05/18/2019 The disease “rheumatoid arthritis” can affect a significant part of the world’s population. It is “not indifferent” to women three to four times more than to the stronger sex, so ladies more often become its victims.
Due to the significant rejuvenation of this disease, neither very young people, nor middle-aged people, nor patients who have celebrated their half-century anniversary are now immune from it. It often happens that the disease starts when a person is no more than 30-35 years old, but its insidious destructive effects appear decades later.
Rheumatoid arthritis: causes
Although the disease has long been known to people, why it occurs is still not entirely clear. Research suggests several reasons.
One of the most popular hypotheses is autoimmune. According to it, after a person has had infectious diseases, antibodies to these viruses remain in the joints. The immune system mistakes them for enemy agents and tries its best to rid the body of them. The struggle is so active that the joints that “fall under attack” suffer. There are also opinions that connect rheumatoid and infectious arthritis, considering the first to be a continuation of the second. Be that as it may, the disease has not been studied enough, and rheumatoid arthritis requires careful study, which should suggest new ways of treating it. Suggestions have also been made about the connection between systematic stress, hormonal imbalances, and pathological flora in the intestines with the onset of the disease. It has become fashionable to talk about hereditary and genetic factors as catalysts for illness. Thus, there are many hypotheses, which of them corresponds to the real state of affairs - medical scientists have yet to find out.
No complications
It is the task of specialists to find out what causes rheumatoid arthritis in a particular case. The task of patients is to promptly detect symptoms of inflammation and seek help, and then follow all the instructions of the attending physician. If this condition is not met, complications of this disease may develop. These include the following problems: contractures (local restrictions on joint mobility) and structural deformation up to disability. Complications can also be systemic:
- malfunction of the spleen, which causes abnormal destruction of blood cells;
- deposition in the kidneys of amyloid, a pathological protein that blocks kidney structures and disrupts their functioning;
- eye diseases;
- vasculitis;
- osteoporosis.
There is no universal cure, as well as ideal prevention, for rheumatoid arthritis. And even avoiding stress, infections, hypothermia and injuries, a person who received a defective gene in the genetic “lottery” will not be 100% protected from the development of one of the types of inflammatory vascular damage called rheumatoid arthritis.
Rheumatoid arthritis: symptoms, causes, diagnosis, treatment
Polyarthritis, that is, simultaneous inflammation of several joints, is one of the most eloquent signs of this particular joint disease. In addition, symmetrical inflammation is observed. If the joint of the right wrist begins to hurt, then the left one is also involved in the process. The joints hurt, look swollen, and the skin over them is red. In the morning, movements in the diseased joints are constrained, and the limbs move poorly. The longer you ignore the disease, the more deformation the joints undergo:
- knees;
- neck;
- stop;
- brushes;
- elbows;
- wrists.
The disease either goes away or attacks the patient with renewed vigor, so doctors note the undulating course of the disease.
The effect of arthritis on the musculoskeletal system
If you have arthritis, it is better to avoid putting stress on your spine
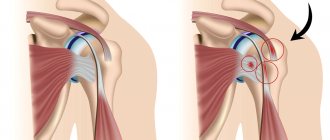
The first complications of the disease spread to the musculoskeletal system. Disruption of one joint due to inflammation leads to the development of complications of rheumatoid arthritis in other joints. This is especially evident when the lower extremities are affected.
Inflammation of the knee or ankle joint significantly limits mobility in this joint. With arthritis, it is necessary to immobilize the affected joint to stop the pathological process. As a result, the patient must walk with a cane or crutch. This entails a redistribution of the body load on the healthy leg. Since an immunopathological process occurs in the body, the increased load on a healthy joint causes immune cells to attack it, resulting in inflammation that affects the joints symmetrically.
Moving with a cane or crutch increases the load on the elbow joints and hands. This entails increased pressure on these joints and can also cause inflammation in the stressed area.
Thus, rheumatoid arthritis, which affects one large joint, spreads over time, affecting all new joints. So the disease can affect all small and large joints, including the hands, feet and spine.
Syndromes in rheumatoid arthritis
In addition to the traditional symptoms of the disease, there are also its syndromes:
- juvenile arthritis - typical for young patients whose age has not yet reached 16 years;
- Felty's syndrome was described in 1929 by A.P. Felty, whose name it received. The specificity of the course of the disease in this syndrome is that in addition to articular pathology, leukopenia is observed (white blood cells in the blood are less than normal) and the spleen is enlarged. At the time of description, it was typical for women over 40;
- Still's syndrome is a dangerous syndrome; here, in addition to direct joint disease and the accompanying high temperature, there is an increase in lymph nodes, disturbances in the functioning of the lungs and organs of the cardiovascular system.
Types of complications of arthritis and their characteristics
Many people ask: why is RA dangerous? RA predominantly affects women and is most often diagnosed between the ages of 40 and 70 years. Sometimes the disease can manifest itself much earlier. Babies also suffer from arthritis. This form of arthritis is called “juvenile”. The pathogenesis of arthritis is not fully understood.
Chronic polyarthritis is a disease that causes inflammation in many joints. The disease manifests itself in the form of swelling, overheating and functional limitation of the affected joints. In the future, RA leads to complete destruction of the joints and deformation of the limbs.
At the onset of the disease, small joints (fingers or feet) are affected. In RA, the joints become inflamed “symmetrically” – on both sides of the body. Seronegative RA differs from seropositive RA by the absence of rheumatoid factor in the blood.
The cause of RA (seronegative and seropositive) is unknown. It is only known that RA causes immune system disorders. Currently, RA is classified as an autoimmune disease.
Inflammation of the joints is expressed in the form of pain, overheating of the joints, swelling, and sometimes effusions (the appearance of fluid in the joints). Unlike arthrosis, arthralgia usually occurs at rest and improves with exercise. Severe inflammation leads to arthralgia at night. Also typical for inflammatory joint diseases is severe morning stiffness, which lasts, depending on the severity and activity of the disease, until the end of the day, and sometimes even for several weeks.
Complications of RA depend on disease activity. Patients generally experience a general feeling of malaise, loss of appetite, loss of body weight, lethargy, depression, fatigue and low-grade fever. Outside of the joints, RA can affect soft tissue. Patients experience tendonitis, rheumatoid nodules, or bursitis.
RA very rarely affects internal organs. In this case, it leads to life-threatening complications. Examples of organ involvement in RA:
- rheumatic pleurisy;
- rheumatic pericarditis;
- rheumatic inflammation of blood vessels (vasculitis).
Vasculitis
The course of RA varies from patient to patient. Symptoms get worse over the years. Severe cases are characterized by the involvement of various organs and systems - the heart, lungs, hematopoietic system, lymphatic system, nervous system or blood vessels. If multiple organ complications occur, the prognosis is unfavorable.
The only way to positively influence the course of the disease and its possible long-term consequences is early treatment of the disease.
In the past, the consequences of RA have been significantly underestimated. Only recently has it become clear that chronic polyarthritis is a serious systemic disease, which, if left untreated, not only leads to long-term disability and desocialization, but also to a significant reduction in life expectancy.
RA was previously thought to be incurable. However, scientific views on the disease are currently changing radically. Current clinical trials show that new treatment approaches for chronic arthritis can put patients into complete remission.
Some studies even show that with effective antirheumatic therapy, bone damage can be completely inhibited. Timely effective therapy helps prevent damage to articular cartilage.
Epidemiological evidence suggests that severe RA has become less common in patients undergoing treatment. Clinical studies also show that even the increased risk of mortality in patients with an initially very poor prognosis is reduced to normal levels with optimally selected antirheumatic therapy.
Diagnosis of the disease
To distinguish this disease from many similar ones, the patient must undergo hardware diagnostics and undergo a series of laboratory tests. Diagnosis of rheumatoid arthritis is characterized by:
- clinical blood test and rheumatoid factor;
- Ultrasound of internal organs;
- joint fluid analysis;
- radiography;
- arthroscopy;
- MRI.
Examination of the patient can also be informative. Joint damage in rheumatoid arthritis is not the only sign of the disease. As a rule, dermatitis or vasculitis, conjunctivitis are detected, and disruptions in the functioning of the cardiovascular system and lungs are observed.
Respiratory system damage
The following problems with the respiratory system may occur:
Pleurisy
Inflammatory process in the serous membrane covering the lungs. Negative changes in the lungs are almost asymptomatic. Signs of damage are comparable to pneumonia.
Bronchiolitis
An inflammatory reaction occurring in bronchiolitis, which leads to disruption and difficulty breathing.
Damage to lung tissue by rheumatoid nodules
The formation of nodules occurs in the tissue of the lungs. The main sign of such a complication is the formation of a cough with blood particles. This is due to damage to the lungs as a result of exposure to rheumatoid nodules.
Interstitial lung pathologies
These include more than a hundred types of lung diseases based on the chronic accumulation of harmful particles in the alveoli, small bronchi, and lung matter. Such deposits lead to pulmonary fibrosis.
Hypertension
Characterized by increased pressure in the circulatory system. As a result, channels occur in the vessels of the lungs.
How to cure rheumatoid arthritis
So far medicine does not know the answer to this question. However, it is quite capable of significantly alleviating the course of the disease, slowing down the destruction of joints, improving their mobility, and preventing a person from becoming disabled. Many techniques have been developed to make the patient healthier. As a rule, they consist of a combination:
- drug therapy;
- compliance with diet instructions;
- health promotion;
- using the possibilities of physiotherapy and physical therapy;
- lotions, compresses, rubbing and other methods of alternative medicine can be used as auxiliary ones.
There is a surgical method to get rid of this disease, but it is resorted to as a last resort, replacing the worn-out joint with an artificial analogue.
What to do if a pathology is detected?
When making this diagnosis, there is only one tactic: treat immediately. The sooner active treatment begins, the higher the likelihood of a favorable course of the disease for the patient and the lower the likelihood of the manifestation of those complications described above. Previously, treatment was aimed at improving quality of life, reducing pain, and so on. This is due to a rather serious, complex and aggressive complex therapy that the patient needs. However, now the approach has changed and treatment is aimed at putting the patient into stable remission (when the disease seems to be put to sleep). This is more productive for a person’s full life and reduces the likelihood of pathological complications.
Science is constantly moving. Scientists and doctors do not stop searching for the causes and methods of the most effective treatment. We just have to believe in the best. Be healthy.
Physiotherapy
Modern methods of treating rheumatoid arthritis also include physiological procedures. They are almost as effective as biological treatments. Among all modern physiological methods, the following are most often prescribed:
- balneotherapy is a new method that facilitates the delivery of nutrients to the bone joint;
- magnetic therapy – reduces swelling, activates cartilage restoration;
- UHF (pulse therapy) – overcomes pain;
- ultrasound stimulates metabolic processes in bone tissue, eliminates swelling;
- electrophoresis - enhances the effect of painkillers and stops the deformation of bone joints.
Treatment principle
Treatment for arthritis includes symptomatic therapy, basic antirheumatic drugs and modern immunosuppressants (cytostatics).
Symptomatic therapy:
- non-steroidal anti-inflammatory drugs;
- glucocorticosteroids for external use;
- injections of glucocorticosteroids.
NSAIDs are used in various forms of release. Diclofenac and nimesulide tablets are effective in the initial stages, with moderate pain. Injections and ointments with anti-inflammatory components are used for severe pain and inflammation of the joint.
Glucocorticosteroids will be prescribed only in severe cases, since they have a systemic effect on the entire body as a whole. The most common practice is to administer such drugs directly into the joint capsule. This allows you to quickly stop the inflammatory process, relieve pain and restore normal joint mobility.
Symptomatic therapy does not cure arthritis, but only alleviates its course. To stop the disease, it is necessary to take special groups of drugs, including immunosuppressants. The first-line drugs of choice are cytostatics. Such drugs belong to antitumor drugs that stop pathological cell division. Drugs in this group affect autoimmune processes, reducing the rate of progression of arthritis in women. In severe forms of the disease, it is advisable to use bioactive agents, for example, monoclonal antibodies. They effectively fight rheumatoid arthritis, affecting the cause of its occurrence. The only disadvantages are the high cost of such drugs and their insufficient prevalence in the CIS.
Additionally, the doctor may prescribe special exercises to restore joint mobility, physical education or manual therapy.
Unconfirmed reasons
Initially, research to identify the causes was carried out only in the direction of searching for the infection that causes the disease, since a narrow interpretation of the clinical picture was taken into account. Symptoms of the disease, expressed in sweating, fever, enlarged lymph nodes, weight loss, and acute onset, suggested an infectious cause. Also important was the misconception that rheumatoid arthritis and rheumatism are somehow related, and that streptococcal infection is to blame for its occurrence. That is why, in the middle of the last century, treatment was based on the principle of removing chronic infectious foci and preventing relapses.
Relapses or the appearance of other symptoms after acute respiratory viral infections and influenza also contributed to strengthening the view of infection as the cause of the disease. But, as it later became clear, it was a pseudo-allergic reaction, which is inherent in autoimmune diseases. The nature of this lies in the influence of infection antigens, high vascular permeability, when autoantigens and autoantibodies interact, etc.
A certain temporary connection between the manifestation of symptoms of joint inflammation and the emerging viral infection gave an erroneous direction to antibiotic therapy, and the name was given inaccurately: infectious nonspecific arthritis.
Several other versions were also put forward, but after careful research they were all rejected because they did not find their confirmation, these are:
- diphtheroid-like microorganisms,
- mycoplasma,
- intestinal microflora.