Is it possible to feed breast milk if you have ARVI?
The period of pregnancy and childbirth makes the female body weakened, as a result of which it becomes susceptible to pathogens of infectious and inflammatory diseases. Some literary sources indicate the impossibility of natural feeding when a young mother has a cold.
As a result of modern research, it has been found that breastfeeding is not only not prohibited, but is also recommended during the period of acute respiratory viral infection.
The benefits of feeding
The benefits of breastfeeding during the period of acute respiratory viral infection can be expressed in the form of a small list that includes the following points:
- The baby receives a timely dose of nutritional components necessary for the harmonious development of organs and systems;
- Together with milk, a massive dose of protective antibodies to respiratory viral infection enters the newborn’s body;
- Even temporary weaning from the mother's breast leads to the formation of stagnation (lactostasis). If stagnation continues for a long time, then the young mother runs the risk of getting mastitis.
Signs of a cold during lactation
Colds during lactation: developmental features and signs of the disease
A nursing mother should not panic when she develops a cold. After all, our body has evolved over many millions of years and has become resistant to various viruses. As for kids, there is no need to worry about them either, because usually such an infection is defeated by the protective forces of the immune system in a matter of days.
The disease begins to develop according to the following principle: first it enters a healthy body and begins its active reproduction, and as a result, the cells of the mucous membrane are damaged. An inflammatory process appears, which manifests itself in skin hyperemia, increased blood circulation and swelling. The development of a runny nose, cough, nasal congestion and sore throat begins. In response to acute respiratory infections, the body's defenses are immediately activated.
The immune system produces specific antibodies that destroy this infection. There is no need to be afraid of complications from a cold if a nursing woman has good body resistance. You should not panic and take the appearance of such a disease calmly.
You need to make every effort to support your body in the fight against the emerging viral infection.
A cold during lactation has the following symptoms:
- Dryness and itching appear in the sinuses, which causes frequent sneezing.
- The voice becomes hoarse, irritated and sore.
- A cough begins.
- Aches joints and muscles.
- A nursing mother experiences severe weakness and fatigue, accompanied by drowsiness.
- The temperature begins to rise from very insignificant numbers on the thermometer to very large ones.
- There is discharge from the nasal sinuses with a transparent tint and a thick liquid structure, which can thicken and turn into crusts.
- There is severe discomfort in the throat, which is associated with pain when swallowing.
- Profuse lacrimation begins, accompanied by a fear of light and pain in the eyes.
A cold can present with a different combination of symptoms. They can be either pronounced or completely insignificant. But all these signs bring severe discomfort to a nursing woman.
Breastfeeding when you have a cold
Some people mistakenly believe that breastfeeding during ARVI is dangerous. But this is absolutely not true. On the contrary, it can help the child. As mentioned earlier, along with mother’s milk, the baby receives a number of antibodies that resist such a virus. With a high degree of probability, it can be said that an infant will not get a cold while breastfeeding.
It is best not to deprive the baby of mother's milk when such a viral infection occurs, trying to protect him from the disease.
But there are situations when feeding a child is contraindicated.
These are cases when the mother has a very serious condition due to a cold, and her state of health does not allow her to properly care for the baby. This disease can lead to complications such as pneumonia and acute bronchitis. If they occur, then it is better for the woman to stop breastfeeding and transfer the child to formula feeding.
Most medications are contraindicated during lactation. This is due to the fact that medications can harm the baby’s health if they enter his body through mother’s milk. It is for this reason that a nursing mother needs to choose only safe drugs that will not harm her newborn baby.
Protection during feeding
In order to protect the child’s body from direct contact with a viral infection, a young mother should follow a number of restrictive rules:
- When in contact with a newborn baby, a woman needs to wear a mask made of cellulose or gauze, which should be changed periodically. In addition, before changing the mask, lubricate the nasal cavity with oxolinic ointment, which promotes the death of viral particles;
- In living areas, perform daily wet cleaning and ventilate the room. During ventilation, the child must be protected from possible drafts;
- A young mother needs to wash her hands with soap before each contact with her baby.
If a nursing woman practices pumping, then boiling breast milk is strictly prohibited. This product is not a potential source of infection for children.
Treatment
Treatment of a common cold in a nursing woman is carried out under the supervision of a medical specialist, since a nursing mother is responsible not only for her own health, but also for the health of the child’s body. The use of antiviral drugs is advisable as a preventive measure, as well as in the first hours after the onset of cold symptoms.
Such a popular drug Immunal can cause allergic reactions in a newborn baby, so you should refrain from taking it. Treatment of nursing women is carried out according to the following plan:
- To prevent and treat manifestations of viral infection, the drug Grippferon is used. This remedy is instilled 2-3 drops into each nasal passage 2-3 times a day. The active component of the drug is interferon;
- If a bacterial infection is added during the course of a viral disease, the young mother will need a course of antibacterial therapy. If the prescribed antibiotic is incompatible with natural feeding, then the woman will be recommended to pump and temporarily transfer the baby to artificial milk formula;
- During the treatment period, the amount of fluid you drink is important. The recommended volume is at least 2 liters per day. Warm herbal tea with raspberry or blackcurrant jam is beneficial;
- If, against the background of a cold, a nursing mother’s body temperature has increased, then antipyretics such as Paracetamol and Ibuprofen are used to reduce it. These medications are safe for both mother and baby;
- Treatment of cough in nursing mothers is carried out using mucolytic and expectorant drugs. The list of approved drugs includes Lazolvan and Ambroxol. It is strictly forbidden to use antitussives based on bromhexine.
To treat colds and bronchitis, it is permissible to use such remedies as Bronchicum, Tussamag, Doctor Mom. If a nursing mother suffers from nasal congestion, then vasoconstrictor drops and sprays (Galazoln, Naphthyzin, Xylometazoline) will help relieve swelling of the mucous membrane.
The duration of use of these products should not exceed 5 days in a row, as they tend to be addictive. To relieve swelling of the mucous membrane of the nasopharynx and sanitize the upper respiratory tract, nasal rinsing is performed. A 0.9% solution of sodium chloride (table salt) is suitable for this purpose.
If a nursing woman experiences a sore throat, she can use Lugol's solution to lubricate the walls of the pharynx and tonsils. Medicines such as Strepsils, Chlorhexidine, Sebidine, Iodinol have a powerful antiseptic effect. Before using each product, consultation with a doctor is required.
Common diseases during breastfeeding and their treatment
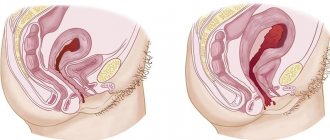
Mastitis
When purulent mastitis appears in a nursing mother, the child can be infected with it through the breast. Mastitis is treated using antibacterial drugs that penetrate milk to a high degree. Therefore, doctors most often decide to temporarily transfer the child to artificial feeding.
Cough, incl. dry
Before starting treatment for a cough, you need to determine what caused it. The cough may be:
- viral;
- bacterial;
- allergic nature.
A dry cough in a lactating woman can be cured with the help of medications and folk remedies.
Allergy
Allergies during breastfeeding can occur as a reaction to:
- food products;
- pet hair;
- plant pollen.
The allergic reaction is not transmitted through breast milk, so it is not necessary to stop breastfeeding. As a rule, it is not prohibited to be treated with drugs such as Clarotadine, Suprastin, etc.
Angina
Sore throat cannot be treated on your own, so you should consult a doctor if its signs appear. Continue breastfeeding - this will strengthen your baby's immunity and prevent contracting the disease. Treatment of sore throat during breastfeeding is carried out using the following drugs that do not harm lactation:
- Septolete;
- Faringosept;
- Hexoral;
- Tantum Verde.
There are also antibiotics that are compatible with breastfeeding.
Bronchitis
With bronchitis, breastfeeding a child is difficult due to the severe condition of the mother, which is characterized by cough, fatigue, respiratory failure, and a decrease in the quality of milk produced.
Mom can help herself if:
- will drink more fluids;
- to eat well;
- make inhalations from herbs.
Your doctor will prescribe you expectorants to help clear mucus. During lactation, it is prohibited to take medications that contain bromhexine.
Vasospasm
Nipple vasospasm manifests itself:
- whitening of the nipple during feeding;
- shooting pain in the chest.
In case of prolonged and severe pain, pain relief with Ibuprofen or Paracetamol is allowed.
Sinusitis
The main symptom of sinusitis is a prolonged runny nose (over two weeks) and accompanying symptoms:
- high temperature, up to 40 degrees;
- feeling of weakness and lethargy.
As soon as you notice these symptoms, consult a doctor immediately! Treatment of sinusitis during breastfeeding is carried out using Interferon, rinsing the nose with a solution of sea salt, inhalations, and punctures.
Haemorrhoids
Hemorrhoids manifest themselves with such unpleasant symptoms as pain during defecation, the appearance of streaks of blood in the stool. In such cases, consultation with a specialist, comprehensive diagnosis and treatment are required. During lactation, treatment is carried out with local agents.
Herpes
It is possible to alleviate its manifestations with the following medications:
- Zovirax;
- Penciclovir;
- Valaciclovir.
However, there is no reason to deprive a baby of breast milk.
Worms
Helminths cannot reach the child directly through milk, but infection is possible, for example, through unwashed hands. When treating for parasites, you will most likely have to stop breastfeeding, but not for long. The course will last a maximum of 5 days. Most often, when infected with worms, the following are prescribed:
- Pyrantel;
- Wormil;
- Vermox et al.
Head
If a woman has headaches, you can take a paracetamol tablet or relieve the pain with simple folk methods:
- very strong black tea with a lot of sugar;
- self-massage of the head;
- warm shower.
Throat
When treating a sore throat, the following procedures are considered harmless to the baby:
- gargling with decoctions of chamomile, sage, calendula;
- inhalations with eucalyptus essential oil;
- inhalation with boiled potatoes and soda.
Medications that are suitable for a nursing mother include:
- Antibiotics of the penicillin group.
- Cephalosporins.
- Macrolides.
But treating a sore throat with antibiotics of the tetracycline and fluoroquinolone groups is strictly prohibited. They negatively affect hematopoiesis and skeletal development in the baby.
Flu
The flu always develops very quickly and is dangerous due to its complications. Therefore, it is strongly recommended that nursing mothers get vaccinated against influenza. After vaccination, antibodies are produced that penetrate into the milk and are passed on to the baby, protecting him too.
But if the disease has already set in, you cannot stop breastfeeding, even temporarily. Because before you know you are sick, your baby has already received the virus through milk and needs the further protection that only your milk can provide.
When treating fever, antipyretic drugs that are compatible with lactation are used, and drinking plenty of fluids with decoctions of herbs and berries is used as an auxiliary therapy.
Pressure
If blood pressure is very high, a breastfeeding woman can take Captopril tablet. The concentration of the drug in milk is minimal. Dibazol is also safe to use during lactation.
Underbelly
If a woman feels nagging pain in the lower abdomen while breastfeeding, then most likely we are talking about the restoration of the uterus after childbirth. This symptom may appear in a nursing mother for 2-3 months.
It is not recommended to use painkillers, because they penetrate into the milk.
Constipation
A common phenomenon after childbirth is usually associated with:
- hormonal changes;
- rectal injuries during childbirth;
- unbalanced diet;
- lack of an active lifestyle;
- stress after the birth of a baby.
Most often, constipation does not require special treatment and goes away on its own after some time. Among the most common quick “helpers” for constipation in a nursing mother are glycerin and sea buckthorn suppositories.
Thrush (vaginal and breast)
Vaginal candidiasis of the mother must be treated, since it can also appear on the chest and be transmitted to the child during feeding. Both mother and child need to be treated simultaneously, without stopping breastfeeding. If a woman is in pain, it is better to feed more often, but for a shorter time.
Modern antibiotics intended for the treatment of thrush are compatible with breastfeeding, and antifungal ointments are also used.
Migraine
Migraines must be treated and not suppressed with painkillers, especially since not all are allowed during breastfeeding. Sumatriptan is considered the most effective against migraines during lactation. It is eliminated from a woman’s body in about 12 hours.
Runny nose
In the vast majority of cases, no treatment is needed at all. You can alleviate symptoms by:
- nasal rinsing;
- instillation or injection of saline solution or sea water into the nostrils.
Usually this symptom lasts 3-4 days. Feeding should be done in a disposable dressing.
ARVI and acute respiratory infections, colds
If you have a cold, then it is not necessary to stop breastfeeding your baby. But any contact with the baby must be carried out in a four-layer gauze or disposable bandage, remembering to change it every 2-3 hours. For colds, the use of herbal remedies is often sufficient.
Diarrhea (diarrhea)
Diarrhea may be a consequence of:
- irritable bowel syndrome;
- food poisoning;
- allergies;
- intestinal infection, etc.
Doctors are confident that diarrhea in a nursing mother most often does not pose a danger to the baby, and many folk remedies and medications will be harmless.
Poisoning
May be caused by:
- fatty and spicy foods;
- food containing chemicals and preservatives;
- spoiled products.
Poisoning in itself does not prevent breastfeeding. However, it is usually accompanied by nausea and vomiting, and fever. If signs of poisoning do not go away for several days, you should urgently contact a specialist to prescribe treatment.
Cystitis
Main symptoms of cystitis:
- frequent painful urination;
- pain and burning when urinating.
With timely treatment, it easily goes away in a few days. During lactation, Canephron, Phytolysin, and folk remedies are used for treatment. Antibiotics that are compatible with feeding:
- cephalosporins (for example, Ceftriaxone);
- penicillins (for example, Amoxiclav);
- macrolides (for example, Vilprafen);
- Monural.
Barley
Occurs on the eye as a result of infection of the hair follicle or sebaceous gland by pathogenic bacteria. As a rule, it is acute and increases rapidly.
Women, on the recommendation of their attending physician, use medications in the form of drops, ointments, and gels. Acceptable use:
- Levomycytin;
- Tobrex;
- Albucid;
- Phloxal.
Temperature
Feeding is allowed if the temperature has risen due to a cold or other non-dangerous disease. To alleviate the condition of the mother, it is recommended to use antipyretic drugs based on paracetamol.
Most diseases do not prevent breastfeeding. In addition, many drugs have now been developed, even antibiotics, that will not harm the baby during the mother’s treatment. We must not forget that by feeding on breast milk from the mother, the child gains immune protection for life.
Is it possible to breastfeed if the mother has ARVI?
Doubts about the possibility of continuing to feed a baby with breast milk by a mother who has been diagnosed with ARVI arise for everyone who finds themselves in such a situation.
Caring women, independently assessing their condition, often decided to continue breastfeeding. And they were not mistaken.
Doctors around the world have carefully studied this issue for several decades.
Observations have confirmed that breastfeeding helps a healthy baby not to get sick, and facilitates and speeds up the recovery process for an ill baby. Thus, it is now officially confirmed that the composition of breast milk stimulates the processes of the immune system. The list of contraindications for the main modern antiviral drugs does not include the lactation period.
The appearance of signs of a cold - cough, fever, runny nose - means that the virus has been in the mother’s body for some time. In addition, the process of fighting them has already been launched, and specific antibodies are actively produced by the body.
By the time a nursing woman begins to sneeze, the pathogens and antibodies have already reached the baby through breast milk.
Read also
Nutritional features for biliary dyskinesia: allowed and prohibited foods, sample menu for the week
During the period of illness, regular, or better yet more frequent, breastfeeding becomes especially important. Increasing a child’s own immunity will help cope with the disease and become a reliable protective barrier against viruses in the future.
This applies to those cases when a sick nursing mother does not take medications, the contraindications of which include refusal to feed. If the disease requires drug treatment, the doctor may individually recommend:
- Completely stop breastfeeding.
- Limit feeding to expressed breast milk, avoiding breastfeeding.
This may be taking medications that are contraindicated for use during lactation, or the severe physical condition of the mother, which does not allow her to hold the child.
Doctors insist on refusing to feed in cases of heart failure, high blood pressure, serious problems with the kidneys and lungs, during the postoperative period.
In other cases, the generally known period of treatment for ARVI is considered to be a week. Since the spread of the virus occurs through airborne droplets, it would not be superfluous to use a mask when interacting with the child, including during feeding, that will protect the baby’s mucous membranes from pathogenic sputum.
Breast milk will help maintain the water-salt balance, which will provide the necessary conditions for the functioning of the respiratory tract and prevent drying out of the nasopharyngeal mucosa.
For what ailments can a mother not continue breastfeeding and what should she do?
The question of the possibility of breastfeeding when the mother is ill remains controversial. You can consult with your doctor and pediatrician, but only you will make the final decision.
It is believed that there are only 4 diseases that are an obstacle to breastfeeding:
- active tuberculosis;
- HIV;
- viral hepatitis B and C;
- syphilis.
But since no research has been conducted in this area, there is no clear answer about continuing feeding even with these diseases. Presumably, since there is a risk of infection of the child, it is necessary to stop breastfeeding.
All other diseases are not a contraindication for breastfeeding. In addition, for the treatment of breastfeeding mothers, the following are used:
- physiotherapy;
- aromatherapy;
- homeopathy;
- antibiotics acceptable during breastfeeding.
Medicines that should not be taken by breastfeeding due to danger to the baby’s health:
- amethopterin, ergotamine, gold salts, thiuracil;
- drugs that increase the radioactivity of milk;
- diazepam, barbiturates, tetracycline, sulfonamides, chloramphenicol;
- hormonal contraception and drugs containing estrogen.
The period of maximum concentration in the blood (and therefore in milk) can be avoided by taking medications during or immediately after feeding.
Of course, this is not the entire list of dangerous drugs. Be sure to read the instructions and consult your doctor before using any medications. And best of all, practice prevention so as not to jeopardize the baby’s health.
What about milk?
So, breastfeeding does not stop during the seasonal cold virus.
During this period, it is especially important to be guided by the knowledge that a mother's milk contains everything she consumes.
Adding vitamin decoctions to the diet will have a beneficial effect on the well-being of both mother and baby.
Being a product of blood synthesis, breast milk contains antibodies that stimulate the immunity of a child who receives breast milk from a sick mother. During this period, it is useful to put the baby to the breast a little more often than usual to prevent dehydration.
Consulting with your doctor will help dispel all doubts about possible treatment.
No matter how many substitutes for breast milk there are, they all remain substitutes, that is, they are not fully breast milk.
It is believed that up to 6 months, the main function of mother's milk is nutritional, since the growth of a child requires a special individual set of nutrients that ensures the growth and development of basic vital systems.
By 6 months, the needs of the growing body change, and along with this the composition of mother's milk changes. There is a decrease in the immunity received at birth. There is a need to strengthen the protection function, which becomes a priority.
The ability of memory cells to accumulate information about previously encountered viruses allows the body to produce the necessary antibodies and create stable protection against known diseases.
So, for example, with mother's milk, the child receives immunity from chickenpox if the mother has suffered this disease, and for up to 8 months does not get sick or suffers the disease without symptoms.
This confirms that the child has received immunity from the mother.
If a mother and child are sick at the same time, or only the mother is sick, her immune system actively fights the virus and produces antibodies that are passed on to the baby and protect him from that particular virus.
If only the baby is sick, then his immune system will have to cope with the disease on its own. But even here, the restorative and nutritional properties of breast milk will help the baby cope with the virus.
And here it is very important to pay due attention to the immunity of a nursing mother. The mother's body spends its most valuable resources on feeding the baby. In case of malnutrition, your own resources will be used, which can cause a decrease in immunity.
To avoid such problems, you must remember that:
- After 1 year of age, breast milk cannot remain the main source of nutrition. It is necessary to introduce complementary foods on time.
- A breastfeeding woman must eat well. The average daily intake is 3200 kcal.
What medications for colds are allowed during lactation?
The list of medicines prohibited for breastfeeding women is long. In the case when a mother has a cold, it is much easier to know what a nursing mother can drink when she has a cold.
Let's consider how to treat a cold for a nursing mother, so as not to harm your baby.
Antiviral drugs
Most antiviral medications are contraindicated for use by a nursing mother for colds. The list of approved drugs for pregnant and lactating women includes Aflubin, Grippferon, and Oscillococcinum.
These antiviral drugs have proven to be effective and absolutely safe medicines. They began to appear in pharmacies relatively recently, so you need to consult a doctor for advice.
Antipyretic drugs
Drugs with an antipyretic effect are also undesirable for a woman who continues to breastfeed her baby. But you still have to bring down the high temperature. Under the influence of elevated temperatures, complete loss of mother's milk can occur.
Before reducing a nursing mother's temperature with medication, you can try wiping with a weak vinegar solution. It is recommended to continue them until the temperature drops to 37.5 C˚. If the temperature has reached 39 C˚, and rubdowns have not been able to reduce it, take Paracetamol, you can also drink Panadol or Nurofen - children's syrups.
Remedies for the treatment of runny nose
It is not allowed to treat a runny nose in a nursing woman using traditional medications. If a mother has a cold, then she can use Aquamaris or Salin to fight a runny nose. Vitaon and Pinasol drops, which have an antimicrobial effect, showed excellent results.
Medicines to treat cough
What medications can nursing mothers take to treat a cough when they have a cold? During breastfeeding, it is possible to cure a cough with the help of Gedelix, Lazolvan, Ambroxol, Breast Elixir or Bronchicum. You can treat with herbal syrups or use anise drops.
General principles of treatment
There is no need to delay treatment, especially when the well-being of two people – mother and child – depends on its effectiveness.
By starting to use medications to alleviate the symptoms of the disease, you can significantly alleviate the course of the disease and its consequences.
The main principle of treating colds during breastfeeding is the safety of the baby.
It is very important to consult your doctor. This will allow you to get recommendations from an experienced specialist and get rid of doubts by asking questions about the impact of the treatment course on the baby’s condition and behavior.
When choosing treatment, you should choose remedies that will have a beneficial effect on both organisms, without side effects. These methods include:
- inhalations with boiled potatoes or decoctions of chamomile, calendula, eucalyptus;
- aromatherapy using essential oils of fir, eucalyptus, rosemary;
- tea with lemon and honey, compotes and fruit drinks with sea buckthorn, raspberries and rose hips.
These traditional medicines will increase the body's defenses and help naturally overcome seasonal illness.
Well-known and recommended mechanisms for alleviating the condition and getting rid of the virus include:
- Drinking plenty of fluids is necessary to thin the mucus, increase sweating and prevent the mucous membranes of the nasopharynx from drying out.
- Instillation of the drug Grippferon into the nose, the basis of which is interferon. The drops have antiviral, anti-inflammatory and immunomodulatory effects, and have no other contraindications other than individual intolerance.
- Vitamin E, ascorbic acid and interferon in Viferon suppositories help cope with the disease and do not have a negative effect on the composition of breast milk and the lactation process.
- To protect against the virus, the body launches a fight mechanism such as an increase in temperature. The recommended elevation for taking antipyretics is 38.5°. The safest way for a nursing mother to reduce her temperature is to take Paracetamol powder. The dose should be calculated in accordance with the instructions for use or together with your doctor. There are no studies guaranteeing safety for infants when processed drugs TeraFlu, Coldrex, Fervex enter breast milk, so their use is not recommended.
- Herbal preparations, which include licorice, anise, plantain, and coltsfoot, will help get rid of a cough. It is necessary to choose agents that dilute mucus and promote its separation and removal from the bronchi. You can take it as a decoction on its own or add it to tea. You should carefully read the dosage recommendations and monitor the condition of your child’s skin while taking herbal drinks.
- Adequate rest promotes a speedy recovery from many ailments, but this rule is especially important during seasonal viral diseases. Adequate sleep, a balanced diet, vitamins, regular ventilation of the room, and walks should become mandatory components of the treatment process.
Read also
How to avoid stretch marks and maintain breast shape after childbirth - tips and recommendations from experts
How to protect your baby?
So, the nursing mother fell ill and has already started treatment. But what measures need to be taken and what to do to avoid infecting the baby? We all know that during breastfeeding, a mother and her baby should never be separated.
Do not stop feeding your baby breast milk when he has a cold, this will allow the baby to fight the disease more effectively.
Take the necessary measures, which are recommended by Dr. Komarovsky, well-known to all parents, to reduce the viral load on the baby:
- Use a four-layer gauze bandage that completely covers the mouth and nose area. You need to put on a new mask every 3 to 4 hours. If it gets wet faster than the specified time, it should also be replaced immediately;
- To prevent other family members from becoming infected, ventilate the children's room every hour for 15 minutes to change the air. As a result, old air carries with it many viruses from the room. The lower their concentration in the air, the less chance other family members have of becoming infected;
- It is necessary to wash your hands frequently, since touching your nose or mouth can cause infection on your palms. Keep a bottle of 72% alcohol or other antiseptic near you and wipe your hands with it. This is especially true if mommy has herpes on her lip as a result of a disease.
Maintaining personal hygiene will protect your baby from colds. A small concentration of viruses in the room and antibodies in breast milk will enable the baby to maintain his health.
Based on the foregoing, we can conclude that when treating colds in mothers during lactation, you can breastfeed your baby. You just need to strictly adhere to the rules that we described in this article.
Breastfeeding during ARVI. Is there a risk for mother and baby?
Is it possible to breastfeed a child during a cold?
Your first vacation with a newborn! A sea of emotions and... reinsurance. Instead of high mountains there are shady alleys, instead of the salty sea there is an inflatable pool. There is a breeze, drafts - and now mom is already opening the first aid kit at the countryside. But there is another topic that concerns women at this moment: is it possible to breastfeed during illness?
There is only one answer - it is possible and necessary! The fact is that even during pregnancy, mothers generously shared their antibodies with their baby. After birth, the baby receives these same antibodies through breast milk. So at first it is reliably protected from viruses.
Medicines to relieve sore throat
To reduce pain in the throat, the use of “Miromestin”, “Inhalipt” and “Iodinol” will help. On various forums for caring for babies, it is recommended to take sucking tablets for sore throats, which are widely available on the shelves of modern pharmacies.
Antibiotics for a nursing mother
When prescribing antibiotics to women who continue to breastfeed their children, doctors are of the opinion that if antibiotics do not harm the child, they do not pose a danger to his mother.
If a nursing mother takes antibiotics when treating flu and colds, then it is necessary to remember that these should not be sulfate-containing drugs, since they are poorly absorbed by infants. Antibiotics for women who are breastfeeding can be used while the baby is sleeping.
Rules for breastfeeding during illness
It is breastfeeding that provides babies with protection and helps our little ones avoid trouble. Many nursing mothers note that during their illness the baby remains absolutely healthy. When a child receives developed immunoglobulins through mother’s milk, he becomes resistant to the attacks of insidious viruses and does not react to them in any way.
Try not to interrupt breastfeeding during ARVI. After all, this will not only deprive the baby of valuable proteins and immunity from the mother, but will also cause stress on the new diet. Don't forget that viruses entered your body much earlier than you felt sick. And the child was already drinking milk with antibodies against viruses appearing in it. This served as a preventive measure for him.
You should also not express milk while breastfeeding. Moreover, there is no need to boil this milk, as some mothers do. It is worth stopping breastfeeding temporarily if the mother has been prescribed medications that are dangerous to the baby. And this happens extremely rarely, since doctors always try to find an alternative treatment that is absolutely safe when feeding.
When interacting with the child (including when feeding), the mother should use a mask. Change your clothes and wash them more often than usual to prevent viruses from getting on your child’s mucous membranes. Constantly ventilate the apartment, but avoid drafts. Monitor the humidity in the room. Too dry air causes the baby's nasal mucosa to dry out, and this increases the risk of viruses.
Cold medicines
The most important question that women ask is how can a nursing mother treat a cold? There are medications that can be used during this period, but they should only be prescribed by a doctor.
When breastfeeding, you can use the following medications for colds.
- Grippferon or Interferon. Medicines that come in the form of nasal drops. Their action is aimed at obtaining and producing interferon. Absolutely safe at any age.
- Viferon. Produced in the form of suppositories with different dosages. They have antiviral and immunomodulatory properties. They have no restrictions, and therefore can be used at any age and position.
- AquaLor, AquaMaris. Cold remedies based on sea salt. Used to rinse and clear the nasal passages of accumulated mucus.
- Ambroxol, Lazolvan, Doctor Mom. Medicines that are used to remove phlegm from the lungs.
- Mirastin, Tantum Verde, Hexoral. Medicines for irrigating the throat. They do not penetrate into the general bloodstream, as they act locally. Prescribed for sore throat and sore throat.
- Pinosol. They are produced in the form of drops, spray and ointment. They have a natural composition, which includes essential oils. Eliminates viral and bacterial infections, while moisturizing the mucous membrane.
Treatment of colds while breastfeeding should not be carried out with the help of:
- products containing bromhexine;
- antiviral agents in the form of Arbidol and Remantadine. This group of medications is effective only in the first hours after the first symptoms appear. In addition to all this, they lead to disruption of the baby’s digestive system and an allergic reaction;
- Immunal and Aflubin. These drugs are very allergenic;
- antipyretics in the form of Fervex, Theraflu and Coldrex. They contain vasoconstrictor components that are harmful to the child.
In any case, in order not to make a mistake in choosing medications, you should consult a doctor.
What to do if you get sick?
You should not self-medicate, because only a doctor can give competent recommendations on how to deal with the disease and not aggravate its course. Only a doctor will be able to determine, for example, what causes your runny nose - viral or allergic. The prescribed treatment and choice of medications will depend on this.
— If your mother has a high fever (above 38 degrees), to cope with it before the doctor arrives, you can use wiping with vinegar diluted with water. A soft towel is moistened with the solution and the entire body, arms, and legs are wiped. Repeat the procedure after 20-30 minutes.
If wiping does not help, you can take paracetamol once in the form of a tablet or rectal suppositories; this will not harm you or your baby.
— For dry coughs, black radish juice mixed with honey helps a lot. This mixture has pronounced bactericidal properties and softens sputum. But you need to be careful and monitor for possible allergic manifestations in your baby.
Inhalations are also used for coughing - you can breathe over a hot infusion of herbs or boiled potatoes.
If possible, purchase a nebulizer (remember that for treatment with a nebulizer you need pharmaceutical products that are recommended by the doctor). A nebulizer will not only help the whole family in treating coughs, but will also become indispensable for your child as he grows up.
— When you have a runny nose, rinsing your nose with salt water is effective. Prepare the solution yourself (1 tablespoon per glass of water) or buy a pharmaceutical preparation based on saline solutions. At home, you can use chamomile infusion (chamomile, coltsfoot, thyme, linden) for rinsing. This decoction is also used to rinse the nose and gargle.
But we must remember that traditional methods of treatment are effective if the disease is mild!
In the age of modern technology, young mothers still prefer pharmaceutical products for treatment. For a runny nose, various drops and sprays are used. Usually these are vasoconstrictor drugs, as well as drugs containing essential oils and sea water.
Before use, you must carefully study the instructions to make sure they are safe for your baby. Sprays and drops are used immediately after feeding to minimize the penetration of the drug into milk. Please note that essential oils can cause allergies in infants.
When coughing, expectorant infusions, for example, infusions of linden, thyme, coltsfoot, which are powerful natural medicines, help well.
Of course, antiviral drugs are also included in the treatment complex. One of the most proven remedies is the drug Viferon, which is available in the form of suppositories, gel and ointment. For the treatment of ARVI, the doctor will recommend Viferon/Suppositories - they are completely suitable for a nursing mother, because the drug does not have such restrictions as lactation.
Read also
Placing a newborn on his stomach - during childbirth and in everyday life up to a year
The standard dosage is considered to be 500,000 IU, but the duration of treatment is determined by the attending physician, usually 5 days. Moreover, during illness, a mother can use Viferon gel for her baby and loved ones to protect them from infection.
Some folk remedies
- Potato inhalations. You need to boil a few potatoes, mash them, add them to the soda. You need to sit over a pan of hot broth for 15–20 minutes. For greater effect, cover the head with a towel. The same inhalations are made from eucalyptus decoction.
- Aloe juice mixed with honey is a good alternative to expensive drops. It rarely causes allergies in the baby. You can also chop a few pieces of juicy garlic and mix with oil.
- Sore throat can be relieved by gargling with herbal infusions: chamomile, sage. You can also use a solution of regular or sea salt.
To prevent a cold, a mother needs to monitor her health, as well as the health of her baby.
Feeding and antibiotics
If a viral infection is accompanied by a bacterial one, complications arise in the form of pneumonia, sore throat, and otitis media. In such cases, antibiotics must be used. But this does not mean that breastfeeding should be stopped. There are medications that are approved for breastfeeding, unless, of course, there are special indications. Be sure to consult your doctor!
After any viral infection, specific immunity is developed, but it does not save us from the next cold, since it will be caused by a completely different strain of the virus. But you shouldn’t despair, because your experiences are always passed on to your baby!
Start treatment on time, do not delay your visit to the doctor. Constantly strengthen your immune system: try to get enough sleep whenever possible! Eat right, be sure to walk in the fresh air with your baby.
This will fill you two with positive emotions and make you resistant to diseases!
VIFERON® Suppositories help alleviate the course of the disease, cope with symptoms and reduce the likelihood of complications. The original formula of the drug, containing interferon and highly active antioxidants, blocks the virus and restores the immune system. Thanks to its convenient release form, VIFERON® acts gently, without having a negative effect on the stomach. It is approved for use by children from the first days of life and by expectant mothers from the 14th week of pregnancy, as well as during breastfeeding.
How to light a candle for a child? Step-by-step video instructions and tips for moms
THERE ARE CONTRAINDICATIONS. SPECIALIST CONSULTATION IS REQUIRED.
Drug treatment
Safe treatment of colds during lactation using medications
Colds during lactation should be treated with medications that do not contain any harmful components:
- To eliminate a severe cough, you should take expectorants. During lactation, a good choice would be to take Lazolvan or Ambroxol. To make breathing easier, products such as Chest Elixir or Doctor Mom are recommended, that is, those syrups that contain medicinal herbs.
- Severe congestion in the nasal sinuses is eliminated with the help of vasoconstrictor drops such as Tizin, Farmazolin or Nazivin. Abuse of such drugs can lead to complications in the form of atrophic rhinitis, so you should not get carried away with these drugs. They can be used for no more than seven days.
- During a sore throat, you should use products that have a local effect and are antimicrobial in nature. These include Hexoral, Iodinol and Strepsils. As for the mucous membrane, it can be smeared with Lugol.
- Herbal oil drops have an excellent anti-inflammatory effect on the sinus area.
- Acute respiratory infections caused by infections of viral origin can be eliminated with the help of Grippferon. This drug has no contraindications to treatment during lactation. In addition, the body tolerates it well.
- During a cold, the nasal mucosa must be additionally moisturized. This can be achieved using sea salt drops and sprays.
It should be remembered that during lactation it is strictly forbidden to use drugs containing bromhexine.
Traditional methods of treatment
The best folk recipes
Since ancient times, treatment of acute respiratory infections using traditional medicine recipes has been not only safe, but also had a fairly good effect:
- The use of inhalations is as safe as possible for the mother’s body. They can be made using herbs (for example, steaming eucalyptus leaves). Using steam from boiled potatoes gives excellent results. To facilitate the process, you can purchase a special drug - a nebulizer. It will also be useful to the mother when the child grows up to treat colds. Inhalations with its help are done using Borjomi, Ambrobene (solution) or saline. The doctor must decide which remedy will be most effective for acute respiratory infections. By doing inhalations three to four times a day, after just two days you can see how your health has improved.
- With the help of raspberry tea, you can easily soften the general condition during such a disease.
- To help a sore throat, use a gargling solution that contains water (1 glass) and apple cider vinegar (1 tablespoon). Procedures with its help should be carried out at least once every hour.
- To make breathing through the nose easier, use the following recipe: heat a quarter cup of sunflower oil in a water bath and mix with garlic and onion, previously crushed into fine crumbs. This mixture is infused for an hour to two, and the resulting composition is lubricated inside the nasal sinuses.
- Linden tea with the addition of honey has an excellent effect. The concentration of such a drink should not be too strong; it should be slightly darker than water. You should not be overzealous with the use of linden; its excessive use is fraught with the appearance of pain in the heart area.
- For acute respiratory infections, the use of onions and garlic is very useful. They can be pre-chopped and mixed with honey. To get rid of colds, one or two teaspoons of this composition are eaten after each meal. However, we should not forget that these odorous products can provoke allergies in an infant. Therefore, before using such a drug, you should consult your doctor.
Useful video - Colds during lactation.
Signs of rhinovirus infection and best treatments for children and adults
Many nursing mothers are concerned about the question: is it possible to steam their feet if they have a cold during lactation? Yes, such procedures are indicated during acute respiratory infections. It is very important to follow one rule: the water temperature should not be more than 40 degrees, and the process itself should last approximately 8-12 minutes. This method is quite effective. And to make its effect even better, you can add a small amount of mustard to the water. Immediately after the procedure, you must put on cotton socks.
Actions at temperature
Effective and safe methods for normalizing body temperature during lactation
If the temperature during lactation rises to 38.5 degrees, the nursing mother can take paracetamol (one tablet) or drugs based on it. This medicine is the safest for reducing high fever. This drug perfectly eliminates pain in the head and muscles that accompany acute respiratory infections.
But before doing this, you should consult your doctor to avoid unwanted effects. As for drugs like Theraflu, Fervex or Coldrex, it is better not to take them on your own, since it has not yet been established how they can affect the baby’s body.
At temperatures below 38 degrees, you can use a wipe based on a weak vinegar solution. Vodka in equal proportions with water is also suitable for this purpose. After the whole body has been rubbed, you need to cover yourself with a light sheet. These steps should be repeated every 15-25 minutes. If the thermometer shows a temperature of 37.5, then there is no need to bring it down.
But when the temperature is very high (more than 38 - 38.5 degrees), the milk may well “burn out” and lactation will stop.
One important rule during acute respiratory infections is that if a prolonged increase in body temperature occurs, you should never self-medicate. You should immediately seek the help of a general practitioner, and do not forget to mention breastfeeding at your appointment. A specialist can prescribe antibiotics and other drugs against this viral infection that will not harm the baby’s health.
Is it possible to feed breast milk if you have ARVI?
The period of pregnancy and childbirth makes the female body weakened, as a result of which it becomes susceptible to pathogens of infectious and inflammatory diseases. Some literary sources indicate the impossibility of natural feeding when a young mother has a cold.
As a result of modern research, it has been found that breastfeeding is not only not prohibited, but is also recommended during the period of acute respiratory viral infection.
The benefits of feeding
The benefits of breastfeeding during the period of acute respiratory viral infection can be expressed in the form of a small list that includes the following points:
- The baby receives a timely dose of nutritional components necessary for the harmonious development of organs and systems;
- Together with milk, a massive dose of protective antibodies to respiratory viral infection enters the newborn’s body;
- Even temporary weaning from the mother's breast leads to the formation of stagnation (lactostasis). If stagnation continues for a long time, then the young mother runs the risk of getting mastitis.
Protection during feeding
In order to protect the child’s body from direct contact with a viral infection, a young mother should follow a number of restrictive rules:
- When in contact with a newborn baby, a woman needs to wear a mask made of cellulose or gauze, which should be changed periodically. In addition, before changing the mask, lubricate the nasal cavity with oxolinic ointment, which promotes the death of viral particles;
- In living areas, perform daily wet cleaning and ventilate the room. During ventilation, the child must be protected from possible drafts;
- A young mother needs to wash her hands with soap before each contact with her baby.
If a nursing woman practices pumping, then boiling breast milk is strictly prohibited. This product is not a potential source of infection for children.
Treatment
Treatment of a common cold in a nursing woman is carried out under the supervision of a medical specialist, since a nursing mother is responsible not only for her own health, but also for the health of the child’s body. The use of antiviral drugs is advisable as a preventive measure, as well as in the first hours after the onset of cold symptoms.
Such a popular drug Immunal can cause allergic reactions in a newborn baby, so you should refrain from taking it. Treatment of nursing women is carried out according to the following plan:
- To prevent and treat manifestations of viral infection, the drug Grippferon is used. This remedy is instilled 2-3 drops into each nasal passage 2-3 times a day. The active component of the drug is interferon;
- If a bacterial infection is added during the course of a viral disease, the young mother will need a course of antibacterial therapy. If the prescribed antibiotic is incompatible with natural feeding, then the woman will be recommended to pump and temporarily transfer the baby to artificial milk formula;
- During the treatment period, the amount of fluid you drink is important. The recommended volume is at least 2 liters per day. Warm herbal tea with raspberry or blackcurrant jam is beneficial;
- If, against the background of a cold, a nursing mother’s body temperature has increased, then antipyretics such as Paracetamol and Ibuprofen are used to reduce it. These medications are safe for both mother and baby;
- Treatment of cough in nursing mothers is carried out using mucolytic and expectorant drugs. The list of approved drugs includes Lazolvan and Ambroxol. It is strictly forbidden to use antitussives based on bromhexine.
To treat colds and bronchitis, it is permissible to use such remedies as Bronchicum, Tussamag, Doctor Mom. If a nursing mother suffers from nasal congestion, then vasoconstrictor drops and sprays (Galazoln, Naphthyzin, Xylometazoline) will help relieve swelling of the mucous membrane.
The duration of use of these products should not exceed 5 days in a row, as they tend to be addictive. To relieve swelling of the mucous membrane of the nasopharynx and sanitize the upper respiratory tract, nasal rinsing is performed. A 0.9% solution of sodium chloride (table salt) is suitable for this purpose.
If a nursing woman experiences a sore throat, she can use Lugol's solution to lubricate the walls of the pharynx and tonsils. Medicines such as Strepsils, Chlorhexidine, Sebidine, Iodinol have a powerful antiseptic effect. Before using each product, consultation with a doctor is required.
What to do if a nursing mother gets the flu
Despite the fact that an influenza epidemic has not been officially declared, the media report dozens of deaths caused by influenza in Ukraine. If a nursing mother gets sick with the flu, the first thing she thinks about is how not to infect her baby.
What to do if a nursing mother gets the flu? How can a mother avoid infecting her infant with the flu? Is it possible to breastfeed at a fever? Are breastfeeding and medications compatible, and can antibiotics be used for nursing mothers?
The most common questions are answered by an infectious disease doctor at Clinical Hospital No. 15, Podolsk District, Kiev and the State Scientific Institution “Scientific and Practical Center for Preventive and Clinical Medicine” of the State Administration of Affairs, assistant at the Department of Internal Diseases of the Institute of Ecology and Medicine, Ph.D. Lidia Mikhailovna Vovk.
How to avoid infecting a child if a nursing mother gets the flu?
If a nursing mother gets sick with the flu or a cold, the most important point must be taken into account: the presence of intoxication. If intoxicated, it is better to refrain from breastfeeding for several days. It is necessary to observe the so-called cough etiquette, respiratory etiquette, if at all possible with such fairly close contact.
There is a very serious nuance: for the majority of the population and even doctors, flu and colds seem to be identical concepts. Actually this is not true. Influenza is a severe infectious disease accompanied by high intoxication, fever, and catarrhal syndrome. A cold has a completely different course. Many other viruses can also cause respiratory diseases that are less dangerous to the health of both mother and child. They are accompanied by less pronounced intoxication and respiratory syndrome, which is why we are again inclined to individualize the approach in each specific situation.
However, the general rule is this: if there is a fever, you need to stop breastfeeding for a while and protect the child from contact with yourself as much as possible, observe respiratory ethics and then look at the situation.
Tell me, how to properly treat the flu if the mother is breastfeeding?
Proper treatment for the flu means consulting the doctor who is next to you. Because it is not correct to give such remote advice.
It must be remembered that flu and colds are different diseases. The approach is simple: the mother must be treated by reducing the temperature and intoxication, and symptomatically - respiratory syndrome. It is advisable to protect the mother from using any medications.
It is very important to evaluate the risks and benefits of using medications, possible side effects, as well as what will happen to the mother and how she will feel if the medications are not used.
For respiratory manifestations, it is also best to limit the use of medications as much as possible. But it all depends on the severity of the mother’s condition, on the course of the disease, and in some cases there may be a question about stopping breastfeeding and using serious medications to save life, improve the condition and health of the mother.
What is the safest way to reduce a high fever in someone who is breastfeeding?
To reduce the temperature, physical methods come first: rubbing with cool water, wrapping. A simple method such as a cleansing enema is quite effective. If these methods do not help, then it is necessary to use medications.
It is difficult to answer the question of which medications can be used while breastfeeding. Widely known antipyretics are labeled “with caution” or “not advisable.” But again, we're talking about the potential risk of not taking them and the potential risk that some side effects might bring.
What antibiotics are allowed while breastfeeding?
There are no completely safe medications. Today, all drugs are considered potential hepatotoxic, toxic, and we can only talk about the degree of their toxicity. Absolutely all manufacturers indicate in their instructions recommendations regarding the possibility of use during pregnancy and lactation.
The American Bureau of Food and Drug Control (FDA) has developed its safety scale for the use of drugs in pregnant women and lactation. This scale has five gradations: A, B, C, D and X. X is something that causes a clearly bad effect on the child, and all the rest either have not been conducted any serious safety studies, or the issue of risk is being considered when using these or other antibiotics.
Almost all antibacterial and antiviral substances belong to category B or C. During lactation, lactation can be used and maintained using drugs from the penicillin group, cyclosporine group and some macrolides. Antibiotics should only be prescribed by a doctor and the potential risks, benefits and optimal choice of drug should be assessed.
REMANTADINE, RIBOVIRIN, ARBIDOL, Oxylococcinum and influenza. Can these drugs be used by breastfeeding women?
Ribovirin, remantadine, arbidol and all the others have contraindications for lactation.
With regard to drugs of the interferon group, which are used both intramuscularly, subcutaneously and nasally, this contraindication does not really apply to administration through the nose, but as for parenteral administration (intramuscular, subcutaneous), according to the FDA classification, interferons are classified as category C and not recommended for lactation.
Regarding homeopathic medicines, I adhere to the point of view that during pregnancy and lactation it is advisable to take fewer medications, especially if you can do without them altogether. And in situations where they are really needed, it is better to use more serious, officially approved drugs that have a more effective effect.
source