Home » Back diseases » Neuropathy » Varieties »
Distal diabetic neuropathy refers to non-inflammatory diseases in which peripheral nerves are damaged. Patients with diabetes are at risk.
What is autonomic diabetic polyneuropathy of the lower extremities in diabetes mellitus - this is one of the most common and serious complications of the disease. It manifests itself within five years after diagnosis of the disease and, if left untreated, quickly leads to disability .
Causes
The main culprit in diabetic neuropathy is high blood sugar. In diabetes, we are talking specifically about polyneuropathy, because the disease affects almost all nerves. Both the somatic nervous system, responsible for motor activity, and the autonomic nervous system , which controls the functioning of internal organs, suffer.
The mechanism of disease development is as follows:
- When blood sugar levels are constantly high, metabolic disorders occur.
- Tissues and cells are in a edematous state.
- Blood pressure increases.
- Blood cannot penetrate into vessels compressed due to edema.
- Small capillaries die first, then larger vessels.
- Due to poor blood supply, the functioning of internal organs is disrupted.
Provided that glucose levels are constantly monitored, neuropathy does not occur. Provoking factors for the development of the disease in diabetics:
- Old age of the patient . Neuropathy usually develops after age 50.
- Duration of the disease. The first signs of the disease appear 5-10 years after the onset of diabetes.
- Constant increase in blood pressure . Swelling of the capillaries is aggravated by increased pressure, and vasospasm occurs.
- Excess body weight.
- Non-compliance with the diet, leading to constant spikes in sugar.
- Consistently high levels of “bad” cholesterol.
- Bad habits of the patient (alcohol, smoking).
- Heredity . The likelihood of neuropathy increases to 30% if close relatives have suffered from the disease. It is believed that some people carry an altered gene in which neurons become much more sensitive to the effects of sugar, they are destroyed and become unable to transmit a signal.
- Limb injuries in which nerve endings are affected. In diabetes, regeneration processes are very poor, so damaged nerves are practically not restored.
- Type of diabetes . In patients with type 2 diabetes, neuropathy develops 2.5 times more often than in diabetics with type 1.
Mechanism of occurrence of violations
The functioning of organs, vessels and glands is carried out under the control of the autonomic (autonomic) nervous system. The somatic system is responsible for the delivery of sensory and motor information to the central nervous system. With sudden changes in sugar levels, they are damaged. It manifests itself as disruptions in the functions of the kidneys, heart, liver, and difficulty breathing.
The mechanism by which sugar levels affect the nervous system is multifaceted:
- a large amount of glucose is concentrated in the intercellular space and causes swelling of nerve tissue;
- the production of myoinositol decreases, and after it, phosphoinositol, which is designed to facilitate the conduction of the impulse, but ceases to cope with this, as a result, energy metabolism decreases;
- the production of free radicals, which have a toxic effect on cells, increases;
- the number of autoimmune complexes that inhibit the reproduction of nerve fibers and have a destructive effect on NS tissue increases.
The described mechanism is activated when blood glucose levels are high for a long time. With significant disturbances of the autonomic system, death is possible, and damage to the somatic system leads to severe pain.
Classification
Depending on which part of the nervous system is affected, the following types of diabetic polyneuropathy are distinguished in medicine:
- Generalized symmetrical.
- Autonomous.
- Multifocal, focal.
- Central.
Generalized symmetrical polyneuropathy
Important ! Characterized by damage to the nerve fibers responsible for movement and sensitivity. In this case, extensive symmetrical damage to the nervous system occurs.
In turn, this type of disease is divided into:
- Sensory neuropathy (the nerves responsible for sensitivity are affected).
- Motor (motor activity is impaired).
- Sensorimotor (combined). Both the patient’s motor and sensory abilities suffer.
- Hyperglycemic . The mildest type of the disease, after normalization of glucose levels, normal functioning of the nervous system is restored.
Autonomous
Autonomic neuropathy is a type of disease in which the innervation of internal organs is disrupted. Their blood supply deteriorates, the body ceases to function normally.
This is the most dangerous type of pathology, leading to death. Death occurs due to heart attack, renal, liver, or heart failure.
The autonomous type of illness combines the following types:
- Respiratory . The functioning of the respiratory system is impaired.
- Cardiovascular . The nerves of the heart and blood vessels are affected.
- Urogenital . The innervation of the urinary organs is reduced, so they work poorly.
- Gastrointestinal . The nerves responsible for the functioning of the gastrointestinal tract are destroyed.
- Endocrine . The activity of the endocrine system deteriorates, and hormonal imbalance begins.
Multifocal and focal
This is a rare form of neuropathy that affects the peripheral nervous system. In patients, tendon reflexes decrease and paresis of the limbs occurs. This type is characterized by slow progression, alternating periods of exacerbation and remission .
Focal form subtypes:
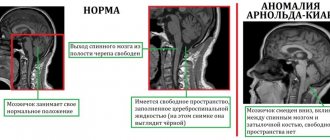
- Radiculoneuropathy . Damage to the spinal cord roots.
- Tunnel . The pathology extends to the radial, ulnar nerve, and carpal tunnel.
- Cranial . Affects the cranial nerves (oculomotor, auditory, facial).
Central
With central neuropathy, the process involves the brain and spinal cord. This is one of the most serious types of pathology. There is a change in brain functions. The result is:
- muscle weakness (myelopathy),
- encephalopathy,
- mental disorders.
A characteristic symptom is cerebrasthenic syndrome, expressed by neurosis-like conditions, depression, cognitive disorders, and phobias.
Attention ! It is impossible to reverse the destruction of the central nervous system. Treatment can only slow down the progression of the disease.
Forms
The disease occurs in different forms: motor, sensory and sensorimotor, depending on the location of the affected nerve endings.
Motor
Motor neuropathy refers to dysfunction of the motor nerves. The main symptoms are impaired movement and muscle weakness.
Sensory
In the sensory form, the main manifestations of the disease are associated with impaired sensitivity. For example, having touched a hot surface, the patient does not have time to feel the burning and pain and react to them by instinctively withdrawing his hand. As a result, the person gets burned. The same is true with other physical sensations - cold, touch, etc. The patient may not feel pain from the injury, tightness when wearing smaller shoes, or swelling of the feet.
Sensorimotor
This form of the disease combines signs of both motor and sensory neuropathy, i.e. problems with sensitivity are accompanied by difficulties with movement.
Sometimes an exclusively distal form of polyneuropathy manifests itself - one in which the work of only the external muscles is impaired. The second type of disease is visceral neuropathy, which is characterized by pathology of internal organs. In their pure form, the distal and visceral forms rarely appear. In addition, as the disease progresses, the presence of one of them often provokes the development of the other.
Signs of damage to the nervous system
It is quite difficult to determine whether a patient has diabetic neuropathy. The disease occurs latently for a long time, the symptoms go unnoticed. Pathology can be suspected based on active and passive signs.
| Active | Passive |
| Sharp pain along the nerve | Stiffness of the limbs |
| Burning sensation in the arms or legs, back. | Lack of skin sensitivity |
| A tingling sensation of needles in the affected area | Feeling of "cottoniness" in the arms and legs |
| Allodynia syndrome (pain from even the slightest touch) | Unsteady gait |
| Reduced pain threshold | Deterioration of vision, hearing, cognitive disorders. |
Timely consultation with a doctor at the stage of indirect signs increases the chances of restoring the functioning of the nervous system by 50%.
Patient examination
Neurologists at the Yusupov Hospital make a diagnosis of “diabetic polyneuropathy” based on the patient’s complaints and neurological symptoms.
Clinical examination of the foot includes assessment of vascular status, biomechanics and structure of the foot, and integrity of the skin. Endocrinologists and neurologists recommend that patients with diabetes undergo examinations for the presence of diabetic polyneuropathy once a year, even in the absence of complaints. If there is a suspicion of peripheral nerve damage, examination should be performed at least once every 6 months. Regular examinations make it possible to detect the disease at an early stage and begin adequate therapy in a timely manner. Since it is impossible to identify diabetic polyneuropathy using one research method, doctors at the neurology clinic conduct a comprehensive examination. It includes visual examination, laboratory and instrumental diagnostic methods. Typically, the patient undergoes a comprehensive examination by a therapist, endocrinologist, neurologist and vascular surgeon. Doctors study the following indicators:
- blood pressure level in the extremities;
- severity of reflexes;
- skin sensitivity;
- presence of edema;
- condition of the skin.
In some cases, the disease is asymptomatic, but this does not mean that patients with diabetes do not have damage to peripheral nerve fibers. To identify the pathological process at the preclinical stage, neurologists at the Yusupov Hospital prescribe electromyography and quantitative sensory testing. The latter method allows you to most accurately determine the condition of the sensory nerves, taking into account the weight, height and age of the patient. Laboratory tests for diabetic angiopathy include the following tests:
- determination of glucose levels in blood plasma;
- cholesterol test;
- identifying the level of toxic substances that are in the body.
Also at the Yusupov Hospital, neurologists conduct the following instrumental studies:
- magnetic resonance imaging;
- electroneuromyography;
- nerve biopsy.
Analysis of research results makes it possible to establish an accurate diagnosis before the appearance of clinical signs of diabetic polyneuropathy or at the onset of the disease.
Symptoms of the disease
Depending on which nerve fibers are damaged, the patient develops different symptoms.
1. Signs of central neuropathy:
- Slowly progressive dementia (encephalopathy). It manifests itself as a decrease in memory, deterioration in thinking and imagination. It becomes difficult for the patient to solve first complex, then simple problems.
- Cerebrasthenic syndrome , expressed in frequent neuroses, depression, phobias, nightmares. The patient feels depressed and apathetic.
- Autonomic manifestations : tinnitus, dizziness, headache, mental disorders, slow pace of physical and mental activity.
2. Symptoms of the autonomous type of disease.
Manifestations depend on which organs’ innervation is impaired:
- The cardiovascular type is characterized by: heart rhythm disturbances, blood pressure surges, painless heart attack, stroke, increased heart rate at rest.
- Urogenital pathology is expressed in urinary retention, erectile dysfunction, frequent cystitis, pyelonephritis, and menstrual irregularities in women.
- In the gastrointestinal form, symptoms such as heartburn are present;
- difficulty swallowing;
- biliary dyskinesia;
- gastroparesis;
- stomach ulcer;
- disturbance of intestinal motility, leading to diarrhea or constipation, fecal incontinence.
3. Symptoms of peripheral.
The first signs do not appear immediately. This is explained by the fact that healthy nerves, up to a certain point, partially compensate for the functions of the sick. Then the following symptoms occur.
Sensory impairments:
- Distortion of sensitivity. A person may experience pain from the slightest touch and, conversely, be absent from strong physical impact.
- Tingling, burning in the extremities.
- Impaired temperature perception (extremities freeze at normal external temperature).
- An unpleasant taste in the mouth.
- Sensitivity to odors.
- Decreased twilight vision.
- "Socks and gloves syndrome." The patient feels as if they are wearing something on their arms and legs.
Motor disorders:
- Unsteadiness when walking. The patient feels like his legs are like cotton wool and is afraid of losing his balance.
- Impaired coordination . Movements are unclear, chaotic.
- Muscle cramps, especially at night.
- Joint stiffness . First, it is difficult to straighten the little fingers, then the remaining fingers. Due to malnutrition of the bones, inflammation and pathological growth occur.
- Muscle weakness. It becomes difficult for the patient to hold objects and stand on his feet for a long time. After some time, muscle atrophy occurs.
Endocrine disorders
- First of all, the work of the sweat glands is disrupted. The patient suffers from excessive sweating and redness of the skin at normal temperatures. Over time, the sweat glands begin to produce little sweat due to capillary spasm. The patient develops dry skin and age spots appear . The skin loses its protective function; with any scratch, infection can occur, turning into purulent inflammation.
- Diabetic foot syndrome . Purulent ulcers and necrotic lesions form on the legs. They do not heal, the process progresses and spreads to the bone tissue, which leads to amputation of the limb. This becomes the cause of gangrene; the patient’s life can only be saved by amputation of the limb.
Sensory disorders - the main group of symptoms
Manifestations of pathology in the leg area can be varied, often depending on the cause of neuropathy. If the disease is caused by injury, symptoms affect one limb. In diabetes mellitus and autoimmune diseases, symptoms spread to both legs.
Sensory disturbances occur in all cases of lower extremity neuropathy. Symptoms are usually observed constantly, do not depend on body position, daily routine, rest, and often cause insomnia.
- numbness of the legs;
- crawling sensation;
- sensation of the presence of foreign objects under the skin.
In addition to the described signs, there are often sensory disturbances - slow recognition of cold and hot, changes in the pain threshold, regular loss of balance due to decreased sensitivity of the feet. Pains also often appear - aching or cutting, weak or literally unbearable, they are localized in the area of the affected area of the nerve.
Stages of development
The development of neuropathy occurs in several stages, each of which produces its own symptoms. Stages of the disease:
- Stage 1, subclinical . There are no clinical signs, but examination reveals nerve damage.
- Stage 2, clinical . The first motor and sensory disturbances and muscle weakness appear.
- Stage 3 late complications . At this stage, the changes are irreversible, complications such as diabetic foot and limb deformity develop. The patient is assigned a disability group.
Reference . Almost 80% of patients consult a doctor at the last stage due to the fact that they do not associate the existing symptoms with the manifestation of diabetic complications.
Diagnostics
Making a diagnosis begins with taking an anamnesis. The doctor asks the patient in detail about all the symptoms present and the time when the first signs appeared. The doctor uses special scales to assess the patient’s condition:
- Michigan scale . Includes 15 questions about various symptoms of the disease (are there numbness, burning, cramps, pain, etc.).
- Neurological Symptom Scale . Evaluates the manifestation of the disease, localization of symptoms, time of onset, etc.
The neurologist then conducts a visual examination of the patient for toe deformities, diabetic foot, ulcers, and dry skin areas.
The next stage is sensitivity tests:
- Vibration sensitivity. The tuning fork is placed on the back of the thumb and the vibration sensitivity time is recorded.
- Measuring tendon and muscle reflexes using a hammer.
- Assessment of tactile sensitivity. The surface of the foot is easily touched by a sharp object.
- Temperature Sensitivity Study . Check the skin's reaction to heat and cold.
- The electrical potential of muscles is measured using electromyography. Needle electrodes are inserted into the muscle to measure the speed at which the impulse travels through the nerves.
To assess the activity of internal organs, it is necessary to conduct a number of laboratory tests:
- General and biochemical analysis of blood and urine.
- Measuring sugar levels.
- Blood test for glycosylated hemoglobin.
- Cholesterol test.
Next, instrumental studies are prescribed to identify malfunctions in the functioning of organs and systems:
- ECG . Detects pathology of the cardiovascular system, heart rhythm disturbances.
- 24-hour monitoring of heart rate and blood pressure.
- Ultrasound of the abdominal organs . Diagnoses cholelithiasis, urolithiasis, narrowing of ducts, increase in size, changes in the structure of organs
- Fibrogastroscopy. Prescribed to confirm gastritis, gastric and duodenal ulcers.
- X-ray with contrast . The functionality of the intestines, kidneys, and stomach is studied.
- Cystoscopy is required for recurrent cystitis.
- Electromyography of the bladder muscles is performed if the patient has problems with urination (urinary retention or incontinence).
To clarify the diagnosis, you will need to consult other specialists: cardiologist, urologist, gastroenterologist, orthopedist, ophthalmologist.
Symptoms of polyneuropathy in diabetes mellitus
Polyneuropathy can be a rather late symptom of type 1 diabetes mellitus, but in non-insulin-dependent diabetes its signs appear very early and sometimes before diabetes is diagnosed. This happens because diabetes has a latent phase, when there are practically no symptomatic manifestations.
Polyneuropathy first affects the distal (remote) parts of the extremities: feet, hands. This is explained by impaired blood supply in diabetes, which is more pronounced in the ends of the legs and arms.
Classification of symptoms of polyneuropathy
Polyneuropathy in diabetics has different symptoms, which can be divided into several groups:
- Sensory symptoms are associated with the peripheral nervous system: pain;
- phenomena of paresthesia;
- loss of certain types of sensitivity.
- the presence of movement disorders;
- change in skin condition (appearance, color, presence of ulcers or wounds);
- visual impairment;
Clinical symptoms of polyneuropathy
Attention! The first signs of diabetes may be: decreased vibration sensitivity and the Achilles tendon reflex; increased thirst and appetite; polyuria (frequent urination); dry mouth and smell of acetone; skin itching; slow healing of wounds.
Diuresis in diabetes (loss of salts needed for the body along with water) leads to dehydration, cardiac arrhythmia, twitching and muscle cramps.
Which nerves are most often affected by diabetes?
- The femoral, tibial, sciatic, median and ulnar nerves are most often affected.
- There may also be lesions in other nerves of the extremities, as well as in the trigeminal, abducens, ophthalmic and nerves innervating the muscles of the genitourinary system. In this case, the innervation of those zones with which the damaged nerves are connected is disrupted.
How does diabetic neuropathy of the lower extremities manifest?
- Pain and burning begin, first in the area of the big toe, and then rising up the shin; paresthesia in the extremities (burning, tingling, goosebumps, numbness). Symptoms worsen at night and with exercise on the legs.
- Sensitivity disturbances occur (vibration, tactile, temperature, pain) - the so-called diabetic foot syndrome. In this case, the patient does not feel pain, touch, temperature changes, or vibration.
- Muscle weakness appears, the gait changes (the patient seems to lose the spatial sensation of the limbs and walks unnaturally, raising his legs high when walking).
- The heels of diabetics often become deformed as a result of arthropathy (Charcot foot).
- The skin of the extremities becomes dry and changes color, initially becoming pink, and at a later stage acquiring a blue-violet and purplish-bluish with black tint.
- The structure of the nails on the feet changes, they thicken, become rough, flake and crumble.
- Wounds often become infected, do not heal for a long time, and in the late stage turn into ulcers.
Early symptoms include the patient's ability to feel vibrations, as well as weakness and sagging of the feet (a consequence of loss of the Achilles reflex).
In severe diabetic neuropathy:
- increasing pain until it feels unbearable;
- expansion of zones of loss of sensitivity;
- extinction of limb tendon reflexes;
- development of muscle atrophy;
- deep trophic ulcers, gangrenous blackening of the skin;
- diseases of organs (vision, heart, blood vessels, central nervous system, genitourinary system).
Complications of polyneuropathy
Diabetic coma (a condition associated with critical blood sugar levels), gangrene and sepsis, and cardiovascular diseases pose a threat to the life of a diabetic patient.
The disease is often complicated by:
- ankle arthrosis;
- ketoacidosis (impaired carbohydrate metabolism);
- atherosclerosis;
- hypertension;
- cardiosclerosis (mainly in juvenile diabetes);
- glomerulosclerosis (more common in older patients);
- diseases of the central nervous system;
- visual pathologies.
Visual disturbances in polyneuropathy
One of the most serious complications of diabetic polyneuropathy is damage to the oculomotor nerves, which leads to strabismus, decreased eye reflexes (they stop responding to light, movement of objects), anisocoria (different pupil sizes and pathological reflexes in one of the pupils), and other visual disorders.
These symptoms may be supplemented by standard diabetic visual pathologies: retinopathy (damage to the retina) and cataracts.
CNS lesions in polyneuropathy
Diabetes is a systemic disease, so polyneuropathy can be combined with:
- with neurasthenic syndrome;
- encephalopathic syndrome;
- myelopathy;
- mental disorders.
These are all signs of severe late diabetes.
Diabetic neurasthenia
Diabetic neurasthenia usually manifests itself as apathy, loss of strength, depression, and indifference to the environment - this is the so-called asthenic syndrome. However, some patients, due to their mental type, may have diametrically opposite symptoms: aggression, anger, irritability.
Diabetic encephalopathy
Encephalopathy in diabetes is observed mainly in cases of violation of insulin treatment in patients who have experienced hyperglycemic or hypoglycemic comas. Symptomatic signs:
- severe headache, nausea;
- unexplained restlessness;
- precomatose or comatose state;
- foci of paresis and aphasia;
- decreased muscle tone;
- constriction of the pupils;
- pseudobulbar disorders (lacrimation, dysphagia, cough while eating, nasal voice, etc.);
- nonhemorrhagic strokes;
- memory loss;
- cognitive personality disorders.
Examination of cerebral fluid punctate may show elevated sugar levels, while in the blood it remains normal.
Myelopathy in diabetes
Diabetic myelopathy is manifested by aching pain, paresis, and muscle atrophy. Sometimes the symptoms correspond to damage to the posterior column of the spinal cord.
Mental symptoms
Mental disorders have a very diverse and contradictory picture: from irritability, insomnia, tearfulness, suspicion, to complete apathy, deep depression, loss of strength. But in any case, the patient experiences a pronounced decrease in performance.
Treatment
The main task of diabetic neuropathy is to reduce sugar levels and maintain them in a stable state. This eliminates the main cause of diabetes complications, which allows the patient’s condition to normalize. It is possible to reduce glucose levels with insulin and antidiabetic drugs .
Important ! Some patients note an increase in symptoms of the disease during treatment. This is a positive result - the nerves are gradually regenerating.
The rest of the treatment measures are symptomatic in nature and are aimed at alleviating the patient’s condition. To relieve unpleasant symptoms and restore damaged nerve fibers, the following groups of drugs are prescribed:
- Non-steroidal anti-inflammatory drugs (Nise, Ibuprofen, Diclofenac). They reduce pain, relieve swelling and inflammation. However, drugs in this group have a negative effect on the stomach, kidneys, and heart. Therefore, they cannot be used for ulcers, heart, liver, or kidney failure.
- Neurotropics (Milgamma, B vitamins). Improve nerve conduction, restore the integrity of nerve fibers.
- Antidepressants of the tricyclic group (Amitriptyline). They inhibit the transmission of pain impulses. This achieves pain relief.
- Anticonvulsants (Neurontin, Pregabalin). Reduces excessive muscle contraction due to its effect on the excitation center in the brain.
- Synthetic opioids (Tramadol, Zaldiar). Reduces the sensitivity of pain and temperature receptors.
- Antiarrhythmic drugs (Mexiletine). Normalizes heart rate by blocking sodium channels.
- Local painkillers (ointments, patches). Reduce receptor sensitivity.
If the patient has formed purulent ulcers, then it is necessary to take broad-spectrum antibiotics and antifungal agents.
Alpha-lipolyic acid (Thioctacid, Thiogamma) has been successfully used to reduce glucose.
The medicines contain a synthetic pancreatic hormone that restores metabolism and prevents the negative effects of free radicals.
The doctor also prescribes antidiabetic drugs (Metformin, Nateglinide and others), depending on the type of diabetes and the stage of the disease.
The average duration of therapy is 2-4 weeks. Antidiabetic medications are taken for a longer period of time, sometimes for life.
Physiotherapy
Physiotherapy in combination with drug treatment accelerates the process of nerve regeneration, helps relieve pain, and restores sensitivity. The most effective methods:
- Magnetotherapy . The affected areas are exposed to an alternating magnetic field. The nutrition of nerve fibers is enhanced and blood supply is improved.
- Electrical stimulation . Functional, motor muscle activity is stimulated by high-frequency currents, thereby restoring muscle tone.
- Electrophoresis . Medicines are administered through the skin using a direct electrical current. In this way, an anti-inflammatory and analgesic effect is achieved.
- Balneotherapy . Radon and turpentine baths are widely used to treat neuropathy. Paraffin applications, mud wraps, and Charcot's shower also give a good effect.
Physiotherapy
Exercise therapy is necessary to maintain joint mobility, restore muscle tone, and improve blood circulation. Due to this, indirect restoration of nerve fibers is achieved. A set of exercises is developed by a specialist. It is best to perform gymnastics under the supervision of an instructor . It is important that the classes are regular and appropriate to the patient’s condition.
Classes begin after the acute period has passed. When performing exercises, the patient should feel comfortable, and movements that worsen the condition should be avoided.
Diet
Nutrition for diabetic polyneuropathy should correspond to the type of diabetes. Basic rules for catering:
- Strict adherence to daily calorie intake and nutrient balance (proteins, fats, carbohydrates).
- Eating at strictly defined hours 5-6 times a day in small portions.
- Accounting for the glycemic and insulin index of foods.
- Cooking dishes by stewing and baking.
This way you can avoid sudden spikes in sugar and improve fat metabolism.
List of prohibited products:
- Simple carbohydrates: sugar, confectionery, white bread, rice, fruit juice.
- Fast food.
- Sausages.
- Pre-finished products.
- Semolina.
- Canned food.
- Sweet dairy products.
- Fatty fish and meat.
- Spicy, salty, smoked products.
The patient's diet consists of the following products:
- Vegetables are raw, stewed.
- Eggs, omelettes.
- Buckwheat, pearl barley, millet porridge.
- Soups with vegetable broth.
- Lean varieties of meat and fish.
- Sour berries, fruits.
- Dairy products without sugar.
- Vegetable oil.
- Sweet fruits, butter, and honey are consumed in limited quantities.
Note !
With mild to moderate severity of the disease, diet plays the main therapeutic role. In severe cases, it serves as a serious addition to drug treatment.
Treatment of diabetic polyneuropathy of the lower extremities
Such complications cannot be completely cured, but their development can be slowed down. How to treat neuropathy of the lower extremities? The main condition is the normalization of blood glucose. Analgesics, loose shoes, minimal walking, and cool baths help reduce pain. A contrast shower relieves burning feet. It is necessary to use drugs that dilate peripheral vessels and affect the transmission of nerve impulses. Treatment of polyneuropathy of the lower extremities becomes more effective when taking B vitamins. It is also important to correct carbohydrate metabolism with diet.
Drug therapy
The main means for the complex treatment of patients diagnosed with polyneuropathy of the lower extremities:
- antidepressants Amitriptyline, Imipramine, Duloxetine, blocking the reuptake of the hormones norepinephrine and serotonin;
- anticonvulsants Pregabalin, Carbamazepine, Lamotrigine;
- analgesics Targin, Tramadol (doses are strictly limited - drugs!);
- vitamin complex Milgamma;
- Berlition (thioctic or alpha lipoic acid), which has the ability to restore damaged nerves;
- Actovegin, which improves blood supply to nerve endings;
- Isodibut, Olrestatin, Sorbinil, protecting nerves from glucose;
- antibiotics - if there is a threat of gangrene development.
Treatment without drugs
The hope of being cured with the help of homemade or folk remedies alone is a utopia. It is necessary to take medications and actively use:
- magnetic therapy;
- electrical stimulation;
- hyperbaric oxygen therapy;
- acupuncture;
- massage;
- Exercise therapy (physical therapy).
Prevention and complications
If the patient ignores the symptoms of the disease for a long time, this will lead to the development of serious complications, most of which are fatal. The most common complications of diabetic neuropathy are:
- Silent myocardial infarction . It is a consequence of a violation of the innervation of the heart muscle.
- Mental illnesses developing against the background of damage to the central nervous system.
- Diabetic foot , ulcerative skin lesions that end in amputation of the limbs.
People with diabetes can prevent neuropathy by following these guidelines:
- Quitting smoking and alcohol.
- Following a special diet according to the type of diabetes.
- Weight control.
- Taking antidiabetic medications prescribed by your doctor.
- Constant monitoring of sugar levels.
Diabetic neuropathy can be completely cured. At the first stage, nerve damage is reversible; with timely treatment, the chances of full recovery are high.