How the umbilical cord attaches to the placenta
The normal option for fixation is the departure of the umbilical cord from the center of the child's place. Anomalies are called lateral, marginal, shell attachment of the “cord”. It is best to examine them in the 2nd trimester using ultrasound diagnostics, when the placenta is on the anterior or anterolateral uterine wall. When it is localized on the posterior wall, it may be difficult to determine. The use of color Dopplerography makes it possible to recognize the exact variant of the pathological exit of the cord to the child's place.
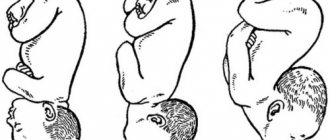
Let's consider several types of abnormal fixation of the umbilical “cord”:
- Central - in the middle of the inner surface of the placenta. Occurs in 9 out of 10 pregnancies and is considered a normal option.
- Lateral (eccentric) - not in the center, but on the side of the embryonic organ, closer to its edge.
- Marginal - from the edge of the placenta. The umbilical arteries and vein pass to the child's place close to its periphery.
- Tunicale (pleated) - attached to the membranes of the fetus without reaching the placenta. The vessels of the umbilical cord are located between the membranes.
Umbilical cord entanglement
The expectant mother is always worried that the pregnancy will proceed without any complications and that the baby will develop systematically and according to indications. Therefore, it is not surprising that such a relative deviation from the norm as entwining the umbilical cord of the fetus makes the pregnant woman worry.
The situation is also aggravated by all sorts of frightening stories from gossips about how dangerous and how undesirable entanglement is for a child.
Modern medicine can already work almost miracles: doctors provide optimal management of pregnancy in the presence of entanglement, and successfully complete the delivery process without harm to the mother and the baby. Which once again confirms the popular wisdom that the devil is not as terrible as he is portrayed.
Causes of umbilical cord entanglement
The umbilical cord, in addition to the placenta, is the main “link” between mother and child. Through the umbilical cord, the fetus receives oxygen, all the necessary nutrients, vitamins and microelements. The umbilical cord is fully formed around the 14th week of pregnancy and normally its length is about 40-60 centimeters.
At the same time, the length of the umbilical cord is determined genetically: that is, its indicators will be equivalent to the indicators of the umbilical cord that once connected the pregnant woman to her mother. So, entanglement with the umbilical cord is typical precisely in the case when its length exceeds the norm, and reaches over 70 centimeters.
Polyhydramnios can also cause entanglement. But the presence of the mentioned factors does not always lead to confusion for the baby. Moreover, sometimes entanglement occurs accidentally, for no apparent reason.
Why is entanglement in the umbilical cord dangerous?
You can detect the entanglement of the umbilical cord starting from the 17th week of pregnancy. But, if its fact has been established, this does not mean that the entanglement will remain until the end of pregnancy: the baby, just as it is entangled, can, by constantly moving, unravel on its own.
The umbilical cord can wrap around the baby’s body, limbs, and neck; and even in the latter case, it is not dangerous for the fetus - the child in the womb does not breathe through the lungs, oxygen comes to him through the umbilical cord.
That is, if the vessels in it are not pinched, then the fetus receives nutrients in full. The situation is aggravated only if, when the umbilical cord is entangled, the vessels are also compressed, as a result of which blood flow is disrupted.
What is the marginal attachment of the umbilical cord?
Marginal deviation means fixation is not in the central zone, but in the peripheral zone. The umbilical arteries and vein enter the child's place too close to the very edge. Such an anomaly usually does not threaten the normal course of pregnancy or childbirth, being considered a feature of a specific period of gestation.
Experts say that marginal discharge is not an indication for a cesarean section: natural delivery is carried out. This attachment does not increase the risk of complications for the mother or baby. However, when doctors try to isolate the placenta by pulling the umbilical cord, the latter may come off.
Making a diagnosis
To make sure that Yulia’s baby is feeling well, we recorded a cardiotocogram (CTG). CTG records the cardiac activity of the fetus, which is an informative indicator of its intrauterine state. To do this, a sensor was attached to the expectant mother’s stomach, which is connected to the device. Yulia lay on the bed on her side for 30 minutes while the machine recorded the fetal heartbeat. No pathological changes were detected on CTG. Together with Yulia, who had already calmed down somewhat and cheered up, we went out to her relatives who were waiting for her. I explained to them that in this situation, when we have a premature pregnancy, the intrauterine state of the fetus is completely normal, it is not advisable to carry out an emergency delivery just because of the entanglement of the umbilical cord. The reassured pregnant woman went home with her husband and mother-in-law.
To fully determine the intrauterine state of the fetus, it is necessary to conduct a set of studies, which includes:
- ultrasound examination, in which it is possible to see or suspect entanglement of the umbilical cord neck or other parts of the fetus, since in some cases it is very difficult to distinguish whether the umbilical cord loops are located near the fetal neck or there is entanglement: with this study we do not have the possibility of a three-dimensional image that allows us to examine the object from all sides - for example, looking back. It should be noted that it is not possible to determine the length of the umbilical cord using ultrasound data during pregnancy, since the umbilical cord is, as it were, “curled” in the tight space between the baby’s body and the wall of the uterus;
- Doppler ultrasound is a method that allows, firstly, to accurately determine whether there is entanglement in the umbilical cord, since the movement of blood flow is displayed in a color image, and secondly, to diagnose the speed of blood flow in various vessels of the uteroplacental complex;
- cardiotocography, which allows you to determine not only the baby’s heart rate, but also his reaction to his own movements (when recording CTG during pregnancy) and to an increase in the tone of the uterus (during childbirth), which allows you to find out how well the fetus is feeling at the moment .
If, after carrying out the entire complex of examinations, it is determined that the baby feels satisfactory, then the fact of entanglement with the umbilical cord alone is not an indication for surgical delivery. Such indications can arise either when there are signs of oxygen deficiency (fetal hypoxia), or when umbilical cord entanglement is combined with other indications for cesarean section.
Possible reasons for this condition
Experts consider the main cause of pathological attachment to be a primary defect in the implantation of the umbilical cord, when it is not localized in the area of the trophoblast that forms the baby's place.
Risk factors for anomalies are:
- First pregnancy;
- Young age, not exceeding 25 years.
- Excessive physical activity combined with a forced vertical position of the body.
- Obstetric factors - oligohydramnios, polyhydramnios, weight, position or presentation.
Most often, abnormal fixation of the umbilical cord occurs simultaneously with several variants of cord pathology - true nodes, non-spiral arrangement of vessels.
The meningeal site of attachment of the cord between the mother and the fetus is fixed much more often when a woman is carrying twins or triplets, or during repeated births. Often such an anomaly accompanies malformations of the child and organs: congenital uropathy, esophageal atresia, heart defects, a single umbilical artery, trisomy 21 in a baby.
Is it possible to avoid umbilical cord entanglement?
Considering the factors predisposing to umbilical cord entanglement, the expectant mother is advised to minimize stressful situations, breathe fresh air more often, and do gymnastics, not forgetting about breathing exercises. All these measures are aimed at ensuring that the child does not experience a lack of oxygen, that is, hypoxia, which causes increased motor activity of the fetus.
In addition, you need to promptly and accurately follow all doctor’s orders and undergo examinations - this will allow you to suspect problems in time and prevent undesirable consequences. You can also advise the expectant mother not to take the scary stories of “well-wishers” to heart, not to use unknown drugs and not to perform acrobatic exercises in order to “remove” the umbilical cord loop.
What is the danger of diagnosis?
The marginal variant of the exit of the umbilical cord is not considered a serious condition. Doctors pay attention to such localization of the “cord” attachment in the case when the umbilical cord is located at a distance not exceeding half the radius of the child’s seat from the edge. This situation causes the development of obstetric complications.
For example, the radius of the placenta is 11 cm. If the cord in this form does not exceed 5.5 cm from the edge, close monitoring of the child’s condition is necessary: there is a high risk of developing oxygen starvation in the womb. For this purpose, medical workers monitor the movements of the babies and conduct CTG at least 2 times a week throughout the entire gestation period.
The shell version poses a much greater threat. The disorder is more typical for multiple pregnancies. The vessels are located between the membranes, are not covered with Vartan jelly, and fibrous tissue is also less developed there. For this reason, they may not be protected from damage during childbirth.
Pathologies
Doctors identify several abnormal variants of attachment of the umbilical cord to the placenta. Thus, the umbilical cord can be directly attached to the edge of the placenta. Experts call this attachment marginal. This condition is characterized by the fact that the blood vessels located in the umbilical cord are located quite close to the edge of the placenta.
Lateral attachment of the umbilical cord to the placenta is not always the reason leading to the development of dangerous complications during pregnancy. Obstetricians-gynecologists especially highlight the condition in which the umbilical cord is located at a distance of less than 0.5 radius of the placenta from the edge. In this case, the risk of developing various complications is quite high.
Another clinical option for attaching the umbilical cord to the placenta is tunical. This condition is also called spiny. In this case, the blood vessels that are located in the umbilical cord are attached to the amniochorial membrane.
Normally, the arterial vessels that are located in the umbilical cord are covered with Wharton's jelly. This gelatinous substance protects the arteries and veins that are present in the umbilical cord from various damages. When the umbilical cord is attached to the placenta, the blood vessels are not covered with Wharton's jelly along their entire length. This contributes to the fact that the risk of developing various traumatic injuries to arteries and veins is quite high.
According to statistics, sheathed umbilical cord attachment occurs during pregnancy with one baby in approximately 1.2% of cases. If the expectant mother is expecting twins, then in such a situation the risk of developing this pathology increases and is already almost 8.8%.
In obstetric practice, there are cases when the umbilical cord can change its attachment to the placenta.
The reasons for this may be different. This may be due to inaccuracies in determining the initial site of attachment of the umbilical cord to the placenta (the notorious human factor), as well as due to the migration of placental tissue during pregnancy. Note that changes in the location of the umbilical cord still occur infrequently.
How is pregnancy progressing?
With marginal attachment, the gestation period and subsequent delivery are most often not accompanied by the development of any complications. With the membrane variant, intrauterine hypoxia occurs during pregnancy with the subsequent development of growth retardation. The risk of premature birth increases.
With sheath fixation of the umbilical cord, damage to the arteries and veins sometimes occurs during gestation. This is accompanied by bleeding from the genital tract in the expectant mother and such manifestations as oxygen deficiency in the baby, rapid heartbeat followed by a decrease, muffled heart sounds, and the passage of meconium during cephalic presentation.
If symptoms appear, seek medical attention immediately to avoid maternal and fetal complications.
Is the umbilical cord entwined visible on ultrasound?
A year has passed, I still can’t come to my senses, I remember and think: was the tight entanglement really not visible on the ultrasound before the birth. Or did the ultrasound specialist get caught blind?
Mobile application "Happy Mama" 4,7
Communicating in the app is much more convenient!
It’s generally visible... but maybe he got confused just before the birth?
if it’s visible and strong, then they send you for a caesarean section and don’t take any risks, but no one saw me personally either, and before giving birth they put devices on my stomach and on the monitor, and my heart, like normal, doesn’t beat faster, etc. but it turned out to be even sadder
They saw it right away on my ultrasound
probably the ultrasound specialist is blind(
It’s been almost a year for me, I also don’t understand... I didn’t do any ultrasounds, paid or free, both externally and internally, they didn’t see anything, they said it wasn’t entwined. And I gave birth, they barely saved it, it turned out to be 4 times and tight
it’s visible, of course, but it doesn’t affect the birth, the main thing is to untangle it right away, instantly, after the baby comes out of you
It affects childbirth and how, if it’s protracted or something else, then you can lose the child. Because when he comes out, the umbilical cord puts more pressure on him and suffocates him
The baby in the birth canal is not breathing on its own yet! what kind of strangulation?
everything is there through the umbilical cord even at this time! except that the umbilical cord is pinched so that nothing comes in, but I can’t imagine how tight it must be... TTT
what are you doing? what a suffocation! the entanglement is very serious, cerebral circulation is disrupted, the flow of nutrients into the body and oxygen itself through the blood vessels is disrupted. With severe suffocation, serious health problems are possible in the future, such as strabismus, stuttering, cerebral palsy and many many others. How many times have I been to childbirth, I have seen enough of everything and then I know about the consequences
The consequences of being entangled in the umbilical cord may occur during childbirth. This may be hypoxia during childbirth and asphyxia after childbirth. In severe extreme cases, respiratory arrest may occur. The consequences of entanglement in the umbilical cord may also include microtrauma of the cervical spine. The symptoms of this damage are insignificant and can manifest as headaches, neck pain, and curvature of the spine subsequently.
When the umbilical cord is entwined during childbirth, all measures are taken, the fetal heartbeat is monitored, when the head appears, the midwife loosens the loop with her fingers, and after birth she immediately unwinds the umbilical cord. If the entanglement is very tight, then an emergency caesarean section is performed. Double and triple entanglements are especially dangerous. Tension of the umbilical cord during childbirth is dangerous due to premature placental abruption. (taken from the Internet because it’s long to write and that’s actually what I meant)
Peculiarities of childbirth with velamentous umbilical cord attachment
Such an anomaly in the origin of the cord is accompanied by a high risk of damage to the umbilical vessels, followed by fetal bleeding and rapid death of the child. To prevent their rupture and death of the baby, timely recognition of the pathological variant of the “cord” exit is necessary.
Natural childbirth requires good specialist skills and constant monitoring of the baby’s condition due to the high risk of death of the mother and baby. Childbirth should be quick and gentle. Sometimes the doctor can feel the pulsating arteries. The doctor opens the amniotic sac in a place so that it is distant from the vascular zone.
If there is a rupture of the membranes with blood vessels, a pedunculated rotation and extraction of the fetus are used. When the head is in the cavity or pelvic outlet, obstetric forceps are used. These benefits can only be applied when the child is alive. To avoid adverse consequences, specialists choose surgical intervention - caesarean section.
Childbirth
In case of complete placenta previa, even in the absence of bleeding, a cesarean section is performed at 38 weeks of pregnancy, because Spontaneous birth is impossible in this case. The placenta is located on the path of the baby’s exit from the uterus, and if an attempt is made to give birth on its own, its complete detachment will occur with the development of very severe bleeding, which threatens the death of both the fetus and the mother.
The operation is also used at any stage of pregnancy if the following conditions are present:
- placenta previa, accompanied by significant bleeding, life-threatening;
- repeated bleeding with anemia and severe hypotension, which are not eliminated by the prescription of special medications and are combined with impaired fetal condition.
A caesarean section is routinely performed at 38 weeks when partial placenta previa is combined with another pathology, even in the absence of bleeding.
If a pregnant woman with partial placenta previa carries the pregnancy to term, in the absence of significant bleeding, it is possible that the birth will occur naturally. When the cervix is dilated by 5-6 cm, the doctor will finally determine the variant of placenta previa. With a small partial presentation and minor bleeding, the amniotic sac is opened. After this manipulation, the fetal head descends and compresses the bleeding vessels. The bleeding stops. In this case, it is possible to complete the birth naturally. If the measures taken are ineffective, the birth is completed promptly.
Unfortunately, after the baby is born, there remains a risk of bleeding. This is due to a decrease in the contractility of the tissues of the lower segment of the uterus, where the placenta was located, as well as the presence of hypotension and anemia, which were already mentioned above. In addition, it has already been said about the frequent combination of previa and tight attachment of the placenta. In this case, after childbirth, the placenta cannot completely separate from the walls of the uterus on its own, and a manual examination of the uterus and separation of the placenta must be performed (the manipulation is carried out under general anesthesia). Therefore, after giving birth, women who have had placenta previa remain under the close supervision of hospital doctors and must carefully follow all their recommendations.
Infrequently, but there are still cases when, despite all the efforts of doctors and a cesarean section, the bleeding does not stop. In this case, you have to resort to removing the uterus. Sometimes this is the only way to save a woman's life.
Norm
The umbilical cord, or, as it may also be called, the umbilical cord, is an elongated flagellum, inside which blood vessels pass. They are necessary to ensure that the fetus, during its intrauterine life, receives all the necessary nutrients for growth and development. The normal umbilical cord appears as a gray-blue cord that is attached to the placenta. Normally, it is formed in the very early stages of pregnancy and continues to develop along with the growing baby.
The umbilical cord can be easily visualized already in the 2nd trimester of pregnancy. It is well determined during an ultrasound examination. Also, through ultrasound, the doctor can assess the condition of the actively developing placental tissue. During the examination, the doctor must also evaluate how the umbilical cord is attached to the placenta.
The umbilical cord is finally formed only by 2 months from the moment of conception. As the umbilical cord grows, its length also increases. At first, the umbilical cord is only a few centimeters long. It gradually increases and reaches, on average, 40-60 cm. The length of the umbilical cord can be definitively determined only after childbirth. While the baby is in the mother's womb, the umbilical cord may curl somewhat.
Abnormalities of the placenta
“Children’s place” is the main “organ” that is necessary for the normal development and growth of the baby. It is through the placenta and the umbilical cord that the relationship between the fetus and the woman is carried out - nutrients are supplied for the “construction” of a new organism, as well as oxygen. The formation of the placenta and umbilical cord occurs before 16-18 weeks.
Exposure to unfavorable factors during this time leads to various abnormalities of the placenta and umbilical cord, which can affect the subsequent development of the fetus, the course of pregnancy and even childbirth. Chromosome pathologies of the fetus can also lead to developmental anomalies, therefore, if abnormalities are detected, all pregnant women undergo consultation with a geneticist to determine the likelihood of such diseases.
Development
The following types of placental development disorders are distinguished:
- Hypoplasia . This reduction in size can be primary or secondary. A similar condition develops with genetic abnormalities of the fetus, with a constitutionally small child (for example, if the parents are short and thin).
- Secondary hypoplasia develops against the background of intrauterine fetal hypoxia with insufficient supply of nutrients and oxygen, for example, if a woman abuses alcohol or nicotine, has arterial hypertension that cannot be corrected, and in many other conditions. Secondary hypoplasia is almost always associated with delayed fetal development - symmetrical and asymmetrical (IUGR of varying degrees).
Ultrasound is performed to diagnose abnormalities of the placenta and umbilical cord
- Hyperplasia . This is an increase in the size of the placenta above the average for the period being measured. May be the norm, for example, in tall women with “good” weight. It can also occur against the background of somatic diseases of the mother - most often it is diabetes mellitus, while the fetus also has an abnormally large size due to impaired carbohydrate metabolism.
- False placental hyperplasia occurs when the chorionic villi swell. This condition develops with intrauterine infection of the fetus - with previous syphilis, sexually transmitted infections, with toxoplasmosis during gestation, with fetal hydrops during Rhesus conflict. In this case, the fetal tissues may also swell, which is noticeable during ultrasound examination.
- Pathology of placental thickness . “Children’s place” can be “thin” or “thick” for a given period. Thin is associated with hypoplasia (primary secondary underdevelopment), thick - with hyperplasia (excessive growth or tissue swelling).
- A thick placenta has a more favorable course and a better prognosis for the fetus. Thin can be combined with developmental defects, chromosomal abnormalities in the fetus, intrauterine growth retardation and dementia after birth.
- Different number of slices . Normally, the placenta is represented by tissue of one area, somewhat reminiscent of a “pancake”. Sometimes several lobules are found, for example, as if two/three separate parts - bilobed/trilobed.
- More dangerous for the course of the postpartum period is the presence of an anomaly in the development of the placenta - an additional lobule. It is usually small in size and located somewhat separately from the main part of the placenta. During labor, it tends to remain in the uterus, causing heavy bleeding.
- Abnormal shape . Normally, the placenta has the shape of a circle. Bean-shaped, oval, encircling, with a “belt”, “fenestrated” and other options are considered pathological.
Expert opinion
Daria Shirochina (obstetrician-gynecologist)
Anomalies in the development of the placenta may be associated with an initially multiple pregnancy, which later turns into a single pregnancy if one fetus freezes and its chorion remains and atrophies.
Attachments and Locations
Such features of the placenta are associated with various factors - the presence of fibroids, postoperative scars, and a history of inflammatory processes of the endometrium. The ideal location of the placenta is along the posterior wall of the uterus at the fundus. This is the most favorable course for both natural and surgical childbirth.
Location along the anterior wall and in the bottom is also considered normal, but can present difficulties during childbirth, and the risk of bleeding and complications increases. The following abnormalities of placental attachment are also detected:
- Low placentation . Detected in the early stages (20 weeks and later). It is considered the most favorable option among other anomalies of placental attachment. At the same time, the “baby place” is located close to the cervix, but within acceptable limits - each period has its own norms.
- Regional presentation . In this case, the area of the placenta is located at the edge of the internal os of the cervix; there is a higher risk of bleeding during gestation and childbirth.
- Central presentation . This is the most dangerous option for the location of the placenta. In this case, the “baby seat” is located directly above the internal os, blocking the path for natural childbirth. Delivery is possible only by caesarean section. Moreover, during them and throughout pregnancy, the risk of bleeding is extremely high, without previous symptoms and against the background of complete well-being and physical calm.
Maturation
There are early and late maturation of the placenta. In the first case, calcifications and other signs of “aging” are detected. Most often, this is diagnosed after 30 weeks. Sometimes signs of early maturation are an indication for early delivery in order to save the fetus.
Late maturation is less common. Most often it is associated with incorrectly set deadlines, as well as the individual characteristics of the woman and baby. Late maturation is more often diagnosed in children whose mothers suffer from diabetes or suffered syphilis during pregnancy. This increases the risk of mental impairment in the fetus after birth, as well as the risk of stillbirth.
Tumors of the placenta
This pathology is extremely rare. The following are found:
- hemangioma (chorioangioma) - formation from the vascular tissue of the placenta;
- hamartomas are tumors of germinal tissue.
As a rule, these tumors do not pose a particular danger to the fetus, but can serve as “traps” for blood, so the baby may suffer from a lack of oxygen and nutrients.
Other violations
Placental infarction is also possible - with signs of abruption in the early or late stages. Such areas after the birth of the placenta appear whitish, as they do not participate in the development of the fetus.
Inflammation is an acquired abnormality of the placenta. It occurs during intrauterine infection - pathogenic microbes enter ascendingly - through the mother's blood, and also descending - through the cervical canal from the vagina.
There is also partial or complete germination of the placenta into the uterine tissue - into the myometrium. This is a serious pathology that threatens the life of the woman and the fetus, especially during childbirth. Germination can occur anywhere, but more often - after a cesarean section in the scar area. Childbirth is possible only through a caesarean section, and often it ends with the removal of the uterus to save the woman’s life.
Watch this video about the structure of the placenta: