Why are droppers prescribed to pregnant women?
A drip is not a treatment, but only a method of administering medicine. During pregnancy and childbirth, there is a risk of symptoms that require medical attention, including:
- severe swelling;
- high blood pressure;
- vomit;
- dehydration;
- infectious diseases;
- placental insufficiency;
- threat of spontaneous abortion;
- uterine bleeding;
- post-term pregnancy;
- weak labor activity.
information Thus, a drip is prescribed if there are deviations in the health of the mother or unborn baby.
Drugs delivered by drip help restore good health. In this case, only medications are used that are approved for pregnant women and do not harm the development of the fetus.
Treatment of feto-placental insufficiency
It should be noted that treatment of placental insufficiency should be carried out exclusively in a hospital setting. The exception is the compensated form of FPN, which requires dynamic outpatient monitoring and treatment.
Unfortunately, there are no effective treatment methods that can immediately cure FPN. The main goal of treatment is primarily to prevent complications of this disease.
For this purpose, the following groups of drugs are prescribed:
- vasodilating agents, such as Curantil, to improve microcirculation, eliminate hypoxia in fetal tissues and to prevent further negative changes in the placenta;
- drugs that activate metabolism in tissues, such as Actovegin, ascorbic acid, vitamin E, Troxevasin;
- drugs that reduce uterine tone, such as Ginipral, Magnesium Sulfate, No-shpa.
To improve uteroplacental blood flow, Eufillin, Trental, and a glucose-novocaine mixture are additionally used.
In case of increased blood clotting, antiplatelet agents (Heparin, Clexane) are used.
To normalize the processes of excitation of the nervous system, drugs that improve sleep are prescribed (tinctures of motherwort or valerian, Glycine).
These are the main drugs used in obstetrics to treat placental insufficiency. On average, FPN treatment is carried out for about 2 weeks under the control of CTG, ultrasound and Doppler. The effect of the treatment directly depends on the duration of pregnancy (if FPN occurs in the later stages, the prognosis is more favorable than in the early stages) and on the lifestyle of the pregnant woman.
If you have been diagnosed with placental insufficiency, pay attention to your lifestyle. Don't deny yourself long sleep. A pregnant woman should sleep at least 8 hours a day, ideally up to 10 hours a day. Protect yourself from stress! Spend more time outdoors.
Additionally, take vitamins and microelements as prescribed by your doctor. This is especially true in the cold season.
Get rid of bad habits (if you have them). During pregnancy, bad habits are contraindicated, and if diagnosed with FPN, this can lead to irreversible consequences for the child.
Droppers for toxicosis
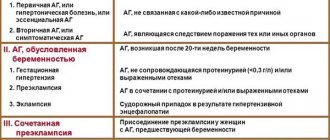
Every fifth pregnant woman experiences toxicosis (preeclampsia). This unpleasant condition is accompanied by constant nausea, frequent vomiting, swelling, headache, and increased blood pressure. If gestosis is too severe, the woman requires hospital treatment. In this case, drip administration of the following drugs is possible:
- Magnesium sulfate (magnesium) for toxicosis helps reduce swelling and lowers blood pressure;
- sodium chloride, Reopoliglucin, Infucol act against dehydration, saturating the blood with liquid and beneficial salts;
- Aminazine is a sedative that helps with persistent vomiting;
- Cerucal is another drug that relieves indomitable vomiting;
- Intercordin and Pentoxifylline improve blood supply to the uterus and placenta;
- Arfonad, Pentamin and Apressin normalize high blood pressure;
- Essentiale supports liver health and improves metabolic processes.
In what cases is Magnesia prescribed during pregnancy?
Why is Magnesia used during pregnancy? Magnesium therapy is effective for late gestosis. The method of introducing the drug into the body depends on the problem that worries the woman. Magnesia is prescribed when the following pathologies are detected:
- threat of premature birth of a baby;
- tension of the uterine muscles;
- oxygen starvation of the fetus due to oligohydramnios;
- swelling and urinary retention;
- the appearance of seizures;
- placental abruption;
- high blood pressure;
- cardiovascular diseases;
- poisoning with toxic substances and heavy metals;
- impaired renal function, manifested in the detection of protein in the urine;
- increased nervous excitability;
- epilepsy;
- insufficient concentration of magnesium in the body;
- predisposition to blockage of veins, blood clots;
- constipation;
- stagnation of bile in the body;
- infections of the bile ducts;
- suspicion of impaired brain development in the fetus.
Magnesia can be used if it is necessary to prepare a woman for an unplanned birth or caesarean section. The use of the drug helps to quickly cleanse the stomach and intestines.
IVs for threatened miscarriage
If dangerous symptoms of a threatened miscarriage occur, the doctor always hospitalizes the woman in the hospital. It is necessary to do everything possible to maintain the pregnancy and bear a healthy child. The following medications are used against threatened miscarriage:
- When there is a threat of spontaneous abortion, magnesium sulfate relaxes the muscles and reduces the tone of the uterus so that premature labor does not begin;
- Ginipral, Alupent and Partusisten also relax the uterus and prevent contractions;
- Dicynon and Tranexam strengthen the walls of blood vessels and are used in the presence of bleeding to stop it;
- intravenous immunoglobulins reduce the number of dangerous cytotoxic cells that threaten pregnancy and restore the balance of the immune system.
Course duration
The drug solution is administered intravenously
within a few days. A certain amount of powder is diluted in sodium chloride solution for infusion and injected with a needle.
The time during which the solution must be completely administered varies from 15 to 20 minutes
. Sometimes injections are prescribed, and the method of administration is chosen depending on the conditions.
The injection can be given almost anywhere: in a gynecologist’s office, in an ambulance, at the patient’s home, or in any room of a medical facility. With drip administration it is more difficult, since it cannot be organized on the road or in other inappropriate conditions.
After the first dose, the patient is taken to the hospital, where she continues to receive IVs according to a certain scheme. Nowadays, most institutions use infusion pumps. This is special equipment that allows you to administer a given amount of the drug and not worry about overdose. How many days to drip depends on the condition of the patient. For example, in a situation of premature birth, the drug is instilled throughout the day.
A similar period of use of magnesium sulfate is recommended in case of gestosis (severe and moderate).
Interesting! Causes and signs of gestosis during late pregnancy
IVs during childbirth
In maternity hospitals, almost all women are given IVs during childbirth. Sometimes it is necessary to slow down or, conversely, speed up the labor process, sometimes medicine is needed to improve the well-being of the mother in labor or the condition of the newborn baby. During childbirth you may encounter the following drugs:
- oxytocin solution and Dinoprost are necessary for weak labor in order to improve the tone of the uterus and induce full contractions;
- Obzidan reduces blood loss during childbirth and the postpartum period;
- prostaglandins help the cervix to ripen and open;
- Sigetin also promotes dilatation of the cervix, and also improves blood supply to the uterus and placenta;
- Hexoprenaline and Terbutaline are used when labor is too strong to slightly relax the uterus and prevent traumatic rapid labor;
- a glucose solution is needed to support a woman in labor who is tired after long hours of labor and helps restore good health;
- Reopoliglyukin and Hemodez are used for large blood loss and restore the amount of fluid in the body.
important The doctor will never prescribe an IV unless there are serious indications for it. Every woman has the right to refuse this procedure, but it is better to wait with such a decision. It is better to ask the doctor what medicine will be in the infusion system, how it will help, and whether it is dangerous for the baby. After a detailed explanation, there should be no doubt.
Treatment of placental insufficiency
At present, unfortunately, it is not possible to completely relieve a pregnant woman from placental insufficiency using any therapeutic interventions. The means of therapy used can only help to stabilize the existing pathological process and maintain compensatory and adaptive mechanisms at a level that allows for the continuation of pregnancy until the optimal date of delivery. Therefore, it is very important to carry out prevention in women who have risk factors for the development of placental insufficiency. The leading place in prevention is the treatment of the underlying disease or complication, which may lead to placental insufficiency. An important condition is for the pregnant woman to follow an appropriate regimen: adequate rest (sleeping on the left side is preferable), elimination of physical and emotional stress, staying in the fresh air for 3-4 hours a day, and a rational, balanced diet. The course of prevention includes multivitamins, iron supplements, oxygen therapy (treatment of diseases by increasing the concentration of oxygen in the tissues of the body, including breathing exercises and increasing the delivery of oxygen through the lungs), the use of amino acids, glucose, galascorbine, potassium orotate, ATP, which serve as a direct source energy for many biochemical and physiological processes.
If indicators deteriorate during treatment, signs of decompensation of placental insufficiency appear, determined by a sharp deterioration in the condition of the fetus and the possibility of its death, explain that emergency delivery by cesarean section is indicated, regardless of the gestational age.
How can you detect uterine tone?
Many women are interested in the question of determining whether the uterus is in good shape.
In most cases, this is not difficult to do. During the period of bearing a baby, the symptoms of this condition are quite simple, although they differ at certain times. In the first period of pregnancy, the main symptoms of the uterus being in good shape are nagging pain that occurs in the lower abdomen. Heaviness appearing in this place. In the second and third trimester, signs of uterine tone can be observed: the abdomen becomes hard and shrinks, while the uterus simply “turns to stone.” That is, when such a condition occurs, the woman understands that the uterus is in good shape.
It is also worth saying that in certain cases, the manifestation of this condition consists of spotting bloody discharge. Such signs are alarming, so you should immediately seek medical help.
Because today, if treated in a timely manner, pregnancy can still be saved. It should be added that the tone of the uterus in some cases passes without the presence of any symptoms, or rather, a pregnant woman may simply not feel them.
Infusion therapy
During infusion therapy, vitamins enter directly into the bloodstream. When using this method, all organs and systems begin to recover as soon as possible. Infusion therapy is used to treat diseases, strengthen the immune system and improve general condition.
To carry out infusion therapy, a needle or catheter is installed in the patient’s vein, through which the necessary substances enter the blood from the reservoir with the infusion solution. Through the device, vitamins can be introduced into the patient’s body in large volumes over a long period of time. The results of therapy are monitored by conducting instrumental and laboratory examinations.
When is it held?
Prescribe intravenous infusion of nutrient solutions to patients who:
- dehydration;
- water-electrolyte balance is disturbed;
- intoxication;
- kidney pathologies;
- problems with the gastrointestinal tract, in which oral intake of vitamins is contraindicated or they are not absorbed.
Doctors recommend administering vitamins intravenously to people who need:
- reduce intoxication;
- saturate tissues with oxygen;
- activate brain function;
- increase resistance to stress factors;
- normalize metabolic processes;
- restore liver function;
- improve tissue nutrition.
Droppers are prescribed for exacerbation of diseases, for low-grade inflammatory processes and seasonal ailments.
Pros of the procedure
The advantage of intravenous drip administration of vitamins is the fact that they enter the body bypassing the digestive organs. When vitamin supplements enter the bloodstream, they are completely absorbed, and the effect of their administration occurs earlier than with oral administration.
With the help of a dropper you can quickly replenish the lack of substances necessary for the body.
How to place an IV
For pregnant women, a solution of magnesium sulfate with a concentration of 25% is used for intravenous drips.
Note!
The dosage is calculated individually, taking into account the symptoms, gestational age and condition of the patient.
The solution can only be administered drop by drop.
, under no circumstances should it be a stream, otherwise the pressure may drop sharply and greatly, which will pose a threat to the condition of the fetus.
Before using magnesia, it is heated to body temperature. Then they put in an IV and monitor the patient’s condition. Depending on whether it improves or not, the dosage is adjusted and the intensity of the medication is adjusted. When simultaneous administration of magnesia and calcium drugs is prescribed, they are injected into the veins of both arms
.
Treating hypertension at home
Sometimes you can really relieve tone and you don’t need to leave the house to do it. In addition, there is no need to resort to drug treatment. The simplest and most effective way to relieve uterine tone is considered to be the “Cat” exercise.
To do this, a woman should get on all fours, her head should be raised up, her back should be arched at this time, she should stay in this position for a few seconds, and then slowly move back to her original position.
You need to repeat this exercise a couple of times; after doing it, it is advisable to lie down for a while.
We invite you to read: Gestational age by ultrasound: how to find out and how to calculate the due date (DA)?
Many people have long known that the relaxation of the uterine muscles is facilitated by the relaxation of the muscles located on the face. If you have hypertonicity, it is advisable to perform the following exercise - lower your head, while you should relax the muscles of your neck and face as much as possible. When performing the exercise, you should breathe through your mouth.
If, with the tone of the uterus, unpleasant sensations appear from getting rid of them, stand on all fours, focusing on your elbows, that is, then the uterus will be in a suspended position.
These simple exercises in combination with sedatives and antispasmodics will help eliminate discomfort. But do not forget that it is important to eliminate the cause of this condition; for this it is necessary to strictly follow the recommendations given by the treating doctor.