a lying position to a sitting and standing position.
11-12 months:
I.P. lying on his stomach, the child begins to walk, and the motor pattern of walking is symmetrical in nature - at the same time the right arm and right leg “walk” forward (he walks, waddling like a bear cub). This can be felt when you place your “helping” hands under the child’s palms - the arm and leg of the same name “go” forward. Very quickly this motor stereotype changes to asymmetrical. Freely stands at the support from a position on all fours; holding onto a support, he takes steps to the side or, by releasing one hand, he can turn around; walks with support; grasping an object in a circular manner with the first and second fingers (ring grip).
12-14 months:
Walks without support.
ADDITIONAL INFORMATION
Recommendations for teaching your baby to walk independently: The mother stands behind the baby, her hands are placed under the baby’s palms (the baby’s arms are bent at the elbows at an angle of 90 degrees). First, the baby leans alternately on one and the other hand, as soon as the mother feels that the baby has begun to lean on only one hand - that’s it, the “helping” hands can be removed! Never give your hands “from above”, never use walkers and other devices that make life easier for mothers. If the child learned to walk in a walker, stirrups, etc. - he simply loses the skill of coordinated movements (this will be especially noticeable when such children fall - they are completely unable to coordinate when falling from their own height).
Child in VOYTA therapy
Reflex movement is extremely effective, but for infants and small children it is unusual and tiring, and therefore emotions are expressed during treatment through screaming. This understandably irritates parents and makes them assume that their child is in pain. Screaming at this age of life is an important and adequate means of expression for a young patient. As a rule, after a short time of adaptation, the cry is not as intense as at the beginning of the course of treatment; in the vast majority of cases, with regular therapy, the child gets used to this effect and the negative perception reaction completely disappears. The precise guidance of a VOYTA therapist gives the mother confidence in treating her child at home. VOYTA therapy has a positive effect on the child’s overall coordination in the presence of spontaneous motor skills with expansion of motor reactions in the form of straightening, grasping function and speech. At the same time, it stimulates the child to master the world around him. In the field of early treatment of infants and children, VOYTA therapists intensively collaborate with pediatricians and doctors of other specialties, teachers and psychologists, speech therapists and occupational therapists. VOYTA THERAPY DOES NOT CAUSE PAIN AND HAS NO HARMFUL EFFECTS ON THE MENTALITY.
In Saratov and the Saratov region, consultation with a Voito therapist can be obtained at the clinic of occupational pathology and hematology of the Saratov Medical University.
We are waiting for you at the address: 53 Rifle Division Street, 6/9.
Directions: trolleybus N2-a, minibus NN82, 59, 103, 110 to the stop “2nd City Hospital” or minibus N105, 42 to the stop “Academy of Law”
This is the most common cause of anxiety in babies. At the age of 2 weeks to 3 months, many children experience functional disorders of the gastrointestinal tract: the child grunts, strains, sometimes cries; periodically there is liquefied greenish stool with white lumps or constipation, severe bloating. It’s a pity that dill water doesn’t help you either. (Then don’t spend money on “Happy-Baby” and “Baby-Calm (baby-calm) - these are all analogues in composition: they are all made on the basis of fennel (dill). You can brew a regular infusion of chamomile flowers and give the child something to drink, starting with a few drops and ending with a teaspoon. Some children are helped by a tiny amount - literally a few grains dissolved in milk or formula. More than once I have given on the site a recipe that I once read in a magazine and which has proven itself very well among children: COLLECTION FOR TREATMENT (Authors - Kosov V.A., Ermolin S.I. et al., Central Clinical Military Sanatorium "Arkhangelskoe"; was published in the "Military Medical Journal" No. 9, 1996, pp. 53-56 ) medicinal, root - 2 parts Chamomile, flowers - 2 parts Peppermint, leaf - 1 part Common raspberry, fruits - 2 parts Mix all components in the indicated proportions. The authors recommended dosing the collection in DROPLES, but it is so pleasant and useful that children they willingly drink it in large doses (at your age they begin to administer it with drops and increase it to a teaspoon). Brew 1 tablespoon of the mixture with 1 glass of boiling water in a thermos, leave for 2-6 hours (or overnight). The course of treatment is 1 month. I'm always a little wary of giving raspberries to children - they often have allergic reactions to the dye that gives fruits and berries their red color. For allergy sufferers, I even advise you to exclude this component of the collection; and without it the collection “works” perfectly. I have prescribed him more than once. If that doesn’t help, you can try the modern probiotic symbiter or the dietary supplement primadophilus. I would also add a tummy massage, gymnastics (bicycle-type leg movements); I would begin to place the baby on my stomach more often and encourage lifting of the upper body. Our grandmothers and parents, in addition to dill water, actively used a gas outlet pipe - no one felt worse from this. It not only allows you to remove gases, but also stimulates bowel movements. And finally, if the baby feels better on his stomach, put him in this position more often (both on your stomach, and even while sleeping in a crib. Many children like to sleep on their tummy - in this position, bloating is less pronounced. Just make sure , so that there is no down pillow or fluffy blanket nearby that could interfere with the baby’s breathing - although at one and a half months he is already able to raise his head and turn it if something interferes). Good luck!
If your baby is five months old, then it would be a good idea to familiarize yourself with the age norms characteristic of this period.
How to determine the location of the fetus yourself by kicks
In addition to accurately determining the position of the child using ultrasound, you can try to find out on your own where the fetus is.
This must be done carefully so as not to damage parts of the baby’s body. One of the ways to determine it is through the tremors that the baby makes while moving.
As a rule, the baby pushes off the walls with his arms and legs, so it will not be difficult to understand where his head is.
Every mother can feel the position of her baby's back by simply running her hand over her stomach. You can also feel the resting legs, and at the very bottom you can feel a certain bulge - the head of the fetus.
This period is characterized by hand tremors in the area of the sacrum or bladder. It is with the help of interpretations that it is possible to determine the approximate location of the child.
- The presence of the baby in the womb, head up, will be characterized by regular tremors above the womb. Where the inguinal folds are located, the movement will be felt most of all.
- The transverse arrangement is characterized by an unusually wide size of the abdomen. A woman may feel pain in the umbilical area due to its stretching. Painful sensations also occur when the baby straightens his head or moves his legs.
- The cephalic location of the presenting part is considered the most common.
In this case, the baby will put pressure on the area of the mother’s lower ribs. This phenomenon occurs at the end of pregnancy. If you run your palm along the anterior abdominal wall, you can feel the baby's head. - A presentation that is too low will be accompanied by sudden movements of the baby's head, and the mother will feel the urge to urinate more often than usual.
- Related Posts
Can a mother independently determine the position of the unborn baby in her tummy? Yes, and it's not that difficult! And it’s useful to learn: your conversations with your tummy will become more meaningful and, if necessary, you can even persuade your baby to roll over!
During pregnancy, sooner or later (usually closer to 40 weeks), in classes to prepare for childbirth, expectant mothers ask the question: “Is it possible to understand for yourself how the baby lies in the stomach?” And with interest they become acquainted with the Belly Mapping or “Belly Map” technique, which was invented by the American midwife Gail Tully. With its help, any mother can determine the position of the baby at any time. All you need is a little curiosity, a couple of days of observation, a piece of paper and a pen.
Why you can't start seating early
All children are born with an incompletely formed spine . He is not able to bend like an adult. In addition, the back muscles should
- maintain posture
- and do not allow the spine to bend too much.
A newborn baby does not have this kind of muscle development.
If a boy tries to sit down prematurely, his spine may be damaged, and the uncontrollable weight will put pressure on the internal organs, disrupting their work and development.
The boy's muscles strengthen over several months of his life. No matter how insignificant you may think
- movements of arms and legs
- attempts to raise and hold your head
- and turning over from tummy to back (or vice versa),
but all this strengthens the muscular system and prepares the baby for the first attempts to sit up.
Contrary to popular belief, early sitting of a boy does not affect the development of the genital organs . Many people claim the opposite, but when writing this article, I consulted with a practicing pediatrician and she confirmed to me that it does not affect the reproductive system in any way. It can only affect if the weight of the child puts pressure on the internal organs, including the organs of the reproductive system.
Preparation
Draw a large circle and divide it into 4 parts. This is your template for the belly map. The top of the circle is the top of your abdomen, where (oddly enough!) the bottom of the uterus is located, and the bottom of the circle is the pubic bone. Left and right change places, as in a mirror: your left side in the picture will be on the right, and vice versa. Now begin to notice your sensations and the baby’s movements.
Midwives know that the position of the baby in the stomach greatly influences the course of labor. For example, when the baby is in the posterior position (back to mother's back and arms and legs to mother's stomach), labor is longer, more intense for the woman and often begins immediately with strong contractions, but without rapid dilatation of the cervix.
The benefits of sleeping on your tummy
When a baby sleeps on his stomach with his butt raised, this has a beneficial effect on the normal development of the hip joint. In addition, there are other obvious advantages of this position:
- A baby in a position on all fours is not often tormented by intestinal colic. While he sleeps on all fours, gases pass away better due to massage with his knees. The entire gastrointestinal tract begins to work more actively. Some babies change their usual position to sleep with their legs bent just when the baby is suffering from colic. Therefore, when changing the usual position to a position on all fours, parents should pay attention to the functioning of the gastrointestinal tract.
- According to statistics and most experts, babies who sleep on all fours hold their heads earlier and more confidently according to their age.
- If the child burps, there is no danger that he will choke. If regurgitation enters the respiratory tract, there is a risk of abscesses, asphyxia, and aspiration pneumonia.
- The child moves his arms less, which promotes sound and healthy sleep.
- There is better blood supply to the brain.
- The baby does not lift his head due to infantile hypertonicity.
You should not wake up or turn the baby over. Parents just need to listen to their breathing. If the baby does not moan or groan, and the sleep is deep and breathing is even, there is no need to touch the baby. Then he will have problems falling asleep.
The benefits of sleeping on your tummy.
Where does the heart beat?
At a doctor's appointment, women learn basic things: cephalic presentation or breech presentation, where the heartbeat can be heard. If it is in the lower abdomen, then the baby lies head down, if it is at the top, the baby lies head up. Remember that after 30 weeks, about 15% of babies are in a breech presentation, and the rest are already ready to go and are in the correct cephalic presentation, so most likely your baby's head is already down. Some mothers easily navigate the position of the baby: the most protruding and hard part is usually the back, and then with some persistence you can feel what else is there: the head (a large and hard thing) or the legs and butt (by the way, your baby’s butt is very tiny and soft). On your map, draw a heart in the segment where it is tapped. This is the baby's upper back. Accordingly, the head will be opposite. If you don't know where the heartbeat was at all, just move on to the next step.
The child is sitting: why can’t you hurry?
When a child sits, a round back and falling to the side warn parents that the back muscles are not yet ready. Therefore, such children need to be seated with back support and only on an inclined surface (on your lap, in a chair with a backrest tilt of 30º).
If you try to sit a baby with a weak back upright, you may end up not with early development, but with early scoliosis or other spinal diseases.
Text: Elena Baburova, consultant - Sergey Vasiliev, pediatrician, doctor of the highest category
Where is the baby's head?
Many women distinguish between several types of movements. Some are very tender and weak, as if someone is tickling inside, as if a butterfly is flapping its wings. They are almost invisible, and are usually handles. If such movements are felt in the front of the abdomen, then most likely the baby is lying head down and his back is turned to the mother’s back (what is called “posterior view”). More noticeable pushes, kicks and even painful pokes (under the ribs - for those whose child lies head down) - this is how the baby usually kicks with his legs. If in the lower abdomen, near the pubic bone, someone is fidgeting a lot, most likely it is not the hands, but the legs of the baby in the breech presentation. Sometimes movements are noticeable to the mother in all segments at once. This happens when the baby is turned with his back to his mother’s back and with his arms and legs outward. Map two types of movements: in which segment are they felt?
Shutterstock/Fotodom Ukraine
When does a newborn begin to hold his head: 4 months
Now he has already learned to lean on his forearms - more and more often you see a curious face studying the room from a position, propped up on his hands while lying on his stomach.
Now the mother knows how many months the child is holding his head and understands that she was worried in vain. Child development is individual. A significant lag or advance may indicate health problems. For example, if a month-old baby is already holding his head up, it is worth visiting a neurologist, because such an early achievement is a symptom of intracranial pressure.
Where are the back, arms and legs?
Usually the belly on this side is rounder and smoother, and the bulge is often noticeable not only to the mother, but also to loved ones. This bulge is the baby's back. And the arms, legs and stomach are on the other side. Draw a line on the map that represents the roundness of the back. Now you can sign all the designations: back, head, arms, legs.
To understand the position of the baby, you can take a doll or toy the size of a baby and place it on your stomach. Looking at the map and remembering your feelings, try to position the doll so that the arms, legs, head and back are in their places. Upside down or upside down? With your arms and legs to the left, to the right, outward or inward of your mother’s belly? Most often, babies lie with their backs to their mother’s left side, but there are other options. Which one is yours most similar to?
Why can't I find anything?
Sometimes your curiosity and observations are still not enough to learn how to draw your belly map. The time factor is important. Until the 7th–8th month, determining the baby’s position may be more difficult due to his mobility and small size. Closer to childbirth, the placenta along the anterior wall, a large amount of water or a large fat layer in the abdominal area can make it difficult to read signals. Then you should try to make a chart for the first time together with the midwife, and then focus on your feelings.
Shutterstock/Fotodom Ukraine
What to do next?
Gail Tully suggests that mothers who find that the baby has not yet reached the optimal position in the stomach (head down, back to the mother's belly or to the left/right side) coax him to roll over and do special exercises to relax and balance the muscles that support the uterus , pay attention to your lifestyle:
- try to squat more (resting your full foot on the floor);
- sit leaning slightly forward or with your back straight;
- When working at the computer or watching movies, do not lean back, for example, by sitting on a slightly deflated fitball (this way it is more stable).
As unusual methods: bring a switched-on flashlight to the stomach (the baby will reach for the light) or place headphones with music (the young music lover may turn over to hear better).
In addition, do pregnancy yoga, walk and dance more: this will help maintain pelvic mobility and strengthen muscles.
If you find an error, please select a piece of text and press Ctrl+Enter
.
Most expectant mothers are very interested in how the baby is located in their belly. The closer the birth is, the more important this information will be for the progress of labor. In some cases of presentation, for example, vaginal delivery is contraindicated. And even with breech presentation, not every doctor or midwife will take care of them. You can ask about the baby’s position at a doctor’s appointment, but sometimes the wait for the next appointment is so long, and you want to know so badly that you can try to calculate the baby’s position yourself. It's not as difficult as it may seem and is definitely a good way to get to know your child better.
It makes sense to try to determine the position of the baby in the stomach after the thirtieth week. The longer the period, the more clear it will be to you how it lies, so if you don’t succeed, try again in a week - the attempt may be successful!
1. Where does the heart beat?
The easiest way to “find” a child is to find out where his heartbeat is best heard. You will need a regular stethoscope, a little patience and luck. Start listening from the lower left segment of the abdomen - this is where the heartbeat can be heard in most "settled" babies. Your goal is to catch sounds with a frequency of 120-160 beats per minute. You don't have to limit yourself to the front of your abdomen—in some positions, the heart can be best heard if the stethoscope is placed against your side. The heartbeat is best heard where the baby's upper back is located.
This method will be very useful to you if you need to understand whether the baby has turned over for birth from a breech presentation to a cephalic presentation. Find the spot where your baby's heartbeat can be heard best, and each day, as you do exercises to help him roll over, see if that spot changes. With a breech presentation it will be higher than with a cephalic presentation.
2. Belly Mapping - belly map.
This is the original method of midwife Gail Tully from the USA. Those who read English will be interested in going here: . This method allows you to independently, without the help of an ultrasound, determine the position of the baby in the stomach, and we teach it in our classes. In short, this is the gist of it. First you need to observe the child’s movements (what kind of movements they occur in him, and in what part of the abdomen you feel them). Then, while in a lying or semi-lying position, palpate the baby while the uterus is in a relaxed state. As a result, you will be able to make a “map” of the abdomen, on which you can mark the following: - where you feel the strongest kicks (these are your legs), - where you feel light movements of small amplitude (most likely these are your arms), - where the large protruding area is located , similar to the head (this is the butt), - on which side the abdomen is firmer and smoother (the child’s back is located there), - where the doctor last heard the child’s heartbeat (the upper part of the child’s back is located there).
How to distinguish a cephalic presentation from a breech presentation?
In any case, you will feel the protruding part of the child from above. But only the neck and back extend from the head, and from the butt there are also legs, which you can feel if you are persistent. In addition, you can remember where the doctor last found the sound of a heartbeat - if from below, then the baby is lying head down, and if from above, then his butt.
What can you pay attention to?
Many experts pay attention to where the baby's back is facing - towards the mother's back, or towards her stomach? This can be important because if the baby is lying with his back towards his mother's back most of the time in the last months before birth (this is called "posterior view"), then he will most likely begin to be born from this position, and in this case, labor may be more painful for the mother, longer lasting, and more likely to result in a caesarean section. Therefore, if when you feel you can never find the baby's back (this indicates that it is facing towards your back), it makes sense to see if you can persuade the baby to roll over. They say that due to the fact that the back is the heavier part of the child compared to the arms and legs, it usually tends to turn downward. In recent decades, women have begun to lead a much less active lifestyle and spend a lot of time half-lying or half-sitting, so that gravity pulls the child’s back down, that is, towards the mother’s back. This can be prevented if the mother more often takes positions in which gravity pulls the baby’s back towards the stomach (these are any straight positions and poses in which the mother’s body leans forward, swimming is also suitable) and generally moves more actively.
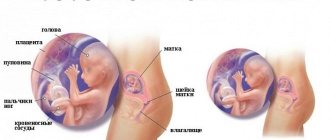
Sometimes, in order to “feel” the position of the child, the mother needs to see how the child, in principle, can lie in her stomach. Here's an illustration to refer to:
Why can't I feel anything?
Sometimes it can be difficult to “look” at a child in this way. In cases where there is a lot of amniotic fluid, or if the placenta is attached to the anterior wall of the uterus, or if the mother is plump and it is difficult to feel anything through the fat layer, the hands will “see” worse. If the uterus constantly tenses from attempts, it is better not to take them - anyway, you will not be able to obtain any reliable information. The baby feels best in the last two months of pregnancy. Naturally, professionals can very quickly determine the position of the child. But mothers have one advantage - they can do this much more often, because the child is always at hand. As a rule, in one or two weeks of attempts, almost any mother can learn to determine the position of the child if nothing interferes with her.
Then, when your baby is born, his body will be much more familiar to you and you will be able to hold him with more confidence. And during pregnancy, it is much more pleasant to feel the baby’s movements when you know how he makes them - where the leg is, where the arms are, where the butt is, etc. And to the questions “how is he doing?” It’s a pleasure to answer - “Everything is fine with him, he’s moving as usual, he stretched his legs several times this morning, he’s lying head down, there’s his back, etc.”
The position of the baby in the uterus varies depending on gestational age. In the first and second trimesters of pregnancy, the fetus is still small, the amount of amniotic fluid is large, and the uterus has the shape of a ball. Therefore, the baby moves and turns over freely in the womb.
Gradually, the baby grows and, starting from the 7th month of pregnancy, it assumes a constant position, which remains until the birth itself.
In what situations can pain occur?
Coccydynia is the result of separation of the pelvic bones during childbirth. The tailbone often hurts under the following circumstances:
- during defecation;
- with a sharp rise after a long stay at rest;
- lying on your back;
- when sitting.
In rare cases, the birth process provokes a fracture of the coccyx. The pathology is accompanied by sharp, constant pain that limits movement. Caring for a child in this situation is difficult, because the woman cannot sit or walk for a long time, she is in pain. It is difficult to confuse a fracture with a dislocation due to the nature of the pain. In this case, you should immediately inform your doctor about the discomfort.
Location of the fetus in the abdomen by week of pregnancy
At the 16th week of pregnancy, the fetus is still quite small: from the crown to the buttocks its length is 11 cm, and its weight is in the range of 80-110 grams. During this period of development, the baby can swim freely in the amniotic fluid - there is still plenty of room for him in the uterus. The baby is constantly moving in the uterus - stretching, moving its limbs, grimacing, bending, stretching.
The position of the fetus at the 16th week of pregnancy is constantly changing, because it has the ability to move and turn over freely.
As pregnancy progresses, the size of the baby increases and, in proportion to this, its free space in the uterus decreases. As a result, the child takes the final position in which it remains, awaiting birth.
How to determine the location of the fetus? A woman can understand the baby's position by palpating the uterus and feeling the baby's back. Tracing his back with your palm, you can feel the tubercle - the buttocks. On the other side you can feel the legs. The head is lowered down and feels like a hard bulge.
The easiest way to study the location of the fetus in the stomach is when the baby is active.
Sometimes it can be difficult to understand how to determine the position of the fetus and whether the bump being felt is the buttocks or the head, in this case you can ask the doctor to determine the position of the fetus.
Another nuance: if the tubercle is the buttocks, then moving it, the baby’s whole body moves; if, on the contrary, it is the head, it means that it will sink and emerge during palpation, but the body does not move.
Obstetric turn - how does it happen?
In the modern world, there are many ways to turn the baby and change the breech presentation to the correct one:
- gymnastics for breech presentation of the fetus. Classes using the methods of Bryukhov, Grishchenko and other specialists give good results. 95% of babies, after completing a set of exercises, are in cephalic presentation.
- conversations with the baby. The baby in the mother’s tummy begins to hear from the 20th week of pregnancy. Parents can talk gently to the future offspring and ask him to roll over. Daily 10-20 minute communication with an unborn baby makes it possible to change its position to the correct one.
- If gymnastics and talking with the baby did not help, there is another way to turn the fetus - external obstetric rotation according to the method of the Soviet obstetrician - gynecologist Arkhangelsky.
If a woman is 37-38 weeks pregnant, the amount of amniotic fluid is within normal limits, there is sufficient fetal mobility, there are no anomalies in the structure of the uterus and there are no signs of umbilical cord entanglement, then she can use the obstetric turning procedure. The process of external rotation must be carried out in a hospital, in an inpatient unit . The pregnant woman lies down on the couch, the obstetrician, making smooth movements along the woman’s abdomen, gradually turns the baby into the correct position.
Types of baby positions in the uterus
The medical literature describes 3 types of presentation, that is, the relationship of one of the large parts of the child’s body to the entrance to the pelvis:
- Head presentation;
- Transverse presentation;
- Breech presentation.
Head presentation - the correct position of the fetus in the womb; vertical position of the child, head down. It is considered the most favorable, since in this case the baby’s head passes first through the birth canal, and the body is born without difficulty and quickly.
Transverse presentation is the position of the baby with his shoulder, and pelvic presentation is with the buttocks and legs down. Breech presentation is determined during examination by a doctor and then viewed using ultrasound diagnostics. If the fetus is positioned in the abdomen with the buttocks and legs down, then the shape of the abdomen will be close to triangular, and arm movements will be felt in the upper abdomen, and not in the bladder area.
The position of the fetus varies from week to week, so there is no need to panic if the baby does not turn over on time.
At the 16th week of pregnancy, the position of the fetus with the pelvis down has the following reasons: malformations in the fetus, polyhydramnios and, at the same time, increased mobility of the child; placenta previa; narrow pelvis; oligohydramnios; uterine abnormalities; decreased uterine tone.
Don't panic if your baby is breech:
- with the current level of medical knowledge, pregnancy with such fetal presentation proceeds completely normally;
- Delivery is possible in 2 ways, both natural and surgical.
But the choice of method of delivery is made by the doctor during a comprehensive examination and assessment of indicators.
First weeks
In the first week, the baby is a collection of cells; by the seventh day, the unborn child is a lump of hundreds of cells. Now this is called a zygote. Moreover, every day the cells divide more and faster.
The second week is not yet an actual pregnancy, although the unborn baby is attached to the wall of the uterus, now the follicle is maturing, after this stage it will be decided whether the woman will be able to bear a child or not.
From the third to the twelfth week there is an embryonic period; only in the fourth week can a girl notice the absence of menstruation and some changes (drowsiness, toxicosis, loss of appetite and others) associated with pregnancy. Now the test will one hundred percent confirm the fact of pregnancy.
How to help a child accept a cephalic presentation?
The expectant mother can use safe methods of influencing the baby so that he takes the most comfortable position - occipital presentation (that is, the baby lies head down in the womb and faces the mother's back).
This position is important for natural childbirth without medical intervention.
Quite often, breech presentation can be converted to cephalic presentation with the help of yoga for pregnant women. Such exercises become especially effective in the third trimester.
Yoga poses help the baby to take the correct position in the womb: inverted poses (handstand, headstand, bridge, half-bridge, birch tree) have the maximum effect - they encourage the baby to roll over. But such exercises can only be performed by women with good physical fitness and who are closely familiar with yoga.
Yoga poses cannot harm and turn the child from the correct cephalic presentation to the pelvic one: the child will take advantage of the shift in the center of gravity and will instinctively move only if the position in the womb is incorrect. The fetus tends to turn over and take the correct position, and not vice versa, and it is when performing exercises such as “bridge” that the most favorable conditions for turning over arise. When practicing yoga, fetal inversion occurs within 7 days. If you feel a large movement or “noise” in your belly, your baby has most likely rolled over. After this, you can verify the results of the gymnastics by doing an ultrasound.
If a woman is not in very good physical shape, but wants to help the baby roll over, she can use the following exercises: raise her hips above her head by 25-30 cm and lie in this position several times a day. A shift in the center of gravity of the child's environment will contribute to a change in the position of the fetus at 16 weeks.
A pregnant woman can also perform the following exercise: leaning on her knees and hands, she needs to rock her pelvis, and so on several times a day for 10 minutes. When performing such exercises, the buttocks and legs of the fetus are removed from the pelvic bones, the revolution and correct positioning of the fetus are stimulated, and it receives more free space for movements.
The position of the fetus during pregnancy determines how a woman’s birth will proceed. If the baby is in a normal position, the woman will be able to give birth on her own. If the baby is not located as nature intended, some manipulations may be required in the prenatal period or even a cesarean section.
Baby sitting: stimulate interest
Stimulate your baby's interest in an upright position by placing him on your lap facing the big world (let your belly and arms support his back). It is permissible to place the baby on a pillow in a stroller - but not straight, but with an inclination of 30º with emphasis on the pillow.
When the child’s musculoskeletal corset is ready for loading, the baby sits up on his own, turning on his side or pulling himself up behind the bars of the crib. Up to 13-14 months, children help themselves with their hands, then the back muscles become so strong that the child can sit up using only the muscles of the abdomen, pelvis and hips.
Types of fetal position during pregnancy
Throughout a woman's pregnancy, the fetus grows and develops in the uterus. If you look at pregnancy week by week, the position of the fetus can constantly change. But only in the first half of pregnancy. As birth approaches, it becomes more difficult for the baby to change his position. For many expectant mothers, the position of the fetus does not change significantly from the 26th week of pregnancy.
Only after 32 weeks can we talk about the type of fetal predisposition, that is, establish whether the head or buttocks are located at the entrance to the woman’s pelvis.
There are several types of fetal position during pregnancy.
Head presentation
It is characterized by the fact that the baby’s head is located at the entrance to the woman’s pelvis. The cephalic position of the fetus can be:
- occipital - the back of the head, facing forward, is the first to be born;
- anterior cephalic or anterior parietal - the baby’s head passes through the woman’s birth canal, slightly larger in size than in an occipital presentation;
- frontal - the forehead serves as the conducting point for expulsion of the fetus;
- facial – the baby’s head is born with the back of the head backwards.
The cephalic position of the fetus is observed in 95-97% of pregnant women.
Breech presentation
It is characterized by the fact that the child’s pelvis lies at the entrance to the woman’s pelvis. The pelvic position of the fetus is:
- gluteal – the fetus is positioned head up, with the legs extended along the body so that the feet are almost near the head;
- foot – one or both legs of the baby are located at the entrance to the woman’s pelvis;
- gluteal-leg (mixed) – both the legs and buttocks are located at the entrance to the small pelvis.
Breech presentation, according to statistics, occurs in 3-5% of women.
Also, the location of the fetus during pregnancy is determined by its position in the womb. The position of the fetus is the relationship of the conditional line of the child (from the back of the head to the tailbone along his back) to the axis of the mother’s uterus. The following types of fetal position are distinguished:
- longitudinal - the axis of the woman’s uterus and the axis of the fetus coincide;
- oblique - the conditional axes of the uterus and fetus intersect at an acute angle;
- transverse - the axis of the fetus intersects the axis of the uterus at a right angle.
Another characteristic of the position of the fetus is the type of position - the relationship of the baby's back to the uterine wall. If the back of the fetus is facing anteriorly, this is an anterior view of the position. In the case when the child’s back is facing posteriorly, this is the posterior view of the position (posterior presentation of the fetus). Anterior presentation of the fetus is considered normal. The posterior one often becomes the cause of long, protracted labor.
Malpresentation of the fetus
After 28-30 weeks of pregnancy, the doctor determines the presentation of the baby. Sometimes even after the 26th week of pregnancy the position of the fetus remains unchanged. But this is the exception rather than the rule.
The cephalic presentation of the fetus is considered the most physiologically correct. With this arrangement of the baby, its largest part, the head, passes through the birth canal first, and the body and legs are born after it without difficulty. In addition, it is good if the child is turned to face the mother's back (occipital position).
Causes
Sometimes the baby may not be positioned correctly in the womb. The following reasons lead to this:
- Polyhydramnios. Since in this case the fetus floats in a large amount of liquid, it often changes its position.
- Repeated births. This is due to the fact that during repeated childbirth, the muscles are often flabby and the anterior abdominal wall is stretched. The uterus and fetus are poorly fixed, which leads to the risk of a breech presentation of the fetus.
- Uterine fibroids or abnormalities in the structure of the uterus.
- Low position or placenta previa, when it is located in the lower part of the uterus.
- Prematurity of the child.
- A narrow pelvis in a pregnant woman.
- Fetal malformations.
- Hereditary predisposition. If the expectant mother herself was born in a breech position, the risk of breech presentation for her child also increases.
If at 28-30 weeks the doctor determines that the baby is malpresented, you can expect that it will gradually improve. But after the 32nd week of pregnancy, the likelihood of the baby being properly positioned for childbirth decreases significantly.
However, you can take certain measures to help your baby get into the correct position. There are special exercises for this. Here are some of them:
- You need to lie on each side for 10 minutes, turning from side to side 3-4 times. It is important that the surface on which the woman lies is not too soft. This exercise is repeated 2-3 times during the day.
- Take a lying position, placing pillows or a rolled blanket under your pelvis and legs. You need to make sure that your legs are 20-30 cm above the level of your head. The exercise is repeated 2-3 times a day for 10-15 minutes.
The expectant mother should understand that these exercises have contraindications. Therefore, before you start performing them, you should definitely consult your doctor.
Sleeping position as a signal of the baby’s well-being
It’s one thing for a child to constantly sleep in one position, but it’s quite another if the position changes during the night. Depending on what new position the baby sleeps in, you can judge his well-being.
The child changed his favorite position to a butt-up position. This means baby Gaziki may have suffered a head injury. Often babies lie in this position with a stuffy nose.
If a baby suddenly begins to sleep on his back with his arms spread wide, although he has not slept like this before, this is a sign of problems with the respiratory system.
When changing your usual sleeping position to an uncomfortable or unusual position, you should observe the baby. If he begins to be capricious, eats poorly, sleeps restlessly, you need to see a doctor.