Utrozhestan: mechanism of action, indications for use
Utrogestan is a semi-synthetic progesterone, which is obtained chemically from the roots and tubers of a plant such as wild yam or dioscorea. The molecular structure of artificial progesterone is almost identical to the hormone produced by the ovaries. In the production of Utrozhestan, a special technology is used - micronization. Micronization is the reduction of the particle size of a substance to microns by grinding. Therefore, the drug is better absorbed and acts more effectively.
Composition of the drug
Utrozhestan was developed in France. Today, the medicine is used in the systemic treatment of infertility and in cases of risk of miscarriage in more than seventy countries.
As noted above, the active substance of the drug is progesterone. Other components are:
- sunflower oil;
- lecithin, derived from soy;
- gelatin;
- glycerol;
- titanium dioxide.
Release forms
Utrozhestan round capsule contains 100 mg of progesterone
Utrozhestan is offered for use in the form of round or oval capsules. Moreover, they can be taken both orally (ingestion) and vaginally. In terms of effect and purpose, both forms (Utrozhestan 100 and Utrozhestan 200) differ only in appearance and dose (100 and 200 mg). Initially, the drug was intended for oral use. It was only registered for vaginal use in 1993. In recent years, the hormone is more often prescribed vaginally. The first method is more convenient, but causes systemic negative effects, while with the second, only a local reaction in the form of mild irritation may appear. In practice, doctors often select treatment regimens that combine both methods of application.
Principle of action, indications for use
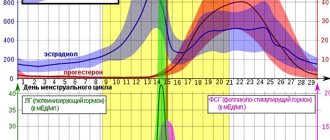
Natural progesterone begins to be produced by a special gland - the corpus luteum, which is temporarily formed in each menstrual cycle in the so-called luteal phase (after ovulation before bleeding begins). During this period, the hormone prepares the lining of the uterus (endometrium) for the implantation of a fertilized egg. A lack of progesterone does not allow this process to complete and pregnancy does not occur.
Progesterone levels begin to rise in the luteal phase, which helps the fertilized egg implant in the inner layer of the uterus.
If the egg manages to gain a foothold in the uterus, the corpus luteum continues to secrete the hormone for another 10–12 weeks. Progesterone helps indirectly support the development of the embryo by stimulating the growth of the endometrium and prevents the release of new eggs. As the placenta grows, the function of producing pregnancy hormones passes to it.
Utrozhestan compensates for the lack of progesterone, and is therefore prescribed by doctors in the following hormone deficiency conditions:
- inability to conceive;
- the appearance of signs of spontaneous abortion;
- repeated miscarriage (two or more spontaneous miscarriages);
- increased risk of premature birth.
Utrozhestan is often used in preparation for in vitro fertilization (IVF).
Obviously, when choosing therapy to maintain pregnancy, it is desirable to use drugs that are as close as possible to the molecules synthesized in the pregnant woman’s body, such as Utrozhestan (Besins Healthcare) - natural micronized progesterone.
E.I. Vovk
"Utrozhestan in maintaining pregnancy"
Spontaneous abortion occurs in 15–25% of all registered pregnancies. Utrozhestan is prescribed when the following painful signs appear:
- uterine bleeding, which can be either regular or irregular, accompanied by pain or painless;
- pain in the lower abdomen or lower back.
The most reliable symptom of spontaneous abortion is bleeding accompanied by pain. The risk of miscarriage increases with each subsequent miscarriage. So, after the second spontaneous abortion, the probability of termination of pregnancy is 25–30%. Despite the advances of modern medicine, the causes of half of cases of recurrent miscarriage remain unknown.
Therapeutic effect and safety of Utrozhestan
In recent years, large-scale studies have been conducted in different countries in which the effect of synthetic progesterone is compared with the effect of placebo or no therapy. A prerequisite for all studies is to study the safety of the drugs used. The greatest relevance for the practicing physician are medications that do not cause fetal malformations when used in the first trimester.
Utrozhestan is one of the most studied and frequently used gestagens. Research on this drug continues today. One of the latest studies was conducted in 2020 in the USA, its results were published in the New England Medical Journal. The use of Utrozhestan in the treatment of pregnant women in the early stages has shown that the drug does not increase the risk of congenital malformations.
The rate of abortion in the first trimester is reduced by half after Utrozhestan therapy
Based on the results of four studies, it was found that the use of progesterone during threatened abortions reduces the frequency of spontaneous miscarriages and does not increase the likelihood of developing fetal abnormalities (more details: Reproductive Endocrinology, Scientific and Practical Medical Journal, No. 4(30)/2016).
It must be admitted that some doctors question the effectiveness and safety of progesterone therapy. Thus, a large-scale study that was conducted in the UK and the Netherlands from 2010 to 2013 did not reveal significant differences between the groups of pregnant women taking Utrozhestan and placebo. Additional research is currently being conducted into the effectiveness of progesterone in reducing the incidence of miscarriage in pregnant women with threatened abortion. The study is being carried out across 47 UK hospitals and results are expected soon.
According to the instructions, Utrozhestan can be taken without fear in the first trimester. In the second and third trimesters, it should be used with caution, since there is evidence that this gestagen increases the risk of developing cholestasis (a pathological disorder in the flow of bile into the duodenum). A study of the safety of Utrozhestan showed that it does not disrupt metabolism, blood clotting, does not change blood pressure, and does not contribute to weight gain.
Indications, contraindications, side effects
Pregnant women are prescribed Utrozhestan for:
- threat of abortion or if the woman has had abortions before;
- the existing threat of premature birth (when the due date has not yet approached, and the cervix has begun to shorten);
- increased uterine tone.
My doctor prescribed this drug to me after an ultrasound at 7–8 weeks of pregnancy. The reason was the discovery of a corpus luteum cyst (as a result, a possible disruption in the production of progesterone). In addition, the gynecologist drew attention to the insufficient attachment of the fertilized egg to the walls of the uterus. The doctor immediately predicted that I would have to drink Utrozhestan until the middle of the second trimester. In addition to taking hormones, motor rest was prescribed at least until the first screening.
To survive, the embryo must literally “grow” into the endometrium, and this requires progesterone
Women planning pregnancy and those diagnosed with infertility are prescribed Utrozhestan in preparation for the IVF procedure:
- to support the luteal phase (this helps the egg, if fertilized, to gain a foothold in the uterus);
- as hormone replacement therapy if the body does not produce enough progesterone.
Instructions for use of Utrozhestan
As noted above, the peculiarity of Utrozhestan capsules is that they can be used both orally and vaginally. The treatment regimen is determined only by the attending doctor, based on the individual characteristics of the woman’s body and the severity of the disease.
The oval capsule of Utrozhestan contains 200 mg of progesterone
How to administer capsules intravaginally
Medical specialists prefer the intravaginal method of using Utrozhestan. This is explained by the fact that the absorption of the drug occurs much faster. The medicine acts directly on the inner layer of the uterus. The concentration of the hormone in plasma reaches a maximum after 2–3 hours. Using more than 200 mg daily dose is likely to increase progesterone levels to the required level.
As previously conducted randomized studies have shown, in the case of intravaginal use of Utrozhestan, the bioavailability of progesterone is high, individual fluctuations in the level of the hormone in the blood are smaller, and the effective concentration is maintained more stably and for a long time.
L.E. Murashko, N.I. Klimenchenko
“Experience of using micronized progesterone in the first half of pregnancy”
Before carrying out the intravaginal procedure, you must wash your hands thoroughly to avoid infection. Next, you need to complete the following steps:
- lie on your back;
- bend your knees and bring them closer to your chest;
- insert the capsule deeply with your finger or applicator.
With certain skill and necessity, this procedure is carried out while sitting or standing.
The dose of Utrozhestan for vaginal administration is selected based on the following therapeutic goals:
- threatened abortion or recurrent miscarriage - from 200 to 400 mg per day, divided into two doses;
- risk of premature birth - 200 mg at night;
- conducting an IVF cycle - from 200 to 600 mg per day;
- infertility due to impaired function of the corpus luteum - from 200 to 300 mg per day from the 17th day of the menstrual cycle for ten days.
How to take Utrozhestan orally
Capsules are advised to be taken orally if irritation of the mucous membrane is observed when they are inserted into the vagina. For most diagnoses, the medicine must be taken at night and after waking up with water. To achieve the required level of progesterone, it is usually enough to take 200–300 mg of medication per day. If there is a risk of miscarriage or the woman is diagnosed with recurrent miscarriage, the dose may be increased by 100–300 mg.
How to properly stop the drug
The duration of the treatment course is determined by the doctor based on the individual characteristics of the woman’s body and the nature of the disease. Only a doctor can stop taking the drug when stable hormonal levels are achieved. Moreover, most experts recommend doing this by reducing the daily dose by 100 mg every seven days. This helps avoid the development of hormone therapy withdrawal syndrome.
Ingestion
Drinking capsules is much easier and more convenient. This can be done in any conditions - at home, at work, on the road and in nature. It is this factor that forces some pregnant women to take the medicine orally, avoiding inserting the capsule into the vagina.
The treatment method is simple: depending on the doctor’s prescription, you need to take Utrozhestan 200 mg several times a day. It is advisable to take each dose with water. The maintenance regimen of therapy implies that you will need to drink at least 2 capsules - 1 in the morning and in the evening. If necessary, the dosage can be increased - one capsule in the morning, afternoon and evening. It is necessary to strictly observe equal intervals of time between taking the drug. With a 3-dose regimen, Utrozhestan must be taken every 8 hours.
Vaginal insertion
Using the method of insertion into the vagina is somewhat more difficult: there are not always suitable conditions for timely and convenient use of the medicine. Especially if the woman is not at home or there is no restroom nearby. However, in most cases, during pregnancy, the doctor will prescribe 1 capsule at night when the pregnant woman is at home.
A preventive regimen is the administration of Utrozhestan 200 mg before bedtime. If there are complications, then the typical treatment regimen for ICI or threatened miscarriage is 200 mg twice a day (morning and evening). The most difficult option is to inject the drug into the vagina three times a day. Typically, this treatment method is required for rapid and pronounced shortening of the cervix, when a pregnant woman must be on sick leave or in hospital for conservation.
For each woman while carrying a child, it is necessary to individually select the dose, administration method and treatment regimen. In addition, it is necessary to reduce or increase the dosage in time if there are reasons for this.
Restrictions on use
Utrozhestan should not be prescribed for the following pathologies:
- hypersensitivity to progesterone or any excipient of the drug;
- deep vein thrombosis, thrombophlebitis;
- vaginal bleeding for an unknown reason;
- when taken orally - in case of severe liver pathologies.
The drug should be used with caution in a number of chronic diseases:
- high blood pressure;
- disorders of the cardiovascular system;
- renal failure;
- diabetes;
- bronchial asthma;
- migraine;
- depressive state.
Contraindications for oral administration
It is possible that during pregnancy it is undesirable to take Utrozhestan orally, but only vaginal administration can be used. You should not take the drug in the following cases:
- against the background of diseases of the digestive system, when there is a risk of worsening a chronic disease or lack of effect from treatment if Utrozhestan does not enter the woman’s blood;
- in case of liver pathology, when the medicine harms liver cells or aggravates hormonal deficiency;
- in case of cardiovascular pathology, when the drug in a certain dose can affect vascular tone or the tendency to edema;
- for endocrine disorders, when the drug provokes hormonal imbalance.
At the stage of preparation for pregnancy, the doctor will identify risk factors, and if they are present, will prescribe Utrozhestan locally in the vagina. It is necessary to listen to the recommendations of a specialist so as not to harm your own body.
It is better to take Utrozhestan correctly from the very beginning. There is no need to experiment or follow the advice of friends: if vaginal administration of the drug is prescribed, then you must follow the recommendations.
Sometimes the smooth gestation of the fetus and the delivery of a healthy baby at term depend on this. It's all worth sticking with a not-so-convenient treatment method for a while, isn't it?
Adverse reactions
When choosing a method of using Utrozhestan, the occurrence of systemic and local adverse reactions should be taken into account. The former are most often observed when capsules are taken orally, and the latter - when used intravaginally. Systemic side effects include the following reactions from the nervous and immune systems, stomach and intestines, liver and gall bladder:
- headache, drowsiness, dizziness;
- increased blood pressure;
- jaundice;
- flatulence, stool disorders, nausea, vomiting;
- menstrual irregularities, increased vaginal discharge;
- depression, insomnia;
- skin rash, itching.
These reactions may occur several hours after using the medicine.
Changes in hormonal levels due to taking Utrozhestan provoke increased vaginal secretion. If the color of the leucorrhoea is slightly pink, white, yellowish, beige, and the consistency is liquid, thick, mucous, and its quantity has increased slightly, then there is no need to worry during pregnancy. If the discharge is curdled, brown or red, containing blood clots and pus, then this most likely indicates some kind of pathological process.
Headache and dizziness are the main side effects of oral Utrozhestan.
If any pronounced negative reactions occur, the pregnant woman should consult a doctor who will select another drug or change the treatment regimen. Most often, the above undesirable reactions occur in case of overdose. Basically, side effects are eliminated by reducing the dose. To relieve the consequences of an overdose, symptomatic therapy is recommended.
special instructions
According to the instructions, Utrozhestan is not recommended to be taken with food because this increases the bioavailability of progesterone. Caution should be exercised when engaging in activities that involve increased concentration, including driving.
It is also noted that in most cases, spontaneous abortion in early pregnancy occurs due to genetic disorders, infections, and mechanical damage. The use of Utrozhestan in such situations will only delay the natural process of rejection and removal of a non-viable egg from the body.
If long-term treatment with the drug is necessary, liver function assessment should be performed regularly.
Woman's feelings from therapy
The effect of administered progesterone on the body of a pregnant woman is usually little noticeable physically. The result of taking the hormone may be some drowsiness, dizziness and mild malaise - these are side effects. Many women are interested in whether Utrozhestan raises basal temperature. There is no official data on this effect from the manufacturer. But there is still a certain hyperthermic effect on the body.
Like progesterone produced by organisms, utrogestan affects a woman’s basal temperature. Those women who regularly keep a schedule of their BBT note that the basal temperature when taking Utrozhestan increases by 0.1-0.5 degrees.
This is a normal reaction of the body, both in the luteal phase of the cycle and during early pregnancy. In rare cases, Utrozhestan also increases body temperature and causes malaise. But usually this phenomenon goes away on its own, a few hours after administration.
What is better: progesterone injections or Utrozhestan?
The product is available in capsules of 100 and 200 mg. It is more rational to use vaginal administration of the drug during pregnancy. There is no load on the liver, the hormone is delivered directly to the target. An analogue is progesterone injections. But not all women are ready to endure injections. In any case, the choice of preparative form and dosage of the hormone is selected by the doctor.
How can I replace Utrozhestan?
If for some reason Utrozhestan is not suitable for use when planning or during pregnancy, then it can be replaced with other medications with a similar therapeutic effect. The following drugs are complete analogues of the drug in question for the active substance (progesterone):
- Progestogel;
- Crinon;
- Prajeesan;
- Progesterone;
- Iprozhin.
But according to indications, only Prajisan, Iprozhin and Progesterone can be considered analogues of Utrozhestan. Only these three drugs are used in planning pregnancy, threatened abortion and recurrent miscarriage.
The most popular substitute for Utrozhestan is Duphaston. The active ingredient of Duphaston is dydrogesterone, which is completely obtained chemically, but its characteristics are close to progesterone. This drug is also effective in preparing for IVF and threatened abortion. Duphaston is available in tablets for oral administration and has no side effects such as drowsiness and dizziness, and does not have a toxic effect on the liver. This drug has virtually no contraindications; it can be used without fear throughout the entire period of pregnancy. A significant advantage of Utrozhestan is the possibility of using it intravaginally, which is beneficial for women suffering from toxicosis in the first trimester. In addition, some doctors attribute its sedative effect to the positive aspects of this medicine.
Table: Utrozhestan and options for its replacement
| Release forms | Limitations in use | Adverse reactions | Manufacturer | price, rub. | |
| Utrozhestan | Capsules for oral and intravaginal administration. |
|
| Group or "Bezen Healthcare" (France, Belgium, Spain, Thailand). | From 380 for 28 capsules (100 mg). |
| Prajeesan | Capsules for oral and intravaginal use. |
|
| (India). | From 330 for 30 capsules (100 mg). |
| Iprozhin | Capsules for oral and vaginal administration. | Similar to Utrozhestan. | Identical to Utrozhestan. | Pharmaceutical (Italy). | From 350 for 30 capsules (100 mg). |
| Progesterone | Injection. |
|
| JSC Dalkhimfarm (Russia). | From 387 for 10 ampoules (1%, 1 ml). |
| Duphaston | Pills. | Hypersensitivity to the components of the drug. |
| Abbott Pharmaceutical Corporation (USA). | From 504 for 20 tablets (10 mg). |
Photo gallery: analogues of Utrozhestan
Prajisan is a complete analogue of Utrozhestan and is produced in India
Iprozhin contains progesterone, is used in the same cases as Utrozhestan, produced in Italy
Progesterone is available in the form of an injection solution
Duphaston, along with Utrozhestan, is the most popular gestagen
Having studied the personal experience of my wife and her friends, I can confirm that Utrozhestan and Duphaston are often used by women planning and expecting a child. Doctors prescribe these drugs when there is the slightest risk of developing a threatened abortion. When my wife was expecting her first baby, she resorted to Duphaston because of low progesterone levels and bleeding. Taking the drug increased the concentration of this hormone in the blood and the bleeding stopped. Duphaston had to be used for several months. No side effects were observed. During the second pregnancy, progesterone levels were also insufficient, but no visual signs of impending abortion were found. The doctor prescribed Utrozhestan to be taken orally. My wife took it for about a month. After the positive results of the following tests, the doctor advised that the medicine could be discontinued, but only gradually. The wife did not experience any negative reactions such as drowsiness or headaches.
Also, one of our family’s good friends was diagnosed with recurrent miscarriage. Regular use of these gestagens helped her give birth to a healthy child after several fruitless attempts.
I would like to note the experience of some of our compatriots living in Germany. In this country, medications to maintain pregnancy such as Utrozhestan or Duphaston are not prescribed. German doctors have a different approach. If the pregnancy was terminated, this means that there was a high risk of developing abnormalities in the fetus. We need to wait for the next pregnancy. And so on in a vicious circle. Therefore, these women come to their homeland, buy gestagens and take them while living in Germany. To select a treatment regimen, you can consult with our doctors via communication. Thus, pregnancy is maintained and healthy and happy children are born.
What does a short cervix mean during pregnancy?
The uterus is located in the pelvic area. Its shape resembles a pear, its main function is to bear a child. In the picture below you can see the structure of the uterus:
- neck,
- isthmus,
- fundus of the uterus,
- body of the uterus.
On average, a normal cervix in women is about 3-5 cm, usually 4. If its length is 2 cm or less, then they speak of a short cervix.
https://www.youtube.com/watch?v=ytpressru
A short cervix during pregnancy can be a congenital phenomenon or acquired after certain surgical interventions (for example, mechanical abortion). It also happens that the cervix can shorten due to a hormonal surge during pregnancy. The most dangerous period in this regard is considered to be from the 1st to the 27th week, the peak falls on the 16th.
If the cervix is shortened from birth, then when a woman is required to regularly visit a gynecologist from the moment of puberty, it will be possible to establish this long before the onset of pregnancy, and to take this point into account at the planning stage.
If a woman is already pregnant, then a simple examination on a gynecological chair will help establish this fact. If the doctor suspects something wrong, he will refer the patient for a transvaginal ultrasound, which will confirm or refute his assumptions.
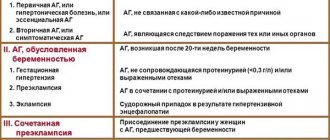
- A short cervix during pregnancy is one of the main signs of ICI (isthvicocervical insufficiency). This is a certain condition when pregnancy is at an increasing risk due to the physical impossibility of holding the constantly growing and gaining weight in the uterine area. Possible miscarriage or premature birth.
- The cervix, under pressure, gradually opens and softens ahead of schedule, which means there is a high risk of all kinds of infections reaching the baby.
- Plus, such an early opening means a rapid birth, which is fraught with ruptures, which then take quite a long time to heal under the condition of complete rest and minimal physical activity. And after the birth of the baby, complete rest is unlikely to be ensured.
The risks increase significantly if a woman has polyhydramnios, a large fetus, or is carrying several babies at once.
If you regularly go to the doctor and undergo all the examinations prescribed by him, then such a factor as a short cervix will not go unnoticed. And forewarned is forearmed!
Fortunately, medicine today has made great progress, so depending on the specific situation, doctors will offer several options for solving this problem.
If ICI is a consequence of hormonal changes in the body, then a treatment regimen with medications will be prescribed.
This procedure can be roughly compared to an inflated balloon, which is tied with a rope so that the air does not escape from the balloon.
This procedure is called cervical cervical cording and is performed under general anesthesia, the composition of which is carefully controlled by an anesthesiologist, taking into account the characteristics of the woman’s position and the duration of her pregnancy.
In some cases, a special gynecological ring or pessary is placed on the cervix, which keeps it in a stable state without the slightest risk of dilatation and the onset of premature labor.
Of course, it happens that even with the diagnosis of ICI, the pregnancy itself proceeded safely and ended in childbirth on time. But the chances of losing a child are great, is it worth the risk? If the doctor insists that certain measures are necessary, then it is better to take them.
We suggest you read: Co-sleeping with your child. Arguments for and against pediatrician Komarovsky
Much depends on the expectant mothers themselves. We must try to organize our daily life in peace and quiet, without unnecessary stress, quarrels and disputes. No excessive physical activity, and special gymnastics classes and swimming in the pool only after the official permission of a gynecologist!
https://www.youtube.com/watch?v=https:tRZSzJdGCyc
The 20th week is a kind of equator, approximately the middle of pregnancy. Most women can already feel the kicks of their baby in their tummy.
Now the active growth of the uterus has begun, it is moving towards the navel and can put pressure on the abdominal wall, causing the navel to protrude outward. Active growth of the uterus is accompanied by the risk of miscarriage in the presence of a short cervix.
Close supervision by a doctor is necessary during this period; a routine ultrasound is performed at 20-21 weeks, so you don’t have to go to the consultation again.
It’s not for nothing that in Russia people go on maternity leave at the 30th week. The belly is already quite large, women are quite clumsy at such a long time.
For women with a short cervix, the risk of premature birth has increased by an order of magnitude, especially if the pregnancy is multiple! The good news is that babies born at this stage are already viable with appropriate medical care.
But it’s better that it doesn’t come to that. Therefore, it’s time to relax, now without work it’s much easier to surround yourself with only pleasant emotions, sleep more, and be less nervous. If you have a short neck, you should not overexert yourself with physical activity and excessive activity.
Only peace and harmony!
32 weeks is the time to have your last ultrasound. If you have a short cervix, a specialist will definitely assess its condition at this time. There is less and less time before birth, which means that the baby has an increasingly greater chance of survival and normal development after birth.
But it’s better that he’s born on time. The recommendations remain the same - more sleep and rest.
Perhaps, at such a long time, the doctor will prescribe bed rest or even suggest hospitalization, so that the pregnant woman is under the supervision of doctors and certainly observes bed rest, which is not so easy to organize at home.
A short cervix during pregnancy is directly related to the threat of miscarriage, and, therefore, is often accompanied by increased uterine tone.
Signs of uterine tone:
- Pain in the lower abdomen.
- Discharge with blood.
- Feeling of a stone, hard, tense abdomen.
- Dizziness, nausea.
A gynecologist will be able to determine the increased tone of the uterus during an examination, and it can be confirmed using an ultrasound machine. In some cases, the expectant mother will be able to guess for herself based on the signs described above. If, with increased tone, a woman has a short cervix, the risks of miscarriage or premature birth increase significantly. Even hospitalization is possible.
https://www.youtube.com/watch?v=https:accounts.google.comServiceLogin
The causes of uterine tone can be malignant tumors, kidney diseases, liver diseases, cardiovascular and hypertension diseases. A woman’s psychological mood also plays an important role.
In a family where the expectant mother is emotionally stable, receives all possible support and care from family and friends, the phenomenon of uterine tone is much less common than in families where quarrels, scandals and showdowns are the daily norm of life.
Doctors, as a rule, prescribe hormonal treatment for women with uterine tone to compensate for the deficiency of the hormone progesterone in order to avoid miscarriage or premature birth.
This is a hormone necessary to maintain pregnancy, which is initially produced by the ovaries, and later by the placenta (as it is finally formed). Progesterone is needed at every stage of pregnancy, from conception to labor.
Without it, the woman’s body simply will not accept foreign DNA and will reject the fetus. But this is not all that the hormone progesterone contributes to a successful pregnancy. It controls the growth of the uterus, preparing it for a strong increase in size.
We invite you to read: Divigel instructions for use when planning pregnancy
It prepares the mammary glands to produce colostrum and then breast milk. It stimulates the growth of the endometrium (the inner layer of the uterus), thereby creating fertile soil for the successful attachment of the embryo, and then its successful growth and active development.
Ultimately, it relaxes the walls of the uterus to avoid hypertonicity.
Progesterone deficiency with a short cervix necessarily requires additional measures to maintain pregnancy. Suturing or installing a pessary is no longer enough; hormonal therapy is also necessary.
Utrozhestan is a synthetic analogue of the hormone progesterone. The hormone molecules are surrounded by peanut butter, since in this form the body is able to accept it and absorb it as much as possible.
Composition of the drug:
- progesterone;
- peanut butter;
- soy lecithin;
- gelatin;
- glycerol
The medicine may interact with other drugs because it does not contain substances that could react negatively to such an interaction.
Progesterone deficiency can occur at any stage of pregnancy planning. But in the 1-2 trimesters, uterine activity is not so great. The danger of a lack of progesterone lies in the fact that the egg (or the fetus subsequently) will be rejected by the mother's body.
And against the background of redistribution of progesterone production between the ovaries and placenta, any violation is fraught. Therefore, at these times there is no danger in taking Utrozhestan. As for the 3rd trimester, excess progesterone is more dangerous here than its deficiency.
Therefore, taking the medicine is no longer advisable.
Like any other drug, Utrozhestan contains a number of contraindications (liver failure, diabetes, bronchial asthma, and so on). Side effects may include dizziness, lethargy, and drowsiness, so after taking it it is better to stay at home for some time.
There are two ways to take the medicine - capsules or suppositories. Typically taken 3 times a day for 2-3 weeks, but this schedule may vary depending on the specific situation.
https://www.youtube.com/watch?v=ytdevru
Never engage in self-diagnosis, much less self-medication! Only a doctor can recommend Utrozhestan and calculate the individual dosage! Therefore, at the first signs of uterine tone, knowing at the same time that you have a short cervix, and, therefore, there is already a high risk of miscarriage/premature birth, you should urgently run to the doctor. And before taking it, be sure to try to relax and calm down.